Abstract
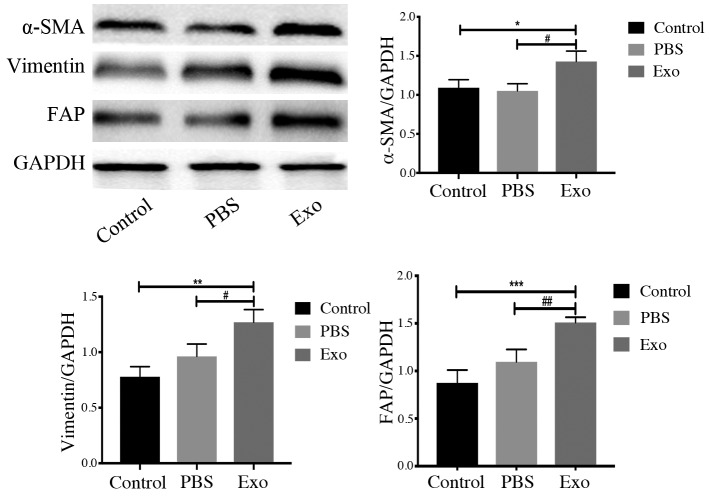
Recently, several studies have demonstrated that cancer cell-derived exosomes can facilitate tumor development and metastasis formation. However, the detailed function of exosomes released by cancer stem cells (CSCs) requires further investigation. The aim of the present study was to investigate the role of CSC-derived exosomes in tumor development. For this purpose, Piwil2-induced cancer stem cells (Piwil2-iCSCs) were used as exosome-generating cells, while fibroblasts (FBs) served as recipient cells. Exosomes were isolated by the ultracentrifugation of Piwil2-iCSC-conditioned medium and identified by transmission electron microscopy, nanoparticle tracking analysis and western blot analysis. To evaluate the effects of the exosomes on cell proliferation, migration and invasion, cell counting assay (CCK-8), a wound healing assay and a Transwell assay were performed. Protein expression [matrix metalloproteinase (MMP)2, MMP9, α-smooth muscle actin (α-SMA) and vimentin and fibroblast-activating protein (FAP)] was examined in FBs by western blot analysis. It was found that the Piwil2-iCSC-derived exosomes (Piwil2-iCSC-Exo) were oval or spherical, membrane-coated vesicles with a uniform size (30–100 nm in diameter). They are characterized by the surface expression of CD9, CD63, Hsp70 and Piwil2 proteins. Additional results from functional analyses revealed that Piwil2-iCSC-Exo enhanced the proliferative, migratory and invasive abilities of FBs, accompanied by the upregulated expression of MMP2 and MMP9. In addition, the increased expression of α-SMA (P<0.05), vimentin (P<0.01 vs. control group, P<0.05 vs. PBS group) and FAP (P<0.001 vs. control group, P<0.01 vs. PBS group) following exposure to Piwil2-iCSC-Exo suggested that the exosomes induced FB transformation into cancer-associated fibroblasts (CAFs). On the whole, the findings of this study demonstrate that Piwil2-iCSC-Exo induce the cancer-associated phenotype in fibroblasts in vitro, suggesting that CSCs can promote tumor development through the modulation of the tumor microenvironment.
Keywords: exosomes, cancer stem cells, cancer-associated fibroblasts, proliferation, migration, invasion
Introduction
Following heart disease, cancer is the leading cause of mortality associated with incommunicable diseases worldwide (1). Local infiltration and distant metastasis are major challenges faced by oncologists, ultimately affecting the call for effective therapy (2). Due to these challenges, the correct diagnosis of the tissue from which the cancer originated and further prognosis for treatment remain an area of great interest. There are several theories that have emerged to explain the mechanisms of a poor prognosis.
A cancerous tumor is an extremely complex ecosystem that consists of both malignant and normal cells. The latter include the reactive tumor stroma, which contributes to the diverse phenotypic heterogeneity of solid tumors (3). All heterogenous cancer cells are derived from cancer stem cells (CSCs), a relatively rare subgroup of tumor cells possessing self-renewal properties, tumorigenicity and multilineage differentiation ability (4–8). CSCs are considered the drivers of malignant growth, treatment resistance, minimal residual disease and the formation of metastases (9–11). Moreover, CSCs have been shown to regulate tumor growth and progression (12–15).
The tumor microenvironment plays an important role in tumor growth and metastasis formation (16–18). It is a dynamic structure consisting of multiple components, including interstitial tissue and extracellular matrix, both of which influence tumor cell properties (19). Exosomes, key players in the tumor microenvironment, are small (between 30 and 100 nm in diameter), membrane-enclosed vesicles secreted by cells and are distributed in bodily fluids (20,21). Transporting a variety of biologically active substances, such as proteins and nucleic acids, exosomes mediate local and systemic cell communication (22,23). Accumulating evidence demonstrates that cancer-derived exosomes play a critical role in tumor metastasis (24–26). However, little is known about CSC-derived exosomes.
For a number of years, fibroblasts (FBs) have been considered an important participant in a variety of aspects involving tumor development and progression. It has been shown that normal FBs can be induced by surrounding tumor cells to differentiate into tumor-promoting cancer-associated fibroblasts (CAFs) (27,28). It has been demonstrated that the Piwi family protein, Piwil2, regulates the self-renewal of germline stem cells and plays an important regulatory role in tumorigenesis (29). Piwil2 is expressed in the human testis and various tumor cells, including colon cancer (30), breast cancer (31) and cervical cancer (32). It has been reported that the expression of Piwil2 in malignant tumors may be related to the incidence, development and prognosis of tumors (33–35). In a previous study by the authors, a Piwil2 GFP lentiviral vector was used to transduce fibroblasts, and the successfully constructed Piwil2-induced tumor stem cells (Piwil2-iCSC) characterized by self-renewal, multiple differentiation capabilities, cell atypia and tumorigenic properties (36). In this study, to elucidate the role of exosomes derived from CSCs in tumorigenesis and cancer progression, these induced tumor stem cells were used to generate Piwil2-iCSC-Exo and investigate their role in the proliferation, migration and invasion of FBs.
