Abstract
Disclosure of HIV status to sexual partners in the context of prevention of mother-to-child transmission (PMTCT) may contribute to improved PMTCT outcomes. We administered a questionnaire to 200 women with HIV enrolled in a PMTCT study during pregnancy at 12 months after birth in Western Kenya between May-September 2017. Descriptive analysis of disclosure patterns and multivariate analysis of factors associated with male partner reactions is presented. Among 180 (90%) women who reported having a male partner, 95.5% reported disclosing their HIV status to that partner. The majority of women (82.8%) reported disclosure occurred within one year of their diagnosis, with 62.7% occurring within one week. The most common forms of disclosure were: self-disclosure (55.4%), during couple’s HIV testing and counselling (CHTC) (31.5%), or at an antenatal care visit (7.7%). Most women (87.5%) reported that male partner reactions to their HIV status disclosure were positive. Those with negative reactions reported their partners were confused, annoyed, or threatened to leave, however there were no reports of intimate partner violence (IPV) or break ups. Disclosure via CHTC was associated with a positive male partner reaction compared to self-disclosure (adjusted OR (aOR) 20.2, 95% Confidence Interval (CI) 1.8 – 221.4). Those in concordant HIV status partnerships were more likely to have a positive reaction (aOR. 6.7, 95% CI 1.7 – 26.6). Women experiencing frequent verbal IPV were less likely to report a positive response (aOR 0.21, 95%CI 0.1 – 0.8). Most postpartum women with HIV in this cohort had disclosed to their male partners early after diagnosis and experienced a positive reaction. However, a minority had still not disclosed by 12 months after the birth and some experienced negative reactions to disclosure. The form of status disclosure and impact of intimate partner violence should be given greater attention within the context of PMTCT.
Keywords: HIV disclosure, women, PMTCT, male partner
Introduction
Of the estimated 1.4 million women living with HIV who give birth each year, over 90% live in sub-Saharan Africa.(UNAIDS, 2012) Involvement of male partners of these women in supporting uptake of prevention of mother to child transmission (PMTCT) has been shown to improve adherence to antiretroviral medication and PMTCT outcomes.(Hodgson et al., 2014; Spangler et al., 2018) Disclosure of the woman’s HIV status to her male partner is a crucial step in involving the male partner in PMTCT care.(Jasseron et al., 2013)
Disclosure affects uptake and retention at all points along the PMTCT cascade (Chinkonde et al., 2009; Nassali et al.,2009; Olagbuji et al., 2011) Although some women experience negative consequences, many women who disclose to their male partner report increased social support, and have higher ARV use for PMTCT, as well as increased HIV-free survival of their infants. (Kiweewa et al., 2015)Spangler et al (2014)(Aluisio et al., 2011) Non-disclosure is associated with poorer adherence (Mepham, Zondi, Mbuyazi, Mkhwanazi, & Newell,2011), increased home delivery, (Awiti Ujiji et al.,2011) and higher MTCT ((McGrath et al., 2018)Torpey, Kabaso, et al.,2012)(Jasseron, et al., 2013).
While fears of abandonment, violence and discrimination prior to disclosure are common, reports suggest most women do not experience these negative reactions.(Medley, Garcia-Moreno, McGill, & Maman, 2004) Yet, negative outcomes do occur with as many as 30% of women reporting a partner conflict, loss of financial support, or separation and up to 15% of women report experiencing violence related to disclosure (Kiweewa, et al., 2015; Odiachi et al., 2018).
Numerous studies indicate the importance of status disclosure for uptake, adherence, and retention in PMTCT; however, little is known about male partner reactions to an HIV-positive status disclosure from a female partner. We report on patterns of disclosure and factors associated with male partner reactions to status disclosure among postpartum women living with HIV in Kenya.
Methods
Study Design
This article reports on findings from a cross-sectional survey with 200 women living with HIV at 12 months postpartum. Survey questionnaires were administered as part of a larger convergent parallel mixed methods study in western Kenya conducted May to September 2017, including the questionnaire with postpartum mothers living with HIV and semi-structured interviews with male partners. We report on postpartum mother respondents. This study was nested within the Mother-Infant Visit Adherence and Treatment Engagement (MOTIVATE) parent study (R01HD0808477; Abuogi, Turan, ClinicalTrials.gov NCT0249117).(Odeny et al., 2018)
Study Population
Women were sampled within the ongoing MOTIVATE parent study. Details of the MOTIVATE trial have been previously described elsewhere (Odeny, et al., 2018). In brief, this cluster randomized trial is comparing the impact of behavioural interventions (text messaging and community-based mentor mothers) on adherence to ART and retention in care among pregnant and postpartum women living with HIV in Kenya. MOTIVATE study clinics are randomized to four trial arms: 1) control, 2) text messaging alone, 3) mentor mothers alone, or 4) text messaging and mentor mothers. Participants for this sub-study were eligible if they remained active in the MOTIVATE study and were at least 12 months postpartum (to ensure the survey did not impact parent study outcomes). Participants were purposively selected based on the above eligibility criteria until the pre-determined sample size was achieved with efforts to roughly balance geographic regions. Potential participants were contacted by phone to learn their interest in sub-study participation. Those who expressed interest underwent in-person consenting and received a small transport reimbursement.
Data Collection
Participants completed an in-person questionnaire verbally-administered by female interviewers in their preferred language (Luo, Swahili, or English). Data were collected on tablet computers using the RedCap Mobile Application (Harris et al., 2009) by interviewers and uploaded to the RedCap server maintained by the University of Colorado, Denver. The questionnaire was designed by adapting validated scales on relevant themes and by the researchers based on their expertise. (Table 1) The questionnaire was translated by local certified translators and pilot tested prior to implementation.
Table 1.
