Abstract
Introduction:
The co-occurrence of posttraumatic stress disorder (PTSD) and alcohol misuse presents a pervasive and clinically relevant concern among US military veterans.
Objective:
The current investigation sought to examine the role of positive emotion dysfunction in the relation between PTSD symptomatology and alcohol misuse. To do so, we examined the separate and sequential roles of positive emotional intensity and positive emotional avoidance in the relation between PTSD symptoms and alcohol misuse among US military veterans.
Method:
Cross-sectional data were collected from 468 US military veterans (M age= 37.74, 70.5% male, 69.0% White) who responded to an online survey.
Results:
Findings suggest that positive emotional avoidance, separately, and positive emotional intensity and positive emotional avoidance, sequentially, mediated the relation between PTSD symptoms and alcohol misuse.
Conclusions:
Findings advance theory on the role of positive emotions and related processes in the co-occurrence of PTSD and alcohol misuse, and highlight important avenues for future research and treatment focused on the PTSD-alcohol misuse co-occurrence.
Keywords: PTSD, posttraumatic stress disorder, alcohol use disorder, emotion dysregulation, emotional avoidance, positive emotions
The co-occurrence of posttraumatic stress disorder (PTSD) and alcohol use disorder (AUD) is highly prevalent and clinically relevant among United States (US) military veterans. Lifetime prevalence rates of AUD among US military veterans with PTSD range from 55 to 68% (Seal et al., 2011; Smith, Goldstein, & Grant, 2016; Wisco et al., 2014). Compared to individuals with either PTSD or AUD alone, those with co-occurring PTSD-AUD have elevated PTSD and AUD symptoms (Driessen et al., 2008; Saladin, Brady, Dansky, & Kilpatrick, 1995), greater functional impairment (Driessen et al., 2008; Riggs, Rukstalis, Volpicelli, Kalmanson, & Foa, 2003), and more comorbid mental and physical health problems (Driessen et al., 2008; Mills, Teesson, Ross, & Peters, 2006; Ouimette, Wolfe, & Chrestman, 1996; Saladin et al., 1995). Moreover, individuals with co-occurring PTSD-AUD exhibit worse alcohol use outcomes when compared with either PTSD or AUD alone, including increased hospital admissions for alcohol-related problems (Driessen et al., 2008), poorer treatment outcome, and higher relapse rates (Mills, Lynskey, Teesson, Ross, & Darke, 2005). Given robust evidence linking PTSD and AUD among military veterans, research is needed to elucidate underlying factors that may be targeted in preventative interventions to reduce PTSD-AUD co-occurrence in this population. To this extent, the current study examined factors that may explain the association between PTSD and alcohol misuse among a community sample of military veterans.
Emerging work supports the role of positive emotion dysfunction in PTSD and alcohol misuse. Specifically, research has shown that the tendency to be non-accepting of positive emotions and to experience behavioral dyscontrol (e.g., impulsive responding) in their presence is elevated among individuals with PTSD (Weiss, Contractor, Forkus, Goncharenko, & Raudales, in press; Weiss, Dixon-Gordon, Peasant, & Sullivan, 2018; Weiss, Nelson, Contractor, & Sullivan, in press; Weiss, Tull, Sullivan, Dixon-Gordon, & Gratz, 2015) and alcohol misuse (Schick, Weiss, Contractor, Dixon-Gordon, & Spillane, in press; Weiss, Forkus, Contractor, & Schick, 2018; Weiss, Risi, Bold, Sullivan, & Dixon-Gordon, in press), separately. Moreover, one aspect of positive emotion dysfunction – positive emotion dysregulation – has been shown to explain the association between PTSD and alcohol misuse (Weiss, Schick, Contractor, & Dixon-Gordon, 2019). Yet, to our knowledge, this is the only study to test the underlying role of positive emotion dysfunction in the PTSD-alcohol misuse association. Further, despite initial evidence for the contribution of positive emotion dysfunction to PTSD, alcohol misuse, and their association, a dearth of literature has examined how positive emotion dysfunction stemming from PTSD relates to alcohol misuse. Research is needed to identify specific mechanisms through which individuals with PTSD may respond to positive emotions that increases their risk for alcohol misuse.
One potential explanation for the PTSD-alcohol misuse link is that individuals with PTSD use alcohol to escape or avoid positive emotional experiences that are perceived as distressing. Research indicates that some individuals with PTSD take an evaluative stance toward positive emotions (Weiss, Contractor, et al., in press; Weiss, Dixon-Gordon, et al., 2018; Weiss, Nelson, et al., in press), judging them to be aversive because they elicit physiological arousal (Litz, Orsillo, Kