Abstract
Background and Aims
Certain situations preclude an endoscopic gastroenterostomy (EUS-GE) or enteral stent placement in gastric outlet obstruction (GOO), leaving patients with the option of a surgical bypass or enteral nutrition beyond the point of obstruction. We present a third option in these situations: an endoscopic duodenojejunostomy (EUS-DJ) or jejunojejunostomy (EUS-JJ).
Methods
This was a retrospective review of 5 patients whose anatomy precluded an endoscopic gastrojejunostomy and an enteral stent, who underwent a successful EUS-DJ or EUS-JJ from 2016 to 2018.
Results
Four EUS-DJs and 1 EUS-JJ were performed, with use of a 15-mm cautery-enhanced lumen-apposing metal stent by direct technique. All cases were technically successful. Three patients tolerated an unrestricted diet, but 2 patients needed enteral supplementation or total parenteral nutrition because of severe gastroparesis. There was 1 moderate adverse event: bleeding from severe reflux esophagitis and gastroparesis. No reinterventions were needed on any of these stents, for a median follow-up time of 23 weeks.
Conclusions
When anatomy precludes an EUS-GE or enteral stent, an EUS-DJ or EUS-JJ may have similarly successful outcomes and could help avoid the need for enteral feeding tubes or surgery.
Abbreviations: GE, gastroenterostomy; GJ, gastrojejunostomy; GOO, gastric outlet obstruction; DJ, duodenojejunostomy; JJ, jejunojejunostomy; LAMS, lumen-apposing metal stent; PEJ, enteral feeds via endoscopic jejunostomy; TPN, total parenteral nutrition
Certain situations preclude an endoscopic gastroenterostomy (EUS-GE) in gastric outlet obstruction (GOO), such as intervening colon, distance of the small bowel from the gastric wall >1 cm, or adhesions trapping the small bowel in the right side of the abdomen.1 Luminal stent placement can also be limited if the stricture is very long or sharply angulated, leaving patients with the option of a surgical bypass or enteral nutrition beyond the point of obstruction.2 We present a third option in these situations: an endoscopic duodenojejunostomy (EUS-DJ) or jejunojejunostomy (EUS-JJ), and we review 5 cases.
Methods
A retrospective review of a maintained database on patients undergoing endoscopic bypass in the setting of gastric outlet obstruction from October 2016 to November 2018 was conducted at 2 tertiary referral centers with extensive experience (>4 years) with EUS-GE. Five patients were identified who could not undergo EUS-GE or enteral stent placement, but a window to create an EUS-DJ or EUS-JJ was found. Written informed consents were obtained from patients explaining the non-U.S. Food and Drug Administration approved use of a lumen-apposing metal stent (LAMS) to create enteroenterostomies. The institutional review boards at both institutions approved this study.
Patients and endoscopic methods
Patient 1
A 63-year-old woman with metastatic pancreatic cancer and prior resection of the distal duodenum presented with GOO. She refused a gastrostomy with feeding J-tube. The stricture was not amenable to luminal stent placement because its length exceeded 15 cm, and it had sharp angulations (Fig. 1). No window for a gastrojejunostomy was found. However, in a long endoscope position, from the second part of the duodenum, the downstream jejunum that was filled with contrast material and methylene blue through a nasocystic catheter was identified. A 15-mm cautery-enhanced lumen-apposing metal stent (LAMS), by use of a direct technique (without a guidewire), was used. Stent deployment was challenging in a long endoscope position. However, shortening the endoscope back into the stomach, advancing the LAMS out into its position to puncture, and then readvancing the endoscope to the duodenum allowed successful deployment of the jejunal flange. The duodenal flange was successfully deployed with EUS guidance alone and pushed out of the echoendoscope as it was being withdrawn, successfully creating an EUS-DJ (Figure 2, Figure 3, Figure 4, Figure 5, Figure 6). This allowed her to eat normally, gain 15 kg, and live the rest of her 18 weeks of life without need for enteral nutrition.