Questionnaire topics and validated source
| Topic | Details | Source |
|---|---|---|
| Sociodemographics | - Age in years (continuous) - Sub-county of residence (categorical) - Completed primary education (binary) - Parity (continuous) - Electricity in the home (binary) - Any food insecurity in the past month (binary)1 - Diagnosed with HIV prior to pregnancy (binary)2 |
Demographic and Health Survey (Kenya National Bureau of Statistics et al., 2015) |
| Depression | - Major depression (binary):3 eight-item scale | Patient Health Questionnaire Depression Scale (PHQ-8) (Kroenke et al., 2009; Monahan et al., 2009) |
|
Stigma Internal/self-stigma |
- Experienced any internal HIV stigma (binary):4 six-item scale | Modified self-stigma subscale from People Living with HIV Stigma Index (International Planned Parenthood Federation, 2008) |
| Anticipated stigma | - Experienced any anticipated HIV stigma (binary):5 five-item scale | Adapted from relevant research studies (Siedner et al., 2012; Turan et al., 2011; Weiser et al., 2006) |
| Relationship satisfaction | Satisfied with relationship (binary)6 | Investment Model Scale: satisfaction level facet (Rusbult, Martz, & Agnew, 1998) |
| Intimate Partner Violence | Experienced frequent emotional IPV in current relationship (binary)7 | Adapted from previous measures of negative and positive interactions/affective support (Schuster, Kessler, & Aseltine, 1990; Turner, Frankel, & Levin, 1983) |
| Experienced frequent physical IPV in current relationship (binary)8 | ||
| Intervention exposure | - Intervention group in parent MOTIVATE! study that was not the control group (binary)9 | Study investigators |
Question asks: in the past 4 weeks how often did it happened that there was no food to eat of any kind in your house because of lack of resources to get food (response options: never, rarely, sometimes, or often). Respondents indicating at least rarely were considered to have food insecurity. Reference group: households never experiencing food insecurity the past month
Reference group: diagnosed with HIV during the most recent pregnancy.
A score of 10 or greater indicates major depression
Response options for six-items are: never, rarely, sometimes, or often. If a participant answered at least rarely to any item, she was considered to have experienced internal stigma. Reference group: participants who reported never experiencing any of the six items.
Response options for five-items are: strongly disagree, disagree, agree, strongly agree. If a participant answered “agree” or “strongly agree” to any item, she was considered to have experienced anticipated stigma. Reference group: participants who reported disagreeing (or strongly disagreeing) to all items.
Question asks: How much do you agree with the following statement: I feel satisfied with our relationship (response options: not at all, a little, somewhat, mostly, almost completely, or completely). Respondents indicating at least mostly were considered to have relationship satisfaction. Reference group: respondents indicating somewhat or less agreement.
Question asks: How often has your partner said cruel or hurtful things to you during a disagreement (all the time, most of the time, more often than not, occasionally, rarely, never). Frequent emotional IPV considered those who report one of the first three response categories. Reference group: occasionally/never/rarely
Question asks: How often has your partner said cruel or hurtful thing to you during a disagreement (all the time, most of the time, more often than not, occasionally, rarely, never). Frequent emotional IPV considered those who report one of the first three response categories. Reference group: occasionally/never/rarely
Intervention groups include: community mentor mothers (cMM) only, text messaging reminders only, and cMM + text. Reference group: participants in control group
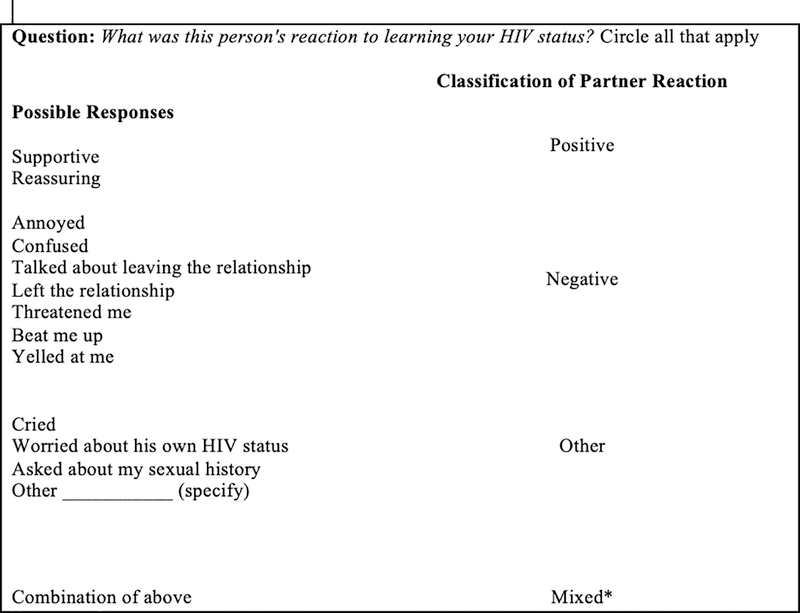
To determine women’s perception of their male partner reaction to learning about their HIV positive status, we asked “What was this person’s reaction to learning your HIV status? the region (Deribe, Woldemichael, Wondafrash, Haile, & Amberbir, 2008). Figure 1 demonstrates possible responses and our classification of the male partner reaction as positive, negative, mixed, or other.
Figure 1.
Assessment of male partner’s reaction to women’s disclosure of HIV status. Note: *Reactions were categorized as mixed if women reported at least one positive and one negative response as outlined in the table.
Statistical Analysis
The primary outcome was woman’s report of a positive reaction from her male partner after HIV status disclosure. Male partner reactions were categorized as a positive reaction, compared to negative/other/mixed as described in Figure 1. Survey data were exported into Stata 14 for analysis. Descriptive analysis of participant characteristics and relationship dynamics by male partner reaction to disclosure are described. Variables potentially associated with male partner reaction were explored in univariate analysis, including sociodemographic characteristics of the woman and her male partner, depression and stigma, method and timing of disclosure, the woman’s knowledge of her male partner’s HIV status, and physical and emotional intimate partner violence. Bivariate analysis using Pearson’s chi-square for categorical variables and t-tests for continuous variables were conducted to examine factors associated with a positive reaction from the male partner to learning the woman’s HIV status. Multivariable logistic regression was then conducted adjusting for control variables, including age, education, and electricity in the home (a proxy for household wealth), variables known to be associated with status disclosure outcomes in the literature, such as time from diagnosis and male partner HIV status, and variables significantly correlated with partner reaction in the bivariate models.
Ethical Considerations
Ethical approval was obtained from participating institutions including the Kenya Medical Research Institute (KEMRI), the University of Colorado, Denver (UCD), and the University of Alabama at Birmingham (UAB). All participants provided individual written consent. Women self-reporting current intimate partner violence or major depression were referred to appropriate resources.
Results
Sociodemographics
Of the 200 women surveyed, 180 (90%) reported having a main romantic male partner in the past 12-month postpartum period. Of those 180 women, 171 (95%) reported disclosing their HIV-positive status to the male partner and 168 (93%) women reported the reaction of that partner. Three women (2%) of the 171 who disclosed their status reported that they did not know or wish to say how the partner reacted.
