Abstract
A 35-year-old male presented with headaches and fevers. MRI of his head showed skull-based infection of the clivus extended to the right internal carotid artery. Blood and sinus cultures were positive for Eikenella corrodens and Streptococcus anginosus. He had intravenous antibiotics and sinus washout. The patient had full neurological recovery following this.
Keywords: Streptococcus anginosus, Eikenella corrodens, Skull-based osteomyelitis, Internal carotid artery infection
Introduction
Skull based osteomyelitis is an uncommon condition that is associated with a 10 % mortality rate and neurologic complication rate of 30 %, as demonstrated by a retrospective study of 42 patients by Johnson et al. [1]. Involvement of Meckel’s cavernous sinus can cause cranial nerve paralysis [[1], [2], [3], [4], [5]]. Patients can have headaches, facial pain, and sinus tenderness. Infections of skull base osteomyelitis can involve temporal, sphenoidal, or frontal bones [[1], [2], [3], [4]]. The incidence of pyogenic osteomyelitis has recently increased, with case reports in the aging population, patients with diabetes, leukemia, and in intravenous drug users [[2], [3], [4], [5]]. The most common organism is Staphylococcus aureus in 21 % and Pseudomonas aeruginosa in 19 % of patients, however oral pathogens have been implicated as well [1].
Initial management when osteomyelitis is suspected is obtaining anaerobic and aerobic blood cultures [6]. Broad spectrum antibiotics must be started as soon as possible and then deescalated based upon sensitivities [6]. Blood cultures are positive in cases of hematogenous osteomyelitis [6]. MRI of the bone has a sensitivity of 82–100 %, and specificity of 75–96 % and aids in the diagnosis of osteomyelitis [6].
Eikenella corrodens is a gram negative facultative anaerobic bacillus and is a part of the normal flora of the upper respiratory tract [7]. The pathogen can adhere to surfaces and create defenses against host immune response, allowing the organism to infect boney structures [8]. Streptococcus anginosus is a gram-positive facultative anaerobe that is also part of the normal human flora of the upper respiratory tract [9,10]. The organism has been implicated in cases of abscess formation, osteomyelitis to the skull base and cranium, and to muscular structures surrounding nearby anatomical structures [9,10].
Eikenella corrodens and Streptococcus anginosus have also been implicated in co-infections, especially abscesses [11]. Theories of this include coaggregation reactions of surface receptors of the organisms and protection from host defenses by biofilm production through communication and creation of autoinducer 2 proteins. However, co-infection causing skull-based osteomyelitis and contiguous spread to the internal carotid artery has not been described in the literature before.
Case report
A 35-year-old male with a past medical history of meningitis at the age of 3 presented to the emergency department due to severe headaches for the past 5 days. He was not able to eat for several days due to pain and states fevers. The pain started around his jaw and also involved the head. The pain was worsened with leaning forward. Physical exam was negative for cardiac murmurs or neck stiffness. Lung exams were clear bilaterally. Other than headache, neurologic exam was unremarkable. He had a white blood cell count of 17.2 k/microliter (reference range 3.8–10.5 k/microliter). Lumbar puncture was unremarkable and showed 0 red blood cells, 0 white blood cells, segmented neutrophils of 1% (ref 0–6 %), monocyte/macrophage 1 (ref 15–45 %), glucose 54 mg/L (ref 50−70 mg/dL), protein 42 mg/dL (ref range 15−45 mg/dL), and no fungal elements, acid fast bacillus, or bacterial elements observed or grown on culture.
The patient was initially started on oral Augmentin due to concern for sinusitis and received 4 doses of that. Aerobic and anaerobic blood cultures were positive for Eikenella corrodens and Streptococcus anginosus on day 2. Both had sensitivities to ceftriaxone, and therapy with ceftriaxone 2 g every 24 h was initiated.
