Abstract
Objective:
To determine whether the prevalence of functional limitations in United States (U.S.) born differs from that of foreign-born Black older adults.
Design:
We performed a cross-sectional analysis of data from 14,438 U.S. born and 1,583 foreign-born Black older adults (≥50 years) in the 2010–2016 National Health Interview Surveys (NHIS). Functional limitations were defined by upper and lower extremity limitations, and global functional limitations. Generalized linear modeling using a Poisson distribution and logarithmic link function was used to compare the predicted probabilities of functional limitations in both groups.
Results:
The mean age (S.E) of U.S. born Blacks was 63.56 (0 .12) years and foreign-born Blacks was 62.06 (0.32). The majority (92%) of foreign-born Blacks had resided in the U.S. for ≥ 10 years. U.S. born older adults were more likely to have upper (46% vs. 29%, p<0.001) and lower (61% vs 40%, p<0.001) extremity limitations than foreign-born Blacks. The prevalence of lower extremity limitations was 22% less in foreign-born Blacks compared to U.S. born Blacks after adjusting for sociodemographic and health profiles (Prevalence Ratio [PR]: 0.78, 95% CI:0.728–0.835). The adjusted prevalence of upper extremity limitations in foreign-born Blacks was 27% (PR: 0.73, 95% CI: [0.680–0.791], compared to U.S. born Black older adults. And that of global functional limitations was 22% less (PR 0.78 95% CI [0.73– 0.83]) in foreign-born compared to U.S born Blacks.
Conclusion:
Compared to their U.S. born counterparts, foreign-born Black older adults had a markedly lower prevalence of upper and lower functional limitations. Future comparative studies should examine reasons for this apparent health advantage among foreign-born adults to inform social and medical interventions to prevent functional decline in Black older adults in the U.S.
Keywords: Functional limitations, Blacks, Older adults, Upper extremity limitations, Lower extremity limitations
Introduction
Functional limitations, defined as the inability to perform a basic physical activity are strongly associated with increased loss of independence, nursing home admission and mortality in older adults (Bentley et al. 2013, 1621–1632; Alecxih 2010; Koroukian et al. 2016, 630–637). Functional limitations are reported by 23% to 41.4% of United States (U.S.) born and 38.5% of foreign-born Black older adults (Fuller-Thomson et al. 2009, 1333–1336; Dallo, Booza, and Nguyen 2015, 535–542). Functional limitations can occur in the upper and lower extremities (e.g. inability to walk, bend or push an object). These limitations increase with age (Ervin 2006, 1–7; Holmes et al. 2009), and are higher in women and ethnic minorities (Clay et al. 2015, 271; Ervin 2006, 1–7; Holmes et al. 2009). However, the burden of functional limitations which can lead to poor health outcomes and increase health costs has not been examined in foreign-born Black older adults.
Blacks in the U.S. are often combined into a single racial category in research and public health programing (Read, Emerson, and Tarlov 2005, 205–212; Fontenot 2018). However, a number of studies have shown that foreign-born Blacks are healthier than U.S. born Blacks of the same age (Dupre, Gu, and Vaupel 2012, e37177; Venters and Gany 2011, 333–344). This phenomenon, known as the healthy immigrant effect, is often explained by heathier lifestyles in immigrants’ home countries, healthy self-selection at migration, extensive screening of immigrants before and after arrival (Venters and Gany 2011, 333–344; Wakabayashi 2010, 697–719), and some immigrants returning to their home country as they become disabled. This aggregation of Blacks – U.S. born and foreign-born limits accurate understanding of the functional health of Black older adults.
Additionally, evidence in support of the healthy immigrant effect is obtained largely from research with non-Black racial/ethnic groups, examines chronic diseases (such as obesity or cardiovascular diseases), and the results have been inconclusive. For example, the literature supports the “Hispanic paradox,” in which Hispanic/Latino immigrants are reported to be generally healthier than their U.S. born counterparts (Markides and Eschbach 2005, 68–75; Ruiz, Steffen, and Smith 2013, e60) but this phenomenon has not been established for functional limitations among Blacks. Some studies have reported that Hispanic and Asian foreign-born older adults have similar or even greater burden of functional limitations compared to U.S. born older adults (Dallo, Booza, and Nguyen 2015, 535–542; Melvin et al. 2014, 497–510; Hayward et al. 2014, 81–96).
Research on the healthy immigrant effect and functional limitations in Black immigrants is limited. In one of the few studies that compares foreign-born and U.S. born, Elo and colleagues (2011) reported that Black Caribbean and African immigrants had lower odds of limitations compared to their U.S. born counterparts. However, this sample included younger adults (aged ≥25 years). In one study, foreign-born Black older adults had an increased odds of functional limitations compared to U.S. born Whites, but the increase in odds did not remain after adjusting for citizenship status, years of U.S. residency, and English language ability (Dallo, Booza, and Nguyen 2015, 535–542). Additionally, among those who were ≥20 years at immigration, longer residence in the U.S. was associated with higher levels of functional limitations. Nevertheless, this study compared the foreign-born populations to U.S. born Whites only. These results may not reflect the differences in the burden of functional limitations experienced by foreign-born Black older adults compared to their U.S.-born Black counterparts.