Table 2 presents the characteristics of the 168 women who gave a specified reaction from the male partner to learning their HIV status. The mean age of women who disclosed their status and reported a reaction was 28.2 years (standard deviation (SD) 5.0). (Table 2) Participants came primarily from Migori county (50%) (mixed urban/rural), followed by Kisumu (31%), the most urban location, and Homa Bay (19%), the most rural location. More than half (54%) had completed a primary education or higher. On average, women reported four pregnancies (SD 2.0). Only 19% of homes had electricity and 44% experienced food insecurity in the past month. The majority of women who disclosed to their partner were married (91%) and 42% report co-wives/polygamy. Over half (58%) of women reported knowing their HIV status prior to the current pregnancy and all were on ART at the time of the survey. Twenty-six percent met the criteria for having major depression. Over half (55%) reported experiencing any internalized HIV-related stigma, while 57% reported anticipated HIV-related stigma. Based on four trial arms, a smaller proportion of women were recruited from the control arm of the parent study (20%) as compared to one of three intervention arms (80%).
Table 2.
Characteristics of surveyed postpartum women living with HIV who report disclosing their HIV status to the male partner
| Male partner reaction | ||||
|---|---|---|---|---|
| Total | Positive | Negative/Mixed | p-value | |
| N=168 (%) or mean (SD) | N=147 (%) or mean (SD) | N=21 (%) or mean (SD) | ||
| Age of woman (mean, years) | 28.2(5.0) | 28.3(5.1) | 27.6(5.0) | 0.56 |
| Location (county) | 0.02 | |||
| Homa Bay | 32 (19.2) | 31 (96.9) | 1 (3.1) | |
| Kisumu | 52 (31.1) | 40 (76.9) | 12 (23.1) | |
| Migori | 83 (49.7) | 75 (90.4) | 8 (9.6) | |
| Education | 0.77 | |||
| Less than primary education | 77 (45.8) | 68 (88.3) | 9 (11.7) | |
| Primary education or higher | 91 (54.2) | 79 (86.8) | 12 (13.2) | |
| Mean number of pregnancies | 3.91 (1.8) | 3.91 (1.74) | 3.90 (1.87) | 0.99 |
| Electricity in home | 0.19 | |||
| No | 135 (80.8) | 121 (89.7) | 14 (10.4) | |
| Yes | 32 (19.2) | 26 (81.3) | 6 (18.8) | |
| Food Insecurity | 0.20 | |||
| No | 94 (56.0) | 85 (90.4) | 9 (9.6) | |
| Yes | 74 (44.1) | 62 (83.8) | 12 (16.2) | |
| Knowledge of HIV status prior to pregnancy | 0.01 | |||
| No | 69 (41.6) | 55 (79.7) | 14 (20.3) | |
| Yes | 97 (58.4) | 90 (92.8) | 7 (7.2) | |
| Major depression | 0.43 | |||
| No | 124 (73.8) | 107 (86.3) | 17 (13.7) | |
| Yes | 44 (26.2) | 40 (90.9) | 4 (9.1) | |
| Internalized HIV Stigma | 0.08 | |||
| No | 72 (45.3) | 67 (93.1) | 5 (6.9) | |
| Yes | 87 (54.7) | 73 (83.9) | 14 (16.1) | |
| Anticipated HIV Stigma | 0.48 | |||
| No | 68 (42.8) | 58 (85.3) | 10 (14.7) | |
| Yes | 91 (57.2) | 81 (89.0) | 10 (11.0) | |
| Study Intervention | 0.19 | |||
| Intervention | 134 (79.8) | 115 (85.8) | 19 (14.2) | |
| Control | 34 (20.2) | 32 (94.1) | 2 (5.9) | |
Male Partner and Relationship Characteristics
Table 3 presents the male partner characteristics and relationship dynamics, stratified by type of partner reaction. The mean age of male partners was 36 years (SD 9) with 70% having a primary education or higher. The most common relationship length was less than five years. The majority of women (61%) report being satisfied with the relationship. Frequent physical intimate partner violence (IPV) was reported by 11% of relationships, while emotional/verbal IPV was reported in 13% of relationships. Almost all women (95%) reported that their male partner had an HIV test. Of those who knew their partner’s HIV status (91%), 71% of male partners were reported to be HIV-positive and 29% HIV-negative. According to the women’s reports, 55 (39%) of the men who had been tested learned their HIV status prior to the woman, but 35% learned their status after the woman was diagnosed.
Table 3.
Male partner characteristics and relationship dynamics
| Male partner reaction | ||||
|---|---|---|---|---|
| Total | Positive | Negative/Mixed | p-value | |
| N=168 (%) or mean (SD) | N=147(%) or mean (SD) | N=21(%) or mean (SD) | ||
| Type of partner | 0.93 | |||
| Husband | 152 (90.5) | 133 (87.5) | 19 (12.5) | |
| Live-in partner | 10 (6.0) | 9 (90.0) | 1 (10.0) | |
| Boyfriend/other | 6 (3.6) | 5 (83.3) | 1 (16.7) | |
| Report co-wife(s) | 0.90 | |||
| No | 68 (58.5) | 77 (89.5) | 9 (10.5) | |
| Yes | 61 (41.5) | 55 (90.2) | 6 (9.8) | |
| Age of male partner (mean yrs) (sd) | 36.2(9.1) | 36.3(9.4) | 35.6(5.9) | 0.72 |
| Partner education | 0.75 | |||
| Less than primary education | 54 (33.1) | 48 (88.9) | 6 (11.) | |
| Primary education or higher | 109 (66.9) | 95 (87.2) | 14 (12.8) | |
| Length of relationship | 0.88 | |||
| 0–5 years | 61 (37.0) | 53 (86.9) | 8 (13.1) | |
| 6–10 years | 58 (35.2) | 52 (89.7) | 6 (10.3) | |
| >10 years | 46 (27.9) | 40 (87.0) | 6 (13.0) | |
| Satisfied with relationship | 0.07 | |||
| Yes | 102(60.7) | 93(91.2) | 9 (8.8) | |
| No | 66 (39.3) | 54 (81.8) | 12 (18.2) | |
| Verbal IPV | 0.004 | |||
| Rare/never | 143(86.7) | 129 (90.2) | 14 (9.8) | |
| Frequent1 | 22(13.3) | 15 (68.2) | 7 (31.8) | |
| Physical IPV | 0.25 | |||
| Rare/never | 145 (88.4) | 128 (88.3) | 17 (11.7) | |
| Frequent2 | 19 (11.6) | 15 (79.0) | 4 (21.1) | |
| Partner HIV status | 0.18 | |||
| HIV negative | 44 (26.2) | 35 (79.6) | 9 (20.5) | |
| HIV positive | 106 (63.1) | 96 (90.6) | 10 (9.4) | |
| Unknown | 18 (10.7) | 16 (88.9) | 2 (11.1) | |
| When partner learned his status | 0.51 | |||
| Prior to woman | 55 (38.7) | 51(92.7) | 4 (7.3) | |
| At the same time | 38 (26.7) | 34 (89.5) | 4 (10.5) | |
| After woman | 49 (34.5) | 42 (85.7) | 7 (14.3) | |
| Time to disclosure (mean days) (sd) | 41.5 (87.9) | 46.9 (92.6) | 2.6 (4.1) | 0.03 |
| Method of disclosure to partner | 0.02 | |||
| Self-disclosed | 90 (54.6) | 77 (85.6) | 13 (14.4) | |
| Couples Testing | 53 (32.1) | 52 (98.1) | 1 (1.9) | |
| Other | 22 (13.3) | 17 (77.3) | 5 (22.7) | |
IPV-Intimate Partner Violence
Participants who report their male partner says cruel or angry things to them all of the time, most of the time, or more often than not, during disagreements
Participants who reported their male partner physically hurts them all of the time, most of the time, or more often than not, during disagreements
HIV status disclosure and male partner reactions
Eight participants with a male partner (5%) reported non-disclosure of their HIV status. Women who did not disclose their status were more likely to be newly diagnosed as HIV-positive (p<0.05) and to report internalized (p<0.01) and anticipated (p<0.001) stigma. Reasons for non-disclosure included fear of partner’s response such as anger, physical violence, or leaving, concern that the partner would judge the woman as unfaithful or a bad person, and not having enough time or not wanting to worry the partner.