Materials and methods
Cell lines and cell culture
Piwil2-iCSCs and FBs were obtained from the Chongqing Key Laboratory of Child Urogenital Development and Tissue Engineering (36). The Piwil2-iCSCs were cultured in Dulbecco's modified Eagle's medium (DMEM) supplemented with penicillin/streptomycin and 10% fetal bovine serum (FBS; Gibco; Thermo Fisher Scientific) depleted of bovine exosomes by overnight ultracentrifugation at 100,000 × g, followed by filtration through a 0.2-µm filter (Millipore). FBs were cultured in DMEM/F-12 medium supplemented with 10% FBS. All the cells were cultured at 37°C in a humidified 5% CO2 atmosphere. All experiments were carried out at a cell confluence of 80 to 90%.
Exosome isolation
Exosomes were isolated through the differential centrifugation of conditioned medium collected from Piwil2-iCSC cultures after achieving 90% confluency. Briefly, the conditioned medium was first subjected to serial centrifugation to remove cells (500 × g, 10 min) and cellular debris (2,000 × g, 20 min). Later the supernatant was filtered (0.22 µm) to remove the remaining debris and larger vesicles and subjected to centrifugation at 100,000 × g for 70 min to pellet the exosomes. Finally, the pellets were washed with phosphate-buffered saline (PBS) and the ultracentrifugation protocol was repeated. The final exosome pellet was resuspended in PBS and frozen in aliquots maintained at −80°C.
Transmission electron microscopy (TEM)
The presence of purified exosomes was confirmed with transmission electron microscopy (TEM). Exosomal proteins were measured using a bicinchoninic acid protein assay kit (BCA, Beyotime). In brief, 10 µg exosomes were placed on a copper grid, followed by negative staining with 2% uranyl acetate for 2 min at room temperature. Grids were rinsed in deionized water and allowed to dry overnight. The samples were then visualized using a Hitachi S-3000 N electron microscope.
Nanoparticle tracking analysis (NTA)
The size and the concentration of the exosome particles resuspended in PBS were determined using NTA (Zetasizer Nano ZS90, Malvern Panalytical). The diluted exosomes were injected into the LM10 unit (Malvern Panalytical). NTA software, v2.3 (Malvern Panalytical) was used to collect and analyze the videos.
Exosome uptake assay
The FBs (3×104 cells/well) were inoculated into 24-well plates (Corning Inc.) pre-loaded with cell slides and allowed to adhere overnight. Subsequently, PKH26 (MINI26; Sigma-Aldrich) pre-stained Piwil2-iCSCs exosomes according to the manufacturer's protocol were added to the wells. After 0, 3, 6, 12 and 24, the cells were fixed in 4% paraformaldehyde for 20 min, washed 3 times with PBS, and stained with DAPI for 1 h at room temperature. After being sealed with an anti-fluorescence quencher, the slides were imaged using a fluorescent microscope (Nikon).
Western blot analysis
Protein samples of exosomes and cells were lysed in RIPA buffer (Beyotime) supplemented with proteinase inhibitors (Beyotime). The protein concentration was determined using a bicinchoninic acid (BCA) assay kit (Beyotime). Equal amounts of proteins (10 µg) were separated on an 8% SDS-PAGE (sodium dodecyl sulfate-polyacrylamide gel electrophoresis) gel and transferred onto polyvinylidene fluoride (PVDF; Millipore) membranes. The membranes were then blocked in 5% (w/v) non-fat milk and incubated with the primary antibodies overnight at 4°C. The following antibodies were used: CD9 (1:1,000, ab92726; Abcam), CD63 (1:1,000, ab134045; Abcam), heat shock protein (HSP)70 (1:1,000, ab181606; Abcam), Piwil2 (1:1,000, ab181340; Abcam), matrix metalloproteinase (MMP)9 (1:1,000 ab76003; Abcam), MMP2 (1:1,000, GTX104577; Genetex), α-smooth muscle actin (α-SMA; 1:1,000, ab32575; Abcam), Vimentin (1:1,000, GTX100619; Genetex), fibroblast-activating protein (FAP; 1:1,000, ab207178; Abcam), GAPDH (1:1,000, ab181602; Abcam). Finally, the membranes were incubated with HRP-conjugated secondary antibody (1:1,000, ZB-2301, ZB-2305; Zhongshan) for 2 h at room temperature. The immunoblots were visualized using the Immobilon Western Chemiluminescent HRP Substrate, and the bands were quantified, relative to GAPDH, by densitometric analysis (GeneGnome, Syngene UK).
Optimization experiments
In the optimization phase, a dose-escalation experiment was performed with increasing concentrations of exosomes (50, 80, 100, 160, 200 and 320 µg/ml) using the Cell Counting Kit-8 (CCK-8, Dojindo Laboratories) following the manufacturer's protocol to determine the optimal exosome concentration. In brief, the cells were seeded in 96-well plates (Corning, Inc.; 3,000 cells/well) in triplicate and cultured in DMEM/F-12 medium supplemented with 10% FBS overnight at 37°C. The exosome suspension was then added, and following incubation at 37°C for 24 h, the cells were treated with the CCK-8 reagent and the absorbance was measured using a spectrophotometer (BioTek Epoch, BioTek Instruments, Inc.) at 450 nm.
Exosome treatment
The FBs which were collected during their logarithmic growth phase, were inoculated into the wells and were divided into the control group (untreated), PBS-treated group (PBS) and the exosome-treated group (Exo). As the exosomes were suspended in PBS, the PBS-treated group served as a control for the experiment. The concentration of the exosomes is relatively low and the addition of exosome suspension reduces the concentration of FBS into the culture medium. In order to control for the effect of PBS altering the dilution of FBS on cell growth, a blank group was added (termed the control group) to ensure that the addition of PBS had no obvious effect on cell growth. Each experimental group was evaluated with 5 duplicate wells and at least 3 independent experiments were performed.
