Abstract
The DASH eating pattern has been shown to reduce blood pressure (BP) in previous clinical trials. In the PREMIER study, an established behavioral intervention, with or without DASH, promoted greater weight loss than an advice-only control group, but effects of the DASH intervention on BP were weaker. In these analyses, PREMIER data were used to evaluate whether change in dairy or fruits and vegetable (FV) intake during the first six intervention months impacted changes in weight and/or BP. Study participants were classified as having low or high intakes of dairy (<1.5 vs. ≥1.5 servings/day) and FV (<5 vs. ≥5 servings/day) at baseline and six months. For dairy, in particular, participants with higher baseline intakes tended to decrease their intakes during the intervention. In these analyses, subjects consuming <1.5 dairy servings/day at baseline who increased intake during the intervention lost more weight than those whose intake decreased or remained low throughout (10.6 vs. 7.0 pounds lost, respectively, p=0.002). The same was true for FV intake (11.0 vs. 5.9 pounds lost, p<0.001). We also found synergistic effects of dairy and FVs on weight loss and BP reduction. Specifically, subjects who increased their intakes of dairy and also consumed ≥5 servings of FV/day lost more weight and had greater reductions in BP than other groups; in addition, higher FV intakes had the greatest benefit to BP among those consuming more dairy. These results provide evidence that the DASH pattern was most beneficial to individuals whose baseline diet was less consistent with DASH.
Keywords: DASH diet, PREMIER, Weight loss, Hypertension
Background
Hypertension is exceedingly common among U.S. adults(1) and is a well-known risk factor for cardiovascular disease,(2; 3) contributing to nearly half of all cardiovascular deaths in the US.(4) Primary prevention of hypertension focuses on key lifestyle strategies including weight reduction, sodium restriction, increased physical activity, moderation of alcohol intake, and other dietary modifications(5).
The Dietary Approaches to Stop Hypertension (DASH), characterized by higher intakes of fruits and vegetables and low-fat dairy, have been shown to have blood pressure-lowering effects in clinical trial settings.(6) Since the initial DASH clinical trial, other studies have confirmed the beneficial effects of DASH on blood pressure and cardiovascular risk in different population groups.(7; 8; 9) Recently, a small randomized cross-over study compared a standard DASH pattern with low-fat dairy foods with a full-fat DASH pattern and found comparable reductions in blood pressure.(10)
The PREMIER clinical trial was designed to test the blood pressure lowering effects of two interventions among individuals with pre-hypertension or Stage 1 hypertension, one of which included standard lifestyle modifications while the other also added a DASH dietary intervention.(11) Both interventions were designed to promote weight loss and both led to reductions in blood pressure, compared with an advice-only control group;(12) the intervention including DASH had a slightly greater beneficial effect on weight loss and SBP and DBP reduction. Subsequent secondary analyses suggested that plant rather than animal protein in the PREMIER diets was linked with greater blood pressure lowering effects.(13) In those analyses, the effect of dairy on blood pressure outcomes was null while fruit and vegetable (FV) intakes were beneficial. These analyses did not account for baseline dietary patterns.
The selection of the population at risk is a crucial element for any clinical trial since beneficial treatment effects are likely to be greater among individuals at higher risk for the outcome. For example, exercise interventions are likely to provide greater benefit for sedentary individuals who are at higher risk for cardiovascular disease and other disorders than for those who are already exercising regularly. In these analyses, we hypothesized that baseline intakes of dairy and fruits and vegetables (FV) in PREMIER might have impacted the effects of the DASH intervention on weight and BP in that study. Specifically, we explored whether changes in the level of dairy and FV intake during the initial six-month exposure period in the PREMIER Study were associated with changes in weight and blood pressure during the intervention period.
Methods
Original Study
The PREMIER study was a randomized multicenter clinical trial that was designed to compare the BP-lowering effects of two comprehensive non-pharmacologic lifestyle interventions (a standard “Lifestyle” intervention and the “Lifestyle plus DASH” intervention) with an advice-only control group. Details of the study design have been previously published.(11) Begun in 2000, the study recruited 810 men and women (34% African American) from four study centers (Baltimore, MD, Baton Rouge, LA, Durham, N.C., and Portland, OR). Eligible subjects were adults at least 25 years of age with a BMI between 18.5 and 45.0 kg/m2 with pre-hypertension (SBP 120–139 mm Hg or DBP 80–89) or untreated Stage I hypertension (SBP: 140–159 mm Hg or DBP: 90–95 mm Hg) based on mean blood pressure from three screening visits. The primary intervention period was six months. Since the current analyses are based on dietary change, those who were missing dietary data at 6 months were excluded (n=119). In addition, 19 subjects with missing activity data at six months and 7 subjects with missing weight measures at 6 months were excluded, leaving data for 665 of the original 810 study participants. These data were obtained from the National Heart, Lung, and Blood Institute Biologic Specimen and Data Repository Information Coordinating Center (BIOLINCC).
In PREMIER, both intervention arms employed an identical series of group and individual sessions to facilitate adoption of lifestyle changes and skills to achieve the intervention goals while the Advice Only group (control) also targeted weight loss and physical activity but without the behavioral intervention. The Lifestyle intervention targeted the following behavior changes: 1) reduce weight by 7 kg (~15 lb.) or more if overweight; 2) limit daily sodium intake to 100 mmol or less; 3) limit fat intake to 30% of calories intake or less; 4) engage in 180 minutes per week (or its equivalent) of moderate physical activity; and 5) limit alcohol intake to no more than one ounce of ethanol per day for men and no more than 0.5 ounce per day for women. Finally, the Lifestyle plus DASH intervention added advice on a DASH-style eating pattern (9–12 servings per day of FV, 2–3 servings per day of low-fat dairy, reduced intakes of saturated and total fat) to the behavioral intervention.
