Abstract
Background
Scotland has three prehospital critical care teams (PHCCTs) providing enhanced care support to a usually paramedic-delivered ambulance service. The effect of the PHCCTs on patient survival following trauma in Scotland is not currently known nationally.
Methods
National registry-based retrospective cohort study using 2011–2016 data from the Scottish Trauma Audit Group. 30-day mortality was compared between groups after multivariate analysis to account for confounding variables.
Results
Our data set comprised 17 157 patients, with a mean age of 54.7 years and 8206 (57.5%) of male gender. 2877 patients in the registry were excluded due to incomplete data on their level of prehospital care, leaving an eligible group of 14 280. 13 504 injured adults who received care from ambulance clinicians (paramedics or technicians) were compared with 776 whose care included input from a PHCCT. The median Injury Severity Score (ISS) across all eligible patients was 9; 3076 patients (21.5%) met the ISS>15 criterion for major trauma. Patients in the PHCCT cohort were statistically significantly (all p<0.01) more likely to be male; be transported to a prospective Major Trauma Centre; have suffered major trauma; have suffered a severe head injury; be transported by air and be intubated prior to arrival in hospital. Following multivariate analysis, the OR for 30-day mortality for patients seen by a PHCCT was 0.56 (95% CI 0.36 to 0.86, p=0.01).
Conclusion
Prehospital care provided by a physician-led critical care team was associated with an increased chance of survival at 30 days when compared with care provided by ambulance clinicians.
Keywords: pre-hospital; trauma; prehospital care; prehospital care, doctors in PHC; prehospital care, critical care transport
Key messages.
What is already known on this subject
Targeted prehospital critical care has been widely adopted as part of many Emergency Medical Services (EMS) systems worldwide. There are several studies suggesting that physician-led prehospital critical care is associated with an outcome benefit for trauma patients.
There is however no definitive evidence of benefit, particularly in the UK.
What this study adds
When trauma patients in Scotland are treated in the prehospital environment by paramedics assisted by a critical care team, versus paramedics providing sole care, patients have a higher chance of survival at 30 days following hospital admission.
Introduction
Trauma results in considerable morbidity and mortality throughout the world.1 The quality of care given to patients before they reach hospital has a critical effect on their chances of survival.2 Trauma remains a leading cause of morbidity and mortality among people under 40 years and the standard of prehospital care they receive has significant effects on their future quality of life and functional ability.3 In the UK, and most of the developed world, prehospital care for major trauma patients is routinely delivered by emergency medical technicians and paramedics. The skillset and current scope of practice of these clinicians, however, limits the range of life-saving interventions which can be given to the patient before they reach hospital.4
A UK-wide report, Trauma: Who Cares? 5 published in 2007 showed that a significant number of seriously injured patients in the UK died due to limitations in their care before they reached hospital. Principally, these deaths were from airway obstruction, chest injuries and hypovolaemic shock, suggesting that ambulance clinicians’ existing capabilities do not always meet the needs of severely injured adult patients. Paramedics in Scotland have a low exposure to minor/moderate and major trauma patients, the latter equating to 0.3% of annual incident volume (personal communication, Sinclair 2019). In addition to this, the vast majority of paramedics in Scotland do not have enhanced critical care skills, leading to potential challenges in treating the most critically injured patients independently.
Scotland’s population of 5.4 million people is served by a single statutory ambulance provider—the Scottish Ambulance Service—covering a mixed urban and rural population. Like other parts of the UK, specialist prehospital critical care teams (PHCCTs) are deployed to incident scenes where patients are thought to have sustained serious injuries. The teams have high levels of experience in trauma management and also have extended skills in patient assessment and treatment. These capabilities include prehospital emergency anaesthesia (PHEA), advanced analgesia and sedation, open/tube thoracostomy, thoracotomy, resuscitative hysterotomy and surgical cricothyroidotomy.
