Abstract
Epidural lipomatosis with associated syrinx formation is an exceedingly rare clinical entity. In this case report we present a 48-year old female who initially presented with symptoms of progressive myelopathy and later developed urinary incontinence. Her imaging studies showed upper thoracic epidural lipomatosis and associated spinal stenosis, cord compression and a mildly expansile right paracentral syrinx at C7-T1. She underwent a decompression surgery which provided her with partial symptomatic relief. On MRI, there was a mild decrease in the size of syrinx and some improvement in the degree of spinal stenosis. However, the subsequent clinical improvement supported the possibility that spinal compression caused by epidural lipomatosis could have resulted in syrinx formation. Therefore, such cases can be appropriately treated with spinal decompression surgeries or syrinx shunting procedures.
Keywords: Case report, Epidural lipomatosis, Syrinx
Introduction
Epidural lipomatosis is a rare condition where excessive adipose tissue deposits around the thecal sac within the spinal canal [1]. The hypertrophy of epidural adipose tissue may result in compression of the spinal cord and nerve roots producing neurologic symptoms like back pain, lower extremity weakness, sensory changes and, in extreme scenarios, bowel and bladder incontinence [2]. The imaging modality of choice for epidural lipomatosis is MRI. Epidural adipose tissue that has a thickness greater than 7 mm has been reported to be the diagnostic criterion for epidural lipomatosis [3], [4]. In the past, only 3 cases have been reported in the literature of epidural lipomatosis associated with a syrinx, all of which were managed by decompression surgery like laminectomy, laminoplasty or laminotomy. This resulted in clinical improvement and radiological resolution of the syrinx, thereby supporting the hypothesis that spinal stenosis caused by epidural lipomatosis can result in syrinx formation. We report a similar case of thoracic epidural lipomatosis and spinal stenosis with associated syrinx formation and infer the treatment outcomes of the patient in terms of clinical improvement and radiologic resolution of the syrinx.
Case report
A 48-year-old female presented with bilateral lower extremity numbness and paralysis which was associated with prolonged sitting that resolved once she changed position. She also reported numbness of her right hand. For the prior 1-2 months, she had been experiencing urinary incontinence at night. She had a complex medical history of juvenile type 1 DM, hypothyroidism and was on dialysis for 2 years. Later she got a pancreas and kidney transplant which resolved her hypertension and DM. Her BMI at presentation was 28 kg/m2. She had no history of long term steroid use. The patient then underwent MRI C-spine and T-spine without contrast.
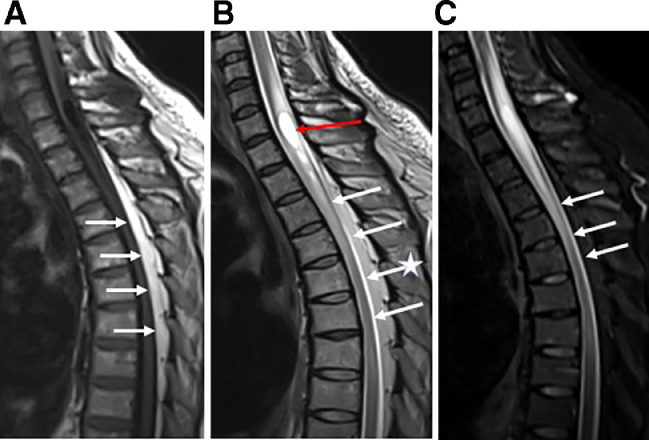
The MRI studies showed marked upper thoracic dorsal epidural lipomatosis, measuring up to 1 cm thickness. This was associated with marked central spinal stenosis and cord compression most pronounced at the T4 level, and at least moderate degree at the T3, T5, and T6 levels. There was associated cord edema extending from C5 through the lower T4 level and a mildly expansile right paracentral syrinx at the C7-T1 levels measuring 1.8 cm craniocaudal and 0.6 cm in diameter. There was no associated abnormal enhancing spinal canal mass. Given her progressive myelopathy, she underwent spinal decompression by thoracic laminotomy with T2-T7 laminoplasty (Fig. 1).
Fig. 1.
