Abstract
Background
It is unknown whether previously noted racial disparities in the use of metabolic and bariatric surgery (MBS) for the management of pediatric obesity could be mitigated by accounting for primary insurance.
Objectives
To examine utilization of pediatric MBS across race and insurance in the U.S.
Setting
Retrospective cross-sectional study.
Methods
The National Inpatient Sample was used to identify patients 12–19 years old undergoing MBS from 2015–2016, and these data were combined with national estimates of pediatric obesity obtained from the 2015–2016 National Health and Nutrition Examination Survey. Severe obesity was defined as class III obesity, or class II obesity plus hypertension, dyslipidemia, or diabetes mellitus.
Results
1,659,507 (5.0%) adolescents with severe obesity were identified, consisting of 35.0% female, 38.0% white, and 45.0% privately insured adolescents. Over the same time period, 2,535 MBS procedures were performed. Most surgical patients were female (77.5%), white (52.8%), and privately insured (57.5%). Black and Hispanic adolescents were less likely to undergo MBS than whites (OR 0.50, 0.46 respectively; p<0.001 both), despite adjusting for primary insurance. White adolescents covered by Medicaid were significantly more likely to undergo MBS than privately insured whites (OR 1.66; p<0.001), while the opposite was true for black and Hispanic adolescents (OR 0.29, 0.75 respectively; p<0.001 both).
Conclusions
Pediatric obesity disproportionately affects racial minorities, yet MBS is most often performed on white adolescents. Medicaid insurance further decreases the use of MBS among non-white adolescents, while paradoxically increasing it for whites, suggesting insurance reform alone is unlikely to eliminate this race-based disparity.
Keywords: Pediatric obesity, Metabolic and Bariatric Surgery, Healthcare Disparities
INTRODUCTION
Pediatric obesity is a national public health crisis involving more than 13 million children and adolescents in the United States (U.S.), and affecting black and Hispanic youth at significantly higher rates than whites.(1,2) Recent studies have demonstrated superior weight loss and improvement of cardiovascular risk factors among youth with obesity treated with metabolic and bariatric surgery (MBS) relative to those treated with medical therapy or lifestyle interventions alone.(3) Moreover, adolescents who undergo MBS experience remission of cardiovascular comorbidities more often than adults(4), which highlights the importance of prompt treatment of this severe disease in order to prevent its long-term deleterious effects.
Significant disparities in the use of MBS attributable to race, insurance, and socioeconomic status (SES) have been demonstrated among adult patients.(5) In the pediatric population, there is a suggestion that similar race-based disparities may exist, but previous studies have been unable to account for insurance,(6) leaving unanswered the question of whether these differences merely reflect inherent SES variations related to race rather than independent race-based disparities.
Such a relationship has been difficult to elucidate due to the lack of a single nationwide database that captures both the exposed (i.e. children and adolescents with severe obesity) and treatment (i.e. surgical) cohorts. To address this limitation, our study combined two national databases to examine the relationship between sex, race, insurance, and utilization of MBS for the treatment of severe pediatric obesity in the U.S.
MATERIALS AND METHODS
Data source and Patient Selection
The National Inpatient Sample (NIS) was used to identify patients 12–19 years old who underwent MBS from 2015–2016 (Supplemental Table 1). Bariatric operations included: open Roux-en-Y gastric bypass (RYGB), laparoscopic Roux-en-Y gastric bypass (LRYGB), sleeve gastrectomy (SG), laparoscopic adjustable gastric band (LAGB), vertical banded gastroplasty (VBG), and biliary pancreatic diversion/duodenal switch (BPD/DS). Age, sex, race, and primary insurance were also extracted. NIS was developed for the Healthcare Cost and Utilization Project (HCUP), and it is the largest publicly available all-payer database, capturing a 20% stratified sample of all discharges for patients of all ages admitted to non-federal, non-rehabilitation hospitals.(7) National estimates of MBS utilization were calculated using sampling weights provided by HCUP. It has been previously demonstrated that calculation of pediatric obesity rates using International Classification of Diseases (ICD) codes results in gross underestimates,(8) hence NIS data should not be used alone to perform adjusted analyses related to pediatric obesity.