Scotland has three PHCCTs: Medic 1 (based in Edinburgh) and the Tayside Trauma Team (Dundee) respond by road from ED, while the Emergency Medical Retrieval Service (Glasgow) responds by both land and air. All teams are staffed by a doctor, who is a consultant or senior registrar in a critical care specialty, accompanied by a nurse or paramedic with extended skills in trauma and critical care. They may have additional staff members present for supervision and/or training purposes. During the period studied, the Emergency Medical Retrieval Service was available to respond immediately 0800–1800 every day, with a longer response time overnight. The other two teams are both essentially available at any time as they deploy staff directly from an ED.
Unlike many other parts of the UK, Scotland’s air ambulance provision is not directly linked with the availability of a critical care team. During the study period, two of the three rotary air ambulances (in Inverness and Perth) were staffed by a paramedic-only crew for primary missions. The third, in Glasgow, was staffed by paramedics 24/7, with a critical care team from the Emergency Medical Retrieval Service available on base to augment this level of care from 0800 to 1800, and available on call from home outwith these hours, but only called in for prolonged entrapment or other cases where the timescale made this worthwhile.
In more rural areas, the Scottish Ambulance Service’s response may be augmented by voluntary responder schemes such as those of BASICS (the British Association for Immediate Care) Scotland, meaning that some patients will be seen by a non-critical care doctor (often a local General Practitioner) or nurse in addition to standard (non-PHCCT) ambulance care.
Specialist PHCCTs are scarce and expensive, so the effects of their interventions should be robustly assessed. Evidence to support the postulated benefits of their attendance, compared with an ambulance clinician response, is not completely established, and the relative lack of high-quality evidence in the field was reinforced by the inclusion of this research topic in a list of the top five prehospital research priorities agreed by a European collaboration in 2011.6 We aimed to use national trauma registry data to assess the association between mortality and the presence of a PHCCT in severely injured adult patients.
Methods
Data set
We performed a secondary analysis of data from a routinely collected national trauma registry, covering the six calendar years 2011–2016. The Scottish Trauma Audit Group (STAG) is part of the Information Services Division of NHS Scotland. As part of an ongoing national project, trauma patients admitted to any of the 25 major hospitals in Scotland are eligible for inclusion in STAG’s data collection. The usual inclusion criterion is a stay in hospital of 3 days or more, although any patients who die during their admission, or are initially managed in the resuscitation area of an ED, are included regardless. A comprehensive list of inclusion and exclusion criteria is included in online supplementary appendix A (a supplementary file which is only available online).
emermed-2019-208458supp001.pdf (62.9KB, pdf)
Patients’ injuries were graded using Abbreviated Injury Scale (AIS) 2005 descriptors7 and these gradings used to calculate Injury Severity Scores (ISS)8 for all patients. Data were then entered onto a computer database.
Data validation
Prior to data extraction, the primary database underwent a quality assurance process to ensure the validity of data. Each individual patient record was checked against possible queries including impossible values and logic flaws between connected data fields. If the electronic record flagged one of these queries, then the electronic record was cross-referenced against the original paper collection form. For this study, the data set was limited to patients over the age of 16 years, as we only wished to investigate adult patients.
Data extraction
Data for each patient included age, gender and ISS. It also indicated whether a physician had attended the accident scene, whether that physician was from one of the three critical care teams and whether the patient had been intubated. The data do not differentiate between patients intubated, without drugs, by paramedics and those who received PHEA from a PHCCT.
Data definitions
PHCCT attended patients—this was defined as the attendance of one of the SAS supported PHCCTs at a trauma patient during their prehospital care, and subsequent PHCCT escort to destination. Patients were included regardless of whether any PHCCT intervention was delivered. Any other medical, paramedical or nursing attendance prior to hospital arrival, without PHCCT’s presence, was classified as routine care.
Major trauma—injuries comprising an ISS8 of greater than 15.
Severe head injury—any injury in head or face region with AIS of 3 or greater.
