Abstract
Background
To analyze the effects of BRCA1/2 mutations on chemotherapy response scores (CRS) and survival in a cohort of patients with advanced-stage ovarian cancer who were treated with neoadjuvant chemotherapy (NAC) followed by interval debulking surgery (IDS).
Methods
We retrospectively reviewed the medical records of 169 high-grade serous ovarian cancer patients who underwent a germline BRCA1/2 test and received three cycles of NAC at the Yonsei Cancer Center from 2006 to 2018. Chemotherapy response scores were compared in patients with and without BRCA1/2 mutations. The effects of BRCA1/2 mutations and CRS on survival were evaluated.
Results
BRCA1/2 mutations were detected in 47 (28.1%) of the 169 patients. Overall, 16 (34.0%) patients with BRCA1/2 mutations had a CRS 3 to chemotherapy compared to scores of 43 in patients (35.2%) without a mutation. Response scores of 3 in patients with BRCA1/2 mutations were not significantly associated with either improved progression-free survival (PFS) (P = 0.949) or overall survival (OS) (P = 0.168). However, CRS 3 in patients without BRCA mutations was significantly associated with both improved PFS (P = 0.030) and OS (P = 0.039). In patients with CRS1/2, carriers of BRCA1/2 mutations had better PFS (P = 0.0344) and OS (P = 0.043) than wild-type BRCA genotype patients.
Conclusion
In ovarian cancer patients treated with NAC, CRS did not predict survival for BRCA 1/2 mutation carriers but did for BRCA wild-type patients.
Keywords: Ovarian cancer, Neoadjuvant chemotherapy, Germline BRCA, Chemotherapy response scores
Background
Primary cytoreductive surgery followed by platinum-based doublet chemotherapy has been considered standard treatment for advanced-stage ovarian cancer. However, several randomized clinical trials showed that their survival outcomes and postoperative morbidity and mortality after neoadjuvant chemotherapy (NAC) followed by interval debulking surgery (IDS) were at least as good as the results for patients who primary cytoreductive surgery [1–4]. Recently, NAC followed by IDS has become an alternative treatment for advanced-stage ovarian cancer patients.
Bohm et al. proposed a three-tiered histopathologic scoring system for grading the response to NAC [5]. A three-tiered chemotherapy response scores (CRS) system was applied to the omental tissue sections and correlated with progression-free survival (PFS) [5, 6]. As a consequence, an increasing body of research has addressed whether CRS 3 can be used as a surrogate marker, similar to the way the pathologic complete response (pCR) is used in breast cancer, in the prognosis for patients with advanced-stage ovarian cancer treated with NAC followed by IDS. However, platinum-based doublet chemotherapy remains the standard of care for advanced-stage ovarian cancer patients who are treated with NAC followed by IDS, regardless of their response to chemotherapy.
Mutations in BRCA1 and BRCA2 have been recognized as a predictor of advanced-stage ovarian cancer susceptibility and a prognostic factor [7–9]. Compared with wild-type BRCA genotype patients, patients with advanced-stage ovarian cancer and BRCA1/2 mutations have been reported to have higher clinical response rates to platinum-based chemotherapy [10–12]. Therefore, there are unanswered questions about whether the higher CRS by carriers of the BRCA1/2 germline mutations represents a better prognosis. In triple-negative breast cancers treated with NAC, several studies have tried to identify the relationships between germline BRCA1/2 mutations, response rates, and prognoses [13, 14]. These studies have shown that patients with BRCA1/2 mutations had superior response rates, and response rate was a weaker predictor of disease-free survival rates compared with wild-type BRCA1/2 genotype patients.
In this study, we analyzed the extent to which CRS depended on germline BRCA1/2 mutations, whether CRS correlates with platinum-based chemotherapy, and whether CRS has an impact on survival outcomes in patients with and without germline BRCA1/2 mutations.
Methods
Study populations
We retrospectively reviewed the medical records of 326 patients with pathologically confirmed ovarian cancer who from 2006 to 2018 received NAC at the Yonsei Cancer Center, Seoul, South Korea. Patients with stage III or IV ovarian carcinoma who received three cycles of NAC followed by IDS were included in the study.
The exclusion criteria were as follows: Patients still receiving chemotherapy at the time of data analysis (N = 19); patients who had not received IDS after NAC (N = 15); patients for whom data was missing (N = 31); and, lastly, patients who had not undergone a germline BRCA test (N = 92). After this review, 169 patients met our criteria. Of these, 122 patients had the wild-type BRCA genotype, and 47 had BRCA1 or BRCA2 mutations (Fig. 1).
Fig. 1.
