Abstract
The long-term sequelae of AKI have received increasing attention so that its associations with a number of adverse outcomes, including higher mortality and development of CKD, are now widely appreciated. These associations take on particular importance when considering the high incidence of AKI, with a lack of proven interventions and uncertainties around optimal care provision meaning that the long-term sequelae of AKI present a major unmet clinical need. In this review, we examine the published data that inform our current understanding of long-term outcomes following AKI and discuss potential knowledge gaps, covering long-term mortality, CKD, progression to ESKD, proteinuria, cardiovascular events, recurrent AKI, and hospital readmission.
Keywords: clinical nephrology, outcomes, progression of renal failure, renal injury, humans, incidence, patient readmission, chronic renal insufficiency, acute kidney injury, chronic kidney failure, disease progression, proteinuria, attention, cardiovascular diseases
Introduction
The incidence of AKI is increasing, affecting up to 20% of hospitalized patients (1–3). Its associations with short-term morbidity and mortality are well recognized, representing a major health care burden, with even small or transient declines in kidney function associating with serious adverse outcomes (4). In parallel, long-term outcomes in AKI survivors have become a major area of interest, with a burgeoning number of studies reporting links between AKI and the development or progression of CKD (5,6), longer-term mortality (5,7), cardiovascular events (8), hospital readmissions (9,10), recurrent AKI (11–14), and poorer quality of life (15). Despite this, there are no established therapeutic interventions to reduce post-AKI sequelae or evidence to inform strategies for health care provision. The latter is important because post-AKI care has been shown to be variable, with many patients not receiving any planned follow-up even when they have received KRT during their acute episode (16,17). This narrative review provides a summary of current evidence regarding the long-term effects of AKI and highlights areas in which controversies or knowledge gaps remain.
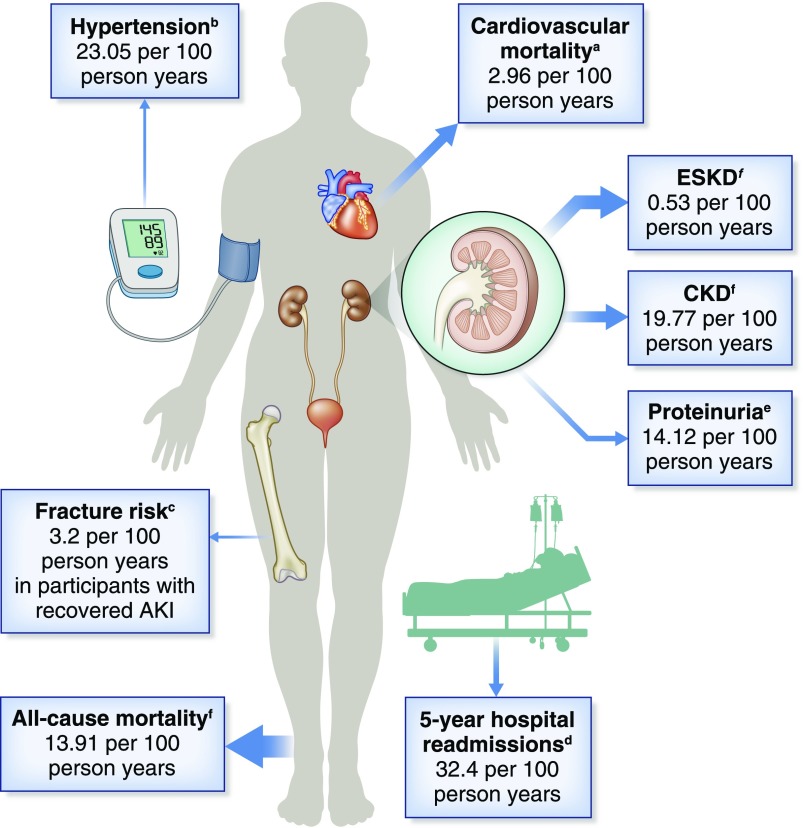
Figure 1.
Summary of reported event rates for long term outcomes after AKI. The size of the arrows are a representation of the number of currently available studies reporting this outcome. It should also be noted that, although the rates are reported in the same units (events/100-person-years), data are taken from different sources and are therefore not directly comparable. The superscript letters indicate the sources of the event rates: aOdutayo et al. (8); bHsu et al. (63); cWang et al. (64); dBrown et al. (9); eHorne et al. (11); and fSee et al. (5).
Long-Term Mortality
Many studies report higher mortality rates in survivors of AKI, which are summarized in two systematic reviews (5,7). In their 2009 review, Coca et al. (7) included 48 studies, but with half exclusively in patients who required KRT, there was a bias toward more severe AKI. Pooled mortality from the 15 studies that had a non-AKI comparator group was 8.9 deaths per 100 person-years following AKI compared with 4.3 deaths per 100 person-years for patients who survived hospitalization without AKI (rate ratio, 2.6; 95% confidence interval [95% CI], 2.0 to 3.4). More recently, See et al. (5) performed a review that included only studies that defined AKI using consensus criteria, thereby ensuring inclusion of patients with all stages of AKI. Additional inclusion criteria were presence of a non-AKI comparator arm and at least 1 year of follow-up. Eighty-two studies were identified, of which 70 reported mortality rates (1,817,999 patients). Mortality in AKI groups (13.2 deaths per 100 person-years) was significantly higher than that seen in comparator groups (7.3 deaths per 100 person-years; hazard ratio, 1.8; 95% CI, 1.6 to 2.0). Both reviews demonstrated that the magnitude of the long-term risk of mortality is higher with increased severity of AKI.
