Abstract
Background
In many low and middle-income countries (LMICs), timely access to emergency healthcare services is limited. In urban settings, traffic can have a significant impact on travel time, leading to life-threatening delays for time-sensitive injuries and medical emergencies. In this study, we examined travel times to hospitals in Nairobi, Kenya, one of the largest and most congested cities in the developing world.
Methods
We used a network approach to estimate average minimum travel times to different types of hospitals (e.g. ownership and level of care) in Nairobi under both congested and uncongested traffic conditions. We also examined the correlation between travel time and socioeconomic status.
Results
We estimate the average minimum travel time during uncongested traffic conditions to any level 4 health facility (primary hospitals) or above in Nairobi to be 4.5 min (IQR 2.5–6.1). Traffic added an average of 9.0 min (a 200% increase). In uncongested conditions, we estimate an average travel time of 7.9 min (IQR 5.1–10.4) to level 5 facilities (secondary hospitals) and 11.6 min (IQR 8.5–14.2) to Kenyatta National Hospital, the only level 6 facility (tertiary hospital) in the country. Traffic congestion added an average of 13.1 and 16.0 min (166% and 138% increase) to travel times to level 5 and level 6 facilities, respectively. For individuals living below the poverty line, we estimate that preferential use of public or faith-based facilities could increase travel time by as much as 65%.
Conclusion
Average travel times to health facilities capable of providing emergency care in Nairobi are quite low, but traffic congestion double or triple estimated travel times. Furthermore, we estimate significant disparities in timely access to care for those individuals living under the poverty line who preferentially seek care in public or faith-based facilities.
Keywords: Emergency care, Kenya, Traffic, Poverty
African relevance
-
•
Heavy traffic congestion is an important issues in many African cities.
-
•
Poverty is an important predictor of access to care and health outcomes.
-
•
There is an increasing burden of stroke and myocardial infarction on the African continent.
-
•
Traumatic injury, and particularly motor vehicle collisions, is associated with a high case fatality in Africa
Introduction
Access to timely emergency healthcare services is critical for time-sensitive conditions such trauma, sepsis, stroke, and myocardial infarction among others [[1], [2], [3], [4]]. In low- and middle-income countries (LMICs) the burden of emergency conditions is particularly high [5], yet emergency medical services are often underdeveloped [6], and access to emergency care can be challenging [7]. Understanding where and why delays occur for time-sensitive conditions is critical as policy makers in LMICs seek ways to improve patient outcomes using a public health approach.
Originally developed in the context of maternal mortality, the “three delays” framework is one way in which to examine delays in receiving emergency care [8]. In this framework, delay in service is broken down into the time it takes the patient or someone they know to decide to seek care; the time it takes to get to a facility that can provide appropriate care; and the time it takes to receive the necessary services. Although the second delay, the time it takes to get to a facility, is often discussed in the context of rural areas [9,10], it can also pose a problem in urban centers.
LMICs are at particular risk for transportation delays in urban environments due to traffic as a result of poor street design, an increasing number of cars on the roads, and a lack of active traffic management [11]. The extent of potential transportation delays due to traffic are important to understand, as prior studies have demonstrated that delays in transporting acutely ill or injured individuals from the field to a health facility adversely impacts mortality [12].
Although delays due to traffic congestion may affect an entire city, their impact may not be universally distributed. Research has already demonstrated that poor individuals face more delays in accessing urgent care than non-poor individuals [13]. However, relatively little is known about the relationship between geography and poverty for access to emergency care in LMICs. Important questions exist about the distribution of health facilities in urban areas as they relate to poverty, whether hospital choice (public/faith-based vs. private) could lead to delays in accessing emergency care for impoverished populations, and whether traffic has a compounding effect in poorer communities for patients who require emergency medical care.
In this study, we examined travel time to health facilities capable of providing emergency care in Nairobi, Kenya. We examined travel time under both congested and uncongested conditions, and considered the relationship between travel time, poverty and facility type.
Methods
Kenya is divided into 47 counties, the most populous of which is Nairobi county, whose borders are synonymous with those of the nation's capital city of Nairobi. The metro area has a rapidly-growing population of greater than 6.5 million people. While communicable diseases remain the most common cause of death in Kenya, non-communicable diseases are becoming more prominent as Kenya goes through its epidemiologic transition. Time-sensitive conditions such as ischemic heart disease (5.0% of deaths), stroke (4.8% of deaths), and injury (7.7% of deaths) have seen a relative increase and are likely to continue to grow in the future [14].