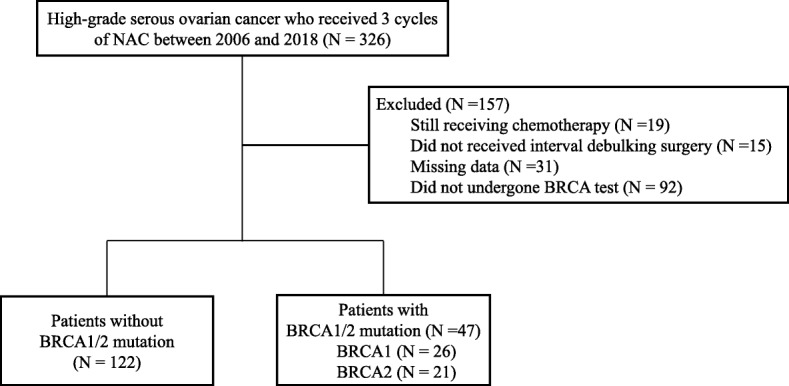
Flow diagram of the study population. NAC, neoadjuvant chemotherapy
Treatment
Most patients received taxane (paclitaxel, docetaxel) and platinum (carboplatin) combination chemotherapy and some patients received paclitaxel, carboplatin and bevacizumab combination chemotherapy. Other treatments such as radiation or endocrine therapy were not performed before surgery. Determination of which patients required NAC was based on initial imaging studies that showed high tumor dissemination with high risk of postoperative comorbidities and poor performance status, or optimal cytoreduction surgery (residual disease measuring 1 cm or less) was unsuitable because of a high tumor burden [predictive index value (PIV) ≥ 8] [15]. For diagnostic laparoscopy, the degree of tumor burden was determined with the PIV [16]. For IDS, all patients underwent surgery with the intent to achieve complete resection with no residual tumor. Standard surgical procedures included hysterectomy, bilateral oophorectomy, omentectomy, pelvic/para-aortic lymph node dissection, and appendectomy. Radical surgery included more aggressive procedures such as liver resection or bowel resection than those who underwent standard surgical procedures [17]. Subsequently, additional cycles of adjuvant chemotherapy were administered to complete a total of six cycles at the discretion of the treating physician. Surgical complexity was classified as low, intermediate, or high [18].
Pathologic review
The resected tissues were formalin-fixed and paraffin-embedded, and stained with hematoxylin and eosin (H&E) in the Department of Pathology, Severance Hospital, Yonsei University College of Medicine. Three expert gynecologic pathologists reviewed all available H&E-stained slides obtained from IDS tissues. They independently scored each slide according to the three-tiered CRS system described by Böhm et al. [5]. Briefly, CRS is defined as follows: CRS 1: No or minimal tumor response; CRS 2: Partial tumor response: CRS 3: Complete or near-complete tumor response.
BRCA testing
From the whole blood samples, genomic DNA was extracted according to the protocol provided by the manufacturer (QIAamp DNA Blood Mini Kit, QIAGEN, USA). To assess the germline mutations in BRCA1 and BRCA2, the entire coding region and intron-exon boundaries of two genes were amplified using polymerase chain reaction (PCR) amplification. We identified all variants using Sanger sequencing on a 3730 DNA Analyzer with the BigDye Terminator v3.1 Cycle Sequencing Kit (Applied Biosystems, Foster City, CA, USA). Sequencing data were aligned against appropriate reference sequences (accession numbers NM_007294 and NM_000059, respectively) and analyzed using the Sequencher 5.3 software (Gene Codes Corp., Ann Arbor, MI, USA). Variations were described following the nomenclature system of the Human Genome Variation Society (http://www.hgvs.org/mutnomen) and the conventional nomenclature system from the Breast Cancer Information Core (BIC; http://research.nhgri.nih.gov/bic/). Pathogenicity interpretation of the variants were performed according to 2015 American College of Medical Genetics and Genomics guideline by professional medical geneticists, using evidences of variant type assessment, population allele frequency, prediction algorithm results, and database search such as Human Gene Mutation Database, ClinVar, and BIC.
Statistical analysis
Descriptive data are reported as the median (range) or frequency (percentage). Categorical variables were compared with the chi-square or continuous variables with the Student’s t-test or Mann-Whitney U test for parametric/non-parametric variables, respectively. Responses were assessed according to the Response Evaluation Criteria in Solid Tumors criteria, version 1.1. We defined PFS as the time from the date of diagnosis to disease progression or death; overall survival (OS) was measured from the date of diagnosis to death or to the date of the last follow-up. Survival analysis was performed using the Kaplan-Meier method with a log-rank test. For all analyses, the significance level was set at 0.05. The statistical analyses were performed with the SPSS statistical software (version 21.0; IBM Corp., Armonk, NY).
Results
Patients’ characteristics
Table 1 contains a comparison of the clinical characteristics between the BRCA wild-type genotype group and the BRCA mutation group. Of the 169 patients included, 122 (71.9%) had the wild-type BRCA genotype, and 47 (28.1%) had the BRCA1/2 mutations. There were no significant between-group differences in patient characteristics such as age, CA-125 level, FIGO stage, histologic type, tumor grade, tumor burden, CRS, residual disease, rate of radical surgery, surgical complexity score, chemotherapy regimen, or cycles of NAC.
Table 1.