Other common themes include the degree of heterogeneity across studies and variation in the magnitude of reported risk. The latter may reflect differences in study design (e.g., duration of follow-up and definition of AKI), but there are also significant effects of clinical setting. AKI is not a single entity but a heterogeneous syndrome with a wide range of etiologies and a complex array of underlying pathophysiologic processes. In many patients, more than one etiologic factor may be present, and the severity of acute illness and coexisting chronic conditions can also have a significant influence on mortality (18). However, assessing this with any degree of granularity is difficult, in part because the majority of studies are retrospective (5,7). Illustrating this challenge, See et al. (5) grouped ten studies under the subheading of “angiography studies,” of which four included patients undergoing transcatheter aortic valve implantation, three included patients with acute myocardial infarction, one included patients in cardiac resynchronization for heart failure, and two studied a mixture of elective and emergency coronary artery angiography. Specific causes of AKI were generally not reported, and comparisons of the effects of these different settings were limited. However, crude mortality was as high as 57.5% in one study of AKI in the setting of acute MI (19) and as low as 6.9% in elective and emergency patients undergoing coronary angiography (20).
It is, therefore, difficult to conclude to what extent AKI is causally related to long-term mortality. Noncausal associations may exist if AKI occurs more frequently in vulnerable patients who intrinsically have a greater risk of mortality (e.g., those who had a more severe acute illness or a greater burden/severity of chronic conditions). In one sense, this may not matter if AKI is viewed as an independent risk factor for longer-term adverse events, but it would be critical to understand if AKI interventions that aim to reduce long-term mortality are being considered. Although the association between AKI and mortality is strong and remains after adjustment for known confounding factors (21), this does not exclude residual confounding. A note of caution is also sounded when looking at causes of long-term mortality following AKI. In a retrospective administrative database study, Silver et al. (22) described how cardiovascular disease and cancer were the two most common causes of death in the year after AKI, each accounting for approximately a third of patients. It is possible to speculate on mechanisms by which AKI may lead to higher cardiovascular risk; in experimental models, AKI has been shown to induce cardiac apoptosis (23), or alternatively, the development of CKD may in turn increase cardiovascular risk. The latter is hinted at by Bucaloiu et al. (24), who reported that de novo CKD rather than AKI per se accounted for some of the association between AKI and long-term mortality. With respect to cancer mortality, this is far more likely to be an example of noncausal association in which a dominant comorbidity increases risk for AKI but is also the main factor that determines prognosis. In this setting, AKI-targeted interventions may not be effective in improving longer-term mortality. Some studies have suggested that preexisting CKD may modulate the strength of association between AKI and long-term mortality. The multicenter observational PICARD study found that, in a critical care setting, the presence of preexisting CKD before an AKI episode was associated with a 9% lower risk of mortality compared with those with de novo AKI (25). Smaller studies have shown conflicting results and lack longer-term follow-up data beyond 90 days (26,27).
The risk of mortality following AKI may also vary with time. In a regional Scottish database, Sawhney et al. (28) compared mortality risk during the first year after AKI with that in subsequent years. Hazard ratios for mortality were higher in the first year compared with the later time period, suggesting that the prognostic importance of a discrete AKI episode lessens over time. Similar observations have been made by others (29); studies with shorter follow-up periods may, therefore, report higher rates of mortality. The relatively high rates of mortality in AKI survivors, particularly in the first year after AKI, also mean that this competing risk should be considered when assessing other long-term outcomes (i.e., only those who are alive can develop the outcome of interest) and importantly, how this may differ across patient groups (e.g., pediatric versus elderly) or clinical settings (30).
CKD
Despite confounding factors, it is easier to argue causality between AKI and CKD. Every nephrologist has seen patients (particularly those with severe or prolonged AKI) who are left with significantly worse kidney function or do not recover from dialysis dependency after an episode of AKI (31). This was reported as long ago as the 1950s and 1960s. Briggs et al. (32) studied 50 young patients (mean age 38 years old) without significant preexisting kidney disease on average at 3 years after severe acute tubular necrosis. Although “normal well-being was restored with a return to their former occupations,” 71% had lower measured GFR, 17% had measured GFR values of <50 ml/min, and 31% had impaired urinary concentrating ability (32). Furthermore, experimental models of AKI have delineated a number of mechanistic pathways by which AKI causes CKD, albeit noting differences between traditional preclinical models and human AKI (33). Mechanisms, described in detail elsewhere, include maladaptive repair, cell senescence, mitochondrial dysfunction, and programmed cell death, which result in nephron loss, tubulointerstitial fibrosis, microvasculature damage with capillary rarefaction, and endothelial injury (34–40), changes that mimic those seen in CKD and which prime the kidney to further damage (41). Furthermore, observational epidemiologic data consistently report that AKI is associated with a higher risk of CKD, that the effect size is large, and that there is a gradated relationship between severity of AKI and magnitude of risk, with this risk remaining after adjustment for known confounders (5,6).
Observational Studies of CKD Post-AKI
A number of studies have reported associations between AKI and the development or progression of CKD on the basis of eGFR. See et al. (5) identified 19 studies from which the pooled hazard ratio of CKD in those sustaining AKI was 2.67 (95% CI, 1.99 to 3.58) referenced against those who did not. Notably, CKD was defined in different ways: eGFR<60 ml/min per 1.73 m2 (CKD stage G3), eGFR<30 ml/min per 1.73 m2 (CKD stage G4), >25% reduction in eGFR from baseline, or increase in CKD stage. AKI was associated with higher relative risk of developing CKD across all definitions, but absolute event rates were significantly different—earlier stages of CKD were relatively common post-AKI sequelae, but advanced CKD and ESKD were less so.
