Abstract
Chronic osteomyelitis can be difficult to diagnose given its similar radiographic appearance to other lesions. This case report describes a 48-year-old woman, who presented with left thigh pain and on radiography a large disorganized sclerotic lesion involving nearly the entire femoral diaphysis, concerning for Paget disease or malignancy. Biopsy suggested chronic osteomyelitis but did not identify a causative organism. Treatment with antibiotics led to resolution of pain and improvement of biochemical markers. This case exemplifies the role of radiographic imaging in the diagnosis of chronic osteomyelitis and the possible utility of antibiotics for culture-negative chronic osteomyelitis. We review imaging modalities for the diagnosis of chronic osteomyelitis and Paget disease.
Keywords: Chronic osteomyelitis, Paget disease of bone, Bone infection, Metabolic bone disease
Introduction
Chronic osteomyelitis is most commonly seen among adults whereas acute osteomyelitis most often affects children. Chronic osteomyelitis is associated with vascular and immune-compromising conditions, such as peripheral vascular disease and diabetes mellitus. Chronically infected ulcers eventually migrate from the soft tissue to the underlying bone. Moreover, traumatic insult to a bone can introduce a nidus for infection which can persist and gradually weaken the bone. On imaging, chronic osteomyelitis presents with features of osteonecrosis including cortical destruction, osteosclerosis, and eventually periosteal thickening. Radiographical diagnosis of chronic osteomyelitis can be complicated by similarly presenting lesions such as Paget disease of the bone. Paget disease of the bone presents as coarsened trabeculae and bony enlargement. The pathophysiology of Paget disease is characterized by 3 distinct phases of excessive bone remodeling. The first phase is dominated by osteoclast activation and osteolytic bone destruction; the second phase involves mixed osteoclast and osteoblast activation. In the final phase, osteoblastic activity predominates and leads to the formation of new bone. Paget disease of the bone is a common condition affecting between 2%-8% of the population, almost exclusively affecting those over the age of 45.
We present the case of a femoral lesion with striking radiographic findings. This lesion led to an extensive differential diagnosis and workup. This case highlights important radiographic distinctions between similarly presenting conditions—chronic osteomyelitis and Paget disease of the bone. Given the nature of these 2 conditions, this case report has widespread applicability in radiology, endocrinology, infectious diseases, and orthopedics.
Case presentation
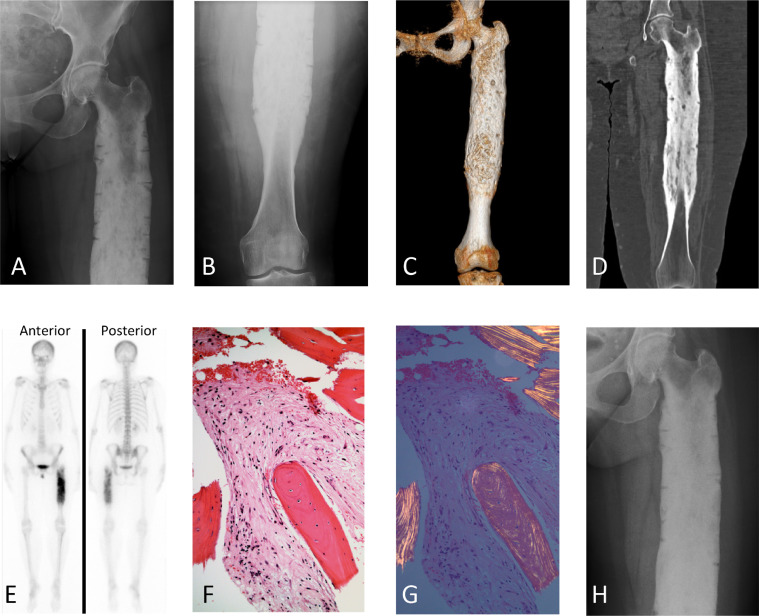
A 48-year-old Bosnian woman with no significant past medical history is referred for “possible Paget disease”. Seven years prior to this presentation, she underwent a lumbar laminectomy for back pain. Soon after, the pain spread to her left thigh. She was diagnosed with sciatica and required increasing doses of oxycodone for the last 7 years. When the pain became unbearable, she sought a second opinion. During this work-up, lower extremity radiography showed an unusual lesion concerning for Paget disease or a malignant bone tumor due to the extensive trabecular disorganization and sclerosis. At our institution, repeat x-rays showed that the lesion involved the entire diaphysis (Fig. 1, Panel A, B, C, D). There were innumerable well-defined defects resembling chronic incomplete intracortical fractures. Conspicuously, the epiphyses and metaphyses were spared (Fig. 1, Panels A, B, C, D). A full body bone scan revealed intense radiotracer uptake along the proximal 2/3 of the left femur without involvement of the femoral head or neck (Fig. 1, Panel E). Despite the widespread involvement of the femur, there was no evidence of active infection.