The majority of women who did disclose (95%), reported disclosure to their male partner occurred within one year of their diagnosis (83%), with 63% of disclosure occurring within one week. The longest reported time to disclosure was more than five years from diagnosis. Compared to those who disclosed during couple’s HIV testing and counselling, women who self-disclosed and those whose partner found out in another manner (during ANC visit, someone else disclosed) time to disclosure was significantly longer (p=0.53 and p=0.03 respectively).
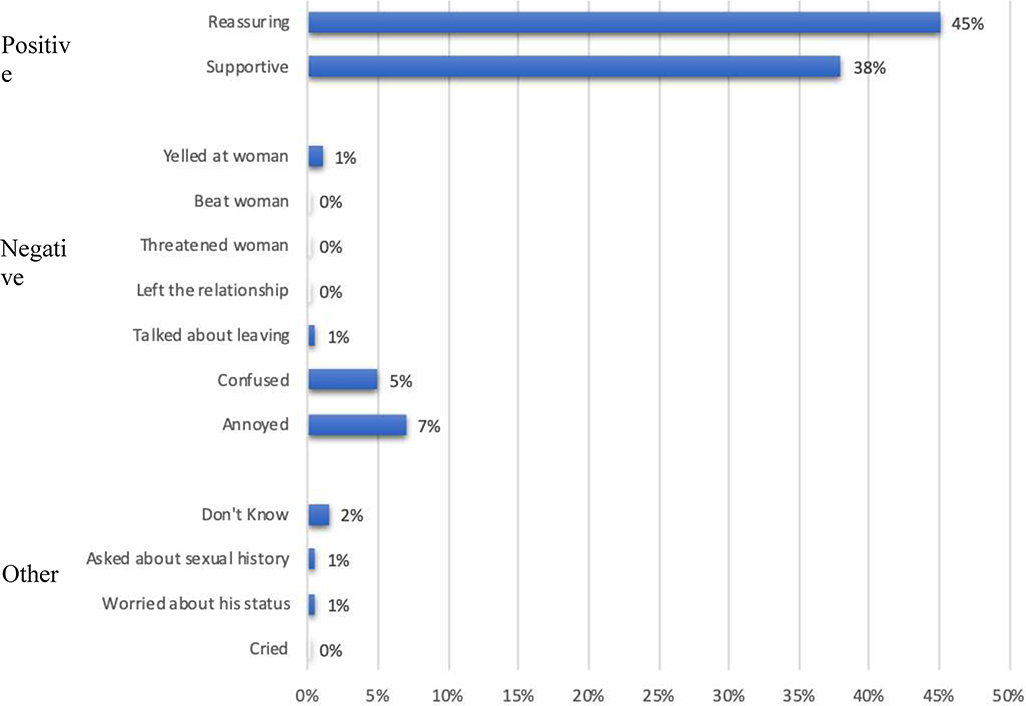
The most common form of disclosure was self-disclosure (i.e., women telling their male partner their status on their own; 54.6%), followed by couple’s HIV counselling and testing (32.1%), and other (13.3), such as during an antenatal care visit. There were no reports of gender-based violence, threats or break up as a result of disclosure.
Characteristics associated with positive male partner reactions to HIV status disclosure
A total of 147 (87.5%) women reported a positive male partner reaction to HIV status disclosure while 21 (12.5%) reported a negative or mixed reaction. In the univariable models, neither age nor education of the woman or male partner were associated with type of male partner reaction. (Table 4) The county in which women reside, however, was associated with partner reaction (p=0.04). In addition, when the woman was diagnosed (during or prior to pregnancy) was associated with partner reaction (p=0.02). Similarly, the male partner’s HIV status (unknown, positive, or negative) was marginally associated with his reaction, with a trend towards a positive reaction (OR 2.5, 95% Confidence Interval (CI) 0.9–6.6; p=0.07). Women who disclosed to male partners via CHTC were nearly nine times more likely to have a positive partner reaction compared to self-disclosure in the unadjusted model (OR 8.8, 95%CI 1.1–69.1; p=0.04). Women experiencing verbal intimate partner violence, on the other hand, were much less likely to experience a positive response to disclosure (OR 0.23, 95%CI 0.1–0.7; p=0.01) but this was not the case for women reporting physical violence (p=0.26). Timing of disclosure and length of relationship were not associated with type of reaction.
Table 4.
