Abstract
Background:
The development of novel revascularization devices has improved procedural and clinical outcomes in acute ischemic stroke (AIS). A direct aspiration first pass technique (ADAPT) has been introduced as a rapid simple method for achieving good recanalization and clinical outcomes using large bore aspiration catheters in the treatment of AIS due to large vessel occlusion (LVO).
Objectives:
The aim of this study was to assess the safety and efficacy of ADAPT in the treatment of AIS due to LVO in the Vietnamese patient population.
Materials and Methods:
A retrospective analysis of a hospital database was conducted on all patients undergoing stroke therapy with the ADAPT technique at the institution from January 2017 to December 2017. Efficacy and safety were evaluated by the variables: revascularization rates (thrombolysis in cerebral infarction [TICI] score), time to revascularization, procedural complications, and clinical outcomes (modified Rankin scale [mRS] score) at the 90-day follow-up visit.
Results:
From the database review, 37 AIS patients treated with ADAPT were identified. The mean NIHSS score at presentation was 17.3 and improved to 8.9 at discharged. The average time arterial puncture to revascularization was 32.5 min. TICI 2b/3 revascularization was achieved in 30/37 (81.1%) patients, good clinical outcomes were achieved (mRS 0–2) in 21/37 (56.7%) patients, and mortality rate was 6/37 (16.2%) during follow-up.
Conclusions:
ADAPT utilizing large bore aspiration catheters appears to be a fast, simple, safe, and effective method for the management of AIS in the Vietnamese patient population.
Keywords: A direct aspiration first pass technique, endovascular management, large vessel occlusion
Introduction
Stroke is the fifth leading cause of death in the United States (U.S.)[1] and the second leading cause of death worldwide.[2] In the U.S., approximately 610,000 new strokes occur each year, contributing to over 140,000 annual deaths from stroke, and ischemic strokes account for more than 85% of strokes.[1] In Vietnam, the annual incidence of new strokes was estimated at 90.2 per 100,000 people, with a third attributable to hemorrhagic stroke.[3]
Six recent randomized controlled trials (RCTs)[4,5,6,7,8,9] demonstrated the safety and efficacy of mechanical thrombectomy for the treatment of acute ischemic stroke (AIS) due to large vessel occlusion (LVO). Based on the results of these studies, the International Medical Community provided updated guidelines for the management of AIS that included a recommendation in favor of mechanical thrombectomy for patients meeting certain criteria,[10,11] further expanding the treatment window in 2018 for selected cases.[12]
Mechanical thrombectomy can be generally categorized into two main techniques: usage of stent retrievers and usage of direct aspiration (a direct aspiration first pass technique [ADAPT]).[13,14,15,16] These two techniques are not mutually exclusive and are often used together.[17] The ASTER, three-dimensional (3D), and COMPASS trials were randomized studies that compared the risks and benefits of aspiration thrombectomy frontline to that of stent retriever frontline.[18,19,20] Results from these studies showed that direct aspiration provided noninferior safety and efficacy outcomes compared with stent retrievers.
In our experience, the ADAPT is not yet widely utilized in Vietnam as compared to internationally. This may be due, in part, to the scarcity of data specific to the Vietnamese patient population. As stroke burden in Southeast Asia increases due to improved life expectancy and high rate of underlying intracranial atherosclerotic disease, it is critical to develop appropriate stroke systems of care.[21,22] Population-specific data may be useful for improving these systems in Southeast Asia. This study was conducted to evaluate the safety and efficacy of ADAPT in the treatment of AIS due to LVO in the population treated at our institution in Vietnam.
Materials and Methods
This study was a retrospective chart review of AIS patients treated with ADAPT at a Vietnamese hospital from January 2017 through December 2017. AIS patients ≥18 years old, with baseline NIHSS ≥6, ASPECTS ≥6, and LVO (internal carotid artery, middle cerebral artery [M1/M2 segments], vertebral artery, and basilar artery) treated with ADAPT within 6 h of stroke symptom onset were included. Intravenous (IV) recombinant tissue plasminogen activator (Alteplase, Genentech, San Francisco, CA, USA) usage before aspiration therapy was permissible.