Fig. 1.
On presentation, radiography (1A, 1B) showed involvement of the femoral diaphysis with sparing of the femoral head, neck and distal femur. 3D CT reconstruction (1C) demonstrated trabecular disorganization, sclerosis, and multifocal areas of complete obliteration the medullary space. Involvement begins in the intertrochanteric region just proximal to the level of the lesser tuberosity and extends to the distal diaphysis 10 cm proximal to the medial knee joint line. Again, sparing of the femoral head and distal femur is observed. Multiplanar reconstruction (MPR) CT (1D) showed a halo of soft tissue density surrounding the midshaft femur, elevating adjacent musculature by about 1 cm. Bone scintigraphy (1E) showed that technetium-99m–labeled bisphosphonates were strongly up taken in the femoral lesion, consistent with elevated bone remodeling and increased blood flow. On H & E stain (1F), the hallmark histologic features of chronic osteomyelitis are evident: marrow fibrosis, scattered chronic inflammatory cells, and rebuttressing of lamellar bone with woven bone, notably lacking abnormal osteoclasts characteristic of Paget. Under polarized light (1G), the bone in the periphery of the field shows collagen that is arranged in parallel fashion, consistent with lamellar bone. Alternatively, the bone that is in the middle of the field, surrounded by fibrotic marrow, has collagen that is arranged in a more haphazard fashion, demonstrating pathologic woven bone. On yearly follow up radiography (1H), the femoral lesion has not progressed. Cortical thickening and fracture lines remain.
Relevant laboratory studies displayed increased inflammatory markers and markers of bone turnover (Table 1). Operative exploration was pursued to establish a diagnosis. Proximal femur intraosseous curettage and biopsy revealed cancellous lamellar bone, inflammatory cells, and fibrosis, most consistent with chronic osteomyelitis (Fig. 1, Panel F and G). Cultures and stains were negative, and the microbiology report showed 2+ polymorphonuclear cells and no microbial organisms. Due to a history of psoriasis with open sores (previously on methotrexate), we postulated that this may have been the route of infection. Additionally, she described a fungal infection of her fingernails/toenails about 7 years ago, and thus chronic Candida was also considered despite fungal cultures also being negative. Vancomycin 1g I.V. q12 hours and Ciprofloxacin 250mg P.O. q12 hours were started for 6 weeks. Inflammatory markers immediately decreased, while markers of bone turnover remained elevated (Table 1). She received 3 cycles of zoledronic acid due to the intracortical fractures and elevated markers of bone turnover.
Table 1.
Laboratory data.
| Initial | After antibiotics | 4 years follow-up | |
|---|---|---|---|
| Ca2+ (8.4-10.5 mg/dL) | 10.0 | 10.0 | 9.7 |
| Bone specific alkaline phosphatase | |||
| (Post menopausal: 7.0-22.4 mcg/L) | 29.9 | – | 10.4 |
| Urine N-telopeptide | |||
| (Postmenopausal: 26-124 nM BCE/mM) | 144 | 133 | 38 |
| Vitamin D total (25-80 ng/mL) | 42 | 32 | 34 |
| WBC (3.9–10.7 × 103 /mcL) | 8.4 | 8.2 | – |
| ESR (0-20 mm/hr) | 92 | 59 | 58 |
| CRP (0-5 mg/L) | 138.8 | 19.5 | 25.7 |
After 4 years of follow-up, she is still using a walker but is independent. She is off all antibiotics, and she is no longer dependent on NSAIDs or opioids for pain control. Inflammatory markers have plateaued above the reference range, and markers of bone turnover are within normal limits (Table 1). Imaging has been repeated yearly and has shown no progression of the bone destruction (Fig. 1, Panel H). Circumferential cortical thickening remains, and incomplete cortical fracture lines are unchanged.