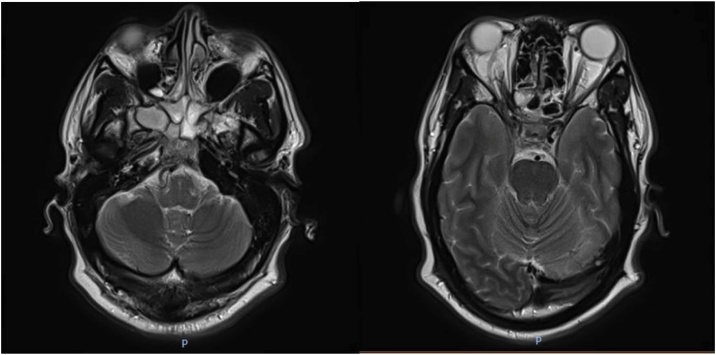
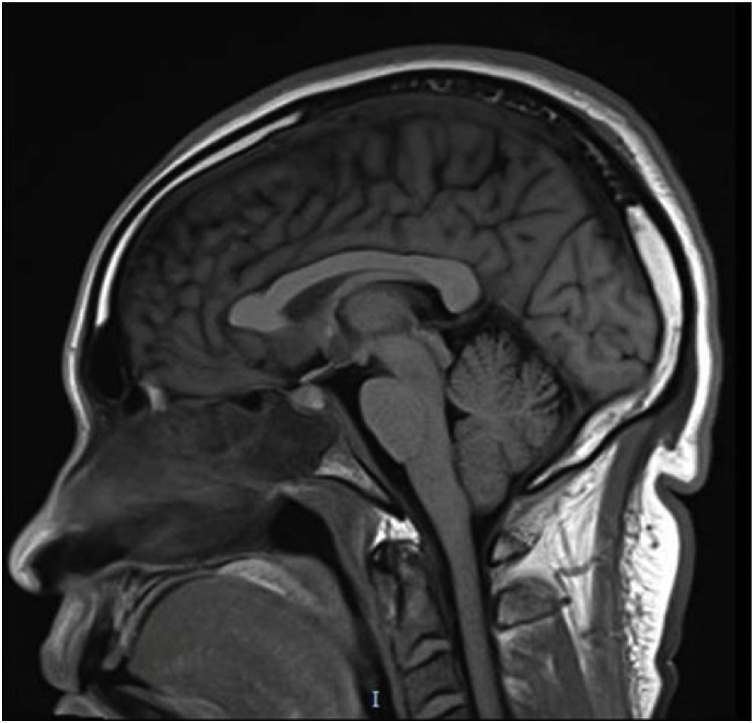
MR brain with contrast revealed abnormal enhancement of clivus and right petrous apex on day 2, consistent with osteomyelitis (Figs. 1 and 2, Fig. 3 ). There was spread of infection to right cavernous sinus, Meckel’s cave, right longus colli muscle, and cervical 2 spine as shown on Figs. 1 and 2, Fig. 3. There was also contiguous spread causing occlusion of internal carotid artery due to co-infection.
Figs. 1 and 2.
Magnetic resonance brain with and without intravenous contrast axial T2 turbo spin echo showing osteomyelitis of clivus extending to cavernous sinus and the internal carotid artery.
Fig. 3.
Magnetic resonance brain with and without intravenous contrast sagittal T1.
Ear, nose, and throat physicians were consulted. The patient had bilateral endoscopic sinus scoping with sphenoidectomy. Right sphenoid sinus was very purulent with exposed bone and was washed. Studies show this improves patient mortality and allows more complete resolution of the infection based on prior interventions [2,12]. Neurosurgery was consulted due to extension of the plaque to the right internal carotid artery. The decision was made to not treat the right internal carotid artery occlusion with antiplatelet medications or endovascular stenting, because there was a high likelihood of infection causing the plaque based on culture data and MRI imaging.
The patient was discharged with peripherally inserted central catheter and received 6 weeks of ceftriaxone and signs and symptoms resolved. He had resolution of his osteomyelitis, contiguous structural infections, and of his right internal carotid artery occlusion post antibiotics on MRI of his head three months later.
Discussion
Skull based osteomyelitis is rare in an immunocompetent host. A review by Johnson et al. reviewed 42 cases of skull-based osteomyelitis. One fourth had paranasal signs and symptoms prior to onset. 19 % of the infections were from Staphylococcus aureus, and 21 % from Pseudomonas aeruginosa [2]. Our case is unique in showing being the first case showing both Eikenella corrodens and Streptococcus anginosus causing skull-based osteomyelitis and is also unique in showing internal carotid artery plaque.
An extensive literature review by Khan et al. showed cases of skull-based osteomyelitis with involvement of the internal carotid artery with resolution of infection after appropriate antibiotic administration based on sensitivity results [2], and our study goes along with this treatment approach.