Factors associated with positive male partner reaction t o woman’s HIV status disclosure
| Odds of a positive reaction from male partner after status disclosure | ||||
|---|---|---|---|---|
| Odds Ratio | p-value | Adjusted Odds Ratio* | p-value | |
| (95% Confidence Interval) (n=168) | (95% Confidence Interval) (n=151) | |||
| Age - female participant_ | 1.0 (0.9 – 1.1) | 0.555 | 0.9 (0.8 – 1.2) | 0.806 |
| Age - male partner | 1.0 (1.0 – 1.1) | 0.720 | 1.0 (0.9 – 1.1) | 0.396 |
| Completed primary education - female participant | 0.9 (0.3 – 2.2) | 0.770 | 0.8 (0.2 – 3.5) | 0.761 |
| Completed primary education–male partner | 0.8 (0.3 – 2.3) | 0.751 | 1.2 (0.2 – 7.9) | 0.816 |
| Electricity in the home | 0.5 (0.2 – 1.4) | 0.196 | 2.6 (0.4 – 15.6) | 0.303 |
| Parent study intervention Exposure (yes)1 | 0.4 (0.1 – 1.7) | 0.207 | 0.3 (0.0 – 33.4) | 0.657 |
| Location | ||||
| Kisumu | ref. | ref. | ||
| Homa Bay | 9.3 (1.1 – 75.4) | 0.037 | 34.9 (0.7 – 1584.8) | 0.068 |
| Migori | 2.8 (1.1 – 7.4) | 0.037 | 20.7 (1.6– 272.9) | 0.021 |
| Diagnosed prior to recent pregnancy (yes) | 3.3 (1.2 – 8.6) | 0.016 | 1.5 (0.2 – 13.7) | 0.735 |
| Any internalized stigma (yes) | 0.4 (0.1 – 1.2) | 0.085 | --- | |
| Any anticipated stigma (yes) | 1.4 (0.5 – 3.6) | 0.486 | --- | |
| Partner HIV status | ||||
| HIV negative | ref | ref | ||
| HIV positive | 2.5 (0.9 – 6.6) | 0.071 | 9.0 (1.6 – 52.3) | 0.014 |
| Unknown | 2.1 (0.4 – 10.6) | 0.389 | 2.6 (0.3 – 23.0) | 0.390 |
| Method of partner disclosure | ||||
| Self-disclosed | ref | ref | ||
| Couples Testing | 8.8 (1.1 – 69.1) | 0.039 | 46.4 (2.7– 807.4) | 0.009 |
| Other | 0.6 (0.2 – 1.8) | 0.347 | 0.5 (0.1 – 2.6) | 0.402 |
| When did partner learn status | ||||
| Prior to woman | ref | |||
| At the same time | 0.7 (0.2 – 2.9) | 0.584 | --- | |
| After woman | 0.5 (0.1 – 1.7) | 0.254 | --- | |
| Time to disclosure (# of days) | 1.0 (0.9 – 1.1) | 0.19 | --- | |
| Length of relationship | ||||
| 0–5 years | ref | |||
| 6–10 years | 1.3 (0.4 – 4.0) | 0.640 | --- | |
| >10 years | 1.0 (0.3 – 3.1) | 0.991 | --- | |
| Satisfied with relationship | 2.3 (0.9 – 5.8) | 0.08 | --- | |
| Emotional IPV | ||||
| Frequent2 | 0.2 (0.1 – 0.7) | 0.01 | 0.2 (0.0 – 1.0) | 0.052 |
| Rare/Never | ref | ref | ||
| Physical IPV | ||||
| Frequent3 | 0.5 (0.1 – 1.7) | 0.26 | --- | |
| Rare/Never | ref | |||
Adjusting for standard demographic variables of the woman and male partner (age, education), electricity (proxy for household wealth), variables significantly associated with the outcome in the univariable models (location, method of disclosure, when woman was diagnosed), and theoretically important variables (male partner HIV status and exposure to parent study interventions)
IPV=Intimate Partner Violence
Participants who received cMM alone, text messages alone, or both (reference: control arm)
Participants who report their male partner says cruel or angry things to them all of the time, most of the time, or more often than not, during disagreements
Participants who report their male partner physically hurts them all of the time, most of the time, or more often than not, during disagreements
In the multivariable model, adjusting for significant covariates, method of disclosure remained associated with a positive male partner reaction: partners disclosing through CHTC had more than twenty times the likelihood of a positive male partner reaction, compared to women’s self-disclosure (adjusted OR (aOR) 20.2, 95%CI 1.8–221.4; p=0.01). (Table 4) Those in concordant partnerships, where the male partner had a known HIV-positive diagnosis, were over six times more likely to have a positive male partner reaction, compared to couples where the male partner was HIV-negative (aOR. 6.7, 95%CI 1.7–26.6; p=0.01). Women experiencing frequent emotional IPV remained much less likely to experience a positive reaction to HIV status disclosure in the adjusted model (aOR 0.21, 95%CI 0.1–0.8; p=0.02). Location and time of diagnosis were not significantly associated with adjusted odds of a positive male partner reaction to women’s status disclosure, although there was a trend towards a positive reaction among women living in Migori (aOR 6.2, 95%CI 0.9–41.9; p=0.06) compared to Kisumu sub-county.
Discussion
Our findings show that the majority of postpartum women living with HIV in our sample in this setting in Western Kenya had disclosed their HIV status to their male partners. However, our study found higher prevalence of disclosure to male partners than studies in Kenya. (Onono, Cohen, Jerop, Bukusi, & Turan, 2014) In a recent national survey at over 140 clinics in Kenya, non-disclosure was over 10% among postpartum women with HIV. (Kinuthia et al., 2018) Our high disclosure of 95% may be a result of the sample selected, which included women participating in an HIV adherence and retention trial and retained in the study for at least 12 months postpartum. In addition, through the study interventions, many of the women received support disclosure. Further, in recent years, Kenya has implemented intensive efforts to improve partner disclosure, social desirability to report disclosure, and increased acceptance of HIV status in this high-prevalence region of Kenya are other potential explanations. Previous studies from other areas of sub-Saharan Africa (Zambia and Zimbabwe), however, have also found similarly high prevalence of status disclosure (Hampanda and Rael, 2018; Shamu, Zarowsky, Shefer, Temmerman, & Abrahams, 2014).
Most reports on women’s disclosure do not describe time to disclosure. This is important during pregnancy as rapid disclosure may facilitate earlier uptake of PMTCT interventions resulting in reduced MTCT and improved health outcomes for women. We found that nearly two thirds of women disclosed in the first week after learning their HIV diagnosis. Similarly, a recent study in Uganda found three quarters of women had disclosed by four months after study enrollment.(Naigino et al., 2017) A study from South Africa found that women who entered ANC knowing their HIV diagnosis but not having disclosed were unlikely to disclose to their male partners.(Myer et al., 2017) This implies that women who do not disclose rapidly may have additional interpersonal barriers that need to be properly addressed or that disclosure may not acceptable in such relationships.
Importantly, we identified several factors that are related to male partner’s reaction to disclosure from women, including the male partner’s HIV status, method of disclosure, and presence of emotional violence in the relationship. It is not surprising that disclosure of one’s HIV positive status to a partner also living with HIV would be more likely to result in a positive reaction than to an HIV negative partner. However, a study recently done in eastern Africa shows that men who disclose within discordant relationships feel more supported than women, revealing the vulnerability of women living with HIV.(Maeri et al., 2016) PMTCT counseling may be able to enhance disclosure and health behaviors by collecting data on the male partner’s status and providing additional psychosocial support, such as assisted disclosure and peer support, for women in serodiscordant partnerships. We found that women who reported being satisfied in their relationships showed a trend towards a more positive male partner reaction; a finding that may warrant further exploration and possible couple’s interventions to support relationship skills that facilitate positive disclosure reactions.