Trained telephone interviewers assessed diet among study participants using unannounced 24-hour recalls. Two recalls (one weekday and one weekend) per participant were collected at baseline and 6 months. Intakes of total energy, nutrients, and food groups (from both whole foods and composite food ingredients) were calculated at the Diet Assessment Center of Pennsylvania State University using the Nutrition Data System, Version NDS-R 1998 (University of Minnesota). In this way, servings per day of dairy (milk, yogurt, cheese) as well as fruits and vegetables were calculated. Total dairy intake included both full-fat and reduced-fat dairy although study recommendations were for consumption of low-fat dairy.
BP was measured by trained and certified individuals following a standardized protocol and using a random zero sphygmomanometer and an appropriate-sized cuff. Two separate measures were taken with at least 30 seconds between measurements. The means of the two SBP and DBP measures were calculated as well as the mean of two measures of weight (to the nearest 0.25 pound) using a calibrated digital scale. Weight, SBP and DBP from the baseline and 6-month follow-up visits are used in these analyses.
Two measures of height to the nearest 0.1 centimeter were taken using a calibrated wall-mounted stadiometer. Body mass index was calculated as weight, in kilograms, divided by the square of height, in centimeters. Physical activity was assessed by means of a standardized 7-Day Physical Activity Recall (PAR).(14; 15) Each subject’s self-reported daily activities were categorized as light, moderate, hard, or very hard, and the number of minutes spent in activities of various intensity levels was used to derive each individual’s estimated average daily energy expenditure for the previous week.
Statistical Analysis
We first estimated mean baseline intakes of dairy and FV in the two original PREMIER intervention groups and the control group as well as mean change in intake from baseline to six months (i.e., mean intake at six months minus mean baseline intake). Change in weight, SBP and DBP were calculated in the same manner.
Since the recommended intakes of dairy in the DASH intervention were 2 or more servings per day, we initially classified dairy intake as follows: <1, 1-<2, and ≥2 servings per day. However, only 22% of subjects at baseline consumed at least 2.0 servings/day and only 28% consumed that amount during the intervention. For FV, recommended intakes were 9 or more servings per day. However, since only 25 subjects at baseline consumed that amount, we chose to use the following cutoff values: <3, 3-<5, and ≥5 servings per day. Finally, to improve statistical power, we chose to dichotomize dietary intakes based on information from sensitivity analyses as follows: <1.5 vs. ≥1.5 servings of dairy per day and <5 vs. ≥5 servings of FV per day.
These dichotomous categorizations were used to classify intake simultaneously during the baseline and intervention periods. For example, four exposure categories for FV intake were defined as follows: (1) low baseline (<5.0 servings) / low intervention (<5.0 servings) intake, (2) low baseline (<5.0 servings) / high intervention (≥5.0 servings), (3) high baseline / low intervention, and (4) high baseline / high intervention). Those with low intakes of FV at both baseline and six months (low/low) served as the referent group. Those in the low/high groups were those who increased their FV intake during the intervention. The same approach was used to consider baseline/intervention dairy intakes.
We used analysis of covariance to compare the mean weight loss in three groups (low/high, high/low, and high/high) compared with the referent groups (low/low). These models were to derive the adjusted mean weight loss controlling for confounding by factors (age, sex, race, and physical activity) found to change the mean differences by 5% of more. Factors that led to no change in the adjusted means were dropped from the final models. This included both non-dietary factors (i.e., height, education, pack-years of smoking) and dietary factors such as intervention intakes of minerals (i.e., sodium, potassium, calcium, magnesium), protein foods (i.e., meats, eggs, poultry, fish), sweets and snacks, total grains, and nuts, beans, and soy. Similar analyses were used to evaluate change in SBP and DBP.
Results
Table 1 shows the characteristics of subjects in the PREMIER trial according to baseline intakes of dairy and FV. Fewer African Americans were in the highest categories of intake for both food groups. Those with the highest baseline intakes of dairy consumed more saturated fat but not more total fat, while both total fat and saturated fat intakes were inversely associated with FV consumption. Despite randomization, there were some apparent differences in baseline dairy intake across the original PREMIER intervention group assignments. In particular, those with the lowest baseline dairy intakes were least likely to be assigned to the DASH intervention group, a finding that could have led to confounding of the original results if baseline intake is a determinant of response to the intervention.
Table 1.