Cell proliferation assay
Cell proliferation assays were performed using a CCK-8 assay (Dojindo Laboratories) following the manufacturer's protocol as described above. In brief, the cells were plated in 96-well plates (Corning, Inc.; 3,000 cells/well) in triplicate and cultured in growth medium overnight. The cells were then divided in accordance with their experimental groups. Subsequently, the cells were treated with the CCK-8 reagent and the absorbance was measured by spectrophotometer (BioTek Epoch, BioTek Instruments, Inc.) at 450 nm. Proliferation rates were determined after 0, 24, 48 and 72 h of exosome treatment.
Cell migration assay
To assess the cell migratory ability, a wound healing assay was performed. The cells were seeded at 2×105 cells/well in 6-well plates (Corning, Inc.) to achieve a confluent monolayer. The monolayer was then scratched with a 200 µl pipette tip to simulate a wound. After washing with PBS, the cells were incubated in the presence or absence of the exosomes (1% FBS; 1% FBS was used as the FB condition deteriorated progressively after 24 h in FBS-free medium). Microscopic evaluation was performed by a fluorescence microscope (K10587; Nikon) after 0, 12 and 24 h of culture.
Cell invasion assay
Cell invasion ability was analyzed in a Transwell chamber assay. First, the cells were incubated at 37°C for 24 h in the presence or absence of exosomes in growth medium. The cells (2×104 cells/well) were then seeded in the upper chamber with serum-free medium, coated with 30 mg/cm2 Matrigel (Sigma-Aldrich) and the lower layer was supplemented with 600 µl of DMEM/F-12 medium containing 10% FBS. Following incubation at 37°C, 5% CO2 for 24 h, the cells remaining on the top surface of the membrane (non-invasive cells) were scraped with cotton swabs, while the cells localized on the bottom sides of the membrane (invasive cells) were washed with PBS, fixed with cold methanol for 20 min, stained with eosin at room temperature for 5 min and mounted. The cells migrating through the membrane were counted in 5 randomly selected fields under a microscope (K10587; Nikon) at magnification, ×100.
Statistical analysis
Each experiment was repeated at least 3 times, and SPSS v24.0 software was used for all statistical analyses. Comparisons between groups were analyzed using one-way ANOVA. In this study, the variance of all experiments was homogeneous; thus, the LSD post hoc test was selected for analysis. Data are expressed as the means ± SEM. P<0.05 was considered to indicate a statistically significant difference.
Results
Characterization of Piwil2-iCSC-Exo
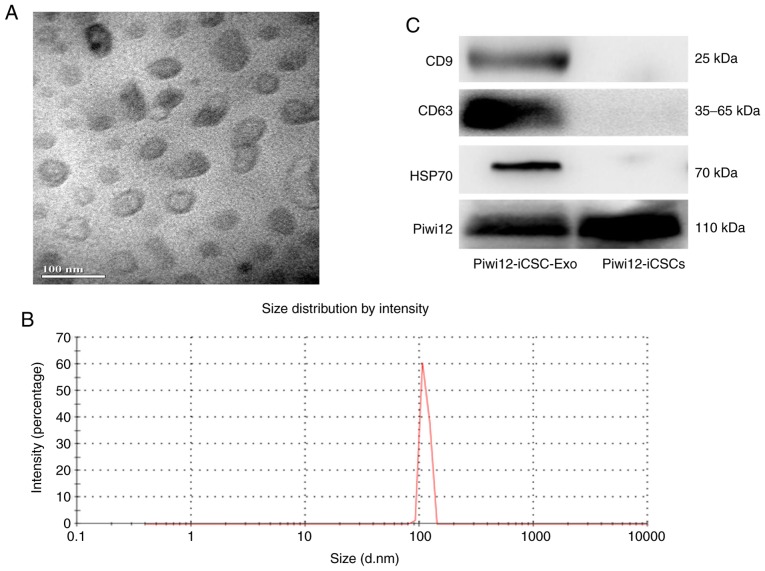
Exosome morphology was examined by TEM. As shown in Fig. 1A, Piwil2-iCSC-Exo are lipid bilayer-coated membrane structures ranging from 30 to 100 nm in diameter. NTA verified a vesicle population with a maximum size of 100 nm (Fig. 1B). The difference in the size distribution of exosomes between NTA and electron microscopy may be due to the possible aggregation of exosomes during the NTA analysis (37). Further investigation of the exosome markers revealed by western blot analysis, confirmed that Piwil2-iCSC-Exo expressed CD63, CD9, HSP70 and Piwil2 (Fig. 1C). At present, the majority of researchers do not detect any housekeeping gene. In this study, GAPDH was selected as a housekeeping gene; however, no bands were detected in the exosomes. Thus, the loading control was not included in Fig. 1C.
Figure 1.
Characterization of Piwil2-iCSC-Exo. (A) Morphology as shown by electron microscopy. (B) Size distribution of exosomes. (C) CD63, CD9, HSP70 and Piwil2 expression. The figure presents representative results of at least 3 independent experiments. Piwil2-iCSC-Exo, exosomes derived from Piwil2-induced cancer stem cells.