This is the first study to our knowledge to reveal that the mode of disclosure is very important in predicting the type of male partner reaction. Women who had assisted disclosure in the form of CHTC reported more frequent positive male partner reaction than those who self-disclosed or disclosed through another means, such as during a regular ANC visit. CHTC may result in more positive reactions as there is pre-test counseling and discussion of the implications of discordancy among couples prior to testing. Alternatively, women who undergo CHTC may already feel comfortable disclosing to their partners as one study in Malawi showed that all women who returned with their male partner for CHTC had already disclosed their status. (Rosenberg et al., 2017) Yet, only a third of women in this cohort underwent couple’s testing indicating that it may not be universally offered as a service or there may be challenges to uptake of the service. Prior studies have shown barriers to couple’s testing include time to test as a couple and not being aware or discussing the benefits of CHTC. (Muhindo, Nakalega, & Nankumbi, 2015) Further, not all CHTC experiences are positive with some males reportedly feeling coerced into testing in this setting and negative outcomes still occurring. (Musheke, Bond, & Merten, 2013) Several approaches to increasing uptake of CHTC have shown promise including invitation letters, community tracing, and home-based CHTC. (Akama et al., 2018; Becker et al., 2014; Rosenberg et al., 2015; Turan et al., 2018) Given the positive associations found in our study between CHTC and positive male partner reactions to disclosure, efforts to increase uptake of CHTC may help support women during PMTCT while acknowledging it may not be ideal for every couple.
IPV emerged as being strongly associated with male partner reaction to HIV disclosure in our study with women who were experiencing frequent verbal IPV much less likely to have a positive male partner reaction. Prior studies have shown the impact of IPV within relationships on PMTCT before and after disclosure. Fear of IPV is commonly cited by women concerned about disclosing their HIV status to a partner. There are mixed reports on actual prevalence of verbal and physical IPV after disclosure.(Colombini, James, Ndwiga, Integra, & Mayhew, 2016) While Kenya has recently introduced standardized IPV screening in PMTCT services, there are not services available except in more extreme cases and focus is on physical violence. (Health, 2016) The importance of identifying all forms of IPV and having interventions and support services to address it when found is emerging as a key factor in PMTCT. (Kennedy, Haberlen, Amin, Baggaley, & Narasimhan, 2015)
The strengths of this study include the systematic assessment of disclosure and male partner reactions to disclosure using standardized questions in a high HIV prevalence setting in Kenya. Limitations include non-random sample of women retained at least 12 months postpartum in the parent intervention trial, which may have biased the sample towards women who disclosed and had positive reactions. We did not select a random sample of trial participants, so it was not possible to determine impact of the parent study interventions (community mentor mother and text messaging) on disclosure. Due to the sample size, some estimates lack precision. Also, the cross-sectional nature of this study precluded prospective collection of time to disclosure and did not allow us to draw conclusions about the directionality of observed associations. For example, does IPV cause negative male partner reactions or do negative reaction result in IPV? Results may also have been affected by recall and social desirability bias.
Conclusions
The majority of postpartum women living with HIV in this sample disclosed to their male partners early after diagnosis and experienced a positive reaction. An increased focus on screening for intimate partner violence prior to disclosure while utilizing CHTC as a method for supported disclosure may increase positive reactions to disclosure among male partners improving support and PMTCT outcomes.
Figure 2. Proportion of women reporting specific male partner reactions1.
1Participants could report more than one response
Acknowledgements
We acknowledge the women who participated in this study and the support of the Director KEMRI and the Director CMR.
Funding: This work was supported by the National Institute of Child Health and Human Development under Grant R01HD080477 and the National Institute of AIDS and Infectious Disease funded Colorado HIV Research Training Program under grant 4T32AI007447. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Child Health and Human Development or the National Institutes of Health. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Disclosure: No potential conflict of interest was reported by the authors
References
- Akama E, Mburu M, Mutegi E, Nyanaro G, Otieno JP, Ndolo S,… Onono M (2018). Impact of a Rapid Results Initiative Approach on Improving Male Partner Involvement in Prevention of Mother to Child Transmission of HIV in Western Kenya. AIDS Behav, 22(9), pp. 2956–2965. doi:10.1007/s10461-018-2140-3 Retrieved from 10.1007/s10461-018-2140-3https://www.ncbi.nlm.nih.gov/pubmed/29948337 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/29948337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aluisio A, Richardson BA, Bosire R, John-Stewart G, Mbori-Ngacha D, & Farquhar C (2011). Male antenatal attendance and HIV testing are associated with decreased infant HIV infection and increased HIV-free survival. J Acquir Immune Defic Syndr, 56(1), pp. 76–82. doi:10.1097/QAI.0b013e3181fdb4c4 Retrieved from 10.1097/QAI.0b013e3181fdb4c4https://www.ncbi.nlm.nih.gov/pubmed/21084999 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/21084999 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker S, Taulo FO, Hindin MJ, Chipeta EK, Loll D, & Tsui A (2014). Pilot study of home-based delivery of HIV testing and counseling and contraceptive services to couples in Malawi. BMC Public Health, 14, p 1309. doi:10.1186/1471-2458-14-1309 Retrieved from 10.1186/1471-2458-14-1309https://www.ncbi.nlm.nih.gov/pubmed/25526799 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/25526799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colombini M, James C, Ndwiga C, Integra t., & Mayhew SH (2016). The risks of partner violence following HIV status disclosure, and health service responses: narratives of women attending reproductive health services in Kenya. J Int AIDS Soc, 19(1), p 20766. doi:10.7448/IAS.19.1.20766 Retrieved from 10.7448/IAS.19.1.20766https://www.ncbi.nlm.nih.gov/pubmed/27037140 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/27037140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deribe