The most appropriate CKD definition in the post-AKI setting has yet to be determined. Grams et al. (42) studied 161,185 postoperative United States veterans, showing that ≥30% decline in eGFR following AKI was strongly associated with subsequent risk of ESKD. This held true regardless of whether the decline was observed at 30, 60, 90, 180, or 365 days, suggesting that this degree of change is clinically meaningful and warrants further investigation, potentially as a surrogate end point for subsequent ESKD. GFR slope has been also proposed as a surrogate end point for kidney disease progression (43) and may have a role in predicting the development of persistent kidney dysfunction post-AKI. GFR slope assumes linear decline in function, and multiple data points are required for the regression line, which may not always be easy to apply.
Interventional Studies of CKD Post-AKI
Causality is also informed by interventional studies that evaluate whether reducing AKI or its severity results in less CKD subsequently. At present, there are few such studies. Garg et al. (44) analyzed 4752 participants having coronary surgery randomized to on- or off-pump procedures and found that, although the off-pump technique had less postoperative AKI, at 1-year follow-up there was no significant difference in rates of subsequent CKD. It is important to note that the majority of AKI in this study was mild (only 7% of AKI was stage 2 or 3), that the effect size of the intervention was modest, and that follow-up duration was only 1 year. These results do not, therefore, refute a causal link between AKI and subsequent CKD but emphasize that this is not ubiquitous in all patients, particularly in those with milder AKI. Similar conclusions come from a meta-analysis of trials that reported increased and decreased risk of acute serum creatinine changes in heart failure and renin-angiotensin-aldosterone system inhibition (45). Conversely, the STOP-AKI trial gives an alternative perspective. Although this was a short-term study with a negative primary outcome, secondary outcomes of kidney recovery (endogenous creatinine clearance at days 21 and 28) were improved with recombinant alkaline phosphatase (46). Although secondary end points should not be overinterpreted, we can speculate as to how this result, if confirmed, may affect on longer-term kidney function. More such studies are clearly needed, ideally incorporating longer-term assessments of kidney function.
ESKD
As with mortality, epidemiologic data on CKD and ESKD following AKI have been summarized in systematic reviews (5,6). Earlier studies tended to focus on more severe AKI, identifying patients via the requirement for acute dialysis or via coded diagnoses and focusing on the development of ESKD. Ishani et al. (47) reported that, in 233,803 Medicare patients, 3.1% had an ICD-9 code of AKI and survived to discharge, and over 2 years, 0.5% subsequently developed ESKD. Adjusted hazard ratios for developing ESKD were much higher with an episode of AKI (41 in patients with AKI and CKD and 13 for AKI alone compared with no kidney disease). Also using Medicare data and studying patients admitted with a myocardial infarction, Newsome et al. (48) described how changes in serum creatinine are also associated with ESKD across all stages of AKI, with progressively larger effect sizes with bigger creatinine increments. More recently, James et al. (21) reported similar patterns in patients who sustained AKI (defined by AKIN criteria) following angiography. Careful statistical analysis, including adjustment for factors that may affect CKD progression (such as baseline eGFR and proteinuria), showed a >4-fold increase in adjusted risk of ESKD in AKI stage 1 and a >11-fold increase in AKI stage 2 or 3, with ESKD occurring in 0.6% of the study population.
Proteinuria following AKI
There are no studies that incorporate the development of albuminuria in their definition of post-AKI CKD, which is a major limitation given the large body of evidence identifying albuminuria as an independent risk factor for adverse outcomes (11). Published data indicate that a substantial proportion of patients have albuminuria following AKI; 41% of those sustaining AKI in a prospective cohort study had albuminuria (>3 mg/mmol) after 3-year follow-up versus 21% of non-AKI comparators (11). In patients with AKI in the ICU, long-term follow-up data from the Randomized Evaluation of Normal versus Augmented Levels of KRT trial showed similar results, with 42% having albuminuria (ACR>3.5 mg/mmol) at a median follow-up of 42 months (49). Including albuminuria has the potential to significantly increase the number of patients identified with CKD following AKI. However, it is known that proteinuria increases the risk of AKI episodes (50), and therefore, differentiating de novo from preexisting proteinuria following AKI can be challenging. Two recent studies have clarified this. In a retrospective cohort study of 90,614 United States veterans with a urine dipstick result in the year before hospitalization, Parr et al. (51) reported that the presence of proteinuria was significantly higher during each month of follow-up in an AKI cohort compared with those without AKI (matched for baseline proteinuria, diabetes, and CKD stage), although ascertainment bias and measurement error with urinalysis are potential limitations. Hsu et al. (52) analyzed data from two prospective cohorts together totaling 2048 patients who either had CKD or had been hospitalized with or without AKI. Annual urine protein-creatinine ratio was collected, and comparisons were made between the 324 patients who experienced AKI during follow-up and those who did not. AKI was independently associated with a 9% increase in urine protein-creatinine ratio that was not due to higher BP or cessation of renin-angiotensin-aldosterone system inhibitors. Together, these data argue that AKI is mechanistically linked to the development or worsening of proteinuria, at least in some patients. A number of unanswered questions then follow as how best to detect and manage proteinuria in AKI survivors.