Baseline characteristics of PREMIER subjects according to baseline intake of dairy and fruits and vegetables
| Subject Characteristics | <1 | l-<2 | ≥2 | <3 | 3-<5 | ≥5 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 278 | 238 | 149 | 232 | 224 | 209 | ||||||
| Age (n, column percent) | ||||||||||||
| % ≤40 yrs | 34 (12.2%) | 35 (14.7%) | 19(12.8%) | 43 (18.5%) | 31 (13.8%) | 14 (6.7%) | ||||||
| % 41–55 yrs | 169(60.8%) | 138(58.0%) | 90 (60.4%) | 148 (63.8%) | 130(58.0%) | 119(56.9%) | ||||||
| % ≥56 yrs | 75 (27.0%) | 65 (27.3%) | 40 (26.8%) | 41 (17.7%) | 63(28.1%) | 76 (36.4%) | ||||||
| Sex (n, % female) | 184(66.2%) | 147(61.8%) | 76(51.0%) | 154(66.4%) | 145 (64.7%) | 108(61.7%) | ||||||
| Race (n, % African American) | 132(47.5%) | 63 (26.5%) | 21 (14.1%) | 94 (40.5%) | 75 (33.5%) | 47 (22.5%) | ||||||
| Intervention assignment | ||||||||||||
| Control | 95 (34.2%) | 76(31.9%) | 52 (34.9%) | 84 (36.2%) | 77 (34.4%) | 62 (29.7%) | ||||||
| Lifestyle | 103(37.1%) | 69 (29.0%) | 47(31.5%) | 73(31.5%) | 77 (34.4%) | 69 (33.0%) | ||||||
| Lifestyle plus DASH | 80 (28.8%) | 93 (39.1%) | 50 (33.6%) | 75 (32.3%) | 70(31.3%) | 78 (37.3%) | ||||||
| s.d. | s.d. | s.d. | s.d. | s.d. | s.d. | |||||||
| Dairy (svg/d) | 0.31 | 0.29 | 0.92 | 1.10 | 1.03 | 1.04 | ||||||
| Fruits and vegetables (svg/d) | 2.23 | 2.36 | 2.37 | 0.78 | 0.59 | 1.79 | ||||||
| Energy intake (kcals) | 538 | 582 | 682 | 586 | 661 | 584 | ||||||
| % calories from fat | 7.8 | 7.3 | 7.7 | 7.2 | 7.1 | 7.7 | ||||||
| % calories from saturated fat | 3.1 | 2.7 | 3.7 | 3.0 | 3.0 | 3.2 | ||||||
| % calories from carbs | 10.5 | 8.3 | 9.1 | 9.1 | 9.2 | 9.4 | ||||||
| % calories from protein | 4.4 | 3.7 | 3.3 | 4.2 | 3.6 | 4.0 | ||||||
| Sodium (mg) | 1100 | 1085 | 1427 | 1135 | 1282 | 1174 | ||||||
| Potassium (mg) | 808 | 799 | 978 | 663 | 779 | 743 | ||||||
| K:Na Ratio | 0.39 | 0.40 | 0.50 | 0.32 | 0.35 | 0.47 | ||||||
| Weight (lbs) | 39 | 40 | 42 | 39.6 | 39.0 | 42.5 | ||||||
| BMI (kg/m2) | 5.7 | 5.5 | 5.8 | 5.7 | 5.4 | 5.8 | ||||||
| SBP | 9.5 | 9.6 | 9.6 | 9.4 | 9.9 | 9.5 | ||||||
| DBP | 4.1 | 4.1 | 4.1 | 4.0 | 4.2 | 4.1 | ||||||
| Physical activity (min/wk)* | 237 | 411 | 254 | 383 | 288 | 246 | ||||||
Moderate to vigorous physical activity
Fig. 1 shows changes in dairy and FV intakes (from baseline to six months) in each assigned PREMIER intervention group, stratifying by baseline intake. For example, those with the lowest baseline dairy intakes (<1 serving/day) in the “Advice Only” (control) group increased their dairy intakes by 0.46 servings/day while those with higher baseline intakes (≥2 servings/day) decreased their intakes by 0.85 servings/day. The same pattern was evident in all three intervention groups—those with lower baseline intakes increased consumption and those with higher baseline intakes reduced consumption. The same was not the case for FV intake where those in the DASH intervention group who already were consuming at least 5 servings/day still increased their intakes by an additional 1.44 servings per day.
Fig. 1. Changes in Dairy and FV intake according to baseline intake in each intervention group.
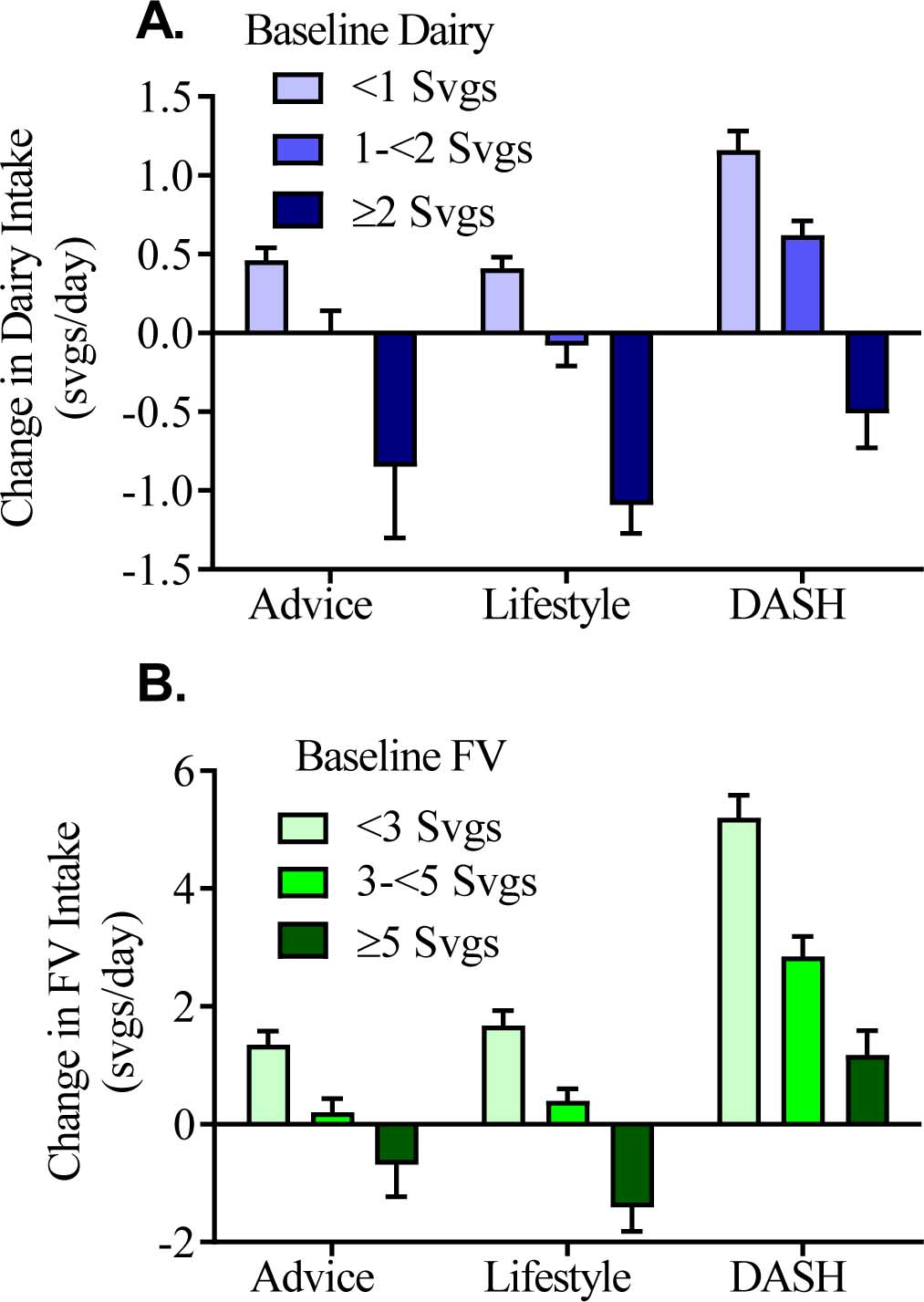
(A) Changes in dairy intake according to baseline dairy intake in the three intervention groups. (B) Changes in FV intake according to baseline FV intake in the three intervention groups; n=655. Data are presented as mean changes ± SEM
Fig. 2 shows changes in weight and BP according to intakes of dairy and FV during the intervention period. For example, Panel A shows that those consuming ≥2 servings of dairy or ≥5 servings of FV during the intervention had statistically significantly greater weight loss than those consuming less (p-trend: 0.009 and <0.001, respectively). Higher FV intakes (Panels B, C) were also strongly inversely associated with both SBP and DBP (p-trend: 0.002 and 0.027, respectively).