Prospective Major Trauma Centre (MTC)—during the study period, there were no designated MTCs officially operating. However, the Scottish Trauma Network was under development during the study period and four centres were provisionally designated to become an MTC. All four are tertiary university hospitals with onsite neurosurgical capability.
Scottish Index of Multiple Deprivation9—SIMD is made of 19 component indicators from across seven domains: income, access, education, housing, crime, employment and health.
30-day mortality status—this was determined by whether the patient was alive or dead exactly 30 days after their trauma incident using data from the National Records of Scotland.
Outcome measure
The primary outcome measure was 30-day mortality.
Statistical analysis
The differences between the PHCCT and non-PHCCT groups were initially assessed using t-tests for continuous variables and proportion tests for categorical variables. The t-tests assume unequal variance.
Given the binary primary outcome variable, logistic regression was used as the modelling approach. This method has been used previously for trauma data as well as for the Trauma Audit and Research Network (TARN) and Trauma and Injury Severity Score (TRISS) models. The covariates included in the analysis were PHCCT, gender, age, ISS, GCS, prehospital intubation, mode of transport to hospital, MTC care, severe head injury and social deprivation (as measured by SIMD quintile). GCS was categorised into five groups and an age–gender interaction term was also included. The significance level was 0.05 (equivalent to 95% CI).
Past research has noted that age and ISS typically exhibit a non-linear relationship with trauma mortality and, in anticipation of this occurring in our analysis, the logistic regression model was extended from a generalised linear model to a generalised additive model or GAM,10 11 which allows for non-linear forms of covariates. Many studies avoid addressing non-linearity in continuous variables by simply categorising the values into distinct groups. However, this approach discards information and the groupings are usually arbitrary. Fractional polynomials for age and injury severity can be used12 13 but GAMs are more flexible and data-driven.
We used a Microsoft Excel spreadsheet to collate all data, and processed them using R14 and its add-on ‘mgcv’ package11 for GAM fitting.
Patient and public involvement
Patients and the public had no input into decisions regarding the research question, outcome measures, study design or recruitment to (or conduct of) the study. Patients and the public were not asked to assess the burden of the intervention, or time required to participate in the research. However, as this study retrospectively examined existing practice, there was no change to the existing care received, or its duration, for those who were studied.
Patients and the public were not involved in our plans to disseminate the study results to participants and relevant wider patient communities. However, anyone who wishes to read our work will be able to do so free of charge via Open Access.
Results
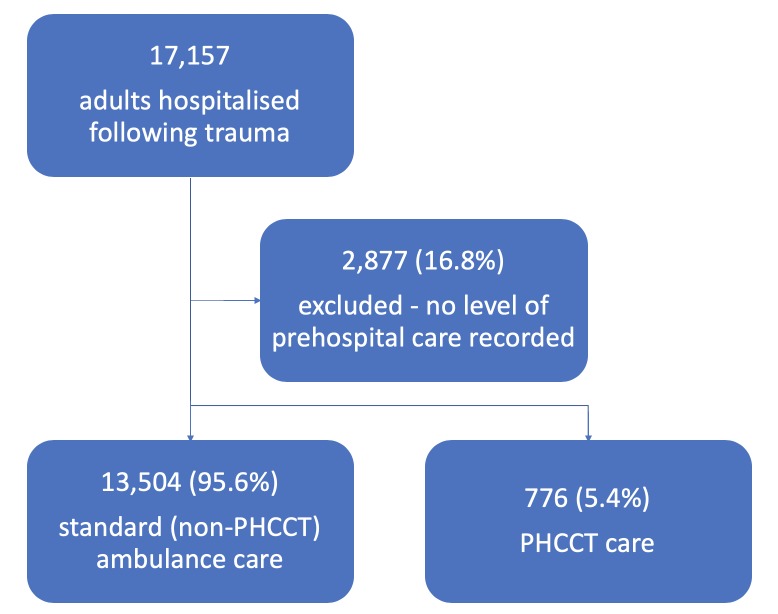
There were 17 157 patients (between 1 January 2011 and 31 December 2016) in the data set who were eligible for analysis. Of these 17 157 patients, 776 (4.5%) saw a PHCCT and 13 504 (78.7%) saw other healthcare personnel—usually a paramedic team, but potentially a nurse or non-PHCCT physician. No level of care information was available for the remaining 2877 (16.8%) patients. These were not included in the analysis, leaving 14 280 with complete data (figure 1).