To overcome this limitation, the 2015–2016 National Health and Nutrition Examination Survey (NHANES)(9) was used to obtain national estimates of severe pediatric obesity among adolescents 12–19 years old. In accordance with the 2018 American Society for Metabolic and Bariatric Surgery (ASMBS) guidelines for the management of pediatric obesity, severe obesity was defined as class III obesity (BMI ≥140% of the 95th percentile for age and sex, or ≥40 kg/m2, whichever is lower), or class II obesity (BMI ≥120% of the 95th percentile for age and sex, or ≥35 kg/m2, whichever is lower) plus an obesity-related comorbidity.(10) NHANES does not capture all comorbidities included in the 2018 ASMBS guidelines, so for the purpose of this study, hypertension (HTN), dyslipidemia (DL) and diabetes mellitus (DM) were extracted. NHANES is widely considered the gold standard for obtaining obesity estimates in the U.S., given that it is the only nationally representative survey that includes in-person height and weight measurements rather than self-reports,(11) along with vital signs measurements and lab draws.
Statistical analysis
Univariate analyses were completed for each database using Student’s t-test and Pearson chi-square. Given that the exposed (i.e. adolescents with severe obesity) and treated (i.e. adolescents status post MBS) cohorts were obtained from two different databases, neither of which provides a patient identifier, the data used in our analysis was not linked at the individual patient level. Therefore, adjusted analyses of this combined dataset to explore the use of MBS as it relates to sex, race and insurance were performed using the Cochran-Mantel-Haenszel (CMH) method.(12) The CMH method is a technique commonly used to perform meta-analyses, which generates an adjusted odds ratio (OR), chi-square statistic, p-value, and 95% confidence intervals (CI) between an exposure and an outcome (as represented by 2×2 contingency tables), while adjusting for confounding variables through stratification (Supplemental Figure 1).(13) All statistical analyses were conducted using the Stata software package (version 15.1, StataCorp LP, College Station, TX).
RESULTS
The rate of severe obesity among adolescents 12–19 years old in 2015–2016 was 5.0%. This corresponds to 1,659,507 individuals (1,084,637 with class III obesity and 574,870 with class II obesity plus HTN, DL, or DM), of which 35.0% were female, 38.0% were white, and 45.0% had private insurance (Table 1). The mean age of adolescents with severe obesity was 16.4 years old (95% CI 15.9 – 16.9), and it did not differ by sex, race, or insurance. The age-adjusted rate of severe obesity was higher among racial minorities than whites (black 8.6%, Hispanic 8.4%, white 4.1%; p=0.03), but did not significantly differ by sex (6.5% males vs. 3.9% females; p>0.10), or primary insurance (6.4% Medicaid vs. 4.7% private insurance; p>0.10). The rates of HTN, DL, and DM among all adolescents with severe obesity were 26.8%, 46.1%, and 3.6% respectively, and they did not differ by race or insurance.
Table 1:
Unadjusted rates and National Population Estimates of Adolescents 12–19 years old with Severe Obesity (NHANES 2015–2016) and Adolescents 12–19 years old who Underwent MBS (NIS 2015–2016)
| Demographics and Unadjusted Analysis | |||
|---|---|---|---|
| Severe Obesity | MBS | ||
| n = 1,659,507 | n = 2,535 | P value | |
| Age (years, mean ± SD) | 16.4 ± 2.4 | 18.0 ± 0.1 | <0.001 |
| Sex, n (%) | |||
| Males | 1,078,700 (65.0) | 570 (22.5) | <0.001 |
| Females | 580,807 (35.0) | 1,965 (77.5) | |
| Race, n (%) | |||
| White | 631,040 (38.0) | 1,255 (52.8) | <0.001 |
| Black | 401,481 (24.2) | 375 (15.8) | |
| Hispanic | 612,766 (36.9) | 595 (25.1) | |
| Insurance, n (%) | |||
| Private | 746,158 (45.0) | 1,455 (57.5) | <0.001 |
| Medicaid | 525,105 (31.6) | 820 (32.4) | |
There were 2,535 MBS procedures performed among adolescents 12–19 years old from 2015–2016, comprised of 2,005 (79.1%) SG, 510 (20.1%) LRYGB, and 15 (0.6%) RYGB. There were ≤10 LAGB, and zero VBG and BPD/DS throughout the study period. The mean age of surgical patients was 18.0 years old (95% CI 17.8–18.1 years old), and it did not differ by sex or race, but it did so by primary insurance (18.2 vs 17.6 years old, private insurance and Medicaid respectively; p<0.001). Most surgical patients were female (77.5%), white (52.8%), and privately insured (57.5%. Table 1). The rates of HTN, DL, and DM among surgical patients were 14.4%, 13.8%, and 9.8% respectively, and they did not differ by race or insurance.