Discussion
The patient was initially referred for suspected Paget disease, due to cortical thickening and sclerosis seen on imaging as well as elevated markers of bone turnover, alkaline phosphatase and urinary N-telopeptide. Based on the radiographic findings, the differential diagnosis included lymphoma, Paget disease of the bone, malignant bone tumors, radiation osteitis (she lived near Chernobyl in the 1980’s), and chronic osteomyelitis. Paget disease of the bone has a higher prevalence in the general population than chronic osteomyelitis, especially when a previous infection or trauma cannot be identified. Several aspects of this patient's case were inconsistent with Paget. Notably, the femur's epiphyses and metaphyses were unaffected, whereas these are the first regions affected by Paget [1,2]. The isolated involvement of the femoral diaphysis is particularly intriguing. Of the long bones, only the tibia is known to have isolated diaphyseal involvement in Paget with sparing of the epiphyses. Diagnoses that present with only diaphyseal involvement and similar radiographic appearances include Ribbings disease and Engelmann-Camurati [3]. This patient's age and clinical history do not support these diagnoses. Serum markers of bone turnover were elevated, but these tests are neither specific nor diagnostic for Paget disease [4]. Given the isolated location in the femur, this case would be classified as monostotic, representing a minority of Paget cases. Seventy percent of cases of Paget disease involve multiple bones, usually long bones, the axial skeleton, or the skull [5]. Based upon the suspicion of Paget disease, there was concern that this large painful lesion represented a malignant bone tumor from the transformation of Paget into osteosarcoma. Neoplastic transformation is a well-documented complication of Paget, occurring in 0.5% of Paget’s cases [2,6]. Most often, Paget disease transforms into osteosarcoma, but less commonly fibrosarcoma, chondrosarcoma, and lymphoma are also encountered [2]. A bone biopsy was sought to identify the lesion and establish a diagnosis to guide further treatment. Histopathologic description of the femur biopsy was inconsistent with that of Paget disease, which typically presents as irregular cement lines and a mosaic pattern of lamellar bone with abnormal osteoclast morphology [5]. Instead, the histopathology showed chronic inflammation and fibrosis more consistent with chronic osteomyelitis (Panels F and G). The biopsy samples, however, lacked osteonecrosis and extensive buttressing of bone which are features of chronic osteomyelitis. The combination of radiographic evidence, histopathologic features of chronic osteomyelitis, and clinical response to antibiotics led to confidence in chronic osteomyelitis as the diagnosis.
Chronic osteomyelitis is distinct from acute osteomyelitis in its clinical course and treatment. The microbial pathogens responsible for acute and chronic osteomyelitis are largely the same. Common causative organisms for osteomyelitis include Staphylococcus and Streptococcus species, most often Staphylococcus aureus. Acute osteomyelitis often develops from hematogenous spread or after a traumatic insult to a bone which introduced a microbial inoculum [7,8]. Chronic osteomyelitis can develop from similar causes as acute osteomyelitis, but is often caused by spread from local soft tissue as is the case of diabetic ulcers progressing into bone infections. Chronic osteomyelitis represents a sequestered region of bone often coated with bacterial biofilm that is impervious to antibiotics [9]. Therefore, chronic osteomyelitis often requires operative debridement and extended courses of intravenous antibiotics, whereas acute osteomyelitis generally resolves with antibiotics alone.
That said, the treatment paradigm for chronic osteomyelitis is poorly researched [10]. Antibiotic choice is guided by microbial culture results. There is a known subset of patients for whom bone specimens do not lead to the identification of a culpable microbe [11]. In these cases, previous inoculation with an infectious organism likely triggered an inflammatory milieu which continued as low-grade chronic inflammation causing progressive destruction of the bone parenchyma. Culture-negative cases are more likely to be insidious, without typical infectious symptoms such as fevers [12]. Though no infectious organism was identified in this case, broad-spectrum antibiotics were initiated and led to a decrease of inflammatory markers and symptomatic improvement for the patient. This case emphasizes a possible role for empiric antibiotics in cases of culture-negative chronic osteomyelitis.
Imaging of osteomyelitis relies on a number of modalities. Plain radiographs lack sensitivity and specificity for detecting osteomyelitis, but can show large lesions as demonstrated in this case [8]. While small lesions may be missed by plain radiographs, this is still the recommended initial imaging for suspected osteomyelitis. MRI is the preferred imaging modality for osteomyelitis when feasible. Use of T1 and T2-weighted MRI sequences allows visualization of soft tissue changes and fluid elements of the bone [13]. Moreover, in cases of chronic infection, MRI has unique utility in assessing the relative activity of the infection by visualizing water content of bone marrow, which is the first detectable sign of osteomyelitis [8]. Bone scintigraphy with technetium-99m–labeled bisphosphonates allows detection of increased blood flow due to the presence of infection-induced hypervascularity. CT imaging is unable to visualize bone marrow edema, decreasing its usefulness for imaging of osteomyelitis. Due to the initial suspicion for Paget disease in this case, CT imaging and reconstruction was used to assess trabecular disorganization, osseous expansion, and possible fractures. MRI lacks specificity for Paget disease due to the phasic nature of the disease. Different MRI signals can be seen based whether the bone is in an osteolytic or osteoblastic phase of Paget disease [2,14]. Similarly, bone scintigraphy is nonspecific for Paget disease with radionucleotide uptake occurring in all 3 phases of the disease [2]. In malignant transformation of Paget disease, both CT and MRI can provide value to the diagnosis. Neoplastic transformation appears as osteolytic cortical destruction and a soft tissue mass, generally without osteosclerosis [2]. These complicated diagnoses require a combination of imaging modalities to differentiate their radiographic features and establish a diagnosis.