Figure 1.
STROBE patient flow diagram. PHCCT, prehospital critical care team; STROBE, Strengthening the Reporting of Observational Studies in Epidemiology.
Patient characteristics dependent on whether PHCCTs were present are shown in table 1a and b.
Table 1a.
Summary of other key categorical variables and PHCCT attendance (yes/no)
| Variable | Category | PHCCT | Non-PHCCT | ||
| N | % | N | % | ||
| Gender | Male | 565 | 72.8 | 7641 | 56.6 |
| Female | 211 | 27.2 | 5863 | 43.4 | |
| Patient taken to prospective Major Trauma Centre (MTC) | Yes | 595 | 76.7 | 4421 | 32.7 |
| No | 181 | 23.3 | 9083 | 67.3 | |
| Mode of transport to hospital | Land ambulance | 569 | 73.3 | 13 288 | 98.4 |
| Air ambulance | 207 | 26.7 | 216 | 1.6 | |
| Severe head injury | Yes | 194 | 25.0 | 2354 | 17.4 |
| No | 582 | 75.0 | 11 150 | 82.6 | |
| Prehospital intubation | Yes | 212 | 27.3 | 109 | 0.8 |
| No | 564 | 72.7 | 13 395 | 99.2 | |
| Major trauma (Injury Severity Score: ISS >15) | Yes | 444 | 57.2 | 2632 | 19.5 |
| No | 332 | 42.8 | 10 872 | 80.5 | |
| Scottish Index of Multiple Deprivation (SIMD) Quintile | 1 (most deprived) | 164 | 21.1 | 3644 | 27.0 |
| 2 | 128 | 16.5 | 2729 | 20.2 | |
| 3 | 143 | 18.4 | 2153 | 15.9 | |
| 4 | 115 | 14.8 | 1903 | 14.1 | |
| 5 (least deprived) | 102 | 13.1 | 1615 | 12.0 | |
| Unknown | 124 | 16.0 | 1460 | 10.8 | |
PHCCT, prehospital critical care team.
Table 1b.
Summary of other key continuous variables and PHCCT attendance at scene (yes/no)
| Variable | PHCCT | Non-PHCCT | ||||||
| Min. | Median | Mean | Max. | Min. | Median | Mean | Max. | |
| Age (years) | 16 | 45 | 45.4 | 95 | 16 | 56 | 55.3 | 103 |
| Injury Severity Score (ISS) | 4 | 17 | 20.9 | 75 | 1 | 9 | 11.5 | 75 |
| GCS | 3 | 14 | 11.9 | 15 | 3 | 15 | 14.1 | 15 |
ISS, Injury Severity Score; PHCCT, prehospital critical care team.
Of note, 5.4% of patients were attended by a PHCCT. The crude mortality rate is higher in the PHCCT group (14.8%) than the non-PHCCT group (6.5%).
Prehospital time is poorly recorded in the data we received from STAG, with 55% of PHCCT cases and 18% of non-PHCCT cases missing data on this variable. When considering cases where prehospital time is recorded, PHCCT patients did tend to have a longer prehospital time, by approximately 21–22 (mean 83.4 vs 64.6; median 77.1 vs 55.0) min. The significant lack of completeness of the time data means it is not a robust variable and we therefore excluded it from further analysis.
Univariate analysis
To assess the statistical significance of the differences between the PHCCT and non-PHCCT groups, two-sample proportion tests were carried out for the categorical variables summarised in table 2.