The review by Johnson et al. also shows that most common signs with skull based osteomyelitis involves headaches and cranial nerve involvement [1]. The most common cranial nerves includes cranial nerve VI, IX, and X [1,2]. Because of the mortality rate of 10 %, prompt evaluation by clinicians is essential [1,2].
Consent
Written and verbal consent was obtained by the patient for this report.
Author contribution
Kishan Patel: Helped write the outline and first draft of this manuscript
Connie Park: Helped with editing the paper and finding appropriate references
Zain Memon: Worked with final edits and obtaining imaging
Nazish Ilyas: Worked on final draft and literature review of relevant material.
Funding
No sources of funding to disclose.
Consent
Written and verbal consent was obtained for this case report and is available upon request from the authors.
Declaration of Competing Interests
No conflicts of interest to disclose for any of the authors.
Acknowledgement
The authors would like to thank the Department of Medicine at Lenox Hill Hospital.
Contributor Information
Kishan Patel, Email: KPatel36@northwell.edu.
Connie Park, Email: cpark9@northwell.edu.
Zain Memon, Email: zmemon@northwell.edu.
Nazish Ilyas, Email: nilyas@northwell.edu.
References
- 1.Johnson A.K., Batra P.S. Central skull base osteomyelitis: an emerging clinical entity. Laryngoscope. 2014;124:1083–1087. doi: 10.1002/lary.24440. [DOI] [PubMed] [Google Scholar]
- 2.Khan M., Quadri S. A comprehensive review of skull base osteomyelitis: diagnostic and therapeutic challenges among various presentations. Asian J Neurosurg. 2018;13(Oct-Dec (4)):959–970. doi: 10.4103/ajns.AJNS_90_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vlastos I.M., Helmis G., Athanasopoulos I., Houlakis M. Acute mastoiditis complicated with bezold abscess, sigmoid sinus thrombosis and occipital osteomyelitis in a child. Eur Rev Med Pharmacol Sci. 2010;14:635–638. [PubMed] [Google Scholar] [PubMed] [Google Scholar]
- 4.Clark M.P., Pretorius P.M., Byren I., Milford C.A. Central or atypical skull base osteomyelitis: diagnosis and treatment. Skull Base. 2009;19:247–254. doi: 10.1055/s-0028-1115325. [PMC free article] [PubMed] [Google Scholar] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zigler J.E., Bohlman H.H., Robinson R.A., Riley L.H., Dodge L.D. Pyogenic osteomyelitis of the occiput, the atlas, and the axis. A report of five cases. J Bone Joint Surg Am. 1987;69:1069–1073. [PubMed] [Google Scholar]
- 6.Fritz J., McDonald J. Osteomyelitis: approach to diagnosis and treatment. Phys Sportsmed. 2008;36 doi: 10.3810/psm.2008.12.11. nihpa116823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arana E., Vallcanera A., Santamaria J.A. Eikenella corrodens skull infection: a case report with review of the literature. Surg Neurol. 1997;47:389–391. doi: 10.1016/s0090-3019(96)00192-9. [DOI] [PubMed] [Google Scholar]
- 8.Azakami H., Teramura I., Matsunaga T., Akimichi H., Noiri Y., Ebisu S. Characterization of autoinducer 2 signal in Eikenella corrodens and its role in biofilm formation. J Biosci Bioeng. 2006;102(2):110–117. doi: 10.1263/jbb.102.110. [DOI] [PubMed] [Google Scholar]
- 9.Ruoff K.L. Streptococcus anginosus (“Streptococcus milleri”): the unrecognized pathogen. Clin Microbiol Rev. 1988;1(1):102–108. doi: 10.1128/cmr.1.1.102. January. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Han J., Kerschner J. Streptococcus milleri an organism for head and neck infections and abscess. Arch Otolaryngol Head Neck Surg. 2001;127(6):650–654. doi: 10.1001/archotol.127.6.650. [DOI] [PubMed] [Google Scholar]
- 11.Young K.A., Allaker R.P., Hardie J.M. Interactions between Eikenella corrodens and ‘Streptococcus milleri-group’ organisms: possible mechanisms of pathogenicity in mixed infections. Antonie van Leeuwenhoek. 1996;69:371. doi: 10.1007/BF00399626. [DOI] [PubMed] [Google Scholar]
- 12.Clark M., Pretorius P. Central or atypical skull base osteomyelitis: diagnosis and treatment. Skull Base. 2009;19(July (4)):247–254. doi: 10.1055/s-0028-1115325. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]