Before intervention, the patients underwent 64–128 slice computed tomographic imaging and/or 1.5–3T magnetic resonance imaging to visualize the extent of cerebral parenchymal injury, identify the site of vascular occlusion, and assess the availability of collateral circulation. Anesthesia was administered as either local anesthesia with IV preanesthesia or general anesthesia. Treatment consisted of the ADAPT using the 5MAX ACE reperfusion catheter (Penumbra Inc., Alameda, CA, USA). A typical procedure with ADAPT has been described previously.[13,14] Direct aspiration at the face of the thrombus with a 50cc syringe was performed. Aspiration alone was performed up to three times. If aspiration alone was unsuccessful, adjunctive therapy with a stent retriever (Solitaire, Medtronic, Dublin, Ireland) and thrombolytic therapy was utilized. Digital subtraction angiography (Artis Zee, Siemens) was performed immediately after intervention to assess efficacy of revascularization.
Baseline characteristics, key time metrics (onset-to-admission, admission-to-puncture, puncture-to-revascularization), postprocedural thrombolysis in cerebral infarction (TICI) score, baseline NIHSS, 24-h postintervention NIHSS, all periprocedural adverse events, and modified Rankin scale (mRS) at 90 days postprocedure were included in this review. All data were collected in accordance with the institutional ethics guidelines. This study was reviewed and approved by our institutional ethics committee (IEC). Patients or their representatives provided informed consent or consent was waived by the IEC due to the retrospective study design.
Results
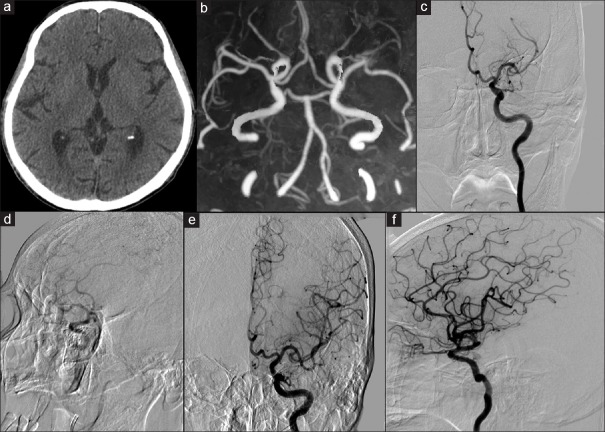
Thirty-seven patients met the study inclusion criteria. The mean age was 61.4 ± 13.4 years (range 27–89 years), with a female/male ratio of 2.4/1. In terms of target vessel locations, 86.5% (32/37) of occlusions were in the anterior circulation and 13.5% (5/37) were in the posterior circulation. For anesthesia, 81.1% (30/37) of cases were treated under local anesthesia and IV preanesthesia, while the remaining 18.9% (7/37) cases were treated under endotracheal intubation/general anesthesia. The mean time from arterial puncture to TICI 2b-3 revascularization was 32.5 min. Direct aspiration was performed for all patients, with 13.5% (5/37) using stent retriever when the optimal recanalization was not achieved. Patient characteristics and procedural time metrics are provided in Table 1. A representative case is available in Figure 1.
Table 1.
Baseline characteristics and procedural times
| Characteristic | Patients (%) |
|---|---|
| Age (years) | 61.4±13.4 |
| Female | 26/37 (70.3) |
| Baseline NIHSS | 17.3±6.9 |
| Baseline ASPECTS | 8.0±1.5 |
| IV tPA before procedure | 13/37 (35.1) |
| Target vessel location | |
| Middle cerebral artery (M1 or M2) | 19/37 (51.4) |
| Internal carotid artery/carotid T | 13/37 (35.1) |
| Vertebral artery | 0/37 (0) |
| Basilar artery | 5/37 (13.5) |
| Time interval (min) | Mean (Minimum-maximum) |
| From onset stroke to admission | 213.6 (1-324) |
| Admission to needle (from admission to arterial puncture) | 95.4 (46-345) |
| Puncture to revascularization (from arterial puncture to revascularization) | 32.5 (10-70) |
IV – Intravenous; NIHSS – National Institutes of Health Stroke Scale; tPA – Tissue plasminogen activator, ASPECTS – Alberta stroke program early CT score
Figure 1.