Table 2.
Results of proportion tests for categorical variables
| Variable (category for proportion) |
PHCCT (proportion) | Non-PHCCT (proportion) | P value | 95% CI for difference |
| Gender (male) | 0.73 | 0.57 | <0.01 | (0.13 to 0.20) |
| Patient taken to prospective MTC (yes) | 0.77 | 0.33 | <0.01 | (0.41 to 0.47) |
| Mode of transport to hospital (land) | 0.73 | 0.98 | <0.01 | (−0.28 to −0.22) |
| Severe head injury (yes) | 0.25 | 0.17 | <0.01 | (0.04 to 0.11) |
| Prehospital intubation (yes) | 0.27 | 0.01 | <0.01 | (0.23 to 0.30) |
| Major trauma (yes) | 0.57 | 0.20 | <0.01 | (0.34 to 0.41) |
MTC, Major Trauma Centre; PHCCT, prehospital critical care team.
There are statistically significant differences between the PHCCT and non-PHCCT cohorts with regard to all six of these categorical variables.
The means of the PHCCT and non-PHCCT groups for age and ISS were compared using two-sample t-tests although the ISS data were log-transformed in order to better satisfy the assumption of normally distributed data. The t-tests also showed statistically significant differences between the PHCCT and non-PHCCT groups (table 3).
Table 3.
Results of two-sample t-tests for continuous variables
| Variable | PHCCT (mean) |
Non-PHCCT (mean) | P value | 95% CI for difference |
| Age | 45.4 | 55.3 | <0.01 | (−11.16 to −8.49) |
| ISS (log-transformed) | 2.8 | 2.3 | <0.01 | (0.52 to 0.61) |
ISS, Injury Severity Score; PHCCT, prehospital critical care team.
The GCS data were not normally distributed (the possible values range from 3 to 15 only) and none of the standard transformations (eg, log, square-root etc) were useful in producing a bell-shaped curve. Therefore, the differences between the PHCCT and non-PHCCT groups for this variable were analysed using the Mann-Whitney U-test, the non-parametric equivalent of the two-sample t-test. The p-value for the test was <0.01, indicating that the distributions of the two groups were significantly different.
Multivariate analysis
Following correction for confounding variables by multivariate analysis, the mortality rate was lower for the PHCCT group compared with the non-PHCCT group. If a patient is treated by a PHCCT, then their odds of mortality decrease by a factor of 0.56 (p-value=0.01). We also found significant evidence to support a link between mortality and age (split by gender), GCS and ISS (p-values all <0.01). The ‘effective df’ for age and ISS are greater than 1, indicating that these variables do not have a linear relationship with mortality and it was correct to fit them in a non-linear manner. These results are summarised in table 4.
Table 4.
Generalised additive model results for categorical variables (model for all patients) with OR of mortality when compared with reference group
| Variable | Category baseline |
OR | 95% CI for OR | P value |
| PHCCT | No | Reference (ref.) group | ||
| Yes | 0.56 | (0.36 to 0.86) | 0.01 | |
| Gender | Female | Ref. group | ||
| Male | 0.93 | (0.75 to 1.15) | 0.50 | |
| Prehospital intubation | No | Ref. group | ||
| Yes | 2.29 | (1.47 to 3.59) | <0.01 | |
| GCS | 13–15 | Ref. group | ||
| 3 | 53.66 | (38.45 to 74.86) | <0.01 | |
| 4–5 | 17.86 | (11.40 to 27.98) | <0.01 | |
| 6–8 | 5.46 | (3.76 to 7.91) | <0.01 | |
| 9–12 | 3.53 | (2.59 to 4.83) | <0.01 | |
| Prospective Major Trauma Centre | No | Ref. group | ||
| Yes | 1.04 | (0.85 to 1.26) | 0.72 | |
| Mode of transport to hospital | Air ambulance | Ref. group | ||
| Land ambulance | 1.79 | (1.04 to 3.07) | 0.04 | |
| Severe head injuries | No | Ref. group | ||
| Yes | 1.04 | (0.84 to 1.29) | 0.71 | |
| SIMD quintile | Quintile 5 | Ref. group | ||
| Quintile 1 | 1.41 | (1.05 to 1.90) | 0.02 | |
| Quintile 2 | 1.20 | (0.89 to 1.63) | 0.24 | |
| Quintile 3 | 1.10 | (0.80 to 1.52) | 0.56 | |
| Quintile 4 | 1.11 | (0.80 to 1.54) | 0.53 | |
| Unknown | 1.05 | (0.73 to 1.51) | 0.81 |
PHCCT, prehospital critical care team; SIMD, Scottish Index of Multiple Deprivation.