The influx of Black immigrants has increased the diversity of Black older adults in the U.S. There were 4.2 million Black immigrants in the United States in 2016 (Anderson and Lopez 2018). The largest groups of Black immigrants are Afro-Caribbean and African whose population has risen by 33% and 137% respectively since 2000 (Anderson 2015). The growth of the Black immigrant population includes a growing share of older adults; 17% of Afro-Caribbean and 6.3% of African immigrants are 65 years and older (Grieco et al. 2012). The median age of an Afro-Caribbean immigrant is 46 and that of an African immigrant 37 years (Anderson 2015). In the next 30 years, these adults will be in their sixties. Older adults will continue to be growing segment of the Black immigrant population.
Immigration influences the health outcomes of Black immigrants through multiple factors including acculturation and migration selectivity (Garcia and Reyes 2017). Acculturation has been associated with both negative and positive health outcomes (Lara et al. 2005, 367–397; Gee and Ponce 2010, 888–895; Gubernskaya, Bean, and Van Hook 2013, 427–443). Immigrants may engage in negative health behaviors through acculturation that subsequently exacerbate diseases (Agyemang et al. 2009, 1; Population Reference Bureau 2013). Some health behavior changes related to acculturation include higher fat intake, lower consumption of fruits and vegetables (Neuhouser et al. 2004, 51–57), increased intake of fast foods (Okafor, Carter-Pokras, and Zhan 2014, 226–235) and smoking (Garcia and Reyes 2017). Older immigrants, especially those who migrate in older age with medical problems (Gubernskaya, Bean, and Van Hook 2013, 427–443; Lum and Vanderaa 2010, 743–753) face greater risk of health decline with adoption of negative health behaviors. Negative health behaviors may increase risk for chronic diseases which in turn affect functional limitations in Black immigrants.
The factors that impact the health of U.S. born Blacks may differ from that of foreign-born Blacks and may lead to differences in physical function related health outcomes. Therefore, the purpose of this study was to examine the relationship between birthplace and functional limitations in Black older adults in the 2010–2016 National Health Interview Surveys. An understanding of these differences will provide insight into the functional health of aging Blacks.
Methods
Data source
We used data from the 2010–2016 National Health Interview Survey (NHIS). The NHIS is an annual cross-sectional household survey of the U.S. population conducted by the National Center for Health Statistics. This survey collects demographic, socioeconomic and health status data on U.S. households from the civilian noninstitutionalized population (excludes persons in nursing homes and prisons) and it uses a multistage sampling approach. Data are collected on the family, adults in the family and children using questionnaires specifically created for each group. A detailed description of the survey methods is published elsewhere (National Center for Health Statistics 2016). The NHIS currently oversamples for ethnic minorities and older adults. One adult participant (≥ 18years) present during the survey is randomly selected to complete the adult questionnaire. Annually, the NHIS has an 80% response rate and collects information on place of birth. Data used in this analysis is obtained from the adult sample.
Measures
Outcomes
We included three measures of functional limitations: lower extremity (LE), upper extremity (UE), and global functional limitations. LE limitations were measured by difficulty in at least one of the following: difficulty walking a quarter of a mile, climbing ten stairs, standing for two hours, or stooping. LE limitations were assessed in NHIS with the question “How difficult is it to walk, stand, climb, or stoop without special equipment?” UE limitations were measured by difficulty in at least one of the following: reaching for overhead objects, grasping small objects, carrying 10 pounds, and pushing large objects. UE limitations were assessed in NHIS with the question: “How difficult is it to reach, grasp, carry or push things without special equipment?” Responses for both UE and LE limitations in the NHIS survey were ordinal from “Not at all difficult”, to “Can’t do at all”. Participants who refused, responses that weren’t ascertained or didn’t know (674 (5% of sample)) were excluded from this analysis. The global functional limitations variable was assessed by asking the participant if they had “Any functional limitation, all conditions” with the following response options: 2- “Not limited in any way” 1- “1 Limited in any way” and 3- unknown if limited. This question is a recoded variable in the NHIS dataset that measures if participants have any difficulty with one or more domains of function that includes upper extremity, lower extremity and other functional domains (difficulty going to events, participating in social activities or relaxing at home without special equipment). Responses were dichotomized into 1 if limited and 0 if not limited. The unknown (3- unknown if limited (n=42)) response was excluded from this analysis.
Exposure
The main exposure of interest was nativity status. A foreign- born Black was defined as any individual who reported their race as Black and who was not born in the United States. While a U.S.-born Black is one who reported Black as their race and was born in the U.S. A birthplace variable was created to represent foreign-born and U.S. born Black older adults, where foreign born was 1, and U.S. born was 0. Amongst foreign-born Blacks, length of stay is explored. This is the number of years that participants have resided in the U.S. Five categories were included in the analyses: “Less than 1 year”, “1 year- less than 5 years”, “5year - less than 10 years”, “10 years- less than 15 years” and “15 years or more”.