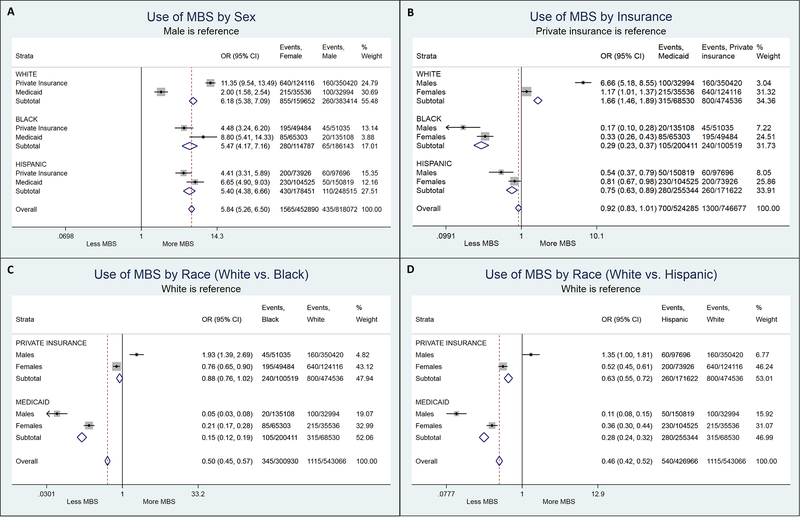
Multivariable analysis of combined NHANES/NIS data using the CMH method to stratify and adjust for sex, race, and insurance (Table 2) demonstrated female adolescents were more likely to undergo MBS than males (OR 5.84; p<0.001), while black and Hispanic adolescents were less likely to undergo MBS compared to whites (OR 0.50, 0.46 respectively; p<0.001 for both). On the other hand, there was no significant difference in utilization of MBS by primary insurance (OR 0.92 for Medicaid vs private insurance; p=0.07). Nevertheless, among black and Hispanic adolescents, Medicaid insurance was indeed associated with a decreased use of MBS regardless of sex (OR 0.29, 0.75 respectively; p<0.001 for both), while the opposite was observed for white adolescents, for whom Medicaid insurance conferred a higher likelihood of undergoing MBS (OR 1.66; p=0.001. Figure 1B). Analysis stratified by sex and insurance demonstrated privately insured black males were more likely to undergo MBS than their privately insured white counterparts (OR 1.93; p<0.001. Figure 1C).
Table 2:
Adjusted analysis of utilization of MBS based on combined NHANES and NIS data using Cochran-Mantel-Haenszel method
| Adjusted Analysis of Utilization of MBS | |||
|---|---|---|---|
| OR | 95% CI | P value | |
| Female sex | 5.84 | 5.26 – 6.50 | <0.001 |
| Race | |||
| White | ref | --- | --- |
| Black | 0.50 | 0.45 – 0.57 | <0.001 |
| Hispanic | 0.46 | 0.42 – 0.52 | <0.001 |
| Insurance | |||
| Private | ref | --- | --- |
| Medicaid | 0.92 | 0.83 – 1.01 | 0.07 |
Figure 1: Cochran-Mantel-Haenszel adjusted analyses and stratification.
A) Use of MBS by sex, adjusted for race and insurance. B) Use of MBS by insurance, adjusted for sex and race. C) Use of MBS for black vs. white adolescents, adjusted for sex and insurance. D) Use of MBS for Hispanic vs. white adolescents, adjusted for sex and insurance. * MBS: Metabolic and Bariatric Surgery
DISCUSSION
In this study, we found female adolescents were significantly more likely than males to undergo MBS for the management of severe obesity, while black and Hispanic adolescents were significantly less likely to undergo MBS compared to whites. Furthermore, a complex relationship between race, insurance, and sex was identified. Among racial minorities, Medicaid insurance was associated with further decreased likelihood of undergoing MBS when compared to their privately insured counterparts, while the opposite effect was observed among whites. This finding is in contrast to the common perception that public insurance acts as a barrier to care for all patients alike.