Patient and clinical characteristics (N = 169)
| Characteristics | BRCA wild-type (N = 122) | BRCA mutation (N = 47) | P |
|---|---|---|---|
| Age, median (range), years | 57 (32–77) | 56 (27–76) | 0.610 |
| CA-125 level, median (range), U/mL | 1958.7 (94.2.0–21,994.8) | 1711.3 (75.0–23,919.0) | 0.759 |
| FIGO stage, n (%) | |||
| III | 56 (45.9%) | 23 (48.9%) | 0.734 |
| IV | 66 (54.4%) | 24 (51.1%) | |
| Grading | |||
| 1 | 3 (2.5%) | 0 (0%) | 0.489 |
| 2 | 11 (9.0%) | 2 (4.5%) | |
| 3 | 102 (83.6%) | 42 (89.4%) | |
| Not available | 6 (4.9%) | 3 (6.4%) | |
| Tumor burden assessed by diagnostic laparoscopy* | |||
| PIV 8 | 27 (22.1%) | 3 (6.4%) | 0.097 |
| PIV 10 | 25 (20.5%) | 14 (29.8%) | |
| PIV 12 | 10 (8.2%) | 4 (8.5%) | |
| PIV 14 | 5 (4.1%) | 1 (2.1%) | |
| Not available | 55 (45.1%) | 25 (53.2%) | |
| CRS, n (%) | |||
| 1–2 | 79 (64.8%) | 31 (66.0%) | 0.516 |
| 3 | 43 (35.2%) | 16 (34.0%) | |
| Residual disease, n (%) | |||
| No | 62 (50.8%) | 18 (38.3%) | 0.344 |
| Any residual | 58 (47.5%) | 28 (59.6%) | |
| Not available | 2 (1.6%) | 1 (2.1%) | |
| Radical surgery†, n (%) | |||
| None | 59 (48.4%) | 19 (40.4%) | 0.354 |
| Any radical surgery | 63 (51.6%) | 28 (59.6%) | |
| Surgical complexity score groups‡ | |||
| 1–2 (Low/intermediate) | 102 (83.6%) | 37 (78.7%) | 0.457 |
| 8 (High) | 20 (16.4%) | 10 (21.3%) | |
| Chemotherapy regimen, n (%) | |||
| Paclitaxel + carboplatin | 91 (74.6%) | 34 (72.3%) | 0.576 |
| Docetaxel + carboplatin | 8 (6.6%) | 6 (12.8%) | |
| Weekly paclitaxel + carboplatin | 15 (12.3%) | 5 (10.6%) | |
| Paclitaxel + carboplatin + bevacizumab | 8 (6.6%) | 2 (4.3%) | |
* According to Fagotti et al. [15]
† Radical surgery includes any of following: bowel surgery, cholecystectomy, diaphragm peritonectomy/resection, distal pancreatectomy video-assisted thoracoscopic surgery, splenectomy, liver resection, supraclavicular fossa resection, ureter resection, and others
‡ According to Aletti et al. [19]
CA-125, cancer antigen 125; FIGO, International Federation of Gynecology and Obstetrics; HGSC, high-grade serous carcinoma; PIV, predictive index value; CRS, chemotherapy response score
CRS relative to BRCA1/2 mutation status
CRS 3 patients were 43 (35.2%) and 16 (34.0%) for patients without and with BRCA1/2 mutations, respectively (P = 0.516) (Table 2). Although CRS 3 rates differed between BRCA1 (26.9%), BRCA2 (42.9%) and the wild-type BRCA genotype, these difference did not achieve statistical significance.
Table 2.
Chemotherapy response score relative to BRCA1/2 mutation status
| CRS | Wild type | Mutation | Total | P value | |
|---|---|---|---|---|---|
| BRCA1 or 2 | 1–2 | 79 (64.8%) | 31 (66.0%) | 110 (65.1%) | 0.516 |
| 3 | 43 (35.2%) | 16 (34.0%) | 59 (34.9%) | ||
| BRCA1 | 1–2 | 91 (63.6%) | 19 (73.1%) | 110 (65.1%) | 0.243 |
| 3 | 52 (36.6%) | 7 (26.9%) | 59 (34.9%) | ||
| BRCA2 | 1–2 | 98 (66.2%) | 12 (57.1%) | 110 (65.1%) | 0.280 |
| 3 | 50 (33.8%) | 9 (42.9%) | 59 (34.9%) |
CRS, Chemotherapy response score
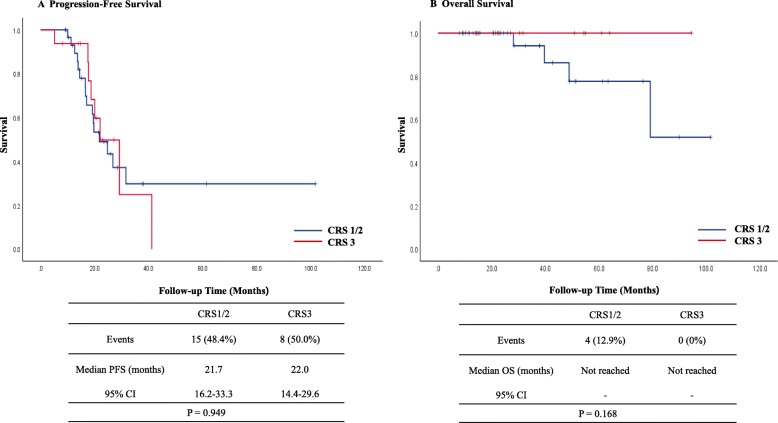
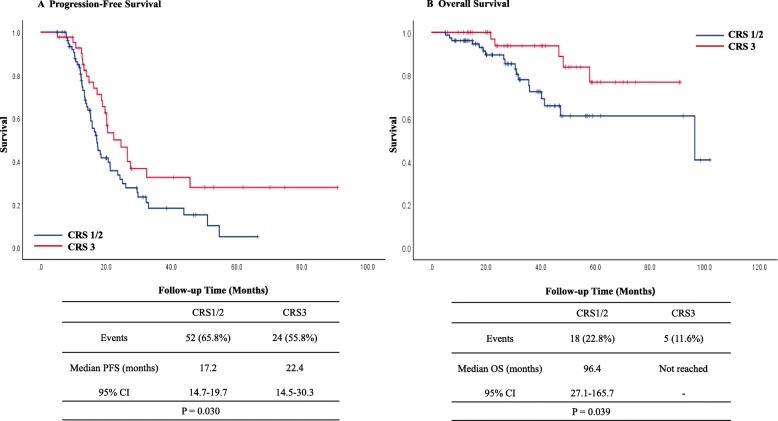