Covariates
Covariates examined include sociodemographic characteristics, medical conditions and physical activity. Age, gender, education, marital status and poverty status are the sociodemographic variables included in this analysis. Poverty status was defined by income to poverty ratio: <1.00 [below federal poverty line], 1.00–1.99, 2.00–2.99, 3.00–4.99, and ≥5.00). NHIS ask about income to poverty threshold using current family size and the U.S. Census Bureau poverty thresholds from the previous year (National Center for Health Statistics 2014). We recoded this variable as not poor/near poor (>2), near poor (between 1–2) and poor (<1). Chronic medical conditions included were: hypertension, diabetes, obesity, arthritis, asthma and visual impairment. All chronic condition responses were categorized as Yes or No. Finally, a physical activity variable was created to represent minutes and frequency of self-reported exercise in relation to the national exercise guidelines for older adults (Centers for Disease Control and Prevention 2015). Physical activity was coded as meeting guidelines if participant exercised moderately over 150 minutes or vigorously for over 75 minutes weekly and not meeting guidelines otherwise. Healthcare access was assessed with a yes or No response to the question whether individuals usually go to routine/preventive care. All medical conditions and related variables are self- reported.
Statistical Analysis
All analyses were conducted in Stata 15 I/C (StataCorp 2015).To increase the stability of estimates, we pooled data from the 2010–2016 NHIS surveys and weighted the dataset to account for the complex sampling design using National Center for Health Statistics (NCHS) guidelines (National Health Interview Survey 2015). To describe the sample, weighted means (continuous variables) and percentages (categorical variables) were computed by birth place. To examine proportions of functional limitations by years of U.S residency in foreign-born Black older adults only, two way tabulations with the Pearson’s chi-square test of independence were used (StataCorp 2009, 113–119). To examine the unadjusted and adjusted relationships between place of birth and functional limitations, we fitted generalized linear models using a Poisson distribution and logarithmic link function. This modified Poisson regression approach has been shown to provide robust estimates of the standard errors for relative risk (Zou 2004, 702–706). We used the margins command to obtain estimates of the adjusted prevalence of functional limitations from the generalized models (Williams, R. 2012, 308). The margins command offers predicted prevalence and prevalence ratios based on the current analytic model. These models were also used to identify the predictors of functional limitations in Black older adults. Covariates included in these models were chosen because of their clinical importance and documented association with functional limitations (Stuck et al. 1999, 445–469). We opted to adjust for risk factors for cancer, stroke and heart disease. Including the risk factors as well as the health outcomes would result in over-adjustment of the model. Sensitivity analyses were done by running models with these health outcomes and results were similar to those in models with the risk factors. U.S. born participants were the reference group in our analyses.
Results
Characteristics of sample by birthplace
We included 14,438 U.S. born and 1,583 foreign-born Black older adults who were 50 years or older. The socio-demographic and health characteristics of the participants by place of birth are described in detail in Table 1. U.S. born Blacks were approximately 1 year older than their foreign-born counterparts [63.56 (0.12) vs.62.06 (0.32)]. Foreign-born older adults were more likely to report having a college degree or higher than the U.S. born older adults (26% vs. 17%; p<0.0001), and were less likely to be poor (have income to poverty ratios between 1–2 or <1 below federal poverty level) than U.S. born adults. The majority (92%) of foreign-born older adults had lived in the U.S. for ten years or more. Those born outside the U.S were less likely to report having health insurance than the U.S-born older adults (87% vs 91%; p<0.0001). Foreign- born Black older adults had significantly lower prevalence of overweight/obesity, hypertension, arthritis, visual impairment and asthma (all p<0.001) than their U.S-born counterparts. There was no significant difference in diabetes prevalence by place of birth. Twenty-three percent of the foreign-born and 26% of the U.S-born Black older adults reported having a diabetes diagnosis. A little over half (53%) of foreign-born and U.S-born Blacks (51%) met national exercise recommendations.
Table1:
Characteristics of the sample by birth place (N=16,021)
| Characteristic [Mean (SE)/ %] | U.S. Born (Number, Weighted %) N=14438 | Foreign-Born (Number, Weighted %) N=1583 | P-value |
|---|---|---|---|
| Age, mean (SE) | 63.56 (0.12) | 62.06 (0.32) | <0.001 |