Health facilities in Kenya are a mix of public and private. Facilities are assigned levels as per the Kenya Essential Packages for Health (KEPH) based on capacity and services [15]. We considered levels 4 and above as viable candidates to provide emergency care [16,17]. Level 4 facilities are primary/first level hospitals, which should provide Basic Life Support. Level 5, or secondary/second level hospitals, should provide emergency services, including Advanced Life Support. Finally, level 6, or tertiary level facilities provide a full complement of tertiary care services. However, the actual level of care provided may vary [18]. Nairobi contains a large number of hospitals, including one public level 6 hospital, Kenyatta, and four level 5 facilities, only one of which is public [19].
Facility data were downloaded from the Kenyan Ministry of Health website [19]. We selected KEPH level 4, 5, and 6 facilities that were in Nairobi, or the surrounding counties of Kiambu, Machakos, or Kajiado. We included facilities from surrounding counties in the event that those were the closest facilities for individuals living on the edge of Nairobi. We excluded specialty facilities, e.g., maternal, eye, mental, or those that were only dispensaries or only saw outpatients. This left us with 70 facilities (Fig. 1) to consider as part of the analysis.
Fig. 1.
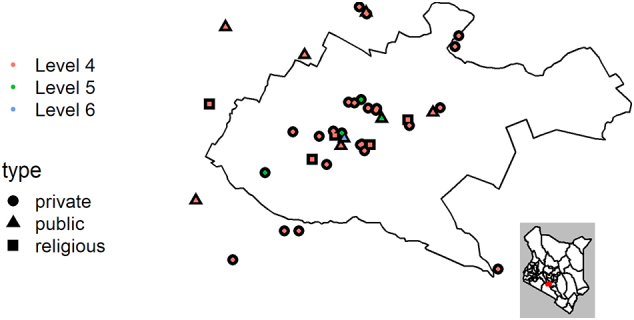
Kenyan health facilities, levels 4–6, in Nairobi and surrounding counties.
Street network data was obtained from Open Street Map, an open-source database of street maps maintained by a global community (https://www.openstreetmap.org/). Population data in 100 m by 100 m squares in 2015 and percent of the population below the poverty line at the 1 km by 1 km square level in 2008 were obtained from the Afripop database (http://www.afripop.org/). The poverty dataset used the Alkire Foster method, where someone was defined as living in poverty if they were deprived in at least one third of ten indices encompassing health, education, and standard of living. Road network data were stored in a PostgresSQL database and converted to a query-able geographic database using PostGIS and pgrouting, extensions to PostgresSQL that allow databases to store geographic data and use algorithms to do different types of routing.
The shapefile for Nairobi was downloaded from the Kenyan Elections portal via the Humanitarian Data Exchange (https://data.humdata.org/dataset/kenya-elections).
Our analysis utilized a method similar to that used by Lee et al. to estimate driving time to eye care services in the United States [20]. Using the network data from Open Street Maps, we created a query-able geographic database, consisting of vertices and edges that correspond to intersections and streets. Because Open Street Maps lacked speed limit information for most streets, we assigned speeds for both uncongested and congested traffic using the speeds suggested by Avner and Lall [21]. Speed limits that were available in the data set were used unless they exceeded the maximum of motorway speed of 110 km/h. For congested speeds in roads not covered by Avner and Lall, we used 2/3 of the uncongested speed.
We created a grid of 0.5 × 0.5 km squares to use as samples, resulting in 2903 sample points throughout the city of Nairobi. This size was selected because it could both show variation over small areas and was computationally manageable. For each grid square centroid, we found the nearest node in the traffic network and the nodes nearest to each of the 70 facilities. The minimum time between each centroid node and each facility node was calculated using Dijkstra's algorithm, where cost was the time it took to travel down each edge [22].
Due to inconsistencies in traffic network data, such as disconnected nodes or closed street loops, our approach yielded a small number (0.4%) of missing values, which were interpolated using simple kriging. This resulted in a raster for each facility that contained travel times to that facility. We then found the minimum value for each pixel in the raster to the closest level 4, 5 or 6 health facility.