Kaplan–Meier curves for OS and PFS stratified by CRS in patients with the BRCA1/2 mutations are shown in Fig. 2. Fifteen (48.4%) in the CRS 1/2 and 8 (50.0%) in the CRS 3 group had recurred by the time of the analysis. Median PFS in the CRS 1/2 group was 21.7 months (95% confidence interval [CI], 16.2–33.3) and 22.0 months (95% CI, 14.4–29.6) in the CRS 3 group. Four (12.9%) in the CRS1/2 and no patients in the CRS3 group had died by the time of the analysis. Median OS was not reached in both groups. CRS 3 in patients with the BRCA1/2 mutations was not significantly associated with improved PFS (P = 0.949) and OS (P = 0.168). In patients without BRCA mutations, 52 (65.8%) in the CRS 1/2 and 24 (55.8%) in the CRS 3 group had recurred by the time of the analysis. Median PFS in the CRS 1/2 group was 17.2 months (95% CI, 14.7–19.7) and 22.4 months (95% CI, 14.5–30.3). Eighteen (22.8%) in the CRS 1/2 and 5 (11.6%) patients in the CRS 3 group had died by the time of the analysis. Median OS in the CRS 1/2 group was 96.4 months (95% C], 27.1–165.7) and not reached in the CRS 3 group. However, CRS 3 in patients without BRCA mutations was significantly associated with improved PFS (P = 0.030) and OS (P = 0.039) (Fig. 3). The results of the multivariate Cox regression analyses of PFS and OS in all patients are shown in Additional file 1. In terms of recurrence, multivariate analysis showed that BRCA1/2 mutation was a marginally significant prognostic factor (HR, 0.65; 95% CI, 0.40–1.04). Multivariate analysis showed CRS 3 (HR, 0.29; 95% CI, 0.10–0.80) and BRCA1/2 mutation (HR, 0.27; 95% CI, 0.08–0.92) were significantly associated with a longer OS.
Fig. 2.
Kaplan-Meier curves of PFS (a) and OS (b) stratified by CRS in patients with BRCA1/2 mutations. CI, confidence interval; CRS, chemotherapy response score; PFS, progression-free survival; OS, overall survival
Fig. 3.
Kaplan-Meier curves of PFS (a) and OS (b) stratified by CRS in patients without BRCA mutations. CI, confidence interval; CRS, chemotherapy response score; PFS, progression-free survival; OS, overall survival
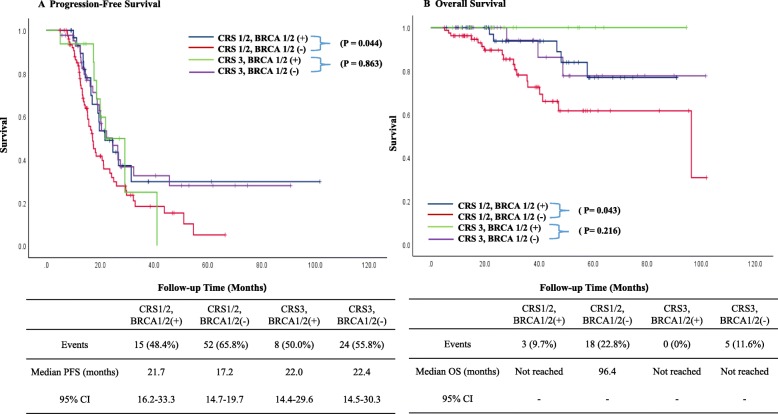
We also categorized the patients based on BRCA mutations and CRS (BRCA1/2 mutations with CRS 1/2; the wild-type BRCA genotype with CRS 1/2; BRCA1/2 mutations with CRS 3; and the wild-type BRCA genotype with CRS 3) to evaluate survival according to the relationship of BRCA1/2 mutations in the CRS. Fifteen (48.4%) in BRCA1/2 mutations with CRS1/2, 52 (65.8%) in the wild-type BRCA genotype with CRS1/2, 8 (50%) in BRCA1/2 mutations with CRS3, and 24 (55.8%) in the wild-type BRCA genotype with CRS3 group had recurred by the time of the analysis. Median PFS in 4 groups were 21.7 (95% CI, 16.2–33.3), 17.2 (95% CI, 14.7–19.7), 22.0 (95% CI, 14.4–29.6), and 22.4 (95% CI, 14.5–30.3), respectively. Three (9.7%) in BRCA1/2 mutations with CRS1/2, 18 (22.8%) in the wild-type BRCA genotype with CRS1/2, 0 (0%) in BRCA1/2 mutations with CRS3, and 5 (11.6%) in the wild-type BRCA genotype with CRS3 group had died by the time of the analysis. Median OS in the BRCA1/2 mutations with CRS3 group was 96.4 and other 3 groups were not reached. In patients with CRS 1/2, the carriers of BRCA1/2 mutations had better PFS (P = 0.044) and OS (P = 0.043) than the wild-type BRCA genotype patients. However, in patients with CRS 3, there was no significant difference in PFS (P = 0.863) and OS (P = 0.216) between BRCA1/2 carriers and the wild-type BRCA genotype patients (Fig. 4). In addition, we performed a subset analysis including only in Grade 3 patients excluding the 16 patients with Grade1 or 2. Similar results were obtained for patients with Grade 3 (Additional file 2). In patients with CRS 1/2, the carriers of BRCA1/2 mutations had better PFS (P = 0.015) and OS (P = 0.049) than the wild-type BRCA genotype patients. However, in patients with CRS 3, there was no significant difference in PFS (P = 0.917) and OS (P = 0.389) between BRCA1/2 carriers and the wild-type BRCA genotype patients.