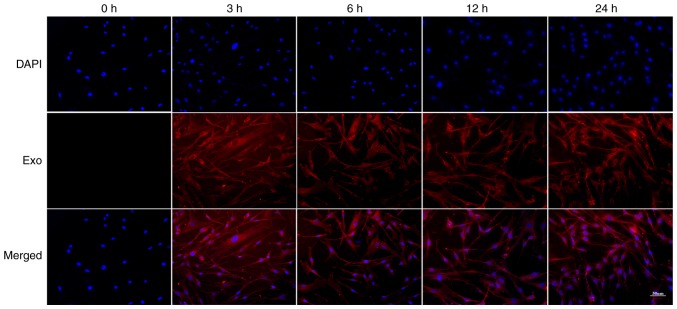
Uptake of Piwil2-iCSC-Exo by FBs
To examine whether FBs can internalize Piwil2-iCSC-Exo, the FBs were incubated with PKH26-labeled Piwil2-iCSC-Exo for 0, 3, 6, 12 and 24 h. The labeled Piwil2-iCSC-Exo was shown to enter the cells in a time-dependent manner. Following 3 and 6 h of co-culture, the exosomes entered the cells, and at 12 h, the exosomes began to accumulate in the cytoplasm. The accumulation of exosomes was time-dependent and reached a maximum in this study at 24 h (Fig. 2).
Figure 2.
Fluorescence microscopy of FBs and Piwil2-iCSC-Exo (80 µg/ml) following co-incubation for 0, 3, 6, 12 and 24 h (×200 magnification). FBs, fibroblasts; Piwil2-iCSC-Exo, exosomes derived from Piwil2-induced cancer stem cells.
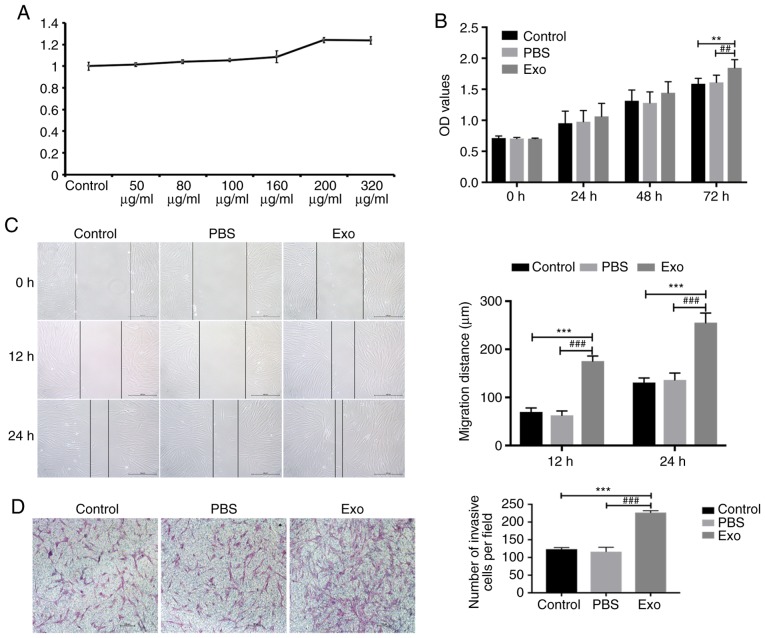
Piwil2-iCSC-Exo enhance the proliferation, migration and invasion of FBs
In the optimization phase, it was found that the high concentration group, namely concentrations of 200 and 320 µg/ml, markedly influenced cell proliferation (Fig. 3A). In these settings, the concentration of 200 µg/ml was more effective than that of 320 µg/ml. The lack of dose-dependency in this case may be due to the low concentration of exosomes in the suspension, resulting in the significant dilution of the culture medium with the vehicle (PBS) that in consequence, affected cell growth. Therefore, in the subsequent experiments, the concentration of 200 µg/ml of exosomes was used only. The potential effect of Piwil2-iCSC-Exo on the proliferation of FBs was analyzed by CCK-8 cell proliferation assay. Compared to the control groups, the exosomes exhibited an increased cell proliferation rate at 72 h (Fig. 3B). The continued exploration into the effects of Piwil2-iCSC-Exo on FB migration was carried out by performing a wound healing assay. Following 12 h of incubation with the exosomes, FB motility significantly increased and the wound was almost closed after 24 h (Fig. 3C). No significant differences were observed between the control group and PBS group at 12 and 24 h (P>0.05; Fig. 3B). Furthermore, in order to investigate whether Piwil2-iCSC-Exo affect the invasion of FBs, a Transwell assay was performed. Similar to the wound healing assay, the results revealed that the exosomes enhanced the invasive ability of the FBs (Fig. 3D) compared with that observed in the control groups.
Figure 3.
Piwil2-iCSC-Exo (200 µg/ml) enhance FB proliferation, migration and invasion. (A) The optimization experiments. (B) Proliferation of FBs after 0, 24, 48 and 72 h of incubation with Piwil2-iCSC-Exo. (C) Wound healing assays; representative images after 0, 12 and 24 h (×100 magnification). (D) Invasion assay; representative images (×100 magnification). At least 3 independent experiments were performed. Results were considered statistically significant at P<0.05 (**P<0.01, ***P<0.001 vs. control group; ##P<0.01, ###P<0.001 vs. PBS group). One-way ANOVA and the LSD post hoc test were selected for analysis. FBs, fibroblasts; Piwil2-iCSC-Exo, exosomes derived from Piwil2-induced cancer stem cells.
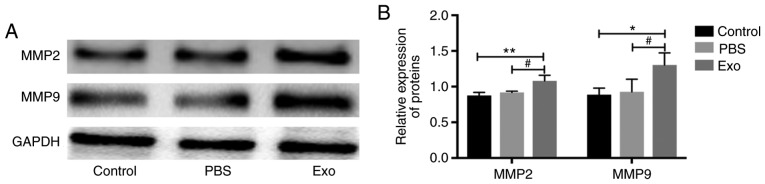
Piwil2-iCSC-Exo enhanced the expression of MMP2 and MMP9 proteins in FBs
MMP2 and MMP9 are matrix mellatoproteases involved in cancer progression and invasion and their expression is considered a marker of cell invasiveness (38–41). In order to investigate the likelihood that Piwil2-iCSC-Exo can increase the invasive properties of FB cells, MMP2 and MMP9 expression levels were measured by western blot analysis. Incubation with Piwil2-iCSC-Exo significantly increased the expression of MMP2 (P<0.01 vs. the control group, P<0.05 vs. the PBS group) and MMP9 (P<0.05) in comparison to the control groups. No statistically significant differences were noted between the control group and the PBS group (P>0.05; Fig. 4).