Factors Associated with CKD following AKI
Factors associated with higher risk of CKD following AKI include AKI severity (53), duration of AKI (54), recurrent AKI episodes (55), and receipt of acute KRT (53). The Acute Disease Quality Initiative has emphasized the importance of AKI duration by proposing the term acute kidney disease to describe AKI stage 1 or greater that is present ≥7 days after AKI initiation (56), and data are beginning to emerge showing that acute kidney disease is associated with increased rates of long-term mortality, CKD, proteinuria, and ESKD (57,58). Baseline kidney function is also of importance because AKI with preexisting CKD dramatically increases risk of subsequent ESKD (47,59,60). Coexisting CKD risk factors that may exist independently of the AKI episode but have been associated with higher risk include age, diabetes mellitus, hypertension, heart failure, liver disease, Charlson index, and serum albumin (61). Attempting to move toward practical risk assessment, James et al. (62) developed a risk prediction tool for advanced CKD (defined as CKD stage G4) following AKI using retrospective data but including internal and external validation. Six variables were independently associated with CKD: age, women, higher baseline creatinine, albuminuria (at the time of AKI or within the following 6 months), AKI stage, and higher creatinine at discharge. Model performance was good, with c-statistic values of 0.86 and 0.81 in development and external validation cohorts, respectively. However, candidate variables were identified from retrospective data, and therefore, important risk factors, particularly details of the AKI episode, were not available. Indeed, many existing studies have similar limitations, and to move toward improved identification of high-risk patients or patient groups, prospective studies are needed with granular descriptions of patient-level data, including specifics of the AKI episode and careful consideration of preexisting risk factors for CKD progression.
Other Long-Term Outcomes Associated with AKI
A number of other clinically relevant outcomes have been reported to occur more frequently following AKI. Further episodes of AKI are more likely in AKI survivors, and they are independently associated with higher risk of subsequent CKD and ESKD (11–14). AKI is associated with risk of hospital readmission, of which a leading cause is pulmonary edema/heart failure; this risk is seen in the first 90 days and persists to 5 years (9,10). Consistent with this, higher risks of cardiovascular events and in particular, heart failure are also reported; a systematic review incorporating 25 studies concluded that AKI was associated with a 58% higher risk of congestive heart failure, a 40% higher risk of acute myocardial infarction, and a 15% higher risk of stroke (8). Additionally, a large retrospective study suggested that AKI is associated with a 22% higher risk of hypertension (63). Other outcomes reported after AKI include a higher risk of hip fracture after dialysis-requiring AKI (64) and higher fibroblast growth factor 23 levels that are associated with higher risk of developing a composite end point of KRT/mortality, an association that persisted when adjusted for age and enrolment creatinine (65). It has also been suggested that dialysis-requiring AKI confers a higher risk of developing new-onset sepsis, possibly due to immunomodulatory responses (66,67). Again, most available data come from retrospective studies, and many arise from highly selected patient groups. To what degree AKI is causally related to these outcomes and which particular patient groups are vulnerable to different outcomes remain to be established.
AKI Aftercare
It is clear that many people who survive an episode of AKI do not receive any follow-up. Silver and Siew (68) concluded that less than half of the highest-risk patients with the most severe forms of AKI were seen by a nephrologist after discharge. Even for patients requiring dialysis for AKI, follow-up rates can be as low as 12% within 3 months (17). Another study of 3929 patients found that just 10.6% (95% CI, 6.4 to 15.9) of patients with AKI stage 3 had been referred for nephrology follow-up by 12 months (16). One observational study has reported that nephrology follow-up for those who receive acute dialysis is associated with better survival, although this finding may reflect patient selection because early nephrology follow-up was also associated with a higher risk of long-term dialysis (69). Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommend that all patients are evaluated at three months (70), but there is currently no consensus as to who should be followed up after an episode of AKI and what form this should take. Communication between health care providers and patients is also important. A recent observational study of 137 patients with moderate to severe AKI showed that 80% of patients were unaware of their diagnosis (71), and it is estimated that less than half of hospital discharge documentation records AKI (72,73). There is, therefore, a significant opportunity to develop and test different approaches to post-AKI care, as well as to work to improve recognition and communication. Because AKI is such a heterogenous syndrome, it is unlikely that a “one size fits all” approach will work, and tailoring post-AKI care to the specific needs of different patients or patient subgroups may be needed.
Conclusions and Areas of Uncertainty
AKI is strongly associated with a number of long-term sequelae, and in some patients, it leads to subsequent CKD. Considering the high incidence of AKI and improvements in short-term survival (74), these long-term sequelae of AKI present a major unmet clinical need, with no proven interventions or data to inform optimal care provision. Patients often receive no follow-up after hospital discharge (16), and they often do not realize that they have had AKI (71,75). The evidence base describing the long-term sequelae of AKI continues to grow, adding to our understanding and increasing awareness of these issues. However, knowledge gaps still remain, and those highlighted in this review are summarized in Table 1. The ultimate goal is to develop effective interventions, which may be pharmacologic interventions or improvements in health care service planning. They may target AKI as the mechanistic driver of the higher rates of adverse long-term outcomes or use AKI as a signpost of more vulnerable patients. It is likely that different interventions will be required in different patient populations or clinical settings, for which better characterization of individual patients is needed to determine high-risk groups, along with standardized approaches to the definition of long-term outcomes (in particular, those around eGFR and albuminuria) and improved understanding of the mechanisms of the AKI to CKD transition in humans.
Table 1.
Summary of knowledge gaps in current understanding of the long-term outcomes of AKI
| Areas of Uncertainty/Knowledge Gaps in Our Understanding of the Long-Term Outcomes of AKI | Suggestions for Next Steps |
|---|---|
| To what degree the association between AKI and mortality is causal | Prospective data collection with adequate consideration of confounding variables, intervention studies that demonstrate reduced mortality |
| Understanding of the mechanism of the link between AKI and CKD in humans | Translation of animal models to humans; clinical studies incorporating methods that improve mechanistic understanding of the AKI to CKD transition in humans (e.g., biopsy, biomarkers, or imaging) |
| Incorporation of etiologic factors into assessment and definition of AKI | Development of tools that include AKI etiology in assessment; prospective data collection focusing on precise etiology of AKI |
| Optimal measurement of kidney function following AKI | Consensus definition to allow for harmonization of data going forward |
| Understanding the incidence of albuminuria post-AKI because this might be a potential target for future intervention | Incorporation of albuminuria into CKD definition post-AKI in line with the KDIGO CKD definition; further study of albuminuria as an independent risk factor for adverse outcomes in a post-AKI setting |
| Establish the role of existing or novel biomarkers in the recovery phase of AKI to improve risk stratification and/or provide mechanistic insights into the AKI to CKD transition | Collection of biomarkers at time of AKI combined with collection of biomarkers during recovery |
| Availability of interventions that reduce long-term sequelae following AKI | Studies into optimal or tailored follow-up strategies and research into gaps in current post-AKI care |
KDIGO, Kidney Disease Improving Global Outcomes.