Discussion
Our results demonstrate a reduction in mortality when trauma patients receive physician-led prehospital critical care when compared with standard (non-PHCCT) ambulance care. This is the first comprehensive national data linkage study undertaken in Scotland to attempt to address the identified gaps in evidence on the effect of PHCCTs on patient outcomes.
Strengths and weaknesses of the study
Initial recruitment was comprehensive, as STAG inclusion criteria (see online supplementary appendix A) should ensure that most significantly injured patients who survive to hospital are enrolled into the database. No patients were lost to follow-up. These positives, however, are tempered by the 2877 patients excluded from the study because their level of care was not recorded. Statistical analysis suggested that these excluded patients were similar to those included, and were therefore likely ‘missing at random’, reducing the chances of bias. Of note, our work was retrospective, and did not include prehospital deaths.
Data on time from 999 call to arrival in the ED was included in the original data set but was excluded from statistical analysis due to poor completeness, as detailed previously. There are various studies15 16 showing a variable effect of PHCCTs on scene (and by implication, prehospital) times in different Emergency Medical Services (EMS) systems. In our system, longer prehospital times in the PHCCT group do not merely represent a longer transport time, but also included extra interventions either at scene or en route in a manner probably correlated with case complexity and injury severity. PHCCTs are generally looking after patients who are more severely injured, as borne out by the relative balances of severe head injury and major trauma in the two groups.
There is also some data that a longer prehospital time in a system providing prehospital critical care is compensated for by a reduced time to hospital interventions like CT scanning—that is, that PHCCTs are simply providing important clinical interventions earlier in a patient’s journey, and that overall they may not affect time to definitive care as much as the prehospital time suggests.17
There are marked differences in characteristics between the PHCCT and routine care cohorts. The methods of dispatch for PHCCTs in Scotland aim to send them to more severely injured patients identified by specialist staff in the Ambulance Control Centre,18 and it is thus expected that the PHCCT cohort had a higher ISS. In addition, the lower age and excess of male patients seen by the critical care teams likely reflects the fact that high-energy trauma is more likely to be incurred by younger men.
There was an excess of patients transported to prospective MTCs in the PHCCT cohort. Although we accounted for this variable in our multivariate analysis, there is potential that this may not have fully adjusted for any fall in mortality engendered by better hospital care. This should be taken in context, bearing in mind that no Scottish hospitals functioned as true MTCs during the period studied. However, one would expect large-volume university hospitals, such as the prospective MTCs, to be more familiar with the management of more severely injured patients—that is, those who have probably have the most to gain from PHCCT care versus standard (non-PHCCT) ambulance care.
Strengths and weaknesses in relation to other studies
The published literature on prehospital critical care suggests that PHCCTs have positive or neutral outcomes when compared with standard (non-PHCCT) ambulance care, depending on the nature of the underlying EMS system. Our work joins a number of other similar studies, from various countries, in suggesting benefit.19 20 As far as we are aware, there is no evidence suggesting that PHCCTs are detrimental to patient outcomes.