Conclusion
We present a case of chronic osteomyelitis after initial suspicion of Paget disease or malignant transformation. We discuss the pathogenesis of chronic osteomyelitis, and imaging methods for differentiating Paget disease of the bone and chronic osteomyelitis. To fully characterize a lesion and establish a diagnosis, the combination of plain radiographs, MRI, CT, and bone scintigraphy is warranted.
Compliance with Ethical Standards
Consent for publication obtained from the patient.
Footnotes
Funding: Two of the authors (SR and JMC) are supported by NIGMS of the National Institutes of Health under award number T32GM007347. The content in this report is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declaration of Competing Interest: The authors declare no conflicts of interest.
Contributor Information
Seth A. Reasoner, Email: seth.a.reasoner@vanderbilt.edu.
Juan M. Colazo, Email: juan.m.colazo@vanderbilt.edu.
Kathryn M. Dahir, Email: kathryn.dahir@vumc.org.
References
- 1.Nebot Valenzuela E, Pietschmann P. Epidemiology and pathology of Paget disease of bone – a review. Wiener Medizinische Wochenschrift. 2017;167(1–2):2–8. doi: 10.1007/s10354-016-0496-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Theodorou DJ, Theodorou SJ, Kakitsubata Y. Imaging of Paget disease of bone and its musculoskeletal complications: review. Am J Roentgenol. 2011;196:64–75. doi: 10.2214/AJR.10.7222. [DOI] [PubMed] [Google Scholar]
- 3.Damle NA, Patnecha M, Kumar P, Gadodia A, Subbarao K, Bal C. Ribbing disease: uncommon cause of a common symptom. Indian J Nucl Med. 2011;26(1):36–39. doi: 10.4103/0972-3919.84612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al Nofal AA, Altayar O, BenKhadra K, Qasim Agha OQ, Asi N, Nabhan M. Bone turnover markers in Paget disease of the bone: a systematic review and meta-analysis. Osteoporos Int. 2015;26(7):1875–1891. doi: 10.1007/s00198-015-3095-0. [DOI] [PubMed] [Google Scholar]
- 5.Shaker JL. Paget disease of bone: a review of epidemiology, pathophysiology and management. Ther Adv Musculoskelet Dis. 2009;1(2):107–125. doi: 10.1177/1759720X09351779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ralston SH. Paget disease of bone. N Engl J Med. 2013;368(7):644–650. doi: 10.1056/NEJMcp1204713. [DOI] [PubMed] [Google Scholar]
- 7.Fritz JM, McDonald JR. Osteomyelitis: approach to diagnosis and treatment. Phys Sportsmed. 2008;36(1):50–54. doi: 10.3810/psm.2008.12.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee YJ, Sadigh S, Mankad K, Kapse N, Rajeswaran G. The imaging of osteomyelitis. Quant Imaging Med Surg. 2016;6(2):184–198. doi: 10.21037/qims.2016.04.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kanakaris NK, Giannoudis PV. Chronic osteomyelitis. Trauma Orthop Classif A Compr Overv. 2015:511–514. [Google Scholar]
- 10.Cortés-Penfield NW, Kulkarni PA. The history of antibiotic treatment of osteomyelitis. Open Forum Infect Dis. 2019;6(5):1–7. doi: 10.1093/ofid/ofz181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zuluaga AF. Etiologic diagnosis of chronic osteomyelitis. Arch Intern Med. 2006;166(1):95. doi: 10.1001/archinte.166.1.95. [DOI] [PubMed] [Google Scholar]
- 12.Floyed RL, Steele RW. Culture-negative osteomyelitis. Pediatr Infect Dis. 2003;22(8):731–735. doi: 10.1097/01.inf.0000078901.26909.cf. [DOI] [PubMed] [Google Scholar]
- 13.Pineda C, Espinosa R, Pena A. Radiographic imaging in osteomyelitis: the role of plain radiography, computed tomography, ultrasonography, magnetic resonance imaging, and scintigraphy. Semin Plast Surg. 2009;23(02):080–089. doi: 10.1055/s-0029-1214160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith SE, Murphey MD, Motamedi K, Mulligan ME, Resnik CS, Gannon FH. Radiologic spectrum of paget disease of bone and its complications with pathologic correlation. Radiographics. 2002;22(5):1191–1216. doi: 10.1148/radiographics.22.5.g02se281191. [DOI] [PubMed] [Google Scholar]