Fig. 2. Changes in Weight, SBP and DBP according to intervention intakes of dairy and FV.
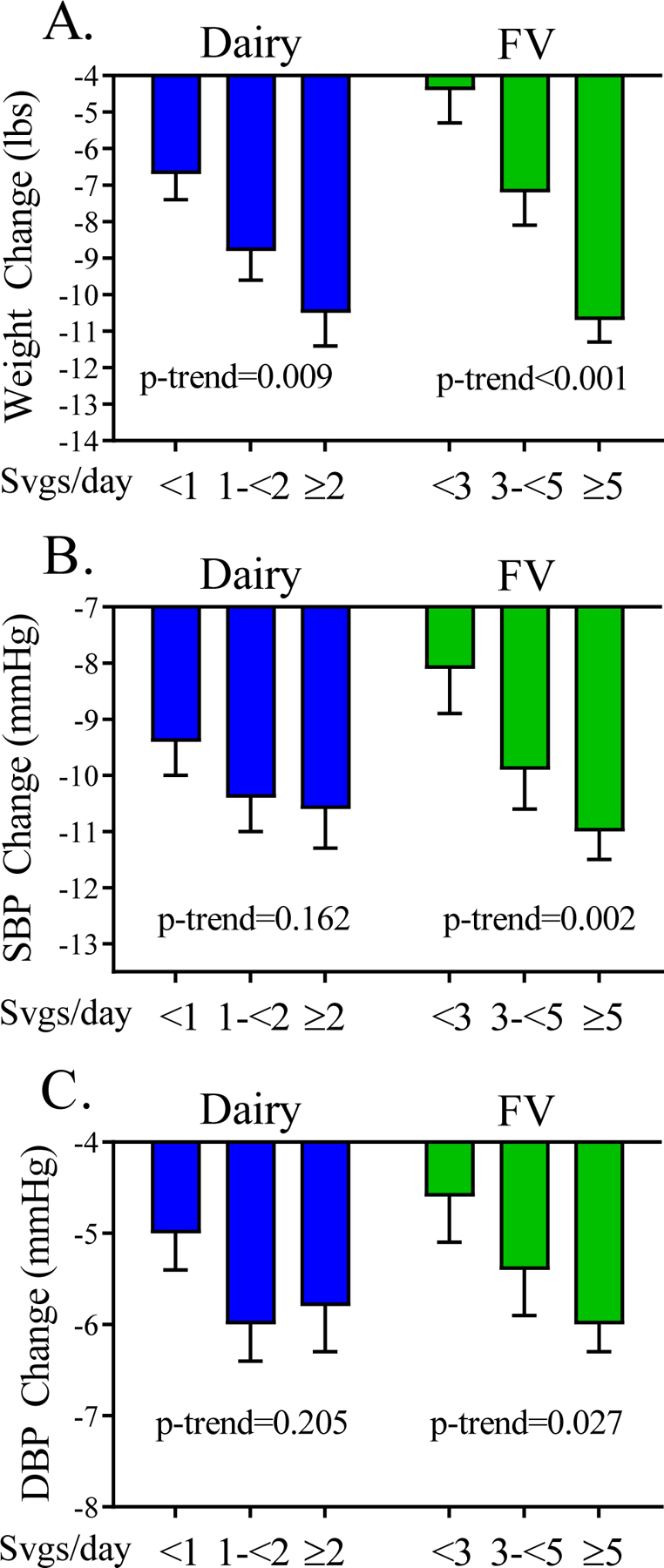
Changes in weight (A), SBP (B), and DBP (C) according to intervention intakes of dairy or FV. Data are presented as mean differences from baseline ± SEM. Mean differences are adjusted for age, sex, race, and physical activity.
Since higher combined intakes of dairy and FV are used to reflect the main components of a DASH-style eating pattern, we examined these combined intakes (Supplemental Table 1) irrespective of the original PREMIER study group assignment. Those with higher intakes of both dairy and FV had the greatest weight loss (12.5 pounds in the high dairy/high FV group vs. 5.6 pounds lost in the low dairy/low FV group, p <0.0001) and the greatest reductions in SBP and DBP. Since weight loss is strongly associated with physical activity and level of obesity, we also stratified by these factors. Regardless of activity level, participants with higher intakes of both dairy and FV had greater reductions in weight than those with lower intakes of dairy or FV. Similarly, both obese and non-obese subjects with higher intakes of both dairy and FV had the greatest weight loss and reductions in blood pressure.