K, Woldemichael K, Wondafrash M, Haile A, & Amberbir A (2008). Disclosure experience and associated factors among HIV positive men and women clinical service users in Southwest Ethiopia. BMC Public Health, 8, p 81. doi:10.1186/1471-2458-8-81 Retrieved from 10.1186/1471-2458-8-81https://www.ncbi.nlm.nih.gov/pubmed/18312653 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/18312653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hampanda KM, & Rael CT (2018). HIV Status Disclosure Among Postpartum Women in Zambia with Varied Intimate Partner Violence Experiences. AIDS Behav, 22(5), pp. 1652–1661. doi: 10.1007/s10461-017-1909-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform, 42(2), pp. 377–381. doi:10.1016/j.jbi.2008.08.010 Retrieved from 10.1016/j.jbi.2008.08.010https://www.ncbi.nlm.nih.gov/pubmed/18929686 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/18929686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health K. M. o. (2016). Guidelines on Use of Antiretroviral Drugs for Treating and Preventing HIV Infection in Kenya. Nairobi, Kenya. [Google Scholar]
- Hodgson I, Plummer ML, Konopka SN, Colvin CJ, Jonas E, Albertini J,… Fogg KP (2014). A systematic review of individual and contextual factors affecting ART initiation, adherence, and retention for HIV-infected pregnant and postpartum women. PLoS One, 9(11), p e111421. doi:10.1371/journal.pone.0111421 Retrieved from 10.1371/journal.pone.0111421https://www.ncbi.nlm.nih.gov/pubmed/25372479 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/25372479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- International Planned Parenthood Federation, G. N. o. P. L. w. H. A., International Community of Women Living with HIV and Joint United Nations Programme on HIV/AIDS. (2008). People Living with HIV Stigma Index: An index to measure the stigma and discrimination experienced by people living with HIV – questionnaire.: Retrieved from http://www.stigmaindex.org/. [Google Scholar]
- Jasseron C, Mandelbrot L, Dollfus C, Trocme N, Tubiana R, Teglas JP,… Warszawski J (2013). Non-disclosure of a pregnant woman’s HIV status to her partner is associated with non-optimal prevention of mother-to-child transmission. AIDS Behav, 17(2), pp. 488–497. doi:10.1007/s10461-011-0084-y Retrieved from 10.1007/s10461-011-0084-yhttps://www.ncbi.nlm.nih.gov/pubmed/22130651 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22130651 [DOI] [PubMed] [Google Scholar]
- Kennedy CE, Haberlen S, Amin A, Baggaley R, & Narasimhan M (2015). Safer disclosure of HIV serostatus for women living with HIV who experience or fear violence: a systematic review. J Int AIDS Soc, 18(Suppl 5), p 20292. doi: 10.7448/ias.18.6.20292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenya National Bureau of Statistics, Ministry of Health/Kenya, National AIDS Control Council/Kenya, Kenya Medical Research Institute, National Council for Population and Development/Kenya, a., & ICF International. (2015). Kenya Demographic and Health Survey 2014. Rockville, MD, USA [Google Scholar]
- Kinuthia J, Singa B, McGrath CJ, Odeny B, Langat A, Katana A,… John-Stewart G (2018). Prevalence and correlates of non-disclosure of maternal HIV status to male partners: a national survey in Kenya. BMC Public Health, 18(1), p 671. doi:10.1186/s12889-018-5567-6 Retrieved from 10.1186/s12889-018-5567-6https://www.ncbi.nlm.nih.gov/pubmed/29848345 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/29848345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiweewa FM, Bakaki PM, McConnell MS, Musisi M, Namirembe C, Nakayiwa F,… Fowler MG (2015). A cross-sectional study of the magnitude, barriers, and outcomes of HIV status disclosure among women participating in a perinatal HIV transmission study, “the Nevirapine Repeat Pregnancy study”. BMC Public Health, 15, p 988. doi: 10.1186/s12889-015-2345-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, & Mokdad AH (2009). The PHQ-8 as a measure of current depression in the general population. J Affect Disord, 114(1–3), pp. 163–173. doi:10.1016/j.jad.2008.06.026 Retrieved from 10.1016/j.jad.2008.06.026https://www.ncbi.nlm.nih.gov/pubmed/18752852 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/18752852 [DOI] [PubMed] [Google Scholar]
- Maeri I, El Ayadi A, Getahun M, Charlebois E, Akatukwasa C, Tumwebaze D,… Camlin CS (2016). “How can I tell?” Consequences of HIV status disclosure among couples in eastern African communities in the context of an ongoing HIV “test-and-treat” trial. AIDS Care, 28 Suppl 3, pp. 59–66. doi: 10.1080/09540121.2016.1168917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGrath CJ, Singa B, Langat A, Kinuthia J, Ronen K, Omolo D,… John-Stewart GC (2018). Non-disclosure to male partners and incomplete PMTCT regimens associated with higher risk of mother-to-child HIV transmission: a national survey in Kenya. AIDS Care, 30(6), pp. 765–773. doi:10.1080/09540121.2017.1400642 Retrieved from 10.1080/09540121.2017.1400642https://www.ncbi.nlm.nih.gov/pubmed/29130333 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/29130333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medley A, Garcia-Moreno C, McGill S, & Maman S (2004). Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ, 82(4), pp. 299–307. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/15259260 [PMC free article] [PubMed] [Google Scholar]
- Monahan PO, Shacham E, Reece M, Kroenke K, Ong’or WO, Omollo O,… Ojwang C (2009). Validity/reliability of PHQ-9 and PHQ-2 depression scales among adults living with HIV/AIDS in western Kenya. J Gen Intern Med, 24(2), pp. 189–197. doi:10.1007/s11606-008-0846-z Retrieved from 10.1007/s11606-008-0846-zhttps://www.ncbi.nlm.nih.gov/pubmed/19031037 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/19031037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhindo R, Nakalega A, & Nankumbi J (2015). Predictors of couple HIV counseling and testing among adult residents of Bukomero sub-county, Kiboga district, rural Uganda. BMC Public Health, 15, p 1171. doi:10.1186/s12889-015-2526-3 Retrieved from 10.1186/s12889-015-2526-3https://www.ncbi.nlm.nih.gov/pubmed/26603280 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/26603280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Musheke M, Bond V, & Merten S (2013). Couple experiences of provider-initiated couple HIV testing in an antenatal clinic in Lusaka, Zambia: lessons for policy and practice. BMC Health Serv Res, 13, p 97. doi:10.1186/1472-6963-13-97 Retrieved from 10.1186/1472-6963-13-97https://www.ncbi.nlm.nih.gov/pubmed/23496926 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/23496926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myer L, Iyun V, Zerbe A, Phillips TK, Brittain K, Mukonda E,… Abrams EJ (2017). Differentiated models of care for postpartum women on antiretroviral therapy in Cape Town, South Africa: a cohort study. J Int AIDS Soc, 20(Suppl 4), p 21636. doi:10.7448/IAS.20.5.21636 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/2877059310.7448/IAS.20.5.21636https://www.ncbi.nlm.nih.gov/pubmed/28770593https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5577773/pdf/zias-20-1324104.pdf Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/28770593 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5577773/pdf/zias-20-1324104.