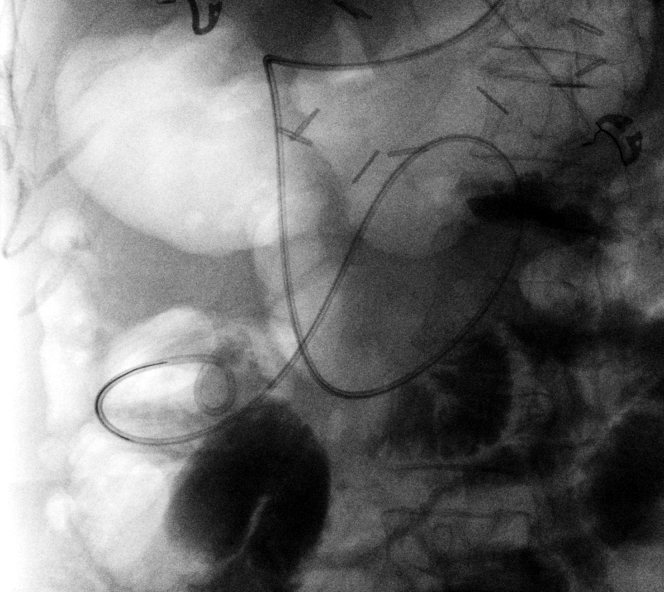
Figure 1.
Fluoroscopic view showing a long and sharply angulated stricture not amenable to EUS-gastrojejunostomy or endoscopic stent placement.
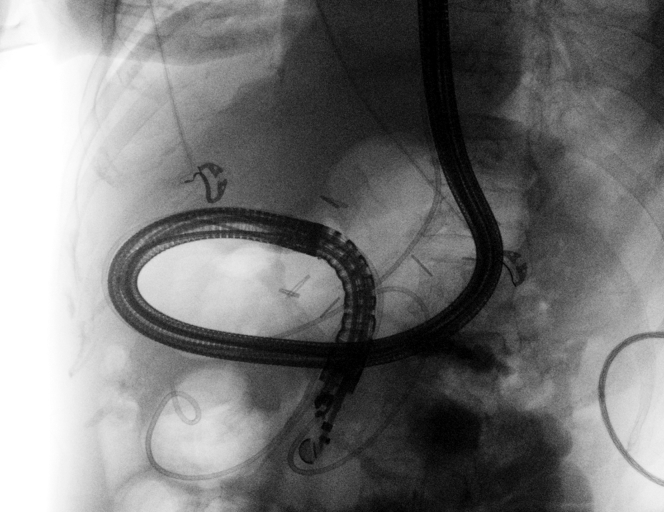
Figure 2.
Nasojejunal tube placed beyond the stricture to allow infusion of dilute methylene blue and contrast material.
Figure 3.
Fluoroscopic view of echoendoscope in a long position, allowing visualization of the postobstructive segment of jejunum from the duodenum.
Figure 4.
Echoendoscopic view of the postobstructive segment of jejunum through the duodenum.
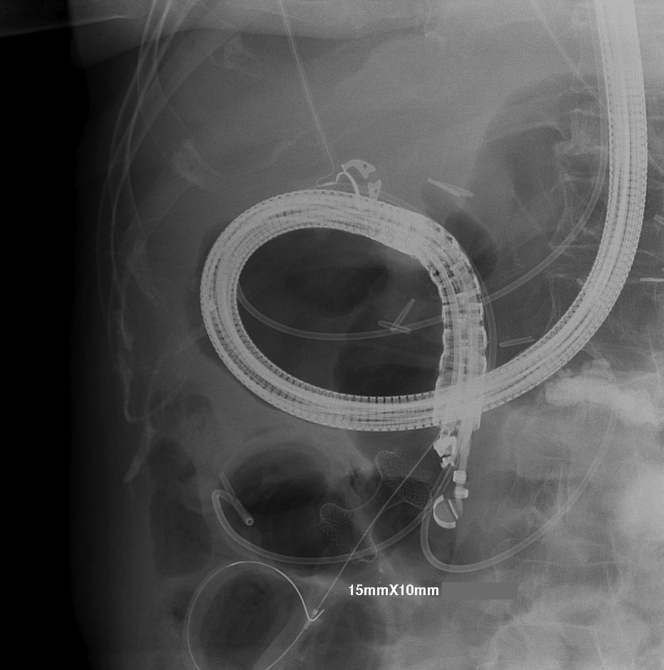
Figure 5.