Table 2 shows changes in weight and BP associated with the change in dairy and FV intakes from baseline to the intervention period. In these analyses, those who started with low baseline intakes (<1.5 servings/day of dairy or <5 servings/day of FV) but who then increased their intakes (to ≥2.5 servings of dairy and ≥5 servings of FV) during the intervention had the greatest weight loss. Of note, participants with lower dairy intakes during the intervention period (low/low and high/low groups) lost similar amounts of weight (7.0 and 7.1 lbs, respectively). Likewise, those with higher intakes of dairy during the intervention period also lost comparable amounts of weight (10.6 and 9.9 lbs in the low/high and high/high groups, respectively). Patterns Results were similar for FV intake. As a result of the comparable amounts of weight loss in the low/low and high/low groups (and to improve statistical power), we combined these two categories for the analyses in Table 3.
Table 2:
Change in intakes of dairy and fruits/vegetables and change in weight and blood pressure
| Intake Change Category | Weight Change (lbs) | SBP Change (mmHg) | DBP Change (mmHg) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Baseline / Intervention Dairy Intakes† | ||||||||||
| Low / Low | 276 | −7.0 | 0.70 | Ref | −10.0 | 0.57 | Ref | −5.2 | 0.39 | Ref |
| Low / High | 142 | −10.6 | 0.95 | 0.002 | −10.6 | 0.77 | 0.518 | −6.0 | 0.54 | 0.229 |
| High / Low | 94 | −7.1 | 1.17 | 0.976 | −9.4 | 0.95 | 0.616 | −5.2 | 0.66 | 0.981 |
| High / High | 153 | −9.9 | 0.96 | 0.018 | −10.3 | 0.77 | 0.730 | −5.9 | 0.54 | 0.351 |
| Baseline / Intervention FV intake† | ||||||||||
| Low / Low | 256 | −6.2 | 0.72 | Ref | −9.3 | 0.58 | Ref | −5.1 | 0.41 | Ref |
| Low / High | 200 | −11.0 | 0.80 | <0.0001 | −10.5 | 0.65 | 0.191 | −5.8 | 0.45 | 0.197 |
| High / Low | 56 | −5.0 | 1.51 | 0.504 | −8.2 | 1.23 | 0.402 | −4.8 | 0.86 | 0.817 |
| High / High | 153 | −10.4 | 0.92 | 0.0004 | −11.7 | 0.75 | 0.016 | −6.2 | 0.53 | 0.097 |
Mean differences adjusted for age, sex, race, and physical activity using analysis of covariance models
Low/Low = low baseline intake / low intervention intake (<1.5 for dairy, <5 for FV); Low/High = low baseline intake / high intervention intake (≥1.5 for dairy, ≥5 for FV); High/Low = high baseline intake / low intervention intake; High/High = high baseline intake / high intervention intake.
Table 3.
Changes in weight and blood pressure according to change in intakes of dairy and FV, stratifying by intervention intake
| Weight Change | SBP Change | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| N | Adj. mean* | SE | p-value | Adj. mean* | SE | p-value | Adj. mean* | SE | |
| Dairy | |||||||||
| Low Dairy‡ | 370 | −7.0 | 0.60 | Ref | −9.8 | 0.49 | Ref | −5.2 | 0.34 |
| Low/High Dairy | 142 | −10.7 | 0.95 | 0.002 | −10.6 | 0.77 | 0.399 | −6.0 | 0.54 |
| High/High Dairy | 153 | −9.9 | 0.96 | 0.013 | −10.3 | 0.77 | 0.589 | −5.9 | 0.54 |
| Fruits and Vegetables | |||||||||
| Low FV‡ | 312 | −5.9 | 0.64 | Ref | −9.1 | 0.52 | Ref | −5.0 | 0.37 |
| Low/High FV | 200 | −11.0 | 0.80 | <0.0001 | −10.5 | 0.65 | 0.102 | −5.9 | 0.45 |
| High/High FV | 153 | −10.4 | 0.92 | <0.0001 | −11.7 | 0.75 | 0.005 | −6.2 | 0.52 |
| Low Intervention FV | |||||||||
| Low Dairy‡ | 206 | −5.7 | 0.79 | Ref | −9.6 | 0.65 | Ref | −5.3 | 0.45 |
| Low/High Dairy | 57 | −6.3 | 1.49 | 0.702 | −7.8 | 1.22 | 0.212 | −4.5 | 0.85 |
| High/High Dairy | 49 | −6.5 | 1.62 | 0.700 | −8.7 | 1.33 | 0.548 | −4.5 | 0.93 |
| High Intervention FV | |||||||||
| Low Dairy‡ | 164 | −8.7 | 0.88 | 0.010 | −10.1 | 0.72 | 0.542 | −5.1 | 0.50 |
| Low/High Dairy | 85 | −13.6 | 1.21 | <0.0001 | −12.4 | 0.99 | 0.016 | −7.1 | 0.69 |
| High/High Dairy | 104 | −11.6 | 1.13 | <0.0001 | −11.1 | 0.92 | 0.175 | −6.5 | 0.64 |
| Low Intervention Dairy | |||||||||
| Low FV‡ | 206 | −5.6 | 0.79 | Ref | −9.5 | 0.65 | Ref | −5.3 | 0.45 |
| Low/High FV | 104 | −8.4 | 1.10 | 0.038 | −10.0 | 0.90 | 0.678 | −5.1 | 0.63 |
| High/High FV | 60 | −9.2 | 1.45 | 0.033 | −10.4 | 1.19 | 0.529 | −5.1 | 0.83 |
| High Intervention Dairy | |||||||||
| Low FV‡ | 106 | −6.4 | 1.10 | 0.571 | −8.2 | 0.90 | 0.238 | −4.5 | 0.63 |
| Low/High FV | 96 | −13.7 | 1.15 | <0.0001 | −11.0 | 0.94 | 0.216 | −6.6 | 0.66 |
| High/High FV | 93 | −11.3 | 1.17 | <0.0001 | −12.5 | 0.96 | 0.012 | −6.9 | 0.67 |
Models adjusted for age, sex, race and physical activity
Low vs. high intake: <1.5 vs. ≥1.5 servings/day for dairy; <5 vs. ≥5 servings/day for FV
Low intake here combines Low/Low and High/Low categories from Table 2