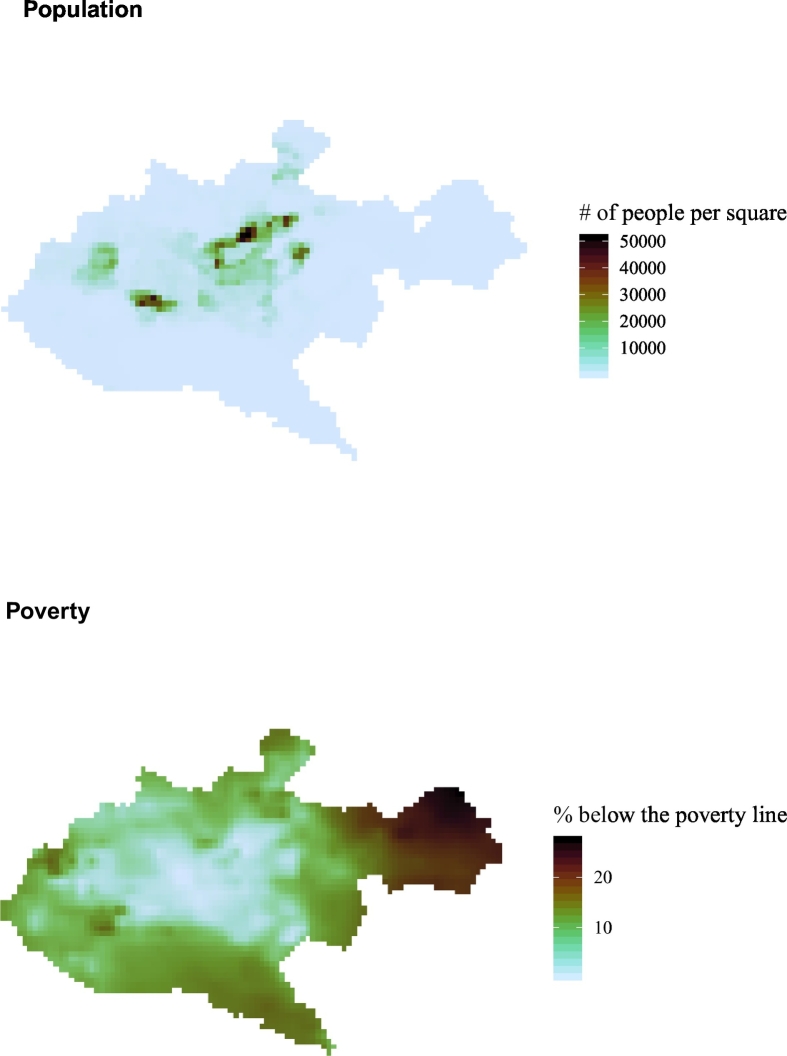
To examine the percentage of the population within a certain travel time of a facility, we aggregated the Afripop population dataset to be the same size squares as our sample grid. Then we resampled to align the grids and scaled to maintain the same overall population total. We followed a similar process for the percent of the population below the poverty line (see Fig. 2 for the resulting rasters). Combined, these two rasters allowed us to estimate the number of people living in each section of the grid, and the number of them living below the poverty line.
Fig. 2.
Rasters of Nairobi population density and poverty.
All database queries, data analyses, and data visualizations were performed using R version 3.3.1 (R Foundation for Statistical Computing, Vienna, Austria. URL http://www.R-project.org).