The race-based disparity observed in this study likely arises from a complex interplay of provider, patient, and systemic factors. Though our study is unable to comment on those specific factors, we believe it is important to propose potential contributing mechanisms rather than simply report our empiric data. Therefore, the remaining of this discussion is strictly the authors’ attempt at explaining the empiric findings of our study, while at the same time generating subsequent research hypotheses that should be tested through a combination of survey and mixed-method studies.
Among provider-related factors we must consider implicit bias, which can lead to disparate treatment recommendations and referral patterns for different patient populations.(14) Despite older reports of lower levels of pro-white implicit bias among pediatricians compared to adult providers, more recent studies have found significant levels of implicit racial bias indeed exist within the field,(15,16) and these have been shown to be associated with disparate treatment recommendations for a host of pediatric conditions.(17) One study by Wee et al. further explored the question of provider bias among adult patients with obesity, finding primary care physicians were less likely to discuss MBS with black patients compared to whites, even though the former were more likely to consider it once their physician introduced the option.(18)
Cultural differences and variations in treatment preferences among different patient populations certainly play a role in this observed race-based disparity. For example, Wee et al. additionally found adult black patients with obesity were less likely than whites to have considered MBS prior to presenting to their primary care office,(18) in part due to a perception of surgery as a high-risk method of last resort.(19) Interestingly, these differences dissipated after adjusting for quality of life, which was higher among black patients with obesity,(18) which further highlights the wide array of factors that can influence a patient’s decision to seek surgical evaluation.
Our study identified a complex relationship between sex, race, insurance and the use of pediatric MBS. White adolescents with Medicaid insurance had an increased use of MBS when compared to their privately insured counterparts, while the opposite was true for racial minorities. Similar findings were reported in a study by Birkmeyer et al., which identified a 1.8–2.2 times higher rate of MBS among white adult patients of low SES compared to whites of high SES, while the opposite was true for black adults.(20) One potential reason for this racial difference among Medicaid patients is the fact that non-white populations of lower SES are known to have higher levels of distrust towards the healthcare system than their white counterparts,(21) which may cause them to seek surgical care less often. Another possible contributor is the presence of intrinsic deficiencies in Medicaid insurance that result in a rate of initial coverage denial for pediatric MBS as high as 54%,(22) prompting the need for lengthy appeals. Unfortunately, minorities are less likely to navigate the appeal process successfully, as demonstrated by a study that examined federal disability benefits appeals data, and found white patients were more likely than blacks to have their appeals approved.(23) Lastly, we recognize that the fact that private insurance mitigates the race-based disparity among non-white males but not females is puzzling. Similar data were again presented by Birkmeyer et al. in their previously mentioned study, where they found the rate of MBS among black males of high SES was about 1.6 times that of their white counterparts.(20)
Our study has important implications. Its findings suggest that race-based disparities in the use of pediatric MBS are unlikely to be eliminated by policy changes focused solely on promoting expansion of government-sponsored insurance. In turn, they emphasize the need for interventions that specifically target provider-related factors such as implicit bias, and patient-related factors such as education about the deleterious effects of obesity as well as the risks and benefits of MBS. Further studies utilizing mixed-methodology are needed to better examine the journey from primary diagnosis of obesity to multidisciplinary evaluation in order to elucidate the stages at which disparities may arise. In the meantime, the insidious effects of implicit bias can be combatted in two ways. First, health systems should incorporate coordinated efforts such as cultural dexterity training and implicit bias rounds into their regular provider education,(24,25) in order to highlight the importance of combatting bias as a way to provide high quality care for all patients. Secondly, system-wide initiatives to improve and standardize care via best practice guidelines have been shown not only to improve quality for all, but also to reduce race and SES-based disparities.(26). We believe similar practice guidelines should be implemented in order to standardize the management of severe pediatric obesity at all stages, from primary care to multidisciplinary evaluation, in order to ensure all children and adolescents who suffer from this disease receive the best possible care regardless of gender, race, or SES. Ongoing parallel efforts should target patient education, especially at the primary care stage, focusing on helping individuals from different cultural backgrounds separate the physical appearance implications of obesity from its current and future medical consequences. This would allow for patients and their families to undergo a truly informed process, especially as they consider the importance of weight loss along with the need for referral for multidisciplinary evaluation, and the risks and benefits of MBS.