Fluoroscopic view of 10- × 15-mm lumen-apposing metal stent used to create a duodenojejunostomy.
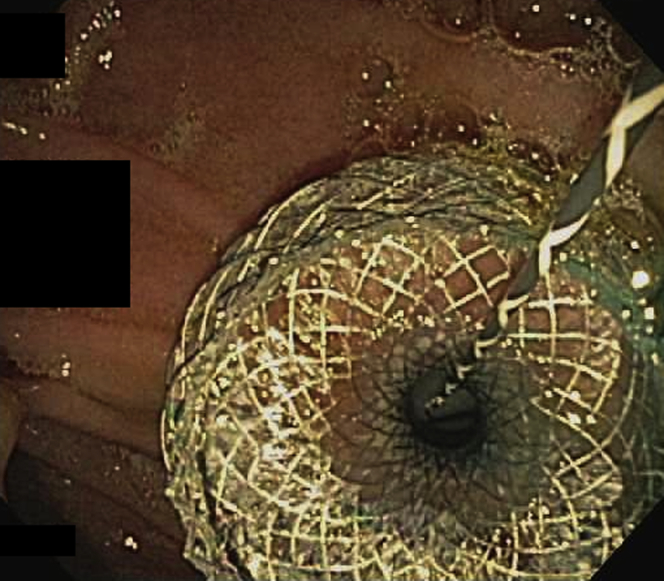
Figure 6.
Endoscopic view of 10- × 15-mm lumen-apposing metal stent used to create a duodenojejunostomy.
Patient 2
A 65-year-old man with prior abdominal radiation for non-Hodgkin’s lymphoma, and a Billroth II procedure for ulcers, presented with GOO and dependence on total parenteral nutrition for 6 months. He was deemed a poor surgical candidate because of his comorbidities and abdominal anatomy. His most severe obstruction was in his efferent jejunal limb, and his anatomy was not amenable to dilations or to enteral stent placement, his condition being of a benign cause. The only window available for bypass was from the proximal efferent jejunal limb to beyond the obstruction. When a 15-mm cautery-enhanced LAMS was used with the direct puncture technique, an EUS-JJ was created. The patient was subsequently found to have an additional narrowing at the surgical gastrojejunostomy, which also underwent stent placement with a 15-mm LAMS. Despite patency of both of these LAMSs and the patient’s toleration of small amounts of a low-residue diet because of significant gastroparesis, he required supplemental enteral nutrition through an endoscopic jejunostomy (Video 1, available online at www.VideoGIE.org).
Patients 3 to 5
Three other cases of EUS-DJ were performed from the first or second portion of the duodenum to the proximal jejunum, by use of a similar technique as described for patient 1. Fluid infusion with a nasobiliary drain was used in 2 of those patients, whereas the other case was performed by infusing 500 mL of methylene blue and contrast material directly past the stricture in the jejunum.
Results
Four EUS-DJs and 1 EUS-JJ have been performed, all by use of a 15-mm cautery-enhanced LAMS by direct technique (without the need for guidewire). The reasons for unsuccessful EUS-GE were either duodenal resections or infiltration with cancers and distance of postobstructive segments of jejunum being >1 cm from the gastric wall. All cases were technically successful (Table 1). Two of the 5 patients needed enteral supplementation or total parenteral nutrition because of severe gastroparesis to meet adequate nutritional needs. The other 3 patients tolerated an unrestricted diet. One patient experienced bleeding from severe reflux esophagitis and gastroparesis (moderate adverse event). No reinterventions were needed on any of these stents during a median follow-up time of 28 weeks (Table 2).