(A) T1-weighted sagittal MRI image of the Spine showing area of hyperintensity in the upper thoracic dorsal epidural space (arrows) indicating epidural lipomatosis. (B) T2-weighted sagittal MRI image of the Spine showing marked central spinal stenosis and cord compression (white arrows) most pronounced at the T4 level (star). Also, syrinx (red arrow) is visualised as an area of paracentral hyperintensity in the cord at the level of C7-T1. (C) STIR sagittal MRI image of showing the spinal stenosis and cord compression (white arrows). (Color version of figure is available online.)
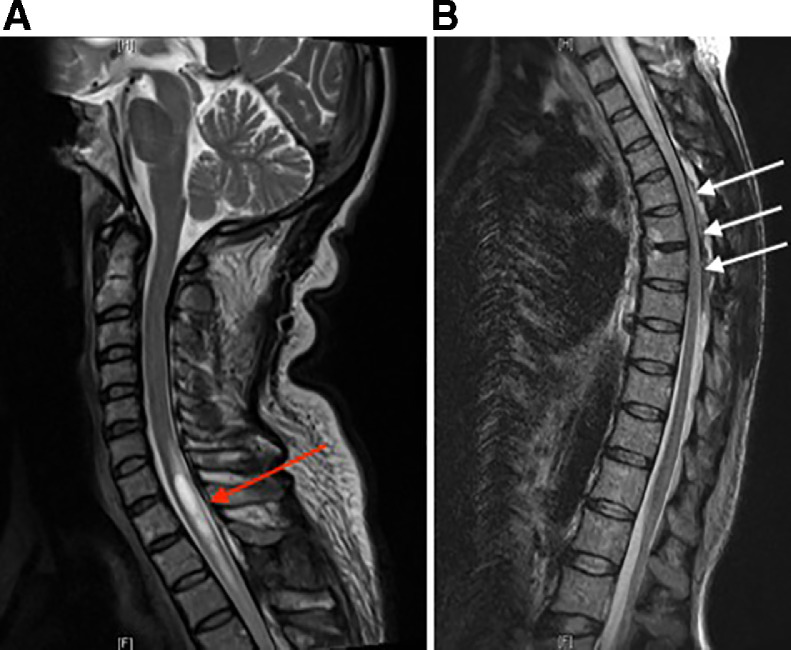
Postprocedure she experienced some clinical relief with near resolution of bladder incontinence. However, she continued experiencing numbness over her bilateral lower extremities and her right hand and continued to experience back pain requiring pain management. Her follow up MRI scans showed mild radiologic resolution of the syrinx. The most recent MR C-spine and T-spine at 18 months post-laminoplasty showed a mild decrease in the size of the cervicothoracic syrinx extending from C2-T2 and some improvement in spinal stenosis with at least moderate residual central spinal stenosis from T3 through T7. There was similar cord T2 hyperintensity extending from C6-T7 likely indicating residual cord edema and/or myelomalacia (Fig. 2).
Fig. 2.
(A) T2-weighted sagittal MRI image of C-Spine showing mildly decreased size of the syrinx (red arrow) post-laminoplasty. (B) T2-weighted sagittal MRI image of T-spine showing unchanged mild to moderate central spinal stenosis (white arrows) T3-T7. (Color version of figure is available online.)
Currently, she is receiving annual follow up MRI imaging and being managed symptomatically for her back pain without any progression of her symptoms so far.
Discussion
Epidural Lipomatosis is a condition characterized by an excess of epidural fat tissue most commonly within the thoracic and lumbar spine. The most common cause of spinal epidural lipomatosis is long term use of exogenous steroids [2], however, several studies have reported an association with morbid obesity [5] and Cushing's syndrome [6], [7]. However, a few cases have also been reported not associated with any of the above conditions. The symptomatology of epidural lipomatosis is varied. Back pain is the most common and earliest symptom. Later, with disease progression the patient may present with other symptoms depending upon the spinal level of involvement. Epidural lipomatosis at the thoracic level produces myelopathic effects such as lower extremity weakness whereas lumbar involvement causes radicular effects. Since, the majority of these patients present with thoracic epidural lipomatosis and, therefore, progressive myelopathy is a more common presentation [2]. However, some cases maybe asymptomatic and detected incidentally [8]. Our case presentation of epidural lipomatosis with associated syrinx formation is relatively rare as only 3 prior cases with such an association have been reported in the literature.