Disclosures
Dr. Lucas, Dr. Noble, and Dr. Selby have nothing to disclose.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Xue JL, Daniels F, Star RA, Kimmel PL, Eggers PW, Molitoris BA, Himmelfarb J, Collins AJ: Incidence and mortality of acute renal failure in Medicare beneficiaries, 1992 to 2001. J Am Soc Nephrol 17: 1135–1142, 2006 [DOI] [PubMed] [Google Scholar]
- 2.Hsu CY, McCulloch CE, Fan D, Ordoñez JD, Chertow GM, Go AS: Community-based incidence of acute renal failure. Kidney Int 72: 208–212, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Susantitaphong P, Cruz DN, Cerda J, Abulfaraj M, Alqahtani F, Koulouridis I, Jaber BL; Acute Kidney Injury Advisory Group of the American Society of Nephrology: World incidence of AKI: A meta-analysis. Clin J Am Soc Nephrol 8: 1482–1493, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chertow GM, Burdick E, Honour M, Bonventre JV, Bates DW: Acute kidney injury, mortality, length of stay, and costs in hospitalized patients. J Am Soc Nephrol 16: 3365–3370, 2005 [DOI] [PubMed] [Google Scholar]
- 5.See EJ, Jayasinghe K, Glassford N, Bailey M, Johnson DW, Polkinghorne KR, Toussaint ND, Bellomo R: Long-term risk of adverse outcomes after acute kidney injury: A systematic review and meta-analysis of cohort studies using consensus definitions of exposure. Kidney Int 95: 160–172, 2019 [DOI] [PubMed] [Google Scholar]
- 6.Coca SG, Singanamala S, Parikh CR: Chronic kidney disease after acute kidney injury: A systematic review and meta-analysis. Kidney Int 81: 442–448, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Coca SG, Yusuf B, Shlipak MG, Garg AX, Parikh CR: Long-term risk of mortality and other adverse outcomes after acute kidney injury: A systematic review and meta-analysis. Am J Kidney Dis 53: 961–973, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Odutayo A, Wong CX, Farkouh M, Altman DG, Hopewell S, Emdin CA, Hunn BH: AKI and long-term risk for cardiovascular events and mortality. J Am Soc Nephrol 28: 377–387, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brown JR, Hisey WM, Marshall EJ, Likosky DS, Nichols EL, Everett AD, Pasquali SK, Jacobs ML, Jacobs JP, Parikh CR: Acute kidney injury severity and long-term readmission and mortality after cardiac surgery. Ann Thorac Surg 102: 1482–1489, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sawhney S, Marks A, Fluck N, McLernon DJ, Prescott GJ, Black C: Acute kidney injury as an independent risk factor for unplanned 90-day hospital readmissions. BMC Nephrol 18: 9, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horne KL, Packington R, Monaghan J, Reilly T, Selby NM: Three-year outcomes after acute kidney injury: Results of a prospective parallel group cohort study. BMJ Open 7: e015316, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holmes J, Geen J, Williams JD, Phillips AO: Recurrent acute kidney injury: Predictors and impact in a large population-based cohort [published online ahead of print August 3, 2019]. Nephrol Dial Transplant doi: 10.1093/ndt/gfz155 [DOI] [PubMed] [Google Scholar]
- 13.Hounkpatin HO, Fraser SDS, Glidewell L, Blakeman T, Lewington A, Roderick PJ: Predicting risk of recurrent acute kidney injury: A systematic review. Nephron 142: 83–90, 2019 [DOI] [PubMed] [Google Scholar]
- 14.Sykes L, Asar O, Ritchie J, Raman M, Vassallo D, Alderson HV, O’Donoghue DJ, Green D, Diggle PJ, Kalra PA: The influence of multiple episodes of acute kidney injury on survival and progression to end stage kidney disease in patients with chronic kidney disease. PLoS One 14: e0219828, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Johansen KL, Smith MW, Unruh ML, Siroka AM, O’Connor TZ, Palevsky PM; VA/NIH Acute Renal Failure Trial Network: Predictors of health utility among 60-day survivors of acute kidney injury in the Veterans Affairs/National Institutes of Health Acute Renal Failure Trial Network Study. Clin J Am Soc Nephrol 5: 1366–1372, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siew ED, Peterson JF, Eden SK, Hung AM, Speroff T, Ikizler TA, Matheny ME: Outpatient nephrology referral rates after acute kidney injury. J Am Soc Nephrol 23: 305–312, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kirwan CJ, Blunden MJ, Dobbie H, James A, Nedungadi A, Prowle JR: Critically ill patients requiring acute renal replacement therapy are at an increased risk of long-term renal dysfunction, but rarely receive specialist nephrology follow-up. Nephron 129: 164–170, 2015 [DOI] [PubMed] [Google Scholar]
- 18.Pereira MB, Zanetta DM, Abdulkader RC: The real importance of pre-existing comorbidities on long-term mortality after acute kidney injury. PLoS One 7: e47746, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chawla LS, Amdur RL, Shaw AD, Faselis C, Palant CE, Kimmel PL: Association between AKI and long-term renal and cardiovascular outcomes in United States veterans. Clin J Am Soc Nephrol 9: 448–456, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kimura T, Obi Y, Yasuda K, Sasaki K, Takeda Y, Nagai Y, Imai E, Rakugi H, Isaka Y, Hayashi T: Effects of chronic kidney disease and post-angiographic acute kidney injury on long-term prognosis after coronary artery angiography. Nephrol Dial Transplant 26: 1838–1846, 2011 [DOI] [PubMed] [Google Scholar]