Figure 4.
MMP2 and MMP9 expression levels in FBs following incubation with Piwil2-iCSC-Exo (200 µg/ml). GAPDH was used as a loading control. At least three independent experiments were conducted. Results were considered statistically significant at P<0.05 (*P<0.05, **P<0.01 vs. control group; #P<0.05 vs. PBS group). One-way ANOVA and the LSD post hoc test were selected for analysis. FBs, fibroblasts; Piwil2-iCSC-Exo, exosomes derived from Piwil2-induced cancer stem cells; MMP, matrix metalloproteinase.
Piwil2-iCSC-Exo promote the transformation of FBs into CAFs
CAFs are important components of the tumor microenvironment and are involved in tumor development (42). CAFs are permanently activated through the elevated expression of specific markers, such as FAP, α-SMA and vimentin (43). As shown in Fig. 5, incubation of the FBs with Piwil2-iCSC-Exo increased the expression of α-SMA (P<0.05), vimentin (P<0.01 vs. the control group, P<0.05 vs. the PBS group) and FAP (P<0.001 vs. the control group, P<0.01 vs. the PBS group) in comparison to the control groups.
Figure 5.
Piwil2-iCSC-Exo (200 µg/ml) promotes the transformation of FBs into CAFs. α-SMA, vimentin and FAP expression levels were measured by western blot analysis. GAPDH was used as a loading control. At least 3 independent experiments were conducted. Results were considered statistically significant at P<0.05 (*P<0.05, **P<0.01, ***P<0.001 vs. control group; #P<0.05, ##P<0.01 vs. PBS group). One-way ANOVA and the LSD post hoc test were selected for analysis. FBs, fibroblasts; Piwil2-iCSC-Exo, exosomes derived from Piwil2-induced cancer stem cells; α-SMA, α-smooth activated protein; FAP, fibroblast-activated protein.
Discussion
Previous studies have confirmed that CSCs are the primary determinant of tumor initiation, propagation, metastasis and recurrence (12–15). However, the exact mechanisms through which CSCs promote tumor development remain unknown. A growing body of data suggest that there is a strong association between exosomes and tumor development (24–26). Exosomes, released by various types of cells, can mediate the biological activities of recipient cells through their contents, including proteins, nucleic acids and lipids. Thus, it was hypothesized that CSC-derived exosomes may promote tumor development by inducing changes in the tumor microenvironment. The results of this study support this hypothesis, as the CSC-derived exosomes significantly enhanced proliferation, migration and invasion of FBs, a major cell-type of the tumor microenvironment. These data suggest that the enhanced migration and invasion may be caused by an increased metalloproteinase activity in FBs. More importantly, it was demonstrated that CSC-derived exosomes can induce the CAF-type phenotype in stromal FBs.
Due in part to the low number of CSCs in tumors and the difficulties encountered in the purification of CSCs from tumor tissues, direct studies on native CSCs remain challenging. Therefore, this study used Piwil2-iCSC reprogrammed cells, transfected with the self-renewing gene Piwil2 (36), that served as a CSC model for in vitro experiments. Using this model, it was demonstrated that Piwil2-iCSC-Exo enhance the proliferation, migration and invasion of FBs in vitro. Similar to the observations in this study, previous studies have suggested that exosomes derived from advanced tumors can enhance cell proliferation and cell motility (44–46). Further evidence has confirmed that stem cell-derived exosomes can carry pluripotent transcription factors, such as Nanog, Oct-4 and Wnt family proteins, which promote the self-renewal of the recipient cells by altering cell plasticity (47,48). Sánchez et al demonstrated that human prostate CSC-derived exosomes can promote the proliferation and migration of prostate FBs through the activation of miR-139 (49). Another study revealed that thyroid tumor stem cell-like exosomes promote distant metastasis formation through non-coding RNAs (lncRNAs) (13). Furthermore, CD105+ renal CSC-derived exosomes activate angiogenesis and promote lung metastasis in vivo through the release of VEGF and MMP2 (50). Some studies have observed that the tetraspanin family of proteins, such as CD9 and CD63, are likely involved in cell proliferation, cell motility and metastasis (51,52). It was thus speculated that the bioactive substances contained in Piwil2-iCSC-Exo may alter the biological behavior of FBs.
Metastasis formation depends on the ability of the tumor cells to degrade the extracellular matrix and destroy the basement membrane (2). MMPs are the most effective proteases for degrading the extracellular matrix and are implicated in multiple steps of tumorigenesis, as well as in tumor invasion and metastasis formation (38,39). MMP2 and MMP9 are the most distinctive MMPs characterized by a strong proteolytic activity in the extracellular matrix (40,41). Multiple studies have reported that MMP9 is overexpressed in tumor cells and is thus linked to metastasis formation and ultimately, a poor prognosis (53,54). Zhang et al (55) reported that the overexpression of MMP9 can promote metastasis formation in non-small cell lung cancer. It has also been shown that MMP2 and MMP9 may contribute to metastasis in gastric adenocarcinoma (40). This study demonstrated that the expression of MMP2 and MMP9 in FBs increased in the presence of Piwil2-iCSC-Exo, an increase likely related to the invasiveness and motility of the exposed cells.
CAFs are important components of the tumor microenvironment and have been closely associated with the occurrence and development of tumors. CAFs are constitutively activated via the elevated expression of specific markers such as α-SMA, vimentin, as well as FAP (42,43). It has been shown that normal FBs can be induced to differentiate into CAFs by exposure to their surrounding tumor cells (27,56). In this study, the expression of α-SMA, vimentin and FAP was increased in FBs exposed to Piwil2-iCSC-Exo, suggesting that Piwil2-iCSC-Exo can induce the transformation of normal FBs into CAFs. Taken together, it can be hypothesized that CSC-derived exosomes can promote the development of tumors by altering the composition of the tumor microenvironment.