The combination of data from two national databases is a key strength of our study, though it does lead to some limitations. Due to sample size limitations inherent to the CMH method, adjustment for age was not possible. Nevertheless, given that neither the mean age of NHANES respondents with severe obesity nor the mean age of surgical patients differed by race, we believe our analyses related to race would not have differed significantly had we been able to adjust for age. Adjustment by income was also deferred given that both databases report it differently, however, we don’t believe our results would have significantly differed had we been able to adjust for income given the strict federal guidelines to qualify for Medicaid insurance. Lastly, as mentioned above, the reader must keep in mind that our study represents a population-level analysis, which despite elucidating a clear race-based disparity and a complex race-insurance interaction, does not allow us to comment on the specific mechanisms behind it, namely patient- and provider- related factors, as well as systematic barriers to care.
CONCLUSION
Despite higher rates of pediatric obesity and its deleterious effects, racial minorities are significantly less likely to undergo MBS, one of the most effective and durable treatments for this severe disease. Medicaid insurance further decreases utilization of MBS for non-white adolescents, while paradoxically increasing it for their white counterparts, which suggests insurance reform alone is unlikely to eliminate this disparity and could in fact worsen it. Rather, close examination of provider referral patterns and improvements of both provider and patient education are required in order to eliminate this disparity for this most vulnerable population.
Supplementary Material
Supplemental Table 1: ICD-9/10-CM Codes for NIS Inclusion and Exclusion Criteria
Supplemental Figure 1: Overview of the Cochran-Mantel-Haenszel (CMH) method: Formulas and Graphic Depiction of Analysis.
HIGHLIGHTS.
Severe obesity affects non-white adolescents more than whites.
Racial minorities are less likely to undergo MBS, despite accounting for primary insurance.
Medicaid increases the likelihood of undergoing MBS for white adolescents.
Medicaid further decreases the likelihood of undergoing MBS for non-white adolescents.
ACKNOWLEDGEMENTS
This work was conducted with statistical support from Harvard Catalyst | The Harvard Clinical and Translational Science Center (National Center for Advancing Translational Sciences, National Institutes of Health Award UL 1TR002541). The content is solely the responsibility of the authors and does not necessarily represent the official views of Harvard Catalyst, Harvard University and its affiliated academic healthcare centers, or the National Institutes of Health.
Financial Disclosure:
Maggie L. Westfal is financially supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under award number T32DK007754.
Fatima Cody Stanford, MD MPH MPA is financially supported by the National Institute of Diabetes and Digestive and Kidney Diseases of the National Institutes of Health under awards number P30DK040561 and L30DK118710. She is additionally an advisor for Novo Nordisk, for which she has received consulting fees.
Numa P. Perez, MD is financially supported by the Massachusetts General Hospital Healthcare Transformation Lab, Healthcare Innovation Research Fellowship.
The remaining authors of this paper have nothing to disclose.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest relevant to this manuscript to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of Obesity and Severe Obesity in US Children, 1999–2016. Pediatrics. 2018. February 26;24(5):1116–23. [Google Scholar]
- 2.Mayer-Davis EJ, Lawrence JM, Dabelea D, et al. Incidence Trends of Type 1 and Type 2 Diabetes among Youths, 2002–2012. N Engl J Med. 2017;376(15):1419–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Inge TH, Laffel LM, Jenkins TM, et al. Comparison of surgical and medical therapy for type 2 diabetes in severely obese adolescents. JAMA Pediatr. 2018;172(5):452–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Inge TH, Courcoulas AP, Jenkins TM, et al. Five-Year Outcomes of Gastric Bypass in Adolescents as Compared with Adults. N Engl J Med. 2019;380(22):2136–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin M, Beekley A, Kjorstad R, Sebesta J. Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obes Relat Dis. 2010;6(1):8–15. [DOI] [PubMed] [Google Scholar]
- 6.Nunez Lopez O, Jupiter DC, Bohanon FJ, Radhakrishnan RS, Bowen-Jallow KA. Health Disparities in Adolescent Bariatric Surgery: Nationwide Outcomes and Utilization. J Adolesc Heal. 2017;61(5):649–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.2015 Introduction to the NIS. Healthcare Cost and Utilization Project (HCUP). February 2018. Agency for Healthcare Research and Quality, Rockville, MD: [Web page]. www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2015.jsp. Accessed Feb 19, 2018. [Google Scholar]
- 8.Woo JG, Zeller MH, Wilson K, Inge T. Obesity Identified by Discharge ICD-9 Codes Underestimates the True Prevalence of Obesity in Hospitalized Children. J Pediatr. 2009;154(3):327–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.NHANES Questionnaires, Datasets, and Related Documentation [Web page]. https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?BeginYear=2015. Accessed Jan 7, 2019.