- 21.James MT, Ghali WA, Knudtson ML, Ravani P, Tonelli M, Faris P, Pannu N, Manns BJ, Klarenbach SW, Hemmelgarn BR; Alberta Provincial Project for Outcome Assessment in Coronary Heart Disease (APPROACH) Investigators: Associations between acute kidney injury and cardiovascular and renal outcomes after coronary angiography. Circulation 123: 409–416, 2011 [DOI] [PubMed] [Google Scholar]
- 22.Silver SA, Harel Z, McArthur E, Nash DM, Acedillo R, Kitchlu A, Garg AX, Chertow GM, Bell CM, Wald R: Causes of death after a hospitalization with AKI. J Am Soc Nephrol 29: 1001–1010, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kelly KJ: Distant effects of experimental renal ischemia/reperfusion injury. J Am Soc Nephrol 14: 1549–1558, 2003 [DOI] [PubMed] [Google Scholar]
- 24.Bucaloiu ID, Kirchner HL, Norfolk ER, Hartle JE 2nd, Perkins RM: Increased risk of death and de novo chronic kidney disease following reversible acute kidney injury. Kidney Int 81: 477–485, 2012 [DOI] [PubMed] [Google Scholar]
- 25.Khosla N, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini E, Mehta RL; Program to Improve Care in Acute Renal Disease (PICARD): Preexisting chronic kidney disease: A potential for improved outcomes from acute kidney injury. Clin J Am Soc Nephrol 4: 1914–1919, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pan HC, Wu PC, Wu VC, Yang YF, Huang TM, Shiao CC, Chen TC, Tarng DC, Lin JH, Yang WS, Sun CY, Lin CY, Chu TS, Wu MS, Wu KD, Chen YC, Huang CC; Taiwan Consortium for Acute Kidney Injury and Renal Diseases (CAKs): A nationwide survey of clinical characteristics, management, and outcomes of acute kidney injury (AKI)—patients with and without preexisting chronic kidney disease have different prognoses. Medicine (Baltimore) 95: e4987, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neyra JA, Mescia F, Li X, Adams-Huet B, Yessayan L, Yee J, Toto RD, Moe OW: Impact of acute kidney injury and CKD on adverse outcomes in critically ill septic patients. Kidney Int Rep 3: 1344–1353, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sawhney S, Marks A, Fluck N, Levin A, Prescott G, Black C: Intermediate and long-term outcomes of survivors of acute kidney injury episodes: A large population-based cohort study. Am J Kidney Dis 69: 18–28, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lafrance JP, Miller DR: Acute kidney injury associates with increased long-term mortality. J Am Soc Nephrol 21: 345–352, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Selby NM, Taal MW: Long-term outcomes after AKI—a major unmet clinical need. Kidney Int 95: 21–23, 2019 [DOI] [PubMed] [Google Scholar]
- 31.Hsu CY: Yes, AKI truly leads to CKD. J Am Soc Nephrol 23: 967–969, 2012 [DOI] [PubMed] [Google Scholar]
- 32.Briggs JD, Kennedy AC, Young LN, Luke RG, Gray M: Renal function after acute tubular necrosis. BMJ 3: 513–516, 1967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.de Caestecker M, Humphreys BD, Liu KD, Fissell WH, Cerda J, Nolin TD, Askenazi D, Mour G, Harrell FE Jr., Pullen N, Okusa MD, Faubel S; ASN AKI Advisory Group: Bridging translation by improving preclinical study design in AKI. J Am Soc Nephrol 26: 2905–2916, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Devarajan P: Update on mechanisms of ischemic acute kidney injury. J Am Soc Nephrol 17: 1503–1520, 2006 [DOI] [PubMed] [Google Scholar]
- 35.Finn WF: Enhanced recovery from postischemic acute renal failure. Micropuncture studies in the rat. Circ Res 46: 440–448, 1980 [DOI] [PubMed] [Google Scholar]
- 36.Fox M: Progressive renal fibrosis following acute tubular necrosis: An experimental study. J Urol 97: 196–202, 1967 [DOI] [PubMed] [Google Scholar]
- 37.Basile DP: Rarefaction of peritubular capillaries following ischemic acute renal failure: A potential factor predisposing to progressive nephropathy. Curr Opin Nephrol Hypertens 13: 1–7, 2004 [DOI] [PubMed] [Google Scholar]
- 38.Burne-Taney MJ, Liu M, Ascon D, Molls RR, Racusen L, Rabb H: Transfer of lymphocytes from mice with renal ischemia can induce albuminuria in naive mice: A possible mechanism linking early injury and progressive renal disease? Am J Physiol Renal Physiol 291: F981–F986, 2006 [DOI] [PubMed] [Google Scholar]
- 39.Basile DP, Donohoe D, Roethe K, Osborn JL: Renal ischemic injury results in permanent damage to peritubular capillaries and influences long-term function. Am J Physiol Renal Physiol 281: F887–F899, 2001 [DOI] [PubMed] [Google Scholar]