In conclusion, the findings of this study provide new evidence that exosomes derived from CSCs may promote tumor progression and the development of distant metastasis by transforming the composition of the tumor microenvironment. The evidence presented herein confirms that exosomes play a role in promoting FB proliferation, migration and invasion. The data contribute to a better understanding of the complex association between the CSCs and tumor development, which in turn could help to develop a potential cancer-microenvironment targeted therapy.
Acknowledgements
Not applicable.
Glossary
Abbreviations
- CSCs
cancer stem cells
- Piwil2-iCSCs
Piwil2 induced cancer stem cells
- FBs
fibroblasts
- Piwil2-iCSC-Exo
exosomes derived from Piwil2-iCSCs
- CAFs
cancer-associated fibroblasts
- DMEM
Dulbecco's modified Eagle's medium
- PBS
phosphate-buffered saline
- PVDF
polyvinylidene fluoride
- TEM
transmission electron microscopy
- NTA
nanoparticle tracking analysis
- MMPs
matrix metalloproteinases
Funding
The present study was supported by the Special Project of Science and Technology Innovation for Social Undertakings and Livelihood Guarantee of Chongqing (grant no. cstc2017shmsA130055 and no. cstc2017shmsA130103).
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors' contributions
DZ and DL performed the experiments. DHu and BT analyzed the results. WG, ZW, ZZ and LS performed the statistical analysis. GW, DHe and DZ designed all the experiments. DZ wrote the manuscript. LS, GW and DoH edited the manuscript. All authors contributed to the revision of the manuscript and approved the final version for publication. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.López-Gómez M, Malmierca E, de Górgolas M, Casado E. Cancer in developing countries: The next most preventable pandemic. The global problem of cancer. Crit Rev Oncol Hematol. 2013;88:117–122. doi: 10.1016/j.critrevonc.2013.03.011. [DOI] [PubMed] [Google Scholar]
- 2.Liao WT, Ye YP, Deng YJ, Bian XW, Ding YQ. Metastatic cancer stem cells: From the concept to therapeutics. Am J Stem Cells. 2014;3:46–62. [PMC free article] [PubMed] [Google Scholar]
- 3.Kreso A, Dick J. Evolution of the cancer stem cell model. Cell Stem Cell. 2014;14:275–291. doi: 10.1016/j.stem.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Ponti D, Costa A, Zaffaroni N, Pratesi G, Petrangolini G, Coradini D, Pilotti S, Pierotti MA, Daidone MG. Isolation and in vitro propagation of tumorigenic breast cancer cells with stem/progenitor cell properties. Cancer Res. 2005;65:5506–5511. doi: 10.1158/0008-5472.CAN-05-0626. [DOI] [PubMed] [Google Scholar]
- 5.Costa FF, Le Blanc K, Brodin B. Concise review: Cancer/testis antigens, stem cells, and cancer. Stem Cells. 2010;25:707–711. doi: 10.1634/stemcells.2006-0469. [DOI] [PubMed] [Google Scholar]
- 6.Kim KM, Calabrese P, Tavaré S, Shibata D. Enhanced stem cell survival in familial adenomatous polyposis. Am J Pathol. 2004;164:1369–1377. doi: 10.1016/S0002-9440(10)63223-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kucia M, Ratajczak MZ. Stem cells as a two edged sword-from regeneration to tumor formation. J Physiol Pharmacol. 2006;57(Suppl 7):S5–S16. [PubMed] [Google Scholar]
- 8.Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. Nature. 2001;414:105–111. doi: 10.1038/35102167. [DOI] [PubMed] [Google Scholar]
- 9.Visvader JE. Cells of origin in cancer. Nature. 2011;469:314–322. doi: 10.1038/nature09781. [DOI] [PubMed] [Google Scholar]
- 10.Prasetyanti PR, Medema JP. Intra-tumor heterogeneity from a cancer stem cell perspective. Mol Cancer. 2017;16:41. doi: 10.1186/s12943-017-0600-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aguilar-Gallardo C, Simón C. Cells, stem cells, and cancer stem cells. Semin Reprod Med. 2013;31:005–013. doi: 10.1055/s-0032-1331792. [DOI] [PubMed] [Google Scholar]
- 12.Phi LTH, Sari IN, Yang YG, Lee SH, Jun NY, Kim KS, Lee KY, Kwon HY. Cancer stem cells (CSCs) in drug resistance and their therapeutic implications in cancer treatment. Stem Cells Int. 2018;2018:5416923. doi: 10.1155/2018/5416923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hardin H, Helein H, Meyer K, Robertson S, Zhang RR, Zhong WX, Lloyd RV. Thyroid cancer stem-like cell exosomes: Regulation of EMT via transfer of lncRNAs. Lab Invest. 2018;98:1133–1142. doi: 10.1038/s41374-018-0065-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Valery AC, Golam K, Xia L, Mary D, Junk DJ, Dongyin G, Chris H, Monica V, Erin MH, Maksim S. Cancer stem cells: Targeting the roots of cancer, seeds of metastasis, and sources of therapy resistance. Cancer Res. 2015;75:924–929. doi: 10.1158/0008-5472.CAN-14-3225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hermann PC, Huber SL, Herrler T, Aicher A, Ellwart JW, Guba M, Bruns CJ, Heeschen C. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell. 2007;1:313–323. doi: 10.1016/j.stem.