Most other works on the topic are also retrospective. A small number of randomised, prospective studies have been performed,21 22 but as physician-led prehospital critical care is considered the gold standard in many countries, there may be insufficient appetite (or equipoise) for such trials. Even where this has been possible, research can be fraught with difficulty. The well-designed and well-funded HIRT study22 was affected by protocol violations and other logistical difficulties, demonstrating the potential difficulties of prospective prehospital research.
Meaning of the study
PHCCTs augment standard paramedic care delivery with advanced interventions. Some interventions, including emergency anaesthesia (PHEA), thoraco(s)tomy, blood transfusion and some medications, are not currently within the clinical remit of the vast majority of UK ambulance clinicians. PHCCTs also offer enhanced experience of managing major trauma, high levels of teamwork, training and triage of patients direct to the most appropriate hospital. Our study suggests that it is these extra interventions and skills which may benefit patients with traumatic injuries above and beyond standard ambulance clinician care.
Conclusion
We believe that we offer further evidence of the utility and positive impact of the care provided by PHCCTs in the treatment of seriously injured patients. This study adds to the growing volume of literature demonstrating an outcome benefit associated with prehospital critical care. This work suggests that the expansion of PHCCT hours and locations, so that more of the population has timely access to such services, may increase survival after injury. Further prospective research is warranted, although this may be difficult to carry out.
Acknowledgments
The Scottish Trauma Audit Group, for providing data for analysis.
Footnotes
Twitter: @OmAndScop, @al_corfield
Contributors: ARC conceived the study. AM, ARC, SH, MJD, RML, NS and DF drafted the protocol. DC, ARC and AM provided statistical analysis and data interpretation. AM performed a literature review and wrote the first draft. All authors critically reviewed and provided input to the submitted manuscript. The majority of the suggested revisions to all versions of the manuscript were discussed and implemented by AM, ARC and DC with some input from the other authors.
Funding: This study was supported with funding from the EMRS endowment fund (ref. 1441) to pay for independent statistical analysis of the data.
Competing interests: MJD and RML are the clinical leads of two of the prehospital critical care teams which were the subject of this study; SH was previously the clinical lead of the third.
Patient and public involvement statement: This research was done without patient involvement. Patients were not invited to comment on the study design and were not consulted to develop patient relevant outcomes or interpret the results. Patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
Patient consent for publication: Not required.
Ethics approval: Ethical approval/clinical trial registration: not required, as data were fully anonymised at source before being released to the investigators.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data may be obtained from a third party and are not publicly available. Data may be obtained for research and audit purposes from the Scottish Trauma Audit Group: https://www.stag.scot.nhs.uk/Contacts/Main.htm.
References
- 1. Lopez AD, Mathers CD, Ezzati M, et al. Global burden of disease and risk factors. The World Bank and Oxford University Press, 2006. [PubMed] [Google Scholar]
- 2. Hussain LM, Redmond AD. Are pre-hospital deaths from accidental injury preventable? BMJ 1994;308:1077–80. 10.1136/bmj.308.6936.1077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Patton GC, Coffey C, Sawyer SM, et al. Global patterns of mortality in young people: a systematic analysis of population health data. Lancet 2009;374:881–92. 10.1016/S0140-6736(09)60741-8 [DOI] [PubMed] [Google Scholar]
- 4. Association of Ambulance Chief Executives and Joint Royal Colleges Ambulance Liaison Committee UK ambulance services clinical practice guidelines. Bridgwater: Class Professional Publishing, 2016. [Google Scholar]
- 5. Findlay G, Martin IC, Carter S, et al. Trauma: who cares? London: NCEPOD, 2007. [Google Scholar]
- 6. Fevang E, Lockey D, Thompson J, et al. The top five research priorities in physician-provided pre-hospital critical care: a consensus report from a European research collaboration. Scand J Trauma Resusc Emerg Med 2011;19:57 10.1186/1757-7241-19-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Association for the Advancement of Automotive Medicine The abbreviated injury scale. 1990 revision. Des Plaines, IL: AAAM, 1990. [Google Scholar]
- 8. Baker SP, O'Neill B, Haddon W, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974;14:187–96. [PubMed] [Google Scholar]
- 9. Scottish index of Multiple Deprivation The Scottish government's official tool to identify areas of multiple deprivation in Scotland. Available: https://www2.gov.scot/Topics/Statistics/SIMD [Accessed 19tth Dec 2018].
