Endoscopic sleeve gastroplasty (ESG) is a minimally invasive, safe, and effective weight-loss technique first described in 2013.1 The principle is to reduce the gastric capacity by creating a restrictive sleeve through an endoluminal suturing system. This is done by the placement of full-thickness sutures along the corpus of the stomach. Although bariatric surgery is recommended for obesity management, the benefits of ESG include less morbidity and mortality, shorter hospital stays, and quicker recovery times. Surgical treatments are also difficult in patients using peritoneal dialysis (PD). Such patients are frequently prone to infections and surgical adverse events, including higher mortality.2 In this video (Video 1, available online at www.VideoGIE.org), we present a successful ESG performed for a PD patient with clinical success and without adverse events.
Case report
A 51-year-old woman with uncontrolled diabetes mellitus type 2, hypertension, and end-stage renal disease, who had been using PD for 3 years, and who was morbidly obese (body mass index 46.35 kg/m2, weight 257 pounds) was referred for ESG. Dietary and lifestyle modifications had failed. She was also deemed ineligible for surgical weight loss because of the high risk of morbidity and mortality. Kidney transplantation was not possible because of her morbid obesity and suboptimal weight loss. The patient successfully underwent ESG and was treated with prophylactic antibiotic agents, antiemetic agents, and pain medications, and she was discharged after tolerating advancement in diet. At her 2-month follow-up visit, the patient had lost 29 pounds, her body mass index was reduced from 46.35 kg/m2 to 43 kg/m2, and her blood pressure was well controlled with the use of only half of her preprocedure medication.
Endoscopic method
Argon plasma coagulation marked the suture sites in the anterior and posterior wall of the stomach (Fig. 1). A triangular stitch pattern was started at the anterior wall and then was extended to the greater curvature and the posterior wall (Fig. 2). Each stitch pattern consisted of 6 full-thickness stitches before the suture was cinched, forming a plication (Fig. 3). In total, 9 sutures were used. To ensure full-thickness placement of the sutures, a helix device was used to capture the muscularis propria (Fig. 4). The sutures were carried out from the distal to the proximal ends, starting at the incisura angularis and ending at the fundus. The patient was treated with 5 days of empiric antibiotic agents, antiemetic agents, and pain medications, and her diet was advanced slowly. Oral contrast studies at postoperative day 1 and again at 2 weeks (Fig. 5) showed no extravasation and intact sleeve.
Figure 1.
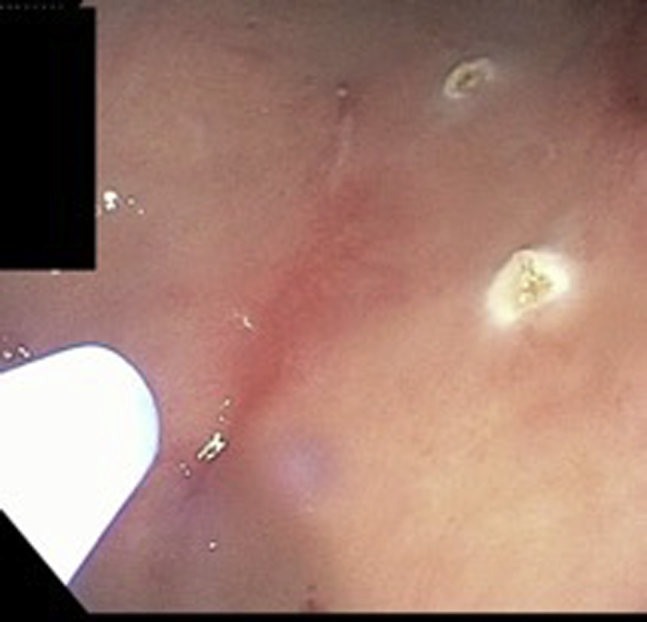
Argon plasma coagulation used to mark walls of stomach.
Figure 2.

Triangular stitch pattern.
Figure 3.