It has been theorized that mechanical spinal compression is the likely mechanism of syrinx formation in the setting of epidural lipomatosis [9]. The principle management for these cases is divided into 2 groups [8]. First is conservative/symptomatic management consisting of follow up and treating the underlying cause of lipomatosis. Second is surgical management which is done in cases where conservative management fails. Surgical management includes decompression surgeries like laminectomy, laminoplasty, and laminotomy. In cases of progressive myelopathy, such as this case, surgical treatment is often performed prior to conservative therapy to decrease the chance of irreversible injury [10].
In all previously reported cases of epidural lipomatosis with syrinx, decompression surgery resulted in significant clinical improvement as well as near-complete radiologic resolution of the syrinx, which is theoretically due to decompression of the spinal canal and restoration of the normal CSF flow [11]. The clinical outcome in our case is somewhat unique with only partial improvement in the clinical symptoms and a relatively mild decrease in size of the syrinx following surgical decompression. In such case scenarios, when the surgery is either unsuccessful or cannot be performed, syrinx shunting procedures or syringostomy could prove beneficial [11].
References
- 1.Fessler R.G., Johnson D.L., Brown F.D., Erickson R.K., Reid S.A., Kranzler L. Epidural lipomatosis in steroid-treated patients. Spine. 1992;17:183–188. doi: 10.1097/00007632-199202000-00011. [DOI] [PubMed] [Google Scholar]
- 2.Fassett Daniel R., H Meic. Schmidt Spinal epidural lipomatosis: a review of its causes and recommendations for treatment. Neurosurg Focus. 2004;16(4) [PubMed] [Google Scholar]
- 3.Kumar K, Nath RK, Nair CP. Symptomatic epidural lipomatosis secondary to obesity. Case report. J Neurosurg. 1996;85:348–350. doi: 10.3171/jns.1996.85.2.0348. [DOI] [PubMed] [Google Scholar]
- 4.Robertson SC, Traynelis VC, Follett KA. Idiopathic spinal epidural lipomatosis. Neurosurgery. 1997;41:68–75. doi: 10.1097/00006123-199707000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Badami J., Hinck V. Symptomatic deposition of epidural fat in a morbidly obese woman. AJNR. 1982;3:664–665. [PMC free article] [PubMed] [Google Scholar]
- 6.Chapman P.H., Mortuza R.L., Poletti C.E., Darchmer A.W. Symptomatic spinal epidural lipomatosis associated with Cushing's syndrome. Neurosurgery. 1981;8:724–727. doi: 10.1227/00006123-198106000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Lipson S.J., Naheedy M.H., Kaplan M.M., Bienfano D.C. Spinal stenosis caused by extradural lipomatosis in Cushing's syndrome. N Engl J Med. 1980;302:36. doi: 10.1056/NEJM198001033020107. [DOI] [PubMed] [Google Scholar]
- 8.Sa´ez-Alegre, M. Epidural Lipomatosis and Syringomyelia in Adulthood: Case Report and Literature Review. World Neurosurg. 2019;Volume 129:341–344. doi: 10.1016/j.wneu.2019.06.075. [DOI] [PubMed] [Google Scholar]
- 9.Noël P, Preux G, Thézé A. Epidural lipomatosis: a possible cause of back pain. Ann Phys Rehabil Med. 2014;57:734–737. doi: 10.1016/j.rehab.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 10.Fessler RG, Johnson DL, Brown FD, Erickson RK, Reid SA, Kranzler L. Epidural lipomatosis in steroid-treated patients. Spine. 1992;17:183–188. doi: 10.1097/00007632-199202000-00011. [DOI] [PubMed] [Google Scholar]
- 11.Batzdorf U. Syringomyelia, Chiari malformation, and hydromyelia. In: Youmans J.R., editor. Neurological Surgery. Philadelphia: W. B. Saunders Co.; 1996. [Google Scholar]