| Female | 8,655 (59.69%) | 882 (55.25%) | 0.005 |
| Marital Status | |||
| Married | 3,944 (28.14%) | 647 (41.53%) | <0.0001 |
| Separated /Divorced | 7,654 (52.82%) | 691 (44.81%) | |
| Single/Never Married | 2,784 (19.05%) | 237 (13.65 %) | |
| Level of Education | |||
| ≤ HS | 7,889 (53.40%) | 849 (50.51%) | <0.001 |
| Above HS but less than college | 4,096 (29.42%) | 339 (23.51%) | |
| College and Above | 2,337 (17.18%) | 364 (25.98%) | |
| Poverty Status | |||
| Not poor/Near poor (>2) | 8,372 (59.76%) | 985 (65.71%) | <0.001 |
| Near Poor (≥1 & <2) | 3,047 (20.30%) | 311 (17.36%) | |
| Poor (<1) | 3,019 (19.94%) | 287 (16.93%) | |
| Health Insurance (Yes) | 13,079 (90.95%) | 1,340 (86.64%) | <0.001 |
| Length of stay ≥10years | N/A | 1,430 (92.43%) | |
| Body Mass Index | <0.001 | ||
| Normal weight | 3,126 (21.67%) | 389 (24.06%) | |
| Overweight | 4,765 (32.82%) | 652 (41.01%) | |
| Obese | 6,351 (44.27%) | 536 (34.55%) | |
| Underweight | 196 (1.25%) | 6 (0.38%) | |
| Diabetes | 3,189 (25.66%) | 324 (23.29%) | 0.17 |
| Hypertension | 9,913 (67.86%) | 852 (54.27%) | <0.001 |
| Visual Impairment | 2,558 (17.50%) | 181 (11.14%) | <0.001 |
| Arthritis | 6,623 (45.50%) | 427 (27.19%) | <0.001 |
| Asthma | 2,129 (14.92%) | 131 (7.62%) | <0.001 |
| Meets Exercise guidelines | 7,359 (50.83%) | 850 (53.19%) | 0.12 |
| Routine Preventive checks | 12,793 (95.78%) | 1,353 (97.21%) | 0.02 |
Prevalence and Prevalence Ratios of Functional Limitations
Unadjusted prevalence, adjusted prevalence and prevalence ratios of functional limitations are presented in Table 2. In the unadjusted analysis, Black older adults born in the U.S. were more likely to have upper (46% vs. 29%; p<0.001) and lower (61% vs. 40%, p<0.001) extremity limitations than their foreign-born participants. Final models were adjusted for age, gender, education, marital status, visual impairment, diabetes, obesity, hypertension, arthritis, and physical activity. After adjusting for these covariates, U.S-born blacks had higher prevalence of lower extremity functional limitations compared to foreign- born blacks (PR 0.78; 95%CI [0.73–0.84]). The prevalence of UE limitations in foreign-born Blacks was 27% lower compared to U.S. born Black older adults (PR 0.73 95%CI [0.68–0.79]). Results were similar for global functional limitations, with a higher prevalence in U.S. born older adults (59.3% vs. 46.4%). The prevalence of global functional limitations was 22% lower in foreign born Blacks compared to U.S born Blacks (PR 0.78 95% CI [0.73– 0.83]. After adjustment for covariates, the prevalence of all limitations in foreign born Blacks increased while that of U.S. born Blacks decreased.
Table 2.
Prevalence and Prevalence Ratios of Lower, Upper Extremity, and global Functional Limitations
| U.S. born Blacks | Foreign-born Blacks | |||||
|---|---|---|---|---|---|---|
| Unadjusted Prevalence (%) | Adjusted† Prevalence (%) | Adjusted† Prevalence Ratio (95% CI) | Unadjusted Prevalence (%) | Adjusted† Prevalence (%) | Adjusted† Prevalence Ratio (95% CI) | |
| Lower Extremity | 60.6 | 59.5 | Reference | 40.3 | 46.4 | 0.78 (0.73–0.84) |
| Upper Extremity | 46.2 | 45.1 | Reference | 28.7 | 33.1 | 0.73 (0.68–0.79) |
| Global Functional Limitations | 60.5 | 59.3 | Reference | 40.5 | 46.4 | 0.78 (0.73–0.84) |
Adjusted for: age, gender, education, marital status, visual impairment, diabetes, obesity, hypertension, arthritis and physical activity
Analysis of functional limitations in the foreign-born Blacks by length of residence in the U.S. was conducted and presented in Figure 1(also see table 5 supplemental material). There was a similar pattern in the prevalence of all (LE, UE & global) functional limitations in immigrants by their years of U.S. residency. Foreign-born Black older adults who had been in the U.S. for less than a year had the highest prevalence of functional limitations (UE, LE & global functional limitations). This was followed by high prevalence for those residing in the country between 5–10 years. The prevalence of limitations for those who have been residing in the U.S. for 1–5, 10–15 and over 15 years were similar hovering between 25–40%. However, only the prevalence of LE limitations was statistically different across the years of U.S. residency.
FIG. 1:
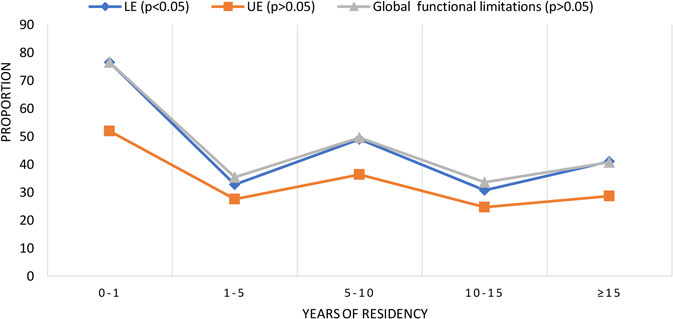
Functional Limitations in Black Immigrant Older Adults by Years of Residency in the U.S.
Older age, being female, single status (separated/divorced/widowed or never married), having less education, visual impairment, diabetes, hypertension, and arthritis were significantly associated with a higher prevalence of limitations (see table 3 in supplemental material). There was a higher prevalence (PR 1.26 95% CI [1.21 – 1.31]) of UE limitations in Black older adults who were over 74 years old compared to those who were 50–64 years older (reference group). Blacks with arthritis had higher prevalence of lower extremity limitations compared to those without arthritis.