- 10.Pratt JSA, Browne A, Browne NT, et al. ASMBS pediatric metabolic and bariatric surgery guidelines, 2018. Surg Obes Relat Dis. 2018;14(7):882–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Funk LM, Shan Y, Voils CI, Kloke J, Hanrahan LP. Electronic Health Record Data Versus the National Health and Nutrition Examination Survey (NHANES). Med Care. 2017;55(6):598–605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mantel N, Haenszel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959. April;22(4):719–48. [PubMed] [Google Scholar]
- 13.Deeks JJ, Altman DG, Bradburn MJ. Statistical Methods for Examining Heterogeneity and Combining Results from Several Studies in Meta-Analysis In: Egger M, Smith GD, Altman DG, editors. Systematic Reviews in Health Care. 2nd ed. London, UK: BMJ Publishing Group; 2001. p. 285–312. [Google Scholar]
- 14.Staats C, Capatosto K, Wright RA, Jackson VW. State of the Science: Implicit Bias Review 2016. 2016;106. [Google Scholar]
- 15.Johnson TJ, Winger DG, Hickey RW, et al. Comparison of Physician Implicit Racial Bias Toward Adults Versus Children. Acad Pediatr. 2017;17(2):120–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson TJ, Ellison AM, Dalembert G, et al. Implicit Bias in Pediatric Academic Medicine. J Natl Med Assoc. 2017;109(3):156–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: Pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J Public Health. 2012;102(5):988–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wee CC, Huskey KW, Bolcic-Jankovic D, Colten ME, Davis RB, Hamel M. Sex, race, and consideration of bariatric surgery among primary care patients with moderate to severe obesity. J Gen Intern Med. 2014. January;29(1):68–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wee CC, Hamel MB, Apovian CM, et al. Expectations for weight loss and willingness to accept risk among patients seeking weight loss surgery. JAMA Surg. 2013. March;148(3):264–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Birkmeyer NJO, Gu N. Race, socioeconomic status, and the use of bariatric surgery in Michigan. Obes Surg. 2012;22(2):259–65. [DOI] [PubMed] [Google Scholar]
- 21.Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health. 2007. July;97(7):1283–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Inge TH, Boyce TW, Lee M, et al. Access to care for adolescents seeking weight loss surgery. Obesity. 2014;22(12):2593–7. [DOI] [PubMed] [Google Scholar]
- 23.United States General Accounting Office. Racial Difference in Disability Decisions Warrants Further Investigation. 1992.
- 24.Blog HA, Equity H. Examining Provider Bias In Health Care Through Implicit Bias Rounds How Does Bias Occur? 2018;1–7.
- 25.Changoor NR, Udyavar NR, Morris MA, et al. Surgeons’ Perceptions Toward Providing Care for Diverse Patients: The Need for Cultural Dexterity Training. Ann Surg. 2019. February;269(2):275–82. [DOI] [PubMed] [Google Scholar]
- 26.Wahl TS, Goss LE, Morris MS, et al. Enhanced Recovery After Surgery (ERAS) Eliminates Racial Disparities in Postoperative Length of Stay After Colorectal Surgery. Ann Surg. 2018. December;268(6):1026–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Table 1: ICD-9/10-CM Codes for NIS Inclusion and Exclusion Criteria
Supplemental Figure 1: Overview of the Cochran-Mantel-Haenszel (CMH) method: Formulas and Graphic Depiction of Analysis.