To determine whether the effect of change in dairy intake was modified by the concurrent intake of FV (and vice versa), we carried out stratified analyses in Table 3. As seen in Table 2, participants who increased their intakes of dairy or FV during the intervention period (low/high) as well as those who had higher intakes throughout (high/high) had greater reductions in weight than those having low intakes during the intervention. This was also the case for SBP and DBP although most changes did not reach statistical significance. When stratifying by concurrent intake of FV, it is evident here that the beneficial effect of increasing dairy intake (Low/High) is modified by FV intake. Compared with the referent group (low/low dairy among those with low FV intakes) with an average weight loss of 5.7 pounds, those who increased their dairy intake and who also consumed at least 5 servings of FV per day had an average weight loss of 13.6 pounds. In contrast, those who increased their dairy intakes but who had lower FV intakes lost only 8.7 pounds. The same pattern was evident for blood pressure change. Finally, higher FV intake (high/high) and increasing FV intake (low/high) led to the greatest weight loss and reductions in BP among those with higher dairy intakes during the intervention.
Discussion
The original PREMIER randomized clinical trial studied the impact of two lifestyle-based interventions, one with a DASH-style dietary pattern and one without, on weight loss and BP reduction. These current secondary analyses examined how baseline intakes of dairy and FV, the two primary DASH components, may have influenced the effects of the intervention on weight loss and changes in BP.
We found that baseline intake, especially for dairy products, may have influenced the effects of the original DASH intervention in PREMIER since those participants consuming ≥2 servings of dairy per day at baseline and who were assigned to the DASH intervention group actually reduced their dairy intake during the intervention period. In contrast, participants in the DASH intervention arm of the trial increased their intakes of FV regardless of baseline intake.
We found that the amount of both dairy and FVs consumed during the intervention was directly associated with weight loss and BP reduction, with higher intakes being associated with greater declines in weight and BP. Further, higher combined intakes of both dairy and FVs (as recommended by DASH) were associated with greater weight loss and greater SBP and DBP reductions than seen in those with lower intakes of both. We found that those who increased their intakes of either dairy (to ≥1.5 servings/day) or FV (to ≥5 servings/day) had substantially greater weight loss after 6 months than those with lower intervention intakes. In addition, more active participants and those who were obese at baseline lost more weight than their more sedentary or non-obese counterparts (supplemental data). Finally, the effects of dairy consumption on mean weight and BP change during the trial were found to be modified by FV intake and vice versa. Increasing dairy consumption led to the greatest weight loss and reductions in SBP and DPB among those with higher FV intakes. Similarly, the greatest FV benefits were seen among those with higher dairy consumption during the intervention. Thus, these analyses support a beneficial effect of the DASH pattern on both weight loss and BP reduction and demonstrate that these benefits were more apparent for dairy intake in particular among those whose baseline intakes were lower.
The original PREMIER study was designed to evaluate a DASH eating plan as part of a multicomponent intervention that simultaneously targeted weight loss (of 15 lbs or more) and BP reduction.(11) While the primary outcome was SBP reduction, it is difficult to separate fully the BP changes from weight reduction in this trial since most subjects lost substantial weight. In the report of the main results, both the Lifestyle-only intervention and the Lifestyle plus DASH intervention led to statistically significant reductions in weight and BP.(12) However, participants in the Lifestyle plus DASH group had only very slightly greater declines in BP than the established Lifestyle intervention (i.e., 0.6 mmHg greater decline in SBP, 0.9 mmHg greater decline in DBP). These results contrast with a previous meta-analysis of 17 controlled trials that found a DASH diet to be associated with an average reduction in SBP of 6.74 mmHg and in DBP of 3.54 mmHg.(16) These results are also at odds with a recent randomized crossover trial showing that a high-dairy diet alone resulted in greater reductions (p=0.009) in both SBP (4.6 mmHg) and DBP (3.0 mmHg) than a diet with lower intakes of dairy.(17) Since the high-dairy diet in that study comprised 5 or 6 servings for men and women, respectively, compared with <1 serving in the low-dairy group, it is possible that the lower intakes of dairy in DASH arm of the PREMIER may explain the weaker dairy-related effects in that study.