A 73-year-old male with admission Glasgow coma scale of 13 and NIHSS of 15 presented with a 2-h history of right-sided weakness, facial droop, and dysarthria. Brain computed tomography identified no hemorrhage and ASPECTS of 10 (a – top left). Computed tomography angiography revealed occlusion of the left middle cerebral artery M1 segments (b – top middle). Preprocedural digital subtraction angiography confirmed occlusion location, and thrombolysis in cerebral infarction score was 0 (c – top right, d – bottom left). After aspiration thrombectomy with the ACE68 reperfusion catheter, digital subtraction angiography imaging showed complete revascularization of the left middle cerebral artery with thrombolysis in cerebral infarction score 3 (e – bottom middle, f – bottom right). Good clinical outcome was observed at discharge (modified Rankin scale = 0)
The mean NIHSS score before intervention was 17.3 and after intervention was 8.4, with the average improvement in NIHSS being 8.9 [Table 2]. After all interventions, 81.1% of cases (30/37) achieved TICI 2b-3 revascularization, with 40% achieving complete restoration of flow (TICI 3). Poor recanalization (TICI 1-2a) and nonrecanalization (TICI 0) totaled 18.9% (7/37). Functional independence, defined as mRS 0–2 at 90 days, was achieved in 56.8% (21/37) of cases [Table 2]. mRS 3–5 was reported in 10 of 37 cases (27.1%). Among patients with occlusions in the vertebral or basilar arteries, patients achieved TICI 2b-3 revascularization in 80% (4/5) and 90-day mRS 0–2 in 60% (3/5) of cases.
Table 2.
Angiographic and clinical outcomes
| Outcome | Patients (%) |
|---|---|
| TICI 2b-3 postprocedure | 30/37 (81.1) |
| 90-day mRS 0-2 | 21/37 (56.8) |
| NIHSS before intervention | 17.3 |
| NIHSS 24 h after intervention | 8.4 |
| Average improvement in NIHSS | 8.9 |
| Intracranial hemorrhage | 5/37 (13.5) |
| Mortality | 6/37 (16.2) |
NIHSS – National Institutes of Health Stroke Scale; TICI – Thrombolysis in cerebral infarction
There were four patients with cerebral vasospasm and five patients with distal embolization. No patients experienced vessel dissection or perforation during the intervention. Intracranial hemorrhage rate within 30 days was 13.5% (5/37). Mortality at 90 days was 16.2% (6/37). Of these deaths two were associated with PH type hemorrhage and four were associated with HI type hemorrhage based on ECASS definitions.
Discussion
In this study of 37 patients with AIS treated with ADAPT, use of direct aspiration thrombectomy appeared to be effective, with an acceptable safety profile. TICI 2b-3 flow was achieved in 81.1% of cases, with a mean time from arterial puncture to revascularization of 32.5 min. The rate of mRS 0–2 at 90 days was 56.8%. With regard to complications, four patients experienced cerebral vasospasm and five patients had embolization of new territories. Most cases were treated under local anesthesia and/or IV preanesthesia; however, the procedure still had promising outcomes and was safe and quick. Throughout the world, the choice of general anesthesia or local anesthesia and the effect of these methods on treatment outcomes remain controversial.
The high rate of revascularization observed in the current study was consistent with our previous observation of 79% revascularization (Khoi et al.'s Clinical application research on endovascular interventional techniques for treatment of acute and chronic stroke. State-level Research KC10-15; 2015, unpublished results) and previous studies on ADAPT[18,19] [Table 3] and lower than the ADAPT FAST multicenter study (97.8%, 5 MAX ACE).[13] The 56.8% rate of 90-day good clinical outcomes (mRS 0–2) in patients with early admission hospitalization was on the higher side compared with previous studies, while the 16.2% rate of mortality compared favorably as well. The current study time to revascularization was slightly shorter than that of the 3D RCT and was in alignment with the ADAPT FAST study (35.6 min). Among patients with occlusions in the vertebral or basilar arteries, the current study found that patients achieved 80% revascularization and 60% 90-day good clinical outcomes, which was similar to outcomes in the anterior circulation and was consistent with 96.4% (54/56) and 42.9% (24/56), respectively, in a study of ADAPT in the posterior circulation.[23] The small sample size, however, should be noted.
Table 3.