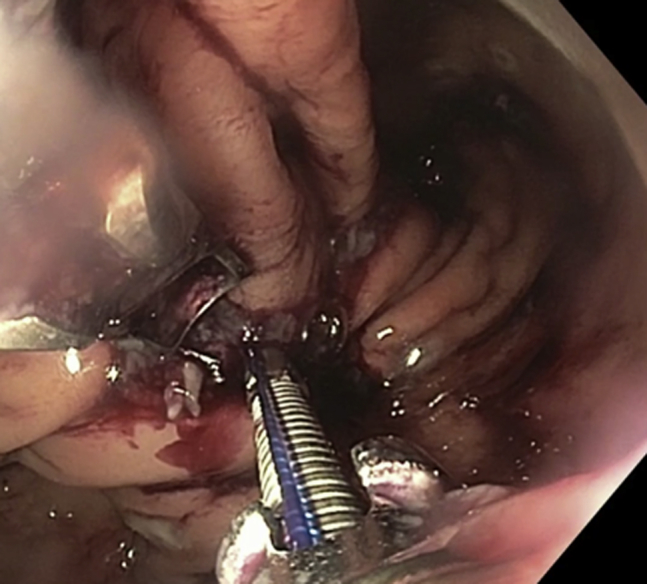
Sutures cinched to form plication.
Figure 4.
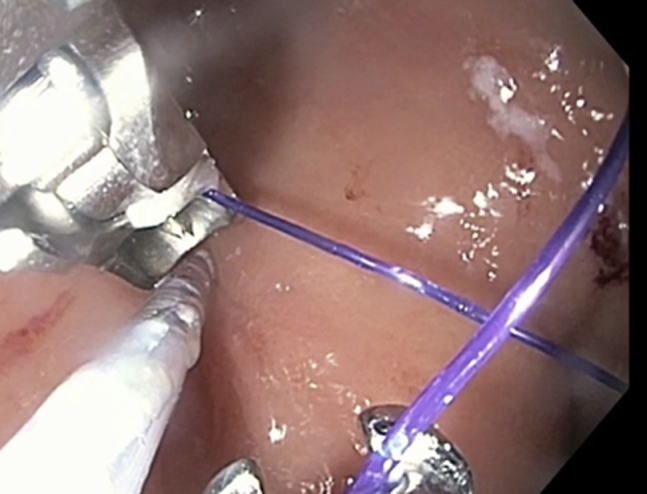
Full-thickness placement of sutures by use of helix device.
Figure 5.
Oral contrast studies at postoperative day 1 and 2 weeks.
Conclusion
This case represents the safety and efficacy of ESG in a patient with end-stage renal disease using peritoneal dialysis. ESG should be considered the first-line therapeutic weight-loss option in this patient population in whom diet and lifestyle modifications have failed, and it may be used as a bridge to kidney transplantation. We recommend that patients be treated with 5 days of prophylactic antibiotics because of increased incidence of infection in this population.
Disclosure
Dr Tyberg is a consultant for Endogastric Solutions, Ninepoint Medical, and Obalon Therapeutics. Dr Kahaleh is a consultant for Concordia Lab and Boston Scientific and the recipient of research funds from Fuji, Pentax, Gore, Aspire, GI Dynamics, Cook, Apollo, Ninepoint Medical, Merit, and Boston Scientific. Dr Sarkar is a consultant for US Endoscopy. All other authors disclosed no financial relationships relevant to this publication.
Footnotes
If you would like to chat with an author of this article, you may contact Dr Kahaleh at mkahaleh@gmail.com.
Supplementary data
Endoscopic sleeve gastroplasty in a patient using peritoneal dialysis.
References
- 1.Abu Dayyeh B.K., Rajan E., Gostout C.J. Endoscopic sleeve gastroplasty: a potential endoscopic alternative to surgical sleeve gastrectomy for treatment of obesity. Gastrointest Endosc. 2013;78:530–535. doi: 10.1016/j.gie.2013.04.197. [DOI] [PubMed] [Google Scholar]
- 2.Andalib A., Aminian A., Khorgami Z. Safety analysis of primary bariatric surgery in patients on chronic dialysis. Surg Endosc. 2016;30:2583–2591. doi: 10.1007/s00464-015-4530-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Endoscopic sleeve gastroplasty in a patient using peritoneal dialysis.