Table 1.
Preprocedural and technical details of 5 patients with gastric outlet obstruction undergoing EUS-DJ or EUS-JJ
| Patient | Cause of GOO | Reason for failed gastrojejunostomy | EUS site | Cautery-enhanced LAMS used (mm) |
|---|---|---|---|---|
| 1 | Recurrent pancreatic cancer after resection | D3-4 duodenectomy | DJ | 10 × 15 |
| 2 | Pancreatic cancer of tail | D3-4 infiltrated; no other loops of jejunum seen | DJ | 10 × 15 |
| 3 | Metastatic ovarian cancer | Carcinomatosis | DJ | 10 × 15 |
| 4 | Metastatic signet cell carcinoma | Jejunum >2 cm from gastric wall | DJ | 10 × 15 |
| 5 | Postsurgical and radiation adhesions | Postobstructive efferent limb not seen from stomach | JJ | 10 × 15 |
GOO, Gastric outlet obstruction; DJ, duodenojejunostomy; JJ, jejunojejunostomy; LAMS, lumen-apposing metal stent.
Table 2.
Clinical outcomes in 5 patients with gastric outlet obstruction undergoing EUS-DJ or EUS-JJ
| Patient | Technical success | Adverse events | Clinical success | Maximum diet tolerated | Reinterventions | Follow-up (weeks) |
|---|---|---|---|---|---|---|
| 1 | Yes | None | Yes | Unrestricted | None | 18 |
| 2 | Yes | None | Yes | Unrestricted | None | 28 |
| 3 | Yes | None | Yes | Unrestricted | None | 59 |
| 4 | Yes | None | No | Full liquids | EGD and TPN∗ | 16 |
| 5 | Yes | Bleeding | No | Low residue | EGD and PEJ† | 40 |
| Median | 28 |
DJ, Duodenojejunostomy; JJ, jejunojejunostomy; PEJ, enteral feeds via endoscopic jejunostomy; TPN, total parenteral nutrition.
Unable to maintain adequate nutrition with full-liquid diet and received supplemental TPN.
Unable to maintain adequate nutrition with low-residue diet because of underlying gastroparesis and received supplemental PEJ.
Conclusions
When advancement of the LAMS is challenging (long endoscope position), withdrawing to a straight endoscope position, advancing the LAMS out of the channel, and then repositioning for puncture can help. Using EUS to deploy the proximal flange in a difficult endoscope position could prevent stent misdeployment.
When an EUS-GE or enteral stent is not possible, an EUS-DJ or EUS-JJ may have similarly successful outcomes and could help avoid the need for enteral feeding tubes or surgery. Larger studies are needed to establish the safety and efficacy of this approach.
Disclosure
Dr Khashab is a consultant for Boston Scientific. The other author disclosed no financial relationships relevant to this publication.
Supplementary data
When unable to do an endoscopic gastroenterostomy or enteral stent, try an endoscopic duodenojejunostomy or jejunojejunostomy.
References
- 1.Chen Y.I., Itoi T., Baron T.H. EUS-guided gastroenterostomy is comparable to enteral stenting with fewer re-interventions in malignant gastric outlet obstruction. Surg Endosc. 2016;31:2946–2952. doi: 10.1007/s00464-016-5311-1. [DOI] [PubMed] [Google Scholar]
- 2.Irani S., Kozarek R.A. Gastrointestinal dilation and stent placement. In: Podolsky D.K., Camillera M., Fitz J.G., editors. Yamada’s textbook of gastroenterology. 6th ed. John Wiley & Sons Ltd; West Sussex, UK: 2016. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
When unable to do an endoscopic gastroenterostomy or enteral stent, try an endoscopic duodenojejunostomy or jejunojejunostomy.