Discussion
Prior studies of functional limitations in Blacks in the U.S. have aggregated data on foreign and U.S. born Black into a homogenous racial group. This study sought to examine differences of functional limitations between older U.S. and foreign-born Blacks. Immigration and other diverse life course factors that affect health and wealth-being can lead to heterogeneity of health outcomes among Blacks. Our results show that both the unadjusted and adjusted prevalence of upper and lower extremity limitations were lower in foreign-born Blacks than in U.S. born Blacks. The adjusted prevalence of lower extremity limitations in foreign-born Blacks was 46%, while that of U.S. Born Blacks was 60%. However, the prevalence of functional limitations in foreign-born older adults increased slightly (while that of U.S. born was attenuated) after adjusting for sociodemographic and medical covariates.
There was a significantly higher prevalence of functional limitations for U.S. born Black older adults. Sixty one percent of U.S. born and 40% of foreign-born Blacks had global functional limitations which was higher than the prevalence of 41.4 % (U.S. born) and 38.5 % (foreign-born) reported by Dallo et al. (Dallo, Booza, and Nguyen 2015, 535–542). These results are similar to the 60% prevalence for males reported by McGrath and colleagues (McGrath et al. 2017, 1–12) from analysis of the National Health and Nutrition Examination Survey. Yet, it was lower than the 68% observed in U.S. born Black female older adults (McGrath et al. 2017, 1–12). However, McGrath and colleagues measured more domains of functional limitations (including ‘getting in and out of bed’, ‘using a fork, knife and cup’, and ‘dressing yourself’) than the current study. Rates of upper and lower extremity limitations in this sample were much higher than those reported by what Elo, Mehta and Wang (9–14.4% in US. born and 3.6–9.4% in foreign-born Blacks) from the 2000 cycle of the NHIS (Elo, Irma, Mehta, and Huang 2008). However, younger adults (25+) were included in the Elo and colleagues’ sample which could have led to an underestimation since functional limitations are more prevalent in older adults. Measurement of functional limitations is very heterogeneous and often poses a challenge in comparing function across different studies.
Analyses of functional limitations by birth place in Black older adults in the U.S. is limited. Using a small sample(N=100), Keane and colleagues report that there were no differences in number of basic and instrumental activities of daily living amongst U.S. born and Afro- Caribbean immigrant older adults (Keane et al. 2009, 44–62). Limitation in ability to perform activities of daily living can include some UE and LE limitations. However, activities of daily living are much further down the disability pathway where UE and LE limitations are considered precursors to limitations in activities of daily living (Verbrugge and Jette 1994, 1–14). So far, studies that compare physical function in foreign born to all U.S born older adults (Gubernskaya, Bean, and Van Hook 2013, 427–443; Wakabayashi 2010, 697–719) or to U.S. born Whites only (Dallo, Booza, and Nguyen 2015, 535–542) suggest that immigration at older age is associated with more functional limitations (Wakabayashi 2010, 697–719; Gubernskaya, Bean, and Van Hook 2013, 427–443), therefore comparison of the differences between U.S. and foreign born Black older adults that include age at migration might be useful.
An unexpected but significant finding was the similarity in prevalence of diabetes for U.S. and foreign born Black older adults. From analyses of the NHIS Ford et al. show that after controlling for sociodemographic factors and obesity, foreign born Blacks and U.S Born Blacks have similar prevalence and odds of diabetes (Ford, Narayan, and Mehta 2016, 71–84). Horlyck-Romanovsky et al reported that foreign-born Blacks in New York had higher odds of diabetes compared to their U.S. born counterparts (Horlyck-Romanovsky et al. 2018, 1–9). Acculturation which can involve the uptake of poor dietary habits may be a possible explanation for the rising prevalence of diabetes in Black immigrants (Garcia and Reyes 2017; Okafor, Carter-Pokras, and Zhan 2014, 226–235; Neuhouser et al. 2004, 51–57). Commodore-Mensah and colleagues found from analyses of the NHIS data that longer residence in the U.S. (a proxy measure of acculturation) was associated with increased odds of diabetes (Commodore-Mensah et al. 2016, e004059). While the pathway is not fully known, diabetes is associated with increased risk of functional limitations (Wong et al. 2013, 106–114).
This cross-sectional analysis supports the healthy immigrant hypothesis but analyses of functional limitations in immigrants by years of residency suggests a more complex picture. The research to date on the healthy immigrant effect in Blacks shows that immigrants fare better on the following outcomes: mortality, perinatal health, mental health, overweight and obesity, cancers, injuries, and self-assessed general health (Cunningham, Ruben, and Narayan 2008, 623–635). Our results show that foreign born Blacks had a lower prevalence of functional limitations. Additionally, except for diabetes, foreign born older adults had a lower prevalence of all chronic conditions compared to their U.S. born counterparts. A possible explanation of this health advantage in foreign born Black older adults’ maybe the absence of the cumulative effects of structural and interpersonal racial discrimination known to impact multiple health outcomes in U.S. born Blacks (Lewis, Cogburn, and Williams 2015, 407–440; Williams, D. R., Neighbors, and James 2003, 200–208; Williams, D. R. and Mohammed 2009, 20–47). Additionally, as suggested by many, migrant self-selection where only the healthy and wealthy are able to migrate (Kennedy, McDonald, and Biddle 2006, 164; Venters and Gany 2011, 333–344; Wakabayashi 2010, 697–719), presents another possible explanation for why the foreign born Black older adults in this sample were healthier that their U.S. born counterparts. More exploration of the functional health prior to migration and health changes after immigration is needed to understand the functional health of foreign born Black older adults.