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Albini A, Bruno A, Gallo C, Pajardi G, Noonan DM, Dallaglio K. Cancer stem cells and the tumor microenvironment: Interplay in tumor heterogeneity. Connect Tissue Res. 2015;56:414–425. doi: 10.3109/03008207.2015.1066780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin WW, Karin M. A cytokine-mediated link between innate immunity, inflammation, and cancer. J Clin Invest. 2007;117:1175–1183. doi: 10.1172/JCI31537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sittichai K. The tumor microenvironment contribution to development, growth, invasion and metastasis of head and neck squamous cell carcinomas. J Cancer. 2013;4:66–83. doi: 10.7150/jca.5112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sund M, Kalluri R. Tumor stroma derived biomarkers in cancer. Cancer Metastasis Rev. 2009;28:177–183. doi: 10.1007/s10555-008-9175-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caby MP, Lankar D, Vincendeau-Scherrer C, Raposo G, Bonnerot C. Exosomal-like vesicles are present in human blood plasma. Int Immunol. 2005;17:879–887. doi: 10.1093/intimm/dxh267. [DOI] [PubMed] [Google Scholar]
- 21.Paul G, Alexander S, Svenja R, Daniela G, Steffen R, Condon TP, Alexander M, Minh-Chau P, Otwin L, Alexander S. Cleavage of L1 in exosomes and apoptotic membrane vesicles released from ovarian carcinoma cells. Clin Cancer Res. 2005;11:2492–2501. doi: 10.1158/1078-0432.CCR-04-1688. [DOI] [PubMed] [Google Scholar]
- 22.Valadi H, Ekström K, Bossios A, Sjöstrand M, Lee JJ, Lötvall JO. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat Cell Biol. 2007;9:654–659. doi: 10.1038/ncb1596. [DOI] [PubMed] [Google Scholar]
- 23.Hannafon BN, Ding WQ. Intercellular communication by exosome-derived microRNAs in cancer. Int J Mol Sci. 2013;14:14240–14269. doi: 10.3390/ijms140714240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jiang S, Hu C, Liu P, Lu M. Tumor-derived exosomes in cancer metastasis risk diagnosis and metastasis therapy. Clin Transl Oncol. 2019;21:152–159. doi: 10.1007/s12094-018-1918-0. [DOI] [PubMed] [Google Scholar]
- 25.Abak A, Abhari A, Rahimzadeh S. Exosomes in cancer: Small vesicular transporters for cancer progression and metastasis, biomarkers in cancer therapeutics. PeerJ. 2018;6:e4763. doi: 10.7717/peerj.4763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sharma A. Role of stem cell derived exosomes in tumor biology. Int J Cancer. 2018;142 doi: 10.1002/ijc.31089. [DOI] [PubMed] [Google Scholar]
- 27.Bhowmick NA, Neilson EG, Moses HL. Stromal fibroblasts in cancer initiation and progression. Nature. 2004;432:332–337. doi: 10.1038/nature03096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lu Y, Yang W, Qin C, Zhang LF, Deng JJ, Liu SB, Qin ZH. Responsiveness of stromal fibroblasts to IFN-gamma blocks tumor growth via angiostasis. J Immunol. 2009;183:6413–6421. doi: 10.4049/jimmunol.0901073. [DOI] [PubMed] [Google Scholar]
- 29.Gao JX. Cancer stem cells: The lessons from pre-cancerous stem cells. J Cell Mol Med. 2008;12:67–96. doi: 10.1111/j.1582-4934.2007.00170.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li D, Sun X, Yan D, Huang J, Luo Q, Tang H, Peng Z. Piwil2 modulates the proliferation and metastasis of colon cancer via regulation of matrix metallopeptidase 9 transcriptional activity. Exp Biol Med (Maywood) 2012;237:1231–1240. doi: 10.1258/ebm.2012.011380. [DOI] [PubMed] [Google Scholar]
- 31.Liu JJ, Shen R, Chen L, Ye Y, He G, Hua K, Jarjoura D, Nakano T, Ramesh GK, Shapiro CL, et al. Piwil2 is expressed in various stages of breast cancers and has the potential to be used as a novel biomarker. Int J Clin Exp Pathpl. 2010;3:328–337. [PMC free article] [PubMed] [Google Scholar]
- 32.He G, Chen L, Ye Y, Xiao Y, Hua K, Jarjoura D, Nakano T, Barsky SH, Shen R, Gao JX. Piwil2 expressed in various stages of cervical neoplasia is a potential complementary marker for p16. Am J Transl Res. 2010;2:156–169. [PMC free article] [PubMed] [Google Scholar]
- 33.Chen C, Liu J, Xu G. Overexpression of PIWI proteins in human stage III epithelial ovarian cancer with lymph node metastasis. Cancer Biomark. 2013;13:315–321. doi: 10.3233/CBM-130360. [DOI] [PubMed] [Google Scholar]
- 34.Wang Y, Liu Y, Shen X, Zhang X, Chen X, Yang C, Gao H. The PIWI protein acts as a predictive marker for human gastric cancer. Int J Clin Exp Pathol. 2012;5:315–325. [PMC free article] [PubMed] [Google Scholar]
- 35.Greither T, Koser F, Kappler M, Bache M, Lautenschläger C, Göbel S, Holzhausen HJ, Wach S, Wurl P, Taubert H. Expression of human Piwi-like genes is associated with prognosis for soft tissue sarcoma patients. BMC Cancer. 2012;12:272. doi: 10.1186/1471-2407-12-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang D, Wu X, Liu X, Cai C, Zeng G, Rohozinski J, Zhang Y, Wei G, He D. Piwil2-transfected human fibroblasts are cancer stem cell-like and genetically unstable. Oncotarget. 2017;8:12259–12271. doi: 10.18632/oncotarget.14696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xue M, Chen W, Xiang A, Wang R, Chen H, Pan J, Pang H, An H, Wang X, Hou H, Li X. Hypoxic exosomes facilitate bladder tumor growth and development through transferring long non-coding RNA-UCA1. Mol Cancer. 