- 10. Hastie TJ, Tibshirani RJ. Generalized additive models. London: Chapman & Hall/CRC, 1990. [Google Scholar]
- 11. Wood SN. Fast stable restricted maximum likelihood and marginal likelihood estimation of semiparametric generalized linear models. J Royal Stats Soc 2011;73:3–36. 10.1111/j.1467-9868.2010.00749.x [DOI] [Google Scholar]
- 12. Jones JM, Skaga NO, Søvik S, et al. Norwegian survival prediction model in trauma: modelling effects of anatomic injury, acute physiology, age, and co-morbidity. Acta Anaesthesiol Scand 2014;58:303–15. 10.1111/aas.12256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Belzunegui T, Gradín C, Fortún M, et al. Major trauma registry of Navarre (Spain): the accuracy of different survival prediction models. Am J Emerg Med 2013;31:1382–8. 10.1016/j.ajem.2013.06.026 [DOI] [PubMed] [Google Scholar]
- 14. R Core Team R: a language and environment for statistical computing. Vienna: R foundation for statistical computing, 2015. Available: http://www.R-project.org/
- 15. Timm A, Maegele M, Lefering R, et al. Pre-Hospital rescue times and actions in severe trauma. A comparison between two trauma systems: Germany and the Netherlands. Injury 2014;45:S43–52. 10.1016/j.injury.2014.08.017 [DOI] [PubMed] [Google Scholar]
- 16. Dissmann PD, Le Clerc S. The experience of Teesside helicopter emergency services: doctors do not prolong prehospital on-scene times. Emerg Med J 2007;24:59–62. 10.1136/emj.2006.038844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. van der Velden MWA, Ringburg AN, Bergs EA, et al. Prehospital interventions: time wasted or time saved? an observational cohort study of management in initial trauma care. Emerg Med J 2008;25:444–9. 10.1136/emj.2007.052662 [DOI] [PubMed] [Google Scholar]
- 18. Sinclair N, Swinton PA, Donald M, et al. Clinician tasking in ambulance control improves the identification of major trauma patients and pre-hospital critical care team tasking. Injury 2018;49:897–902. 10.1016/j.injury.2018.03.034 [DOI] [PubMed] [Google Scholar]
- 19. Den Hartog D, Romeo J, Ringburg AN, et al. Survival benefit of physician-staffed helicopter emergency medical services (HemS) assistance for severely injured patients. Injury 2015;46:1281–6. 10.1016/j.injury.2015.04.013 [DOI] [PubMed] [Google Scholar]
- 20. Garner A, Rashford S, Lee A, et al. Addition of physicians to paramedic helicopter services decreases blunt trauma mortality. Aust N Z J Surg 1999;69:697–701. 10.1046/j.1440-1622.1999.01688.x [DOI] [PubMed] [Google Scholar]
- 21. Bernard SA, Nguyen V, Cameron P, et al. Prehospital rapid sequence intubation improves functional outcome for patients with severe traumatic brain injury: a randomized controlled trial. Ann Surg 2010;252:959–65. 10.1097/SLA.0b013e3181efc15f [DOI] [PubMed] [Google Scholar]
- 22. Garner AA, Mann KP, Fearnside M, et al. The head injury retrieval trial (Hirt): a single-centre randomised controlled trial of physician prehospital management of severe blunt head injury compared with management by paramedics only. Emerg Med J 2015;32:869–75. 10.1136/emermed-2014-204390 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
emermed-2019-208458supp001.pdf (62.9KB, pdf)