Results
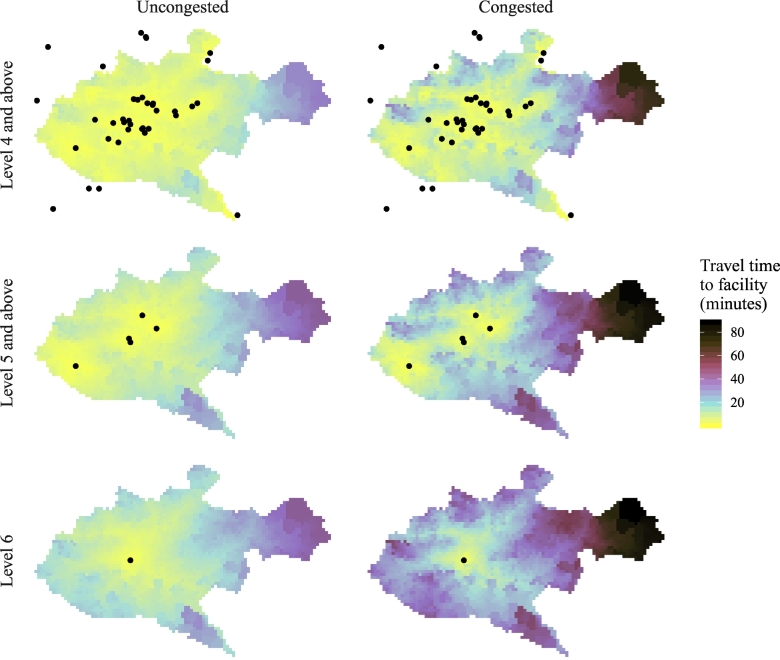
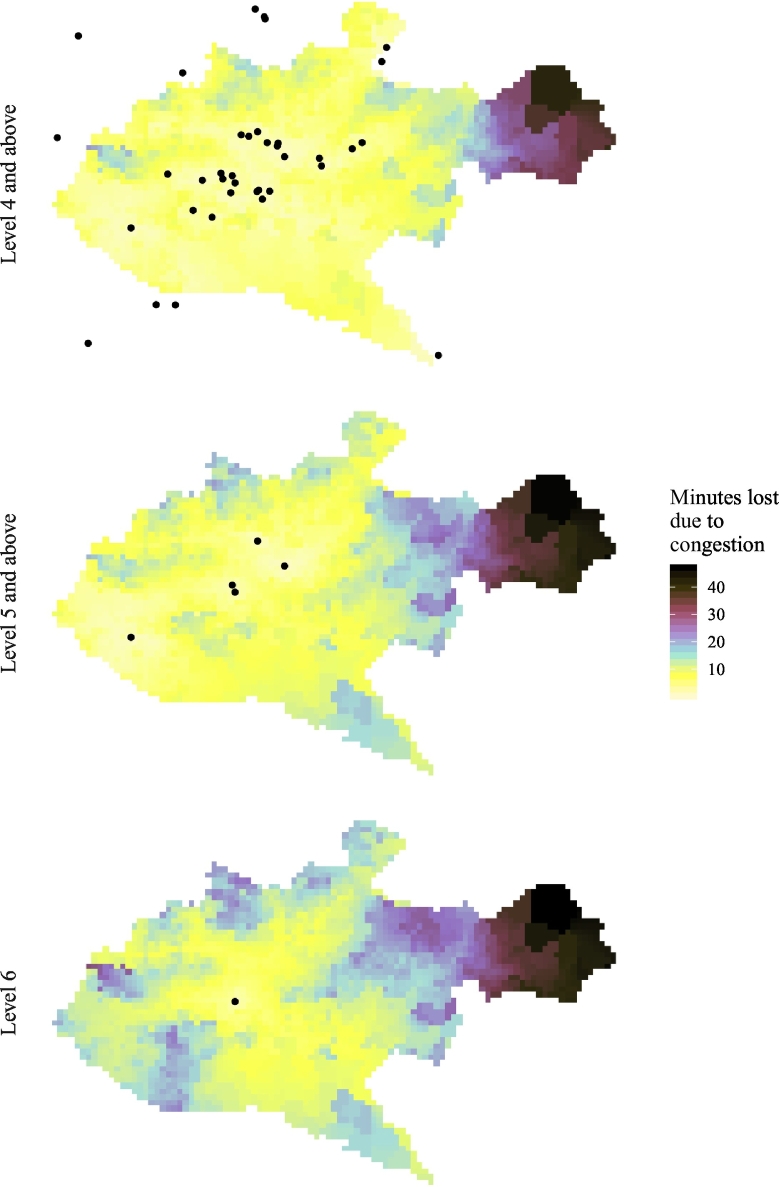
Table 1 presents a summary of average minimum travel times to the nearest level 4, 5 or 6 health facility across Nairobi. These results are presented graphically in Fig. 3. Estimated mean minimum travel time for the population within Nairobi to any facility level 4 and above was 4.5 min (IQR 2.5–6.1) under uncongested conditions and 9.2 min (IQR 4.8–12.4) under congested conditions. Mean travel time to any level 5 and above facilities was 7.9 min (IQR 5.1–10.4) and 14.7 min (IQR 9.7–19.6) under uncongested and congested conditions respectively. For the single level 6 facility, Kenyatta National Hospital, mean travel time was 11.6 min (IQR 8.5–14.2) in uncongested conditions and 22.7 min (IQR 17.0–27.6) when congested. Across all grid points in the city, congestion contributed an additional average travel time of 9 min (IQR 3.4–10.2) to level 4 and above facilities, 13.1 min (IQR 6.6–15.7) for level 5 and above, and 16 min (IQR 10.0–18.6) for transportation to Kenyatta National Hospital (Fig. 4).