The effects observed in PREMIER were much weaker than those seen in the earlier DEW-IT trial in which subjects in a lifestyle intervention group (a low-calorie, low-sodium DASH plus exercise) had substantially greater reductions in BP than those in the advice only group.(18) In an editorial accompanying the publication of the PREMIER study, Pickering explored the possible explanations for this weaker effect of the DASH intervention arm on BP.(19) One potential explanation for these weaker effects was poorer adherence to the DASH plan in the PREMIER study (since foods were purchased and prepared by the subjects rather than provided). Adherence issues are supported by the finding that the Lifestyle plus DASH group in PREMIER had only a 28.3% increase in potassium intake;(20) in contrast, the potassium intake in the combined diet group in the original DASH study was 152.0% higher than that of the control diet.(6) The weaker observed effects of DASH in PREMIER could also have resulted from a greater reduction in BP in the control group than was observed among controls in previous studies.(6; 7) Further, the PREMIER authors speculated that weaker effects on BP in PREMIER might have resulted from a subadditivity of intervention effects (i.e., the total effect of the Lifestyle intervention plus DASH may have been less than the sum of the two individual interventions), since it may have been difficult for subjects to self-manage two interventions simultaneously.(11)
In the current analyses, we propose an additional explanation for the weaker effects of the DASH intervention on BP in PREMIER. Specifically, we propose that subjects with higher baseline intakes of dairy should likely have been excluded from the trial. Alternatively, they could have maintained their already-adequate intake of dairy rather than decreasing intake during the intervention. Our current analyses suggest that subjects who increased their intake (e.g., from low to high) had a somewhat greater benefit (although not statistically significant) than those who had higher intakes throughout. It is possible that those who increased their intakes may have replaced less healthy food choices with healthier foods recommended as part of the DASH pattern. Previous substitution analyses have suggested that replacement of red meat, for example, with low-fat dairy, fish, or other protein sources could lower cardiovascular disease occurrence and mortality risk.(21; 22) However, in confounding analyses in the current study, we controlled for changes in snacking behaviors and other changes in diet but we found that none of these altered the results.
In this study, we focused on dairy and FV intakes as the primary components of the DASH pattern. There are several mechanisms by which these foods may benefit blood pressure. Fruits and vegetables are rich in polyphenols and also raise anti-oxidant capacity, lowering oxidative stress. These mechanisms have been linked with beneficial effects on BP regulation and downstream effects on cardiovascular health.(23; 24) Glutamic acid, an amino acid in vegetable protein, has also been inversely associated with BP.(25) Further, potassium, magnesium, and calcium (all of which are found in abundance in fruits, vegetables, and dairy) have been linked with lower BPs through regulation of vascular resistance and promotion of vasodilation.(26) A higher potassium-to-sodium ratio has been linked with decreases in renal sodium retention, thereby lowering blood pressure.(27) Higher potassium intakes have also been shown to reduce salt sensitivity while magnesium aids in the regulation of intracellular calcium, potassium and sodium, thereby promoting insulin sensitivity and reducing vascular resistance. The role of dairy per se in BP regulation has been somewhat controversial. However, at least one meta-analysis of nine randomized controlled trials found that dairy-derived tripeptides lower blood pressure.(28) Specifically, angiotensin-I-converting enzyme (ACE) inhibitory peptides that inhibit the renin-angiotensin system have been found in both milk and cheese.(29)
There are some limitations to the present study but the biggest may be the limited power for stratified analyses. We were unable to look at sex- or race-specific differences and some categories in the current analyses had small numbers. In addition, we used lower cutoff values to define “higher” intakes of both dairy (1.5 servings per day) and FVs (5 servings per day) since too few subjects consumed the recommended 2–3 servings of dairy and 9–12 servings of FV. Another limitation of this study relates to the self-report of diet (since the PREMIER study was not a feeding trial) which could have introduced bias in the reported intakes of dairy and FVs. In addition, dietary intake in this study was assessed at each time point using only two 24-hour recalls, which may have yielded less precise estimates of intake than would have been obtained if more days of recall had been available(30). However, a previous study from the EFCOSUM group shows that two days of dietary records may be used to estimate intakes of frequently-consumed foods in different population groups.(31) Nonetheless, this study is strengthened by the use of carefully-controlled measured data for the weight and blood pressure outcomes as well as important potential confounders.
This study adds important new data supporting the beneficial effects of a DASH intervention on weight loss among overweight individuals and blood pressure reduction in those with borderline high blood pressure or stage 1 hypertension. It also demonstrates that the combined benefits of dairy and fruits and vegetables is greater than that seen with individual food groups. Finally, this study demonstrates that the DASH pattern is most beneficial to those with lower baseline intakes of dairy and fruits and vegetables.
Supplementary Material
Acknowledgements
These secondary analyses were supported by the National Heart Lung and Blood Institute (NHLBI; grant no. 5T32HL125232) and the National Dairy Council. None of the funders had any role in the analysis, design, or writing of this manuscript. This Manuscript was prepared using A Trial of Lifestyle Interventions for Blood Pressure Control (PREMIER) Research Materials obtained from the NHLBI Biologic Specimen and Data Repository Information Coordinating Center and does not necessarily reflect the opinions or views of the PREMIER or NHLBI.