- 40.Zuk A, Bonventre JV: Recent advances in acute kidney injury and its consequences and impact on chronic kidney disease. Curr Opin Nephrol Hypertens 28: 397–405, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Venkatachalam MA, Griffin KA, Lan R, Geng H, Saikumar P, Bidani AK: Acute kidney injury: A springboard for progression in chronic kidney disease. Am J Physiol Renal Physiol 298: F1078–F1094, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Grams ME, Sang Y, Coresh J, Ballew SH, Matsushita K, Levey AS, Greene TH, Molnar MZ, Szabo Z, Kalantar-Zadeh K, Kovesdy CP: Candidate surrogate end points for ESRD after AKI. J Am Soc Nephrol 27: 2851–2859, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Inker LA, Heerspink HJL, Tighiouart H, Levey AS, Coresh J, Gansevoort RT, Simon AL, Ying J, Beck GJ, Wanner C, Floege J, Li PK, Perkovic V, Vonesh EF, Greene T: GFR slope as a surrogate end point for kidney disease progression in clinical trials: A meta-analysis of treatment effects of randomized controlled trials. J Am Soc Nephrol 30: 1735–1745, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Garg AX, Devereaux PJ, Yusuf S, Cuerden MS, Parikh CR, Coca SG, Walsh M, Novick R, Cook RJ, Jain AR, Pan X, Noiseux N, Vik K, Stolf NA, Ritchie A, Favaloro RR, Parvathaneni S, Whitlock RP, Ou Y, Lawrence M, Lamy A; CORONARY Investigators: Kidney function after off-pump or on-pump coronary artery bypass graft surgery: A randomized clinical trial. JAMA 311: 2191–2198, 2014 [DOI] [PubMed] [Google Scholar]
- 45.Coca SG, Zabetian A, Ferket BS, Zhou J, Testani JM, Garg AX, Parikh CR: Evaluation of short-term changes in serum creatinine level as a meaningful end point in randomized clinical trials. J Am Soc Nephrol 27: 2529–2542, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pickkers P, Mehta RL, Murray PT, Joannidis M, Molitoris BA, Kellum JA, Bachler M, Hoste EAJ, Hoiting O, Krell K, Ostermann M, Rozendaal W, Valkonen M, Brealey D, Beishuizen A, Meziani F, Murugan R, de Geus H, Payen D, van den Berg E, Arend J; STOP-AKI Investigators: Effect of human recombinant alkaline phosphatase on 7-day creatinine clearance in patients with sepsis-associated acute kidney injury: A randomized clinical trial. JAMA 320: 1998–2009, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ishani A, Xue JL, Himmelfarb J, Eggers PW, Kimmel PL, Molitoris BA, Collins AJ: Acute kidney injury increases risk of ESRD among elderly. J Am Soc Nephrol 20: 223–228, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Newsome BB, Warnock DG, McClellan WM, Herzog CA, Kiefe CI, Eggers PW, Allison JJ: Long-term risk of mortality and end-stage renal disease among the elderly after small increases in serum creatinine level during hospitalization for acute myocardial infarction. Arch Intern Med 168: 609–616, 2008 [DOI] [PubMed] [Google Scholar]
- 49.Gallagher M, Cass A, Bellomo R, Finfer S, Gattas D, Lee J, Lo S, McGuinness S, Myburgh J, Parke R, Rajbhandari D; POST-RENAL Study Investigators and the ANZICS Clinical Trials Group: Long-term survival and dialysis dependency following acute kidney injury in intensive care: Extended follow-up of a randomized controlled trial. PLoS Med 11: e1001601, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.James MT, Hemmelgarn BR, Wiebe N, Pannu N, Manns BJ, Klarenbach SW, Tonelli M; Alberta Kidney Disease Network: Glomerular filtration rate, proteinuria, and the incidence and consequences of acute kidney injury: A cohort study. Lancet 376: 2096–2103, 2010 [DOI] [PubMed] [Google Scholar]
- 51.Parr SK, Matheny ME, Abdel-Kader K, Greevy RA Jr., Bian A, Fly J, Chen G, Speroff T, Hung AM, Ikizler TA, Siew ED: Acute kidney injury is a risk factor for subsequent proteinuria. Kidney Int 93: 460–469, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hsu CY, Hsu RK, Liu KD, Yang J, Anderson A, Chen J, Chinchilli VM, Feldman HI, Garg AX, Hamm L, Himmelfarb J, Kaufman JS, Kusek JW, Parikh CR, Ricardo AC, Rosas SE, Saab G, Sha D, Siew ED, Sondheimer J, Taliercio JJ, Yang W, Go AS; Chronic Renal Insufficiency Cohort (CRIC) Study Investigators and the Assessment, Serial Evaluation, and Subsequent Sequelae of Acute Kidney Injury (ASSESS-AKI) Study: Impact of AKI on urinary protein excretion: Analysis of two prospective cohorts. J Am Soc Nephrol 30: 1271–1281, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chawla LS, Amdur RL, Amodeo S, Kimmel PL, Palant CE: The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int 79: 1361–1369, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kellum JA, Sileanu FE, Murugan R, Lucko N, Shaw AD, Clermont G: Classifying AKI by urine output versus serum creatinine level. J Am Soc Nephrol 26: 2231–2238, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thakar CV, Christianson A, Himmelfarb J, Leonard AC: Acute kidney injury episodes and chronic kidney disease risk in diabetes mellitus. Clin J Am Soc Nephrol 6: 2567–2572, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chawla LS, Bellomo R, Bihorac A, Goldstein SL, Siew ED, Bagshaw SM, Bittleman D, Cruz D, Endre Z, Fitzgerald RL, Forni L, Kane-Gill SL, Hoste E, Koyner J, Liu KD, Macedo E, Mehta R, Murray P, Nadim M, Ostermann M, Palevsky PM, Pannu N, Rosner M, Wald R, Zarbock A, Ronco C, Kellum JA; Acute Disease Quality Initiative Workgroup 16.: Acute kidney disease and renal recovery: Consensus report of the Acute Disease Quality Initiative (ADQI) 16 Workgroup. Nat Rev Nephrol 13: 241–257, 2017 [DOI] [PubMed] [Google Scholar]