Table 1.
Average minimum travel time (in minutes) to health facilities in Nairobi.
| Travel to any facility |
Travel to public/faith-based facilities ONLY |
|||||
|---|---|---|---|---|---|---|
| Level 4 and above | Level 5 and above | Level 6 | Level 4 and above | Level 5 and above | Level 6 | |
| Uncongested | 4.5 | 7.9 | 11.6 | 7.7 | 10.4 | 13.0 |
| Congested | 9.2 | 14.7 | 22.7 | 15.2 | 19.5 | 25.7 |
Fig. 3.
Travel time to the nearest facility under congested and uncongested conditions. Dots represent health facilities.
Fig. 4.
Additional travel time (i.e. minutes lost) to the nearest facility due to congested travel conditions.
Nearly the entire population of Nairobi (99%) was estimated to be within a half hour drive of a level 4 and above facility in uncongested conditions, with an estimated maximum drive time of 33.9 min for the entire population. Estimated maximum drive time to level 5 and above facilities was 41.9 min. Under congested conditions, the estimated maximum drive times within the city were 72.3, 88.0, and 88.5 min to levels 4, 5 and 6 facilities, respectively, although only a small percentage of the population live in such inaccessible areas.
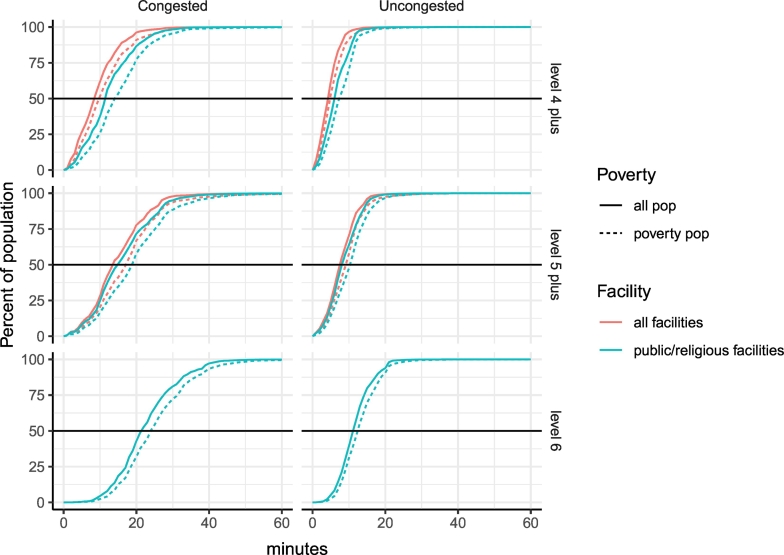
We estimate that individuals living below the poverty line would need to travel slightly longer than the general population to reach care (0.9, 1.4, and 1.4 additional minutes in uncongested conditions for levels 4, 5, and 6 facilities). However, the combined effect of poverty and facility type (public/faith-based vs. private) resulted in more notable effects on travel time (Fig. 5). For people living below the poverty line who had to travel to level 4 or above public or faith-based facilities to receive care, average travel time was estimated to increase to 15.2 min under congested conditions. This represents a 65% increase in travel time compared to the average travel time under the same traffic conditions (9.2 min) if individuals could receive care at any facility, public or private. For travel to level 5 and above facilities, travel time increased by 33% in congested conditions (19.5 vs. 14.7 min). Finally, we found a smaller 11% increase in travel time under congested travel conditions to Kenyatta National Hospital for individuals living in areas of high poverty (25.3 vs. 22.7 min).
Fig. 5.
Percent of the population with access to a specified level of care under congested and uncongested condition. Differentiated by facility ownership (all facilities vs. public/faith-based) and socioeconomic status (general population vs. below poverty line).
Discussion
In this study, we created a novel raster of minimum travel times in uncongested and congested conditions to various levels of health facilities across Nairobi, one of the largest and busiest urban hubs in sub-Saharan Africa. Compared to transport times from high-income settings [23], we found reasonable average travel times to all levels of health facilities in uncongested conditions. However, we noted a marked increase in travel time under heavy traffic conditions, wide variations in travel times across the county, and important differences in equitable access to timely emergency care.