Fig. 4.
Kaplan-Meier curves of PFS (a) and OS (b) stratified by BRCA mutations and CRS. CI, confidence interval; CRS, chemotherapy response score; PFS, progression-free survival; OS, overall survival
Discussion
In this study, we evaluated the relationship between BRCA1/2 mutations and CRS and survival outcomes in advanced-stage ovarian cancer patients treated with NAC followed by IDS. The patients with BRCA1/2 mutations did not show higher CRS rates than patients without these mutations. In patients without the BRCA1/2 mutations, the CRS 3 patients showed superior survival outcomes compared to the patients with CRS 1/2. In addition, in the CRS 1/2 patient group, the survival outcomes of the BRCA1/2 carriers were superior to those of the wild-type BRCA genotype patients. In the BRCA wild-type group, patients who achieved CRS 1/2 after NAC had a poor prognoses compared to the patients with CRS 3. Therefore, patients with the BRCA wild-type should be considered for additional treatments to achieve CRS 3 after NAC, such as adding a bevacizumab or immune checkpoint inhibitors to platinum-based NAC. In addition, BRCA wild-type patients with CRS 1/2 after platinum-based NAC expected to have a poor prognosis due to residual tumors after NAC that may be resistant to platinum-based NAC if they receive the same NAC regimen after IDS. To improve the survival of the BRCA wild-type patients with CRS 1/2, the genomic profiles of the post-NAC tissues should be evaluated to identify biomarkers and to select targeted therapies [19].
Response rates to platinum-based NAC predict survival and may be regarded as a surrogate prognostic marker [5, 6]. A three-tiered CRS system showed a significant association with survival outcomes. The CRS system for assessing platinum-based NAC response rates can be a reproducible prognostic tool, and the incorporation of the CRS system after NAC can help determination of adjuvant treatment in advanced-stage ovarian cancer patients. Previous studies [10–12] showed that advanced-stage ovarian cancer patients with BRCA1/2 mutations tend to have higher response rates to platinum-based chemotherapy, longer PFS, and a higher benefit from NAC. The BRCA1/2 mutations are also being considered as specific targets. Recent randomized studies on poly (adenosine diphosphate–ribose) polymerase inhibitors have demonstrated a substantial survival benefit in BRCA1/2 carriers [20–24], hence germline BRCA1/2 testing is becoming a mandatory in treatment decisions in advanced-stage ovarian cancer.
In triple-negative breast cancer, several studies have shown that in the relationships between germline BRCA1/2 mutations, response rates, and prognoses. In patients with triple-negative breast cancer, BRCA1/2 mutation patients had higher pCR rates than those with BRCA wild-type patients. However, BRCA mutation patients do not benefit as much from a pCR compared with patients without BRCA mutation. In ovarian cancer patients, no such studies have yet been reported. Hahnen et al. [13] showed that triple-negative breast cancer patients without germline BRCA1/2 mutations benefit from the addition of carboplatin and that BRCA1/2 mutation carriers had superior response rates. Fasching et al. [14] showed the effect of BRCA1/2 mutations in the NAC of triple-negative breast cancer. Patients with BRCA1 or BRCA2 mutations had higher pCR rates than patients without a mutation. However, BRCA1/2 mutation patients who receive standard treatment do not benefit as much from a pCR as patients with the wild-type BRCA. These results were similar to our study.
Our study showed that patients with BRCA1/2 mutations enjoyed a good survival outcome regardless of their CRS. In contrast, CRS 3 had a significant survival benefit on PFS and OS for wild-type BRCA genotype patients. In addition, the BRCA1/2 mutations had a significant influence on survival in the CRS 1/2 patient group. One plausible explanation for the absence of the effect of CRS 3 on the prognoses for patients with the BRCA1/2 mutations is the influence of the platinum-based adjuvant treatment after IDS. Although the CRS 1/2 group of patients was expected to have a poor prognosis, their prospects were improved if they had the BRCA1/2 mutations because of their conferred sensitivity to platinum-based adjuvant chemotherapy after IDS. The mechanism of action by platinum drugs is mediated by the formation of the covalent binding of platinum to DNA. This binding interferes with DNA synthesis and ultimately leads to cell death [25]. It seems likely that partially formed covalent bindings cause replication of fork stalling when it is encountered by the DNA replication machinery during the S phase. These stalled replication forks may degenerate into double-stranded DNA breaks [26] in which tumor cells with defects in their DNA repair pathways achieves increased response rates against platinum drugs, as investigated in previous studies [27–30].
However, unlike in breast cancer studies, the status of BRCA1/2 mutations in our study was unrelated to CRS. In previous studies [31, 32], patients with germline BRCA1/2 mutations were associated with wider disease diffusion than BRCA wild-type patients in terms of peritoneal spread and incidence of bulky lymph nodes. Furthermore, Soslow et al. [33] showed the correlations between the genotype and characteristic morphologic appearance of ovarian cancer. The BRCA1 mutation group had more tumor-infiltrating lymphocytes, thus suggesting that the status of BRCA mutations could influence the immunological microenvironment sufficiently to eventually drive the specific characteristics of disease presentation. Therefore, BRCA1/2 mutation carriers may have a lower CRS following NAC as compared to BRCA wild-type patients.