The growing Black immigrant population, and increasing calls from researchers and public health planners has led to more initiatives to disaggregate health outcomes of the U.S. Black population. The U.S. Census bureau will begin to disaggregate the race/ethnicity of Blacks in the 2020 census (Fontenot 2018). This data collection approach and over-sampling for diverse Black ethnic groups in national surveys will enable adequate samples in publicly available datasets and facilitate more in-depth explorations of the heterogeneity of functional health outcomes of Black older adults in the United States.
This study has some limitations. Our measures of functional limitations; upper and lower extremity limitations was an index of self-reported difficulty in performing everyday physical activities. Also, many of the study covariates were self-reported. Self-report is prone to bias and it might be possible that the prevalence of functional limitations and chronic conditions might be under or overestimated which can affect the relationships and differences examined in this study. The NHIS is a cross-sectional survey which precludes any determination of causality and limits our ability to determine whether immigrants arrive in the U.S. healthy and without any functional limitations. The analyses of functional limitations by length of stay showed that newly arrived immigrants (≤1years of U.S. residency) had the highest prevalence of functional limitations, this finding may suggest that some immigrant older adults may be immigrating with functional limitations.
This study has several strengths. It uses a large, nationally representative population-based dataset to examine the differences in the specific and global functional limitations in immigrant Black older adults in the U.S. We believe this study adds to the body of knowledge on functional limitations in Black older adults in the U.S. as it uses a Black immigrant sample that is older than the samples typically used in examining functional limitations. It also adds to the healthy immigrant effect literature by examining the relationship between birthplace and functional limitations in Blacks older adults in the U.S.
Disaggregation of the health outcomes in Black ethnic groups is relatively new and this study adds to this body of evidence and can inform health interventions. Older adults typically have more chronic conditions that interact with the aging process to impact functional health. Our results showed that U.S. born Black older adults had greater prevalence of functional limitations compared to their foreign-born counterparts, which supports the healthy immigrant hypothesis. Despite this, almost a third of the sample had limitations which have significant personal and societal costs. This study identified the differences in the prevalence of functional limitations between U.S and foreign born Black older adults. Immigration and the post migration process affects the health of Black immigrants, suggesting that the health trajectories of foreign-born Blacks might be different from those of their U.S. born counterparts. Studies such as these highlight the need for adequate tailoring of medical and social interventions to decrease functional limitations, improve health outcomes and quality of life for all Black older adults in the United States.
Supplementary Material
Acknowledgments
Funding details
This work was supported by grants from the Robert Wood Johnson Foundation Health Policy Research Scholar program; National Institute on Aging (NIA# 1F31AG057166-01); and Johns Hopkins Institute for Clinical and Translational Research (ICTR) which is funded in part by Grant Number TL1 TR001078 from the National Center for Advancing Translational Sciences (NCATS) a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins ICTR, NCATS or NIH.
Footnotes
No potential conflict of interest was reported by the authors.
Bibliography
- Agyemang Charles, Addo Juliet, Bhopal Raj, de Graft Aikins Ama, and Stronks Karien. 2009. “Cardiovascular Disease, Diabetes and Established Risk Factors among Populations of Sub-Saharan African Descent in Europe: A Literature Review.” Globalization and Health 5 (1): 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alecxih Lisa Maria B. 2010. Individuals Living in the Community with Chronic Conditions and Functional Limitations: A Closer Look Office of the Assistant Secretary for Planning & Evaluation, United States Department of Health and Human Services. [Google Scholar]
- Anderson Monica. 2015. A Rising Share of the U.S. Black Population is Foreign Born
- Anderson Monica and Lopez Gustavo. 2018. Key Facts about Black Immigrants in the U.S
- Bentley John P., Brown Cynthia J., Gerald McGwin Jr, Patricia Sawyer, Allman Richard M., and Roth David L.. 2013. “Functional Status, Life-Space Mobility, and Quality of Life: A Longitudinal Mediation Analysis.” Quality of Life Research 22 (7): 1621–1632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. “How Much Physical Activity do Older Adults Need?” last modified June 4, accessed December 10th, 2017, https://www.cdc.gov/physicalactivity/basics/older_adults/index.htm.