2017;16:143. doi: 10.1186/s12943-017-0714-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Deryugina EI, Quigley JP. Tumor angiogenesis: MMP- mediated induction of intravasation- and metastasis-sustaining neovasculature. Matrix Biol. 2015;44-46:94–112. doi: 10.1016/j.matbio.2015.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yamamoto K, Murphy G, Troeberg L. Extracellular regulation of metalloproteinases. Matrix Biol. 2015;44-46:255–263. doi: 10.1016/j.matbio.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 40.Huang Q, Lan F, Wang X, Yu Y, Ouyang X, Zheng F, Han J, Lin Y, Xie Y, Xie F, et al. IL-1β-induced activation of p38 promotes metastasis in gastric adenocarcinoma via upregulation of AP-1/c-fos, MMP2 and MMP9. Molecular cancer. 2014;13:18. doi: 10.1186/1476-4598-13-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liu J, Ping W, Zu Y, Sun W. Correlations of lysyl oxidase with MMP2/MMP9 expression and its prognostic value in non-small cell lung cancer. Int J Clin Exp Pathol. 2014;7:6040–6047. [PMC free article] [PubMed] [Google Scholar]
- 42.Shimoda M, Mellody KT, Orimo A. Carcinoma-associated fibroblasts are a rate-limiting determinant for tumour progression. Semin Cell Dev Biol. 2010;21:19–25. doi: 10.1016/j.semcdb.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Liu R, Li H, Liu L, Yu J, Ren X. Fibroblast activation protein: A potential therapeutic target in cancer. Cancer Biol Ther. 2015;13:123–129. doi: 10.4161/cbt.13.3.18696. [DOI] [PubMed] [Google Scholar]
- 44.Wu L, Zhang X, Zhang B, Shi H, Yuan X, Sun Y, Pan Z, Qian H, Xu W. Exosomes derived from gastric cancer cells activate NF-κB pathway in macrophages to promote cancer progression. Tumour Biol. 2016;37:12169–12180. doi: 10.1007/s13277-016-5071-5. [DOI] [PubMed] [Google Scholar]
- 45.Gangoda L, Liem M, Ang CS, Keerthikumar S, Adda CG, Parker BS, Mathivanan S. Proteomic profiling of exosomes secreted by breast cancer cells with varying metastatic potential. Proteomics. 2017;17 doi: 10.1002/pmic.201600370. [DOI] [PubMed] [Google Scholar]
- 46.Sakha S, Muramatsu T, Ueda K, Inazawa J. Exosomal microRNA miR-1246 induces cell motility and invasion through the regulation of DENND2D in oral squamous cell carcinoma. Sci Rep. 2016;6:38750. doi: 10.1038/srep38750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tooi M, Komaki M, Morioka C, Honda I, Iwasaki K, Yokoyama N, Ayame H, Izumi Y, Morita I. Placenta mesenchymal stem cell derived exosomes confer plasticity on fibroblasts. J Cell Biochem. 2016;117:1658–1670. doi: 10.1002/jcb.25459. [DOI] [PubMed] [Google Scholar]
- 48.Julia Christina G, Varun C, Kerstin B, Michael B. Active Wnt proteins are secreted on exosomes. Nat Cell Biol. 2012;14:1036–1045. doi: 10.1038/ncb2574. [DOI] [PubMed] [Google Scholar]
- 49.Sánchez CA, Andahur EI, Valenzuela R, Castellón EA, Fullá JA, Ramos CG, Triviño JC. Exosomes from bulk and stem cells from human prostate cancer have a differential microRNA content that contributes cooperatively over local and pre-metastatic niche. Oncotarget. 2016;7:3993–4008. doi: 10.18632/oncotarget.6540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Grange C, Tapparo M, Collino F, Vitillo L, Damasco C, Deregibus MC, Tetta C, Bussolati B, Camussi G. Microvesicles released from human renal cancer stem cells stimulate angiogenesis and formation of lung premetastatic niche. Cancer Research. 2011;71:5346–5356. doi: 10.1158/0008-5472.CAN-11-0241. [DOI] [PubMed] [Google Scholar]
- 51.Berditchevski F. Complexes of tetraspanins with integrins: More than meets the eye. J Cell Sci. 2001;114:4143–4151. doi: 10.1242/jcs.114.23.4143. [DOI] [PubMed] [Google Scholar]
- 52.Mantegazza AR, Barrio MM, Moutel S, Bover L, Weck M, Brossart P, Teillaud JL, Mordoh J. CD63 tetraspanin slows down cell migration and translocates to the endosomal-lysosomal-MIICs route after extracellular stimuli in human immature dendritic cells. Blood. 2004;104:1183–1190. doi: 10.1182/blood-2004-01-0104. [DOI] [PubMed] [Google Scholar]
- 53.Roy R, Yang J, Moses MA. Matrix metalloproteinases as novel biomarkers and potential therapeutic targets in human cancer. J Clin Oncol. 2009;27:5287–5297. doi: 10.1200/JCO.2009.23.5556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nart D, Yaman B, Yilmaz F, Zeytunlu M, Karasu Z, Kiliç M. Expression of matrix metalloproteinase-9 in predicting prognosis of hepatocellular carcinoma after liver transplantation. Liver Transpl. 2010;16:621–630. doi: 10.1002/lt.22028. [DOI] [PubMed] [Google Scholar]
- 55.Zhang W, Zhang T, Lou Y, Yan B, Cui S, Jiang L, Han B. Placental growth factor promotes metastases of non-small cell lung cancer through MMP9. Cell Physiol Biochem. 2015;37:1210–1218. doi: 10.1159/000430244. [DOI] [PubMed] [Google Scholar]
- 56.Yu L, Yang W, Qin C, Zhang L, Deng J, Liu S, Qin Z. Responsiveness of stromal fibroblasts to IFN-gamma blocks tumor growth via angiostasis. J Immunol. 2009;183:6413–6421. doi: 10.4049/jimmunol.0901073. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.