The main limitation of our study was its low sample size and the small number of patients with BRCA1/2 mutations. Although 169 patients were genotyped, there were only 47 carriers of these mutations. Second, considering the family history of patients who were diagnosed with ovarian cancer before 2017, the germline BRCA test was recommended for patients with a high probability of being a BRCA1/2 mutation carrier. Olaparib treatment in the maintenance setting has been covered by Korean National Health Insurance since 2017, we have been routinely offered the germline BRCA test in patients diagnosed with high-grade serous ovarian cancer. In addition, because 92 people did not receive BRCA test during the study period, a selection bias may have influenced the outcomes. Third, NAC was only incorporated into our institution in late 2010; thus, our cohort was limited by the short follow-up period. Fourth, the type of NAC is important because CRS is affected by the response to chemotherapy. About 75% of patients received paclitaxel and carboplatin combination chemotherapy in our study, an analysis of the relationship between CRS and the type of NAC could not be conducted. \.
Conclusion
In conclusion, in advanced-stage ovarian cancer patients treated with NAC followed by IDS, CRS 3 was not associated with increased survival for BRCA1/2 mutation carriers than for patients without these mutations. Additional studies are needed to elucidate the effect of CRS on prognoses in advanced-stage ovarian cancer patients with and without BRCA1/2 mutations.
Supplementary information
Additional file 1. Multivariate analyses for progression-free and overall survival using a Cox proportional hazards model.
Acknowledgments
None.
Abbreviations
- CRS
Chemotherapy response scores
- IDS
Interval debulking surgery
- NAC
Neoadjuvant chemotherapy
- OS
Overall survival
- pCR
Pathologic complete response
- PCR
Polymerase chain reaction
- PFS
Progression-free survival
- PIV
Predictive index value
Author contributions
Conceptualization: L.Y.J., L.J.Y., K.S.H.; Methodology: L.Y.J., L.J.Y.; Validation: L.Y.J.; Formal analysis and investigation: L.Y.J.; Resources and data curation: L.Y.J., K.H.S., R.J.H; Writing - original draft preparation: L.Y.J.; Writing - review and editing: L.J.Y., N.E.J.; Supervision: N.E.J., K.S.W., K.Y.T.; Project administration: L.Y.J., L.J.Y.; Funding acquisition: L.J.Y. All authors have read and approved the manuscript.
Funding
This study was supported by a faculty research grant of Yonsei University College of Medicine for 6–2018-0169. Research grants are administered by the Ministry of Science, ICT & Future Planning (2017M3A9E8029714). This funding source had no role in study design, data collection and analysis, and interpretation of data and in writing the manuscript.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The need for an approval was waived by the ‘Institutional Review Board of Severance Hospital at Yonsei University College of Medicine’ as the study was retrospective and individual patients were not identifiable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12885-020-6688-8.
References
- 1.Onda T, Matsumoto K, Shibata T, Sato A, Fukuda H, Konishi I, Kamura T, Yoshikawa H. Phase III trial of upfront debulking surgery versus neoadjuvant chemotherapy for stage III/IV ovarian, tubal and peritoneal cancers: Japan clinical oncology group study JCOG0602. Jpn J Clin Oncol. 2008;38(1):74–77. doi: 10.1093/jjco/hym145. [DOI] [PubMed] [Google Scholar]
- 2.Vergote I, Trope CG, Amant F, Kristensen GB, Ehlen T, Johnson N, Verheijen RH, van der Burg ME, Lacave AJ, Panici PB, et al. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. N Engl J Med. 2010;363(10):943–953. doi: 10.1056/NEJMoa0908806. [DOI] [PubMed] [Google Scholar]
- 3.Kehoe S, Hook J, Nankivell M, Jayson GC, Kitchener H, Lopes T, Luesley D, Perren T, Bannoo S, Mascarenhas M, et al. Primary chemotherapy versus primary surgery for newly diagnosed advanced ovarian cancer (CHORUS): an open-label, randomised, controlled, non-inferiority trial. Lancet. 2015;386(9990):249–257. doi: 10.1016/S0140-6736(14)62223-6. [DOI] [PubMed] [Google Scholar]
- 4.Fagotti A, Ferrandina G, Vizzielli G, Fanfani F, Gallotta V, Chiantera V, Costantini B, Margariti PA, Gueli Alletti S, Cosentino F, et al. Phase III randomised clinical trial comparing primary surgery versus neoadjuvant chemotherapy in advanced epithelial ovarian cancer with high tumour load (SCORPION trial): final analysis of peri-operative outcome. Eur J Cancer. 2016;59:22–33. doi: 10.1016/j.ejca.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 5.Bohm S, Faruqi A, Said I, Lockley M, Brockbank E, Jeyarajah A, Fitzpatrick A, Ennis D, Dowe T, Santos JL, et al. Chemotherapy response score: development and validation of a system to quantify Histopathologic response to Neoadjuvant chemotherapy in Tubo-ovarian high-grade serous carcinoma. J Clin Oncol. 2015;33(22):2457–2463. doi: 10.1200/JCO.2014.60.5212. [DOI] [PubMed] [Google Scholar]