- Clay Olivio J., Thorpe Roland J. Jr, Wilkinson Larrell L., Plaisance Eric P., Crowe Michael, Sawyer Patricia, and Brown. Cynthia J. 2015. “An Examination of Lower Extremity Function and its Correlates in Older African American and White Men.” Ethnicity & Disease 25 (3): 271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Commodore-Mensah Y, Ukonu N, Obisesan O, Aboagye JK, Agyemang C, Reilly CM, Dunbar SB, and Okosun IS. 2016. “Length of Residence in the United States is Associated with a Higher Prevalence of Cardiometabolic Risk Factors in Immigrants: A Contemporary Analysis of the National Health Interview Survey.” Journal of the American Heart Association 5 (11): e004059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham Solveig Argeseanu, Ruben Julia D., and Venkat Narayan. KM 2008. “Health of Foreign-Born People in the United States: A Review.” Health & Place 14 (4): 623–635. [DOI] [PubMed] [Google Scholar]
- Dallo FJ, Booza J, and Nguyen ND. 2015. “Functional Limitations and Nativity Status among Older Arab, Asian, Black, Hispanic, and White Americans.” Journal of Immigrant and Minority Health / Center for Minority Public Health 17 (2): 535–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dupre Matthew E., Gu Danan, and Vaupel James W.. 2012. “Survival Differences among Native-Born and Foreign-Born Older Adults in the United States.” PLoS ONE 7 (5): e37177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo Irma T., Mehta Neil K., and Huang Cheng. 2011. “Disability among Native-Born and Foreign-Born Blacks in the United States.” Demography 48 (1): 241–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo Irma, Mehta Neil, and Huang Cheng. 2008. “Health of Native-Born and Foreign-Born Black Residents in the United States: Evidence from the 2000 Census of Population and the National Health Interview Survey”
- Ervin R. Bethene. 2006. “Prevalence of Functional Limitations among Adults 60 Years of Age and Over: United States, 1999–2002.” Advance Data (375): 1–7. [PubMed] [Google Scholar]
- Fontenot AE Jr 2018. 2020 Census Memo on Race and Ethnicity Questions, January 26, 2018[Memorandum], edited by United State Department of Commerce. Washington DC: [Google Scholar]
- Ford Nicole D., Venkat Narayan KM, and Mehta. Neil K. 2016. “Diabetes among US-and Foreign-Born Blacks in the USA.” Ethnicity & Health 21 (1): 71–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuller-Thomson E, Yu B, Nuru-Jeter A, Guralnik JM, and Minkler M. 2009. “Basic ADL Disability and Functional Limitation Rates among Older Americans from 2000–2005: The End of the Decline?” The Journals of Gerontology Series A: Biological Sciences and Medical Sciences 64A (12): 1333–1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia MA and Reyes AM. 2017. “Physical Functioning and Disability Trajectories by Age of Migration among Mexican Elders in the United States.” The Journals of Gerontology Series B, Psychological Sciences and Social Sciences. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gee GC and Ponce N. 2010. “Associations between Racial Discrimination, Limited English Proficiency, and Health-Related Quality of Life among 6 Asian Ethnic Groups in California.” American Journal of Public Health 100 (5): 888–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grieco EM, Acosta YD, de la Cruz GP, Gambino C, Gryn T, Larsen LJ, Trevelyan EN, and Walters NP. 2012. The Foreign-Born Population in the United States: 2010.
- Gubernskaya Z, Bean FD, and Van Hook J. 2013. “(Un)Healthy Immigrant Citizens: Naturalization and Activity Limitations in Older Age.” Journal of Health and Social Behavior 54 (4): 427–443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayward Mark D., Hummer Robert A., Chiu Chi-Tsun, González-González César, and Wong. Rebeca 2014. “Does the Hispanic Paradox in US Adult Mortality Extend to Disability?” Population Research and Policy Review 33 (1): 81–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes Julia, Powell-Griner Eve, Lethbridge-Cejku Margaret, and Heyman Kathleen. 2009. “Aging Differently: Physical Limitations among Adults Aged 50 Years and Over: United States, 2001–2007.” NCHS Data Brief 20 (1). [PubMed] [Google Scholar]
- Horlyck-Romanovsky Margrethe F., Wyka Katarzyna, Echeverria Sandra E., May Leung May, Melissa Fuster, and Huang. Terry T-K 2018. “Foreign-Born Blacks Experience Lower Odds of Obesity but Higher Odds of Diabetes than US-Born Blacks in New York City.” Journal of Immigrant and Minority Health: 1–9. [DOI] [PubMed]
- Keane Florence, Tappen Ruth M., Williams Christine L., and Rosselli Monica. 2009. “Comparison of African American and Afro-Caribbean Older Adults’ Self-Reported Health Status, Function, and Substance Use.” Journal of Black Psychology 35 (1): 44–62. [Google Scholar]
- Kennedy Steven, McDonald James Ted, and Biddle Nicholas. 2006. “The Healthy Immigrant Effect and Immigrant Selection: Evidence from Four Countries”: 164. https://socialsciences.mcmaster.ca/sedap/p/sedap164.pdf.
