Abstract
This case was about a 71‐year‐old man presented to our clinic for an anterior mediastinal mass found on routine chest computed tomography (CT). CT scan showed a lobulating contoured mass in the anterior mediastinum. A preliminary diagnosis was thymoma. The patient underwent subxiphoid uniportal video‐assisted thoracoscopic surgery for the extended thymectomy and complete excision of the tumour. The pathological examination showed a micronodular thymoma with lymphoid stroma (MTWLS). In conclusion, this report described an extremely rare tumour, MTWLS, and MTWLS might be considered in the differential diagnosis of mediastinal tumour, especially thymoma.
Keywords: Lymphoid tissue, micronodular thymoma with lymphoid stroma, thymoma
Here, we describe the surgical treatment of extremely rare thymoma—micronodular thymoma with lymphoid stroma (MTWLS).
Introduction
Micronodular thymoma with lymphoid stroma (MTWLS) is an extremely rare type of thymoma, which was first described in 1991 by Suster and Moran 1. A total of 75 cases have been identified in the English literature until now 2. MTWLS is characterized by proliferation of multiple small nodules divided by abundant lymphoid stroma with multiple lymphoid follicles and prominent germinal centres. MTWLS is classified as an unusual type in the World Health Organization (WHO) classification. To date, there is an insufficient understanding of the pathology of MTWLS because of its paucity. The present study presents a case of MTWLS, which was treated by surgical resection.
Case Report
A 71‐year‐old man presented to the Thoracic Surgery Department with a history of persistent anterior mediastinal mass. He denied history of significant disease. A computed tomography (CT) demonstrated a 3.8‐cm lobulating contoured mass in the anterior mediastinum. A preliminary diagnosis by radiologist was thymoma. No lymphadenopathy or other mass lesions were identified. The patient underwent subxiphoid uniportal video‐assisted thoracoscopic surgery (VATS) for the extended thymectomy. The lesion showed a well‐circumscribed solid mass, measuring 4.0 × 4.0 × 2.0 cm. Gross and microscopic features of the lesion were described as shown in Figures 1 and 2. The patient had an uneventful clinical course and discharged without complication. In a recent follow‐up nine months after discharge, he had no recurrence.
Figure 1.
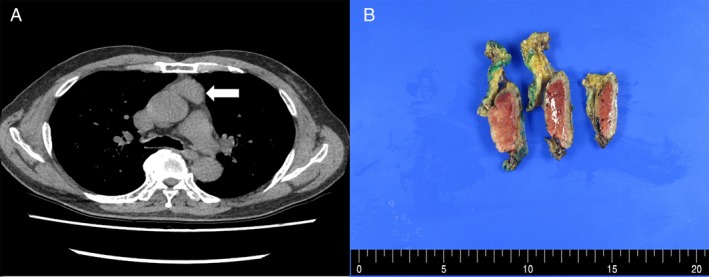
Computed tomography demonstrating approximately 3.8 cm sized lobulating contoured mass in the anterior mediastinum (white arrow) (A) and gross image of the mass, which is well circumscribed and reveals a homogeneous, solid cut surface (B).
Figure 2.
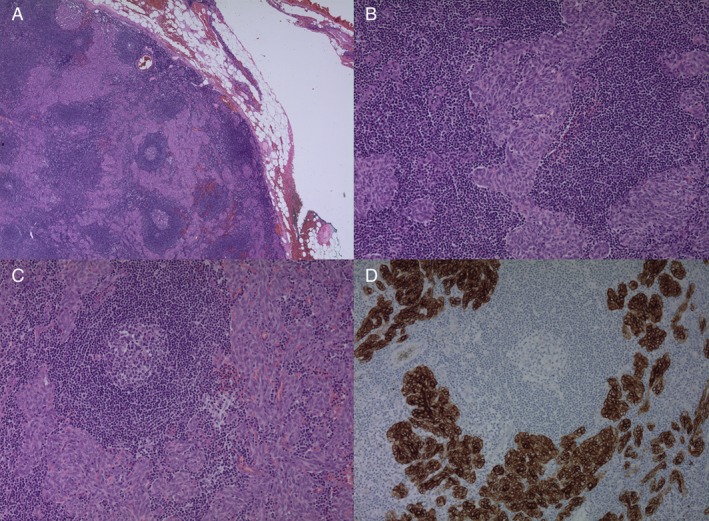
Low‐magnification view shows multiple small nodules of tumour cells separated by abundant lymphoid stroma (A). The tumour cells are bland‐looking, short spindled and oval, epithelial cells (B). The intervening lymphoid stroma contains lymphoid follicles with germinal centres (C). Immunohistochemistry for pancytokeratin is positive in tumour cells, confirming the diagnosis of thymoma (D).
Discussion
In the WHO classification, thymoma is classified according to epithelium and lymphocyte contents. Compared with the usual thymoma including types A, AB, B1, B2, and B3, which consist of immature T cells, MTWLS includes abundant lymphoid stroma consisting of mature B and T cells and does not contain epithelium contents in the lymphocytic‐rich areas. Immunohistochemical staining pattern varied in the literature. CD5 and CD117 immunostaining could be useful for the differential diagnosis. Noticeably, CD5 immunostaining is positive in thymic carcinoma but not in other tumours 3. Although there has been no known characteristic symptoms of MTWLS, myasthenia gravis and hypogammaglobulinaemia have been reported 4. Surgical resection would be the treatment of choice because there have been no reports of recurrence in the literature 5. However, further long‐term follow‐up studies would be required for the clear understanding of pathology. Our report serves as reminder that MTWLS might be considered in the treatment of thymoma, although it is a very rare type of thymoma, which could be best treated by surgical resection.
Disclosure Statement
Appropriate written informed consent was obtained for publication of this case report and accompanying images.
Kang, MK , Kang, DK , Hwang, Y‐H , Kim, JY . (2020) Surgical treatment of micronodular thymoma with lymphoid stroma. Respirology Case Reports, 8(3), e00548 10.1002/rcr2.548
Associate Editor: Michael Hsin
References
- 1. Suster S, and Rosai J. 1991. Multilocular thymic cyst: an acquired reactive process. Study of 18 cases. Am. J. Surg. Pathol. 15:388–398. [PubMed] [Google Scholar]
- 2. Qu L, Xiong Y, Yao Q, et al. 2017. Micronodular thymoma with lymphoid stroma: two cases, one in a multilocular thymic cyst, and literature review. Thorac. Cancer. 8(6):734–740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Travis WD, Brambilla E, Burke AP, et al. 2015. Introduction to the 2015 World Health Organization classification of tumors of the lung, pleura, thymus, and heart. J. Thorac. Oncol. 10:1240–1242. [DOI] [PubMed] [Google Scholar]
- 4. Tateyama H, Saito Y, Fujii Y, et al. 2001. The spectrum of micronodular thymic epithelial tumours with lymphoid B‐cell hyperplasia. Histopathology 38:519–527. [DOI] [PubMed] [Google Scholar]
- 5. Kaminuma Y, Tanahashi M, Yukiue H, et al. 2019. Micronodular thymoma with lymphoid stroma diagnosed 10 years after the first operation: a case report. J. Med. Case Rep. 13(1):69. [DOI] [PMC free article] [PubMed] [Google Scholar]