- 6.Lee JY, Chung YS, Na K, Kim HM, Park CK. External validation of chemotherapy response score system for histopathological assessment of tumor regression after neoadjuvant chemotherapy in tubo-ovarian high-grade serous carcinoma 2017; 10.3802/jgo.2017.28.e73. [DOI] [PMC free article] [PubMed]
- 7.Antoniou A, Pharoah PD, Narod S, Risch HA, Eyfjord JE, Hopper JL, Loman N, Olsson H, Johannsson O, Borg A, et al. Average risks of breast and ovarian cancer associated with BRCA1 or BRCA2 mutations detected in case series unselected for family history: a combined analysis of 22 studies. Am J Hum Genet. 2003;72(5):1117–1130. doi: 10.1086/375033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen S, Parmigiani G. Meta-analysis of BRCA1 and BRCA2 penetrance. J Clin Oncol. 2007;25(11):1329–1333. doi: 10.1200/JCO.2006.09.1066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang YW. Association of BRCA1/2 mutations with ovarian cancer prognosis: an updated meta-analysis. Medicine (Baltimore) 2018;97(2):e9380. doi: 10.1097/MD.0000000000009380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alsop K, Fereday S, Meldrum C, de Fazio a, Emmanuel C, George J, Dobrovic a, Birrer MJ, Webb PM, Stewart C, et al. BRCA mutation frequency and patterns of treatment response in BRCA mutation-positive women with ovarian cancer: a report from the Australian ovarian Cancer study group. J Clin Oncol. 2012;30(21):2654–2663. doi: 10.1200/JCO.2011.39.8545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mahdi H, Gockley A, Esselen K, Marquard J, Nutter B, Yang B, Hinchcliff E, Horowitz N, Rose PG. Outcome of neoadjuvant chemotherapy in BRCA1/2 mutation positive women with advanced-stage Mullerian cancer. Gynecol Oncol. 2015;139(3):407–412. doi: 10.1016/j.ygyno.2015.07.101. [DOI] [PubMed] [Google Scholar]
- 12.Gorodnova TV, Sokolenko AP, Ivantsov AO, Iyevleva AG, Suspitsin EN, Aleksakhina SN, Yanus GA, Togo AV, Maximov SY, Imyanitov EN. High response rates to neoadjuvant platinum-based therapy in ovarian cancer patients carrying germ-line BRCA mutation. Cancer Lett. 2015;369(2):363–367. doi: 10.1016/j.canlet.2015.08.028. [DOI] [PubMed] [Google Scholar]
- 13.Hahnen E, Lederer B, Hauke J, Loibl S, Krober S, Schneeweiss A, Denkert C, Fasching PA, Blohmer JU, Jackisch C, et al. Germline mutation status, pathological complete response, and disease-free survival in triple-negative breast Cancer: secondary analysis of the GeparSixto randomized clinical trial. JAMA Oncol. 2017;3(10):1378–1385. doi: 10.1001/jamaoncol.2017.1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fasching PA, Loibl S, Hu C, Hart SN, Shimelis H, Moore R, Schem C, Tesch H, Untch M, Hilfrich J, et al. BRCA1/2 mutations and Bevacizumab in the Neoadjuvant treatment of breast Cancer: response and prognosis results in patients with triple-negative breast Cancer from the GeparQuinto study. J Clin Oncol. 2018;36(22):2281–2287. doi: 10.1200/JCO.2017.77.2285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee YJ, Lee JY, Cho MS, Nam EJ, Kim SW, Kim S, Kim YT. Incorporation of paclitaxel-based hyperthermic intraperitoneal chemotherapy in patients with advanced-stage ovarian cancer treated with neoadjuvant chemotherapy followed by interval debulking surgery: a protocol-based pilot study. J Gynecol Oncol. 2019;30(1):e3. doi: 10.3802/jgo.2019.30.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fagotti A, Ferrandina G, Fanfani F, Garganese G, Vizzielli G, Carone V, Salerno MG, Scambia G. Prospective validation of a laparoscopic predictive model for optimal cytoreduction in advanced ovarian carcinoma. Am J Obstet Gynecol. 2008;199(6):642.e1–642.e6. doi: 10.1016/j.ajog.2008.06.052. [DOI] [PubMed] [Google Scholar]
- 17.Lee YJ, Chung YS, Lee JY, Nam EJ, Kim SW, Kim S, Kim YT. Impact of the time interval from completion of neoadjuvant chemotherapy to initiation of postoperative adjuvant chemotherapy on the survival of patients with advanced ovarian cancer. Gynecol Oncol. 2018;148(1):62–67. doi: 10.1016/j.ygyno.2017.11.023. [DOI] [PubMed] [Google Scholar]
- 18.Aletti GD, Eisenhauer EL, Santillan A, Axtell A, Aletti G, Holschneider C, Chi DS, Bristow RE, Cliby WA. Identification of patient groups at highest risk from traditional approach to ovarian cancer treatment. Gynecol Oncol. 2011;120(1):23–28. doi: 10.1016/j.ygyno.2010.09.010. [DOI] [PubMed] [Google Scholar]