Our underlying assumption is that longer travel times contribute to delays to definitive care that may lead to poorer outcomes. Data on this topic is somewhat limited, as many studies have focused on the impact of sending patients directly to facilities with specialized services for trauma, stroke or ST-elevation myocardial infarction. However, one study examining 30-day mortality rates on days of major marathon events in the United States found a 13.3% increase in mortality compared to non-marathon days, despite controlling for multiple covariates and performing numerous sensitivity analyses [24]. The author also noted a statistically significant increase in average scene to hospital transport time of 4.4 min. These findings likely provide a best-case scenario when compared to low-resource settings where few if any interventions are available in the pre-hospital setting [6,25].
Acknowledging the importance of time-sensitive conditions, transport time has been studied in numerous contexts, including Nairobi. A recent study by Shaw et al. estimated transport time from the site of road traffic collisions (RTCs) to level 4 and above facilities vs. Kenyatta National Hospital for nearly 1000 RTCs in 2015 [26]. They found a median travel time of 7 min vs. 18 min. These findings are consistent with what we report using a different methodology. However, the authors did not examine the impact of traffic nor the relationship between poverty and transport time, which we note can have important repercussions on estimated duration of travel.
Our findings regarding increased average travel time to public/faith-based institutions vs. all facilities is important for several reasons. First, prior research suggests that Kenyans are more likely to seek care at public facilities [27]. Despite the fact that emergency capacity is often less adequate in the public sector and wait times are often longer, the cost of care is a major issue for many Kenyans. Second, Kenyans living below the poverty line often face a double burden of living further away from facilities, and not being able to afford facilities that may be nearby. This means that they may have to travel 50–60% longer, on average, than an individual with more economic resources who could reasonably seek care at any facility. Our finding adds quantitative evidence to prior, mostly qualitative work in sub-Saharan Africa, that suggests that those living below the poverty line often have more limited access to services [28].
Future interventions will require a multifaceted approach to improve transport times for time-sensitive conditions. Urban planning interventions, including pull-out lanes, could improve transport time if they are not used by other vehicles. Stricter enforcement of the laws requiring drivers to pull over for emergency vehicles could significantly reduce transport times during high traffic congestion. The government has already made changes to improve access to emergency care through the Health Act of 2017, which states “any medical institution [public or private] that fails to provide emergency medical treatment while having ability to do so commits an offence and is liable upon conviction to a fine.” [29]. Furthermore, the law states that the national government shall “establish an emergency medical treatment fund.” Future analyses using updated datasets could help establish the impact of this law as it relates to access to emergency care and transport time by widening the potential number of facilities available to the most vulnerable and socioeconomically disadvantaged populations.
Finally, when considering interventions aimed at improving time to emergency care, it is critical to go back to the concept of the “three delays” framework. Transport time from the scene is only one step in this process. There must also be a focus on improving demand-side components through early recognition and increasing utilization of pre-hospital emergency medical services [27]. At the same time, supply-side constraints regarding the availability of ambulances, access to low cost or free pre-hospital services, and having pre-hospital personnel with capacity (i.e. supplies and training) to provide early life-saving treatments will need to be addressed as Nairobi and other cities consider how best to develop comprehensive pre-hospital care systems.
This study is subject to several limitations in terms of data availability, data quality and methodology. Most important was the lack of data on traffic speeds on individual roads. Without such data, our estimates are based on an assumed distribution of speeds during uncongested and congested periods, which is not detailed enough to reflect all real traffic patterns. For example, certain locations, such as the Pushorttam Place, Barclays Plaza, and other locations often act as common choke-points, but our model did not give special consideration to these edges and nodes. However, it should be noted that our results are quite consistent with those obtained through the use of time data used by Shaw and colleagues [26].
Poor data quality regarding directionality of one-way streets also caused challenges. Specifically, when one-way streets are taken into account, poor data quality in local streets meant that many routes had no solution, causing the algorithm to get “trapped” in a circle of one-way streets. Due to this limitation in the data quality, we chose to use an undirected graph, where all streets could be traveled in either direction. This most likely led to an underestimate in travel time because our algorithm could always use the most convenient streets, even if they were one-way. We also did not take into account time taken at stoplights or slowing down to turn. As such, the estimates in this paper should be considered to be minimum travel times.
Finally, limitations exist around the population and poverty data we use in this analysis. The population raster data came from 2008, and well known slums do not appear as prominent on the poverty map as one may expect. Despite these limitations, this paper demonstrates the potential for inequity associated with travel time to a healthcare facility, and raises concerns about treatment for time-sensitive emergent conditions.