- Koroukian Siran M., Schiltz Nicholas, Warner David F., Sun Jiayang, Bakaki Paul M., Smyth Kathleen A., Stange Kurt C., and Given Charles W.. 2016. “Combinations of Chronic Conditions, Functional Limitations, and Geriatric Syndromes that Predict Health Outcomes.” Journal of General Internal Medicine 31 (6): 630–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara Marielena, Gamboa Cristina, Iya Kahramanian M, Morales Leo S., and Hayes Bautista. David E. 2005. “Acculturation and Latino Health in the United States: A Review of the Literature and its Sociopolitical Context.” Annu. Rev. Public Health 26: 367–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis Tené T., Cogburn Courtney D., and Williams David R.. 2015. “Self-Reported Experiences of Discrimination and Health: Scientific Advances, Ongoing Controversies, and Emerging Issues.” Annual Review of Clinical Psychology 11: 407–440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lum Terry Y. and Vanderaa Julianne P.. 2010. “Health Disparities among Immigrant and Non-Immigrant Elders: The Association of Acculturation and Education.” Journal of Immigrant and Minority Health 12 (5): 743–753. [DOI] [PubMed] [Google Scholar]
- Markides KS and Eschbach K. 2005. “Aging, Migration, and Mortality: Current Status of Research on the Hispanic Paradox.” The Journals of Gerontology.Series B, Psychological Sciences and Social Sciences 60 Spec No 2: 68–75. [DOI] [PubMed] [Google Scholar]
- McGrath Ryan P., Ottenbacher Kenneth J., Vincent Brenda M., Kraemer William J., and Peterson Mark D.. 2017. “Muscle Weakness and Functional Limitations in an Ethnically Diverse Sample of Older Adults.” Ethnicity & Health: 1–12. [DOI] [PubMed]
- Melvin J, Hummer R, Elo I, and Mehta N. 2014. “Age Patterns of Racial/Ethnic/Nativity Differences in Disability and Physical Functioning in the United States.” Demographic Research 31: 497–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. 2014. 2013 National Health Interview Survey (NHIS) Public use Data Release: Survey Description Hyattsville, Maryland. [Google Scholar]
- National Center for Health Statistics. 2016. “National Center for Health Statistics. National Health Interview Survey, 2010–2014. Public-use Data File and Documentation 2015” National Health Interview Survey, 2014.Public-use Data File and Documentation. [Google Scholar]
- National Health Interview Survey. 2015. Variance Estimation and Other Analytic Issues, NHIS 2006–2014; 2015
- Neuhouser Marian L., Thompson Beti, Coronado Gloria D., and Solomon Cam C.. 2004. “Higher Fat Intake and Lower Fruit and Vegetables Intakes are Associated with Greater Acculturation among Mexicans Living in Washington State.” Journal of the American Dietetic Association 104 (1): 51–57. [DOI] [PubMed] [Google Scholar]
- Okafor Maria-Theresa C., Carter-Pokras Olivia D., and Zhan. Min 2014. “Greater Dietary Acculturation (Dietary Change) is Associated with Poorer Current Self-Rated Health among African Immigrant Adults.” Journal of Nutrition Education and Behavior 46 (4): 226–235. [DOI] [PubMed] [Google Scholar]
- Population Reference Bureau. 2013. Elderly Immigrants in the United States
- Read Jen’nan Ghazal, Emerson Michael O., and Tarlov Alvin. 2005. “Implications of Black Immigrant Health for U.S. Racial Disparities in Health Blacks are different-can’t lump them together.” Journal of Immigrant Health 7 (3): 205–212. [DOI] [PubMed] [Google Scholar]
- Ruiz John M., Steffen Patrick, and Smith Timothy B.. 2013. “Hispanic Mortality Paradox: A Systematic Review and Meta-Analysis of the Longitudinal Literature.” American Journal of Public Health 103 (3): e60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp. 2015. Stata Statistical Software: Release 14 College Station, TX: StataCorp LP. [Google Scholar]
- StataCorp. 2009. Stata Survey Data Reference Manual Stata Press
- Stuck Andreas E., Walthert Jutta M., Nikolaus Thorsten, Büla Christophe J., Hohmann Christoph, and Beck. John C. 1999. “Risk Factors for Functional Status Decline in Community-Living Elderly People: A Systematic Literature Review.” Social Science & Medicine 48 (4): 445–469. [DOI] [PubMed] [Google Scholar]
- Venters H and Gany F. 2011. “African Immigrant Health.” Journal of Immigrant and Minority Health / Center for Minority Public Health 13 (2): 333–344. [DOI] [PubMed] [Google Scholar]
- Verbrugge LM and Jette AM. 1994. “The Disablement Process.” Social Science & Medicine (1982) 38 (1): 1–14. [DOI] [PubMed] [Google Scholar]
- Wakabayashi Chizuko. 2010. “Effects of Immigration and Age on Health of Older People in the United States.” Journal of Applied Gerontology 29 (6): 697–719. [Google Scholar]
- Williams David R. and Mohammed Selina A.. 2009. “Discrimination and Racial Disparities in Health: Evidence and Needed Research.” Journal of Behavioral Medicine 32 (1): 20–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams David R., Neighbors Harold W., and James. S 2003. “Racial/Ethnic Discrimination and Health: Findings from Community Studies.” American Journal of Public Health 93 (2): 200–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams Richard. 2012. “Using the Margins Command to Estimate and Interpret Adjusted Predictions and Marginal Effects.” Stata Journal 12 (2): 308. [Google Scholar]
- Wong Evelyn, Backholer Kathryn, Gearon Emma, Harding Jessica, Freak-Poli Rosanne, Stevenson Christopher, and Peeters Anna. 2013. “Diabetes and Risk of Physical Disability in Adults: A Systematic Review and Meta-Analysis.” The Lancet Diabetes & Endocrinology 1 (2): 106–114. [DOI] [PubMed] [Google Scholar]
- Zou Guangyong. 2004. “A Modified Poisson Regression Approach to Prospective Studies with Binary Data.” American Journal of Epidemiology 159 (7): 702–706. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