Comparison of rates of revascularization, functional outcome, time to revascularization, mortality among studies
| Current study | ASTER aspiration group[18] | 3D RCT aspiration group[19] | |
|---|---|---|---|
| n | 37 | 192 | 100 |
| Time from arterial puncture to revascularization, mean (min) | 32.5 | Not reported | 39* |
| TICI 2b-3 (%) | 81.1 | 85.4 | 69.8 |
| TICI 3 (%) | 40 | 37.5 | 45.4 |
| 90-day mRS 0-2 (%) | 56.8 | 45.3 | 45.8 |
| Mortality (%) | 16.2 | 19.3 | 26.0 |
*Median. 3D-RCT – Three-dimensional randomized controlled trial; TICI – Thrombolysis in cerebral infarction; mRS – Modified Rankin scale
We elected frontline aspiration thrombectomy over stent retriever thrombectomy due to recent clinical studies, demonstrating significantly lower costs with ADAPT[20,24] while maintaining noninferior outcomes.[18,19,20] At our institution, the supplier price of the ACE68 reperfusion catheter is approximately 44%–68% lower than several popular stent retrievers. Cost-effective treatments are especially of interest in Vietnam due to both the increased healthcare costs associated with a rapidly aging population[25] and the large proportion of patients without health insurance.[26] Aspiration may reduce healthcare cost and allow greater healthcare access for the uninsured.
In addition, ADAPT is less technically complex and has no wait time for device integration into clot. This may result in reduced procedure time,[19] leading to increased ischemic area salvage and reduced neurological damage.[27] These benefits may become more apparent as newer generation aspiration catheters with larger bores and better traceability, like the ones used in this study, continue to be introduced.
Limitations of this study included the evaluation of retrospective data from one institution and absence of blinded assessment of angiographic and clinical outcomes. Strengths included the analysis of data from all patients presenting with AIS and treated with ADAPT at a Vietnamese stroke center.
Conclusion
In 37 cases of endovascular neurointervention for the treatment of AIS due to LVO by ADAPT, we found that ADAPT is an effective method, with high revascularization rates and low procedural complication rates. These findings of safety and efficacy in a Vietnamese population were comparable with previous studies in other cohorts.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S, et al. Heart disease and stroke statistics-2018 update: A report from the American Heart Association. Circulation. 2018;137:e67–492. doi: 10.1161/CIR.0000000000000558. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Mortality and Global Health Estimates. Geneva: [Last accessed on 2018 Sep 10]. Available from: http://www.who.int/gho/mortality_burden_disease/en/ [Google Scholar]
- 3.Yamanashi H, Ngoc MQ, Huy TV, Suzuki M, Tsujino A, Toizumi M, et al. Population-based incidence rates of first-ever stroke in central Vietnam. PLoS One. 2016;11:e0160665. doi: 10.1371/journal.pone.0160665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berkhemer OA, Fransen PS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015;372:11–20. doi: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 5.Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015;372:1019–30. doi: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 6.Campbell BC, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi N, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015;372:1009–18. doi: 10.1056/NEJMoa1414792. [DOI] [PubMed] [Google Scholar]
- 7.Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI, Pereira VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs.t-PA alone in stroke. N Engl J Med. 2015;372:2285–95. doi: 10.1056/NEJMoa1415061. [DOI] [PubMed] [Google Scholar]
- 8.Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015;372:2296–306. doi: 10.1056/NEJMoa1503780. [DOI] [PubMed] [Google Scholar]
- 9.Bracard S, Ducrocq X, Mas JL, Soudant M, Oppenheim C, Moulin T, et al. Mechanical thrombectomy after intravenous alteplase versus alteplase alone after stroke (THRACE): A randomised controlled trial. Lancet Neurol. 2016;15:1138–47. doi: 10.1016/S1474-4422(16)30177-6. [DOI] [PubMed] [Google Scholar]
- 10.Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association Focused Update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: A Guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015;46:3020–35. doi: 10.1161/STR.0000000000000074. [DOI] [PubMed] [Google Scholar]