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naigino R, Makumbi F, Mukose A, Buregyeya E, Arinaitwe J, Musinguzi J, & Wanyenze RK (2017). HIV status disclosure and associated outcomes among pregnant women enrolled in antiretroviral therapy in Uganda: a mixed methods study. Reprod Health, 14(1), p 107. doi:10.1186/s12978-017-0367-5 Retrieved from 10.1186/s12978-017-0367-5https://www.ncbi.nlm.nih.gov/pubmed/28854944 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/28854944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odeny TA, Onono M, Owuor K, Helova A, Wanga I, Bukusi EA,… Abuogi LL (2018). Maximizing adherence and retention for women living with HIV and their infants in Kenya (MOTIVATE! study): study protocol for a randomized controlled trial. Trials, 19(1), p 77. doi:10.1186/s13063-018-2464-3 Retrieved from 10.1186/s13063-018-2464-3https://www.ncbi.nlm.nih.gov/pubmed/29378622 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/29378622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odiachi A, Erekaha S, Cornelius LJ, Isah C, Ramadhani HO, Rapoport L, & Sam-Agudu NA (2018). HIV status disclosure to male partners among rural Nigerian women along the prevention of mother-to-child transmission of HIV cascade: a mixed methods study. Reprod Health, 15(1), p 36. doi:10.1186/s12978-018-0474-y Retrieved from 10.1186/s12978-018-0474-yhttps://www.ncbi.nlm.nih.gov/pubmed/29499704 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/29499704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Onono MA, Cohen CR, Jerop M, Bukusi EA, & Turan JM (2014). HIV serostatus and disclosure: implications for infant feeding practice in rural south Nyanza, Kenya. BMC Public Health, 14, p 390. doi:10.1186/1471-2458-14-390 Retrieved from 10.1186/1471-2458-14-390https://www.ncbi.nlm.nih.gov/pubmed/24754975 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/24754975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg NE, Gross R, Mtande T, Maman S, Golin CE, Saidi F,… Miller WC (2017). “We have heard it together”: a qualitative analysis of couple HIV testing and counselling recruitment in Malawi’s Option B+ programme. Afr J AIDS Res, 16(3), pp. 215–223. doi:10.2989/16085906.2017.1362017 Retrieved from 10.2989/16085906.2017.1362017https://www.ncbi.nlm.nih.gov/pubmed/28978289 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/28978289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg NE, Mtande TK, Saidi F, Stanley C, Jere E, Paile L,… Hosseinipour M (2015). Recruiting male partners for couple HIV testing and counselling in Malawi’s option B+ programme: an unblinded randomised controlled trial. Lancet HIV, 2(11), pp. e483–491. doi:10.1016/S2352-3018(15)00182-4 Retrieved from 10.1016/S2352-3018(15)00182-4https://www.ncbi.nlm.nih.gov/pubmed/26520928 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/26520928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusbult C, Martz J, & Agnew C (1998). The Investment Model Scale: Measuring commitment level, satisfaction level, quality of alternatives, and investment size. [Article]. Personal Relationships, 5(4), pp. 357–391. doi: 10.1111/j.1475-6811.1998.tb00177.x [DOI] [Google Scholar]
- Schuster TL, Kessler RC, & Aseltine RH Jr. (1990). Supportive interactions, negative interactions, and depressed mood. Am J Community Psychol, 18(3), pp. 423–438. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/2264558 [DOI] [PubMed] [Google Scholar]
- Shamu S, Zarowsky C, Shefer T, Temmerman M, & Abrahams N (2014). Intimate partner violence after disclosure of HIV test results among pregnant women in Harare, Zimbabwe. PLoS One, 9(10), p e109447. doi:10.1371/journal.pone.0109447 Retrieved from 10.1371/journal.pone.0109447http://www.ncbi.nlm.nih.gov/pubmed/25350001 Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/25350001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siedner MJ, Tsai AC, Dworkin S, Mukiibi NF, Emenyonu NI, Hunt PW,… Weiser SD (2012). Sexual relationship power and malnutrition among HIV-positive women in rural Uganda. AIDS Behav, 16(6), pp. 1542–1548. doi: 10.1007/s10461-012-0162-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spangler SA, Abuogi LL, Akama E, Bukusi EA, Helova A, Musoke P,… Turan JM (2018). From ‘half-dead’ to being ‘free’: resistance to HIV stigma, self-disclosure and support for PMTCT/HIV care among couples living with HIV in Kenya. Cult Health Sex, 20(5), pp. 489–503. doi:10.1080/13691058.2017.1359338 Retrieved from 10.1080/13691058.2017.1359338https://www.ncbi.nlm.nih.gov/pubmed/28812457 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/28812457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan JM, Bukusi EA, Onono M, Holzemer WL, Miller S, & Cohen CR (2011). HIV/AIDS Stigma and Refusal of HIV Testing Among Pregnant Women in Rural Kenya: Results from the MAMAS Study. AIDS Behav, 15(6), pp. 1111–1120. Retrieved from http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=20827573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turan JM, Darbes LA, Musoke PL, Kwena Z, Rogers AJ, Hatcher AM,… Bukusi EA (2018). Development and Piloting of a Home-Based Couples Intervention During Pregnancy and Postpartum in Southwestern Kenya. AIDS patient care and STDs, 32(3), pp. 92–103. doi:10.1089/apc.2017.0285 Retrieved from 10.1089/apc.2017.0285https://www.ncbi.nlm.nih.gov/pubmed/29620927 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/29620927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner RJ, Frankel BG, & Levin DM (1983). Social support: Conceptualization, measurement, and implications for mental health.. Research in Community & Mental Health, 3, pp. 67–111. [Google Scholar]
- UNAIDS. (2012). Regional Fact Sheet 2012: Sub-Saharan Africa.. Geneva, Switzerland: UNAIDS; Retrieved from http://files.unaids.org/en/media/unaids/contentassets/documents/epidemiology/2012/gr2012/2012_FS_regional_ssa_en.pdf. [Google Scholar]
- Weiser SD, Heisler M, Leiter K, Percy-de Korte F, Tlou S, DeMonner S,… Iacopino V (2006). Routine HIV testing in Botswana: a population-based study on attitudes, practices, and human rights concerns. PLoS Med, 3(7), p e261. doi:10.1371/journal.pmed.0030261 Retrieved from 10.1371/journal.pmed.0030261https://www.ncbi.nlm.nih.gov/pubmed/16834458 Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/16834458 [DOI] [PMC free article] [PubMed] [Google Scholar]