- 57.Kellum JA, Sileanu FE, Bihorac A, Hoste EA, Chawla LS: Recovery after acute kidney injury. Am J Respir Crit Care Med 195: 784–791, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.James MT, Levey AS, Tonelli M, Tan Z, Barry R, Pannu N, Ravani P, Klarenbach SW, Manns BJ, Hemmelgarn BR: Incidence and prognosis of acute kidney diseases and disorders using an integrated approach to laboratory measurements in a Universal health care system. JAMA Netw Open 2: e191795, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sawhney S, Mitchell M, Marks A, Fluck N, Black C: Long-term prognosis after acute kidney injury (AKI): What is the role of baseline kidney function and recovery? A systematic review. BMJ Open 5: e006497, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wu VC, Huang TM, Lai CF, Shiao CC, Lin YF, Chu TS, Wu PC, Chao CT, Wang JY, Kao TW, Young GH, Tsai PR, Tsai HB, Wang CL, Wu MS, Chiang WC, Tsai IJ, Hu FC, Lin SL, Chen YM, Tsai TJ, Ko WJ, Wu KD: Acute-on-chronic kidney injury at hospital discharge is associated with long-term dialysis and mortality. Kidney Int 80: 1222–1230, 2011 [DOI] [PubMed] [Google Scholar]
- 61.Fortrie G, de Geus HRH, Betjes MGH: The aftermath of acute kidney injury: A narrative review of long-term mortality and renal function. Crit Care 23: 24, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.James MT, Pannu N, Hemmelgarn BR, Austin PC, Tan Z, McArthur E, Manns BJ, Tonelli M, Wald R, Quinn RR, Ravani P, Garg AX: Derivation and external validation of prediction models for advanced chronic kidney disease following acute kidney injury. JAMA 318: 1787–1797, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hsu CY, Hsu RK, Yang J, Ordonez JD, Zheng S, Go AS: Elevated BP after AKI. J Am Soc Nephrol 27: 914–923, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang WJ, Chao CT, Huang YC, Wang CY, Chang CH, Huang TM, Lai CF, Huang HY, Shiao CC, Chu TS, Chen YM, Wu VC, Ko WJ, Wu KD; National Taiwan University Study Group on Acute Renal Failure: The impact of acute kidney injury with temporary dialysis on the risk of fracture. J Bone Miner Res 29: 676–684, 2014 [DOI] [PubMed] [Google Scholar]
- 65.Leaf DE, Wolf M, Waikar SS, Chase H, Christov M, Cremers S, Stern L: FGF-23 levels in patients with AKI and risk of adverse outcomes. Clin J Am Soc Nephrol 7: 1217–1223, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lai TS, Wang CY, Pan SC, Huang TM, Lin MC, Lai CF, Wu CH, Wu VC, Chien KL; National Taiwan University Hospital Study Group on Acute Renal Failure (NSARF): Risk of developing severe sepsis after acute kidney injury: A population-based cohort study. Crit Care 17: R231, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mehta RL, Bouchard J, Soroko SB, Ikizler TA, Paganini EP, Chertow GM, Himmelfarb J; Program to Improve Care in Acute Renal Disease (PICARD) Study Group: Sepsis as a cause and consequence of acute kidney injury: Program to Improve Care in Acute Renal Disease. Intensive Care Med 37: 241–248, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Silver SA, Siew ED: Follow-up care in acute kidney injury: Lost in transition. Adv Chronic Kidney Dis 24: 246–252. [DOI] [PubMed]
- 69.Harel Z, Wald R, Bargman JM, Mamdani M, Etchells E, Garg AX, Ray JG, Luo J, Li P, Quinn RR, Forster A, Perl J, Bell CM: Nephrologist follow-up improves all-cause mortality of severe acute kidney injury survivors. Kidney Int 83: 901–908, 2013 [DOI] [PubMed] [Google Scholar]
- 70.Khwaja A: KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract 120: c179–c184, 2012 [DOI] [PubMed] [Google Scholar]
- 71.Siew ED, Parr SK, Wild MG, Levea SL, Mehta KG, Umeukeje EM, Silver SA, Ikizler TA, Cavanaugh KL: Kidney disease awareness and knowledge among survivors of acute kidney injury. Am J Nephrol 49: 449–459, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Greer RC, Liu Y, Crews DC, Jaar BG, Rabb H, Boulware LE: Hospital discharge communications during care transitions for patients with acute kidney injury: A cross-sectional study. BMC Health Serv Res 16: 449, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sautenet B, Caille A, Giraudeau B, Léger J, Vourc’h P, Buchler M, Halimi JM: Deficits in information transfer between hospital-based and primary-care physicians, the case of kidney disease: A cross-sectional study. J Nephrol 28: 563–570, 2015 [DOI] [PubMed] [Google Scholar]
- 74.Hoste EAJ, Kellum JA, Selby NM, Zarbock A, Palevsky PM, Bagshaw SM, Goldstein SL, Cerdá J, Chawla LS: Global epidemiology and outcomes of acute kidney injury. Nat Rev Nephrol 14: 607–625, 2018 [DOI] [PubMed] [Google Scholar]
- 75.Ortiz-Soriano V, Alcorn JL 3rd, Li X, Elias M, Ayach T, Sawaya BP, Malluche HH, Wald R, Silver SA, Neyra JA: A survey study of self-rated patients’ knowledge about AKI in a post-discharge AKI clinic. Can J Kidney Health Dis 6: 2054358119830700, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]