- 11.Wahlgren N, Moreira T, Michel P, Steiner T, Jansen O, Cognard C, et al. Mechanical thrombectomy in acute ischemic stroke: Consensus statement by ESO-Karolinska Stroke Update 2014/2015, supported by ESO, ESMINT, ESNR and EAN. Int J Stroke. 2016;11:134–47. doi: 10.1177/1747493015609778. [DOI] [PubMed] [Google Scholar]
- 12.Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: A Guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018;49:e46–110. doi: 10.1161/STR.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 13.Turk AS, Frei D, Fiorella D, Mocco J, Baxter B, Siddiqui A, et al. ADAPT FAST study: A direct aspiration first pass technique for acute stroke thrombectomy. J Neurointerv Surg. 2014;6:260–4. doi: 10.1136/neurintsurg-2014-011125. [DOI] [PubMed] [Google Scholar]
- 14.Kowoll A, Weber A, Mpotsaris A, Behme D, Weber W. Direct aspiration first pass technique for the treatment of acute ischemic stroke: Initial experience at a European stroke center. J Neurointerv Surg. 2016;8:230–4. doi: 10.1136/neurintsurg-2014-011520. [DOI] [PubMed] [Google Scholar]
- 15.Gory B, Armoiry X, Sivan-Hoffmann R, Piotin M, Mazighi M, Lapergue B, et al. Adirect aspiration first pass technique for acute stroke therapy: A systematic review and meta-analysis. Eur J Neurol. 2018;25:284–92. doi: 10.1111/ene.13490. [DOI] [PubMed] [Google Scholar]
- 16.Vargas J, Spiotta A, Fargen K, Turner R, Chaudry I, Turk A, et al. Long term experience using the ADAPT technique for the treatment of acute ischemic stroke. J Neurointerv Surg. 2017;9:437–41. doi: 10.1136/neurintsurg-2015-012211. [DOI] [PubMed] [Google Scholar]
- 17.Hesse AC, Behme D, Kemmling A, Zapf A, Große Hokamp N, Frischmuth I, et al. Comparing different thrombectomy techniques in five large-volume centers: A 'real world' observational study. J Neurointerv Surg. 2018;10:525–9. doi: 10.1136/neurintsurg-2017-013394. [DOI] [PubMed] [Google Scholar]
- 18.Lapergue B, Blanc R, Gory B, Labreuche J, Duhamel A, Marnat G, et al. Effect of endovascular contact aspiration vs. stent retriever on revascularization in patients with acute ischemic stroke and large vessel occlusion: The ASTER randomized clinical trial. JAMA. 2017;318:443–52. doi: 10.1001/jama.2017.9644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nogueira RG, Frei D, Kirmani JF, Zaidat O, Lopes D, Turk AS, 3rd, et al. Safety and efficacy of a 3-dimensional stent retriever with aspiration-based thrombectomy vs.aspiration-based thrombectomy alone in acute ischemic stroke intervention: A randomized clinical trial. JAMA Neurol. 2018;75:304–11. doi: 10.1001/jamaneurol.2017.3967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Turk AS, 3rd, Siddiqui A, Fifi JT, De Leacy RA, Fiorella DJ, Gu E, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): A multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet. 2019;393:998–1008. doi: 10.1016/S0140-6736(19)30297-1. [DOI] [PubMed] [Google Scholar]
- 21.Koo J. The latest information on intracranial atherosclerosis: Diagnosis and treatment. Interv Neurol. 2015;4:48–50. doi: 10.1159/000438779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ng JC, Churojana A, Pongpech S, Vu LD, Sadikin C, Mahadevan J, et al. Current state of acute stroke care in Southeast Asian countries. Interv Neuroradiol. 2019;25:291–6. doi: 10.1177/1591019918811804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alawieh A, Vargas J, Turner RD, Turk AS, Chaudry MI, Lena J, et al. Equivalent favorable outcomes possible after thrombectomy for posterior circulation large vessel occlusion compared with the anterior circulation: The MUSC experience. J Neurointerv Surg. 2018;10:735–40. doi: 10.1136/neurintsurg-2017-013420. [DOI] [PubMed] [Google Scholar]
- 24.Turk AS, Turner R, Spiotta A, Vargas J, Holmstedt C, Ozark S, et al. Comparison of endovascular treatment approaches for acute ischemic stroke: Cost effectiveness, technical success, and clinical outcomes. J Neurointerv Surg. 2015;7:666–70. doi: 10.1136/neurintsurg-2014-011282. [DOI] [PubMed] [Google Scholar]
- 25.Takashima K, Wada K, Tra TT, Smith DR. A review of Vietnam's healthcare reform through the direction of healthcare activities (DOHA) Environ Health Prev Med. 2017;22:74. doi: 10.1186/s12199-017-0682-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoang CK, Hill P, Nguyen HT. Universal health insurance coverage in Vietnam: A Stakeholder analysis from policy proposal (1989) to implementation (2014) J Public Health Manag Pract. 2018;24(Suppl 2):S52–9. doi: 10.1097/PHH.0000000000000729. [DOI] [PubMed] [Google Scholar]
- 27.Saver JL. Time is brain – Quantified. Stroke. 2006;37:263–6. doi: 10.1161/01.STR.0000196957.55928.ab. [DOI] [PubMed] [Google Scholar]