Conclusion
This study estimated travel time to facilities in Nairobi using a network approach. We found that simulated traffic congestion resulted in notable transport time delays, with maximum travel times reaching more than half an hour under uncongested conditions and more than an hour under congested conditions. Lower-level hospitals were much more accessible than high-level facilities, with a lower mean travel time across the population. In addition, individuals living below the poverty line were slightly further away from facilities than the overall population, but significant delays were notable when facility choice was restricted to public or faith-based facilities. Future studies should attempt to use actual transport time data, and interventions will need to look across supply and demand-side barriers in addition to transportation specific options in order to improve outcomes from time-sensitive injuries and medical conditions.
Dissemination of results
Results of this study have been shared with some emergency physicians in Nairobi. An earlier version of this manuscript was presented at the University of Washington MPH Thesis Seminar.
Author contribution
Authors contributed as follows to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: MSF contributed 55%; HCD 20%; BWW 15%; ADF 5%, and AYL contributed 5% each. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of competing interest
The authors declared no conflicts of interest. Dr Benjamin Wachira is an editor of the African Journal of Emergency Medicine. Dr Wachira was not involved in the editorial workflow for this manuscript.
Contributor Information
Maya S. Fraser, Email: fraser.maya@gmail.com.
Herbert C. Duber, Email: hduber@uw.edu.
References
- 1.Scholz K.H., Maier S.K.G., Maier L.S., Lengenfelder B., Jacobshagen C., Jung J. Eur Heart J. 2018. Impact of treatment delay on mortality in ST-segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: results from the German prospective, multicentre FITT-STEMI trial. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mueller-Kronast N.H., Zaidat O.O., Froehler M.T., Jahan R., Aziz-Sultan M.A., Klucznik R.P. Systematic evaluation of patients treated with neurothrombectomy devices for acute ischemic stroke: primary results of the STRATIS registry. Stroke. 2017;48:2760–2768. doi: 10.1161/STROKEAHA.117.016456. [DOI] [PubMed] [Google Scholar]
- 3.Seymour C.W., Gesten F., Prescott H.C., Friedrich M.E., Iwashyna T.J., Phillips G.S. Time to treatment and mortality during mandated emergency care for sepsis. N Engl J Med. 2017;376:2235–2244. doi: 10.1056/NEJMoa1703058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McLaughlin C., Zagory J.A., Fenlon M., Park C., Lane C.J., Meeker D. Timing of mortality in pediatric trauma patients: a National Trauma Data Bank analysis. J Pediatr Surg. 2018;53:344–351. doi: 10.1016/j.jpedsurg.2017.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chang C.Y., Abujaber S., Reynolds T.A., Camargo C.A., Obermeyer Z. Burden of emergency conditions and emergency care usage: new estimates from 40 countries. Emerg Med J EMJ. 2016;33:794–800. doi: 10.1136/emermed-2016-205709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mould-Millman N.-K., Dixon J.M., Sefa N., Yancey A., Hollong B.G., Hagahmed M. The state of emergency medical services (EMS) systems in Africa. Prehospital Disaster Med. 2017;32:273–283. doi: 10.1017/S1049023X17000061. [DOI] [PubMed] [Google Scholar]
- 7.Obermeyer Z., Abujaber S., Makar M., Stoll S., Kayden S.R., Wallis L.A. Emergency care in 59 low- and middle-income countries: a systematic review. Bull World Health Organ. 2015;93:577–586G. doi: 10.2471/BLT.14.148338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barnes-Josiah D., Myntti C., Augustin A. The “three delays” as a framework for examining maternal mortality in Haiti. Soc Sci Med 1982. 1998;46:981–993. doi: 10.1016/s0277-9536(97)10018-1. [DOI] [PubMed] [Google Scholar]
- 9.Vanderschuren M., McKune D. Emergency care facility access in rural areas within the golden hour?: Western Cape case study. Int J Health Geogr. 2015;14:5. doi: 10.1186/1476-072X-14-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ouma P.O., Maina J., Thuranira P.N., Macharia P.M., Alegana V.A., English M. Access to emergency hospital care provided by the public sector in sub-Saharan Africa in 2015: a geocoded inventory and spatial analysis. Lancet Glob Health. 2018;6:e342–e350. doi: 10.1016/S2214-109X(17)30488-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jain V., Sharma A. Subramanian L. Road traffic congestion in the developing world. 2012 [Google Scholar]