Footnotes
None of the authors have conflicts of interest to declare
REFERENCES
- 1.Centers for Disease Control and Prevention (2011) Vital signs: prevalence, treatment, and control of hypertension--United States, 1999–2002 and 2005–2008. MMWR Morb Mortal Wkly Rep 60, 103–108. [PubMed] [Google Scholar]
- 2.Stamler J, Stamler R, Neaton JD (1993) Blood pressure, systolic and diastolic, and cardiovascular risks. US population data. Arch Intern Med 153, 598–615. [DOI] [PubMed] [Google Scholar]
- 3.Vasan RS, Larson MG, Leip EP et al. (2001) Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 345, 1291–1297. [DOI] [PubMed] [Google Scholar]
- 4.Ezzati M, Lopez AD, Rodgers A et al. (2002) Selected major risk factors and global and regional burden of disease. Lancet 360, 1347–1360. [DOI] [PubMed] [Google Scholar]
- 5.Whelton PK, He J, Appel LJ et al. (2002) Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA 288, 1882–1888. [DOI] [PubMed] [Google Scholar]
- 6.Appel LJ, Moore TJ, Obarzanek E et al. (1997) A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med 336, 1117–1124. [DOI] [PubMed] [Google Scholar]
- 7.Sacks FM, Svetkey LP, Vollmer WM et al. (2001) Effects on blood pressure of reduced dietary sodium and the Dietary Approaches to Stop Hypertension (DASH) diet. DASH-Sodium Collaborative Research Group. N Engl J Med 344, 3–10. [DOI] [PubMed] [Google Scholar]
- 8.Blumenthal JA, Babyak MA, Hinderliter A et al. (2010) Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: the ENCORE study. Arch Intern Med 170, 126–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azadbakht L, Fard NR, Karimi M et al. (2011) Effects of the Dietary Approaches to Stop Hypertension (DASH) eating plan on cardiovascular risks among type 2 diabetic patients: a randomized crossover clinical trial. Diabetes Care 34, 55–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chiu S, Bergeron N, Williams PT et al. (2016) Comparison of the DASH (Dietary Approaches to Stop Hypertension) diet and a higher-fat DASH diet on blood pressure and lipids and lipoproteins: a randomized controlled trial. Am J Clin Nutr 103, 341–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Svetkey LP, Harsha DW, Vollmer WM et al. (2003) Premier: a clinical trial of comprehensive lifestyle modification for blood pressure control: rationale, design and baseline characteristics. Ann Epidemiol 13, 462–471. [DOI] [PubMed] [Google Scholar]
- 12.Appel LJ, Champagne CM, Harsha DW et al. (2003) Effects of comprehensive lifestyle modification on blood pressure control: main results of the PREMIER clinical trial. JAMA 289, 2083–2093. [DOI] [PubMed] [Google Scholar]
- 13.Wang YF, Yancy WS, Yu D et al. (2008) The relationship between dietary protein intake and blood pressure: results from the PREMIER study. J Hum Hypertens 22, 745–754. [DOI] [PubMed] [Google Scholar]
- 14.Sallis JF, Haskell WL, Wood PD et al. (1985) Physical activity assessment methodology in the Five-City Project. Am J Epidemiol 121, 91–106. [DOI] [PubMed] [Google Scholar]
- 15.Blair SN, Haskell WL, Ho P et al. (1985) Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol 122, 794–804. [DOI] [PubMed] [Google Scholar]
- 16.Saneei P, Salehi-Abargouei A, Esmaillzadeh A et al. (2014) Influence of Dietary Approaches to Stop Hypertension (DASH) diet on blood pressure: a systematic review and meta-analysis on randomized controlled trials. Nutr Metab Cardiovasc Dis 24, 1253–1261. [DOI] [PubMed] [Google Scholar]
- 17.Rietsema S, Eelderink C, Joustra ML et al. (2019) Effect of high compared with low dairy intake on blood pressure in overweight middle-aged adults: results of a randomized crossover intervention study. Am J Clin Nut, 110, 340–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller ER, Erlinger TP, Young DR et al. (2002) Results of the Diet, Exercise, and Weight Loss Intervention Trial (DEW-IT). Hypertension 40, 612–618. [DOI] [PubMed] [Google Scholar]
- 19.Pickering TG (2003) Lifestyle modification and blood pressure control: is the glass half full or half empty? JAMA 289, 2131–2132. [DOI] [PubMed] [Google Scholar]
- 20.Elmer PJ, Obarzanek E, Vollmer WM et al. (2006) Effects of comprehensive lifestyle modification on diet, weight, physical fitness, and blood pressure control: 18-month results of a randomized trial. Ann Intern Med 144, 485–495. [DOI] [PubMed] [Google Scholar]
- 21.Bernstein AM, Sun Q, Hu FB et al. (2010) Major dietary protein sources and risk of coronary heart disease in women. Circulation 122, 876–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Song M, Fung TT, Hu FB et al. (2016) Association of Animal and Plant Protein Intake With All-Cause and Cause-Specific Mortality. JAMA Intern Med 176, 1453–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lopes HF, Martin KL, Nashar K et al. (2003) DASH diet lowers blood pressure and lipid-induced oxidative stress in obesity. Hypertension 41, 422–430. [DOI] [PubMed] [Google Scholar]
- 24.Medina-Remón A, Zamora-Ros R, Rotchés-Ribalta M et al. (2011) Total polyphenol excretion and blood pressure in subjects at high cardiovascular risk. Nutr Metab Cardiovasc Dis 21, 323–331. [DOI] [PubMed] [Google Scholar]
- 25.Stamler J, Brown IJ, Daviglus ML et al. (2009) Glutamic acid, the main dietary amino acid, and blood pressure: the INTERMAP Study (International Collaborative Study of Macronutrients, Micronutrients and Blood Pressure). Circulation 120, 221–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Houston MC, Harper KJ (2008) Potassium, magnesium, and calcium: their role in both the cause and treatment of hypertension. J Clin Hypertens (Greenwich) 10, 3–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gallen IW, Rosa RM, Esparaz DY et al. (1998) On the mechanism of the effects of potassium restriction on blood pressure and renal sodium retention. Am J Kidney Dis 31, 19–27. [DOI] [PubMed] [Google Scholar]
- 28.Xu JY, Qin LQ, Wang PY et al. (2008) Effect of milk tripeptides on blood pressure: a meta-analysis of randomized controlled trials. Nutrition 24, 933–940. [DOI] [PubMed] [Google Scholar]
- 29.Kris-Etherton PM, Grieger JA, Hilpert KF et al. (2009) Milk products, dietary patterns and blood pressure management. J Am Coll Nutr 28 Suppl 1, 103S–119S. [DOI] [PubMed] [Google Scholar]
- 30.Basiotis PP, Welsh SO, Cronin FJ et al. (1987) Number of days of food intake records required to estimate individual and group nutrient intakes with defined confidence. J Nutr 117, 1638–1641. [DOI] [PubMed] [Google Scholar]
- 31.Biro G, Hulshof KF, Ovesen L et al. (2002) Selection of methodology to assess food intake. Eur J Clin Nutr 56 Suppl 2, S25–32. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