- 19.Lee YJ, Kim D, Shim JE, Bae SJ, Jung YJ, Kim S, Lee H, Kim SH, Jo SB, Lee JY, et al. Genomic profiling of the residual disease of advanced high-grade serous ovarian cancer after neoadjuvant chemotherapy. Int J Cancer. 2020;146(7):1851–1861. doi: 10.1002/ijc.32729. [DOI] [PubMed] [Google Scholar]
- 20.Coleman RL, Oza AM, Lorusso D, Aghajanian C, Oaknin A, Dean A, Colombo N, Weberpals JI, Clamp A, Scambia G, et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390(10106):1949–1961. doi: 10.1016/S0140-6736(17)32440-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaufman B, Shapira-Frommer R, Schmutzler RK, Audeh MW, Friedlander M, Balmana J, Mitchell G, Fried G, Stemmer SM, Hubert A, et al. Olaparib monotherapy in patients with advanced cancer and a germline BRCA1/2 mutation. J Clin Oncol. 2015;33(3):244–250. doi: 10.1200/JCO.2014.56.2728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ledermann J, Harter P, Gourley C, Friedlander M, Vergote I, Rustin G, Scott CL, Meier W, Shapira-Frommer R, Safra T, et al. Olaparib maintenance therapy in patients with platinum-sensitive relapsed serous ovarian cancer: a preplanned retrospective analysis of outcomes by BRCA status in a randomised phase 2 trial. Lancet Oncol. 2014;15(8):852–861. doi: 10.1016/S1470-2045(14)70228-1. [DOI] [PubMed] [Google Scholar]
- 23.Mirza MR, Monk BJ, Herrstedt J, Oza AM, Mahner S, Redondo A, Fabbro M, Ledermann JA, Lorusso D, Vergote I, et al. Niraparib maintenance therapy in platinum-sensitive, recurrent ovarian Cancer. N Engl J Med. 2016;375(22):2154–2164. doi: 10.1056/NEJMoa1611310. [DOI] [PubMed] [Google Scholar]
- 24.Moore K, Colombo N, Scambia G, Kim BG, Oaknin A, Friedlander M, Lisyanskaya A, Floquet A, Leary A, Sonke GS, et al. Maintenance Olaparib in patients with newly diagnosed advanced ovarian Cancer. N Engl J Med. 2018. 10.1056/NEJMoa1810858. [DOI] [PubMed]
- 25.Nafisi S, Norouzi Z. A comparative study on the interaction of cis- and trans-platin with DNA and RNA. DNA Cell Biol. 2009;28(9):469–477. doi: 10.1089/dna.2009.0894. [DOI] [PubMed] [Google Scholar]
- 26.Lord CJ, Garrett MD, Ashworth A. Targeting the double-strand DNA break repair pathway as a therapeutic strategy. Clin Cancer Res. 2006;12(15):4463–4468. doi: 10.1158/1078-0432.CCR-06-1269. [DOI] [PubMed] [Google Scholar]
- 27.Sirohi B, Arnedos M, Popat S, Ashley S, Nerurkar A, Walsh G, Johnston S, Smith IE. Platinum-based chemotherapy in triple-negative breast cancer. Ann Oncol. 2008;19(11):1847–1852. doi: 10.1093/annonc/mdn395. [DOI] [PubMed] [Google Scholar]
- 28.Beheshti F, Hassanian SM, Khazaei M, Hosseini M, ShahidSales S, Hasanzadeh M, Maftouh M, Ferns GA, Avan A. Genetic variation in the DNA repair pathway as a potential determinant of response to platinum-based chemotherapy in breast cancer. J Cell Physiol. 2018;233(4):2752–2758. doi: 10.1002/jcp.26091. [DOI] [PubMed] [Google Scholar]
- 29.Zhao EY, Shen Y, Pleasance E, Kasaian K, Leelakumari S, Jones M, Bose P, Ch'ng C, Reisle C, Eirew P, et al. Homologous recombination deficiency and platinum-based therapy outcomes in advanced breast Cancer. Clin Cancer Res. 2017;23(24):7521–7530. doi: 10.1158/1078-0432.CCR-17-1941. [DOI] [PubMed] [Google Scholar]
- 30.Arun B, Bayraktar S, Liu DD, Gutierrez Barrera AM, Atchley D, Pusztai L, Litton JK, Valero V, Meric-Bernstam F, Hortobagyi GN, et al. Response to neoadjuvant systemic therapy for breast cancer in BRCA mutation carriers and noncarriers: a single-institution experience. J Clin Oncol. 2011;29(28):3739–3746. doi: 10.1200/JCO.2011.35.2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gourley C, Michie CO, Roxburgh P, Yap TA, Harden S, Paul J, Ragupathy K, Todd R, Petty R, Reed N, et al. Increased incidence of visceral metastases in Scottish patients with BRCA1/2-defective ovarian Cancer: an extension of the ovarian BRCAness phenotype. J Clin Oncol. 2010;28(15):2505–2511. doi: 10.1200/JCO.2009.25.1082. [DOI] [PubMed] [Google Scholar]
- 32.Petrillo M, Marchetti C, De Leo R, Musella A, Capoluongo E, Paris I, Benedetti Panici P, Scambia G, Fagotti A. BRCA mutational status, initial disease presentation, and clinical outcome in high-grade serous advanced ovarian cancer: a multicenter study. Am J Obstet Gynecol. 2017;217(3):334.e1–334.e9. doi: 10.1016/j.ajog.2017.05.036. [DOI] [PubMed] [Google Scholar]
- 33.Soslow RA, Han G, Park KJ, Garg K, Olvera N, Spriggs DR, Kauff ND, Levine DA. Morphologic patterns associated with BRCA1 and BRCA2 genotype in ovarian carcinoma. Mod Pathol. 2012;25(4):625–636. doi: 10.1038/modpathol.2011.183. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Multivariate analyses for progression-free and overall survival using a Cox proportional hazards model.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.