- 12.Jena A.B., Mann N.C., Wedlund L.N., Olenski A. Delays in emergency care and mortality during major U.S. marathons. N Engl J Med. 2017;376:1441–1450. doi: 10.1056/NEJMsa1614073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Herdman M.T., Maude R.J., MdS C., HWF K., Jeeyapant A., Samad R. The relationship between poverty and healthcare seeking among patients hospitalized with acute febrile illnesses in Chittagong, Bangladesh. PLoS ONE. 2016;11 doi: 10.1371/journal.pone.0152965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet. 2018;392: 1736–1788. doi: 10.1016/S0140-6736(18)32203-7 [DOI] [PMC free article] [PubMed]
- 15.Kenya Health Sector Strategic Investment Plan 2013 to 2017. http://e-cavi.com/wp-content/uploads/2014/11/kenya-health-sector-strategic-investiment-plan-2013-to-2017.pdf Available:
- 16.Wachira B., Martin I.B.K. The state of emergency care in the Republic of Kenya. Afr J Emerg Med. 2011;1:160–165. [Google Scholar]
- 17.Burke T.F., Hines R., Ahn R., Walters M., Young D., Anderson R.E. Emergency and urgent care capacity in a resource-limited setting: an assessment of health facilities in western Kenya. BMJ Open. 2014;4 doi: 10.1136/bmjopen-2014-006132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Institute for Health Metrics and Evaluation. Health Service Provision in Kenya: Assessing Facility Capacity, Costs of Care, and Patient Perspectives. [cited 7 Mar 2018]. Available: http://www.healthdata.org/policy-report/health-service-provision-kenya-assessing-facility-capacity-costs-care-and-patient
- 19.Kenya Master Health Facility List: Find all the health facilities in Kenya. [cited 7 Mar 2018]. Available: http://kmhfl.health.go.ke/#/facility_filter/results
- 20.Lee C.S., Morris A., Van Gelder R.N., Lee A.Y. Evaluating access to eye care in the contiguous United States by calculated driving time in the United States medicare population. Ophthalmology. 2016;123:2456–2461. doi: 10.1016/j.ophtha.2016.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matchmaking in Nairobi: the role of land use (English) | The World Bank. [cited 7 Mar 2018]. Available: http://documents.worldbank.org/curated/en/716381480965677299/Matchmaking-in-Nairobi-the-role-of-land-use
- 22.Dijkstra E.W. A note on two problems in Connexion with graphs. Numer Math. 1959;1:269–271. [Google Scholar]
- 23.Carr B.G., Caplan J.M., Pryor J.P., Branas C.C. A meta-analysis of prehospital care times for trauma. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 2006;10:198–206. doi: 10.1080/10903120500541324. [DOI] [PubMed] [Google Scholar]
- 24.Jena A.B., Mann N.C., Wedlund L.N. Olenski a. delays in emergency care and mortality during major U.S. marathons. N Engl J Med. 2017;376:1441–1450. doi: 10.1056/NEJMsa1614073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kobusingye O.C., Hyder A.A., Bishai D., Hicks E.R., Mock C., Joshipura M. Emergency medical systems in low- and middle-income countries: recommendations for action. Bull World Health Organ. 2005;83:626–631. [PMC free article] [PubMed] [Google Scholar]
- 26.Shaw B.I., Wangara A.A., Wambua G.M., Kiruja J., Dicker R.A., Mweu J.M. Geospatial relationship of road traffic crashes and healthcare facilities with trauma surgical capabilities in Nairobi, Kenya: defining gaps in coverage. Trauma Surg Acute Care Open. 2017:2. doi: 10.1136/tsaco-2017-000130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Broccoli M.C., Calvello E.J.B., Skog A.P., Wachira B., Wallis L.A. Perceptions of emergency care in Kenyan communities lacking access to formalised emergency medical systems: a qualitative study. BMJ Open. 2015;5 doi: 10.1136/bmjopen-2015-009208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peters D.H., Garg A., Bloom G., Walker D.G., Brieger W.R., Rahman M.H. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008;1136:161–171. doi: 10.1196/annals.1425.011. [DOI] [PubMed] [Google Scholar]
- 29.Kenyan Health Act of 2017. [cited 12 Dec 2018]. Available: http://www.kenyalaw.org/lex/actview.xql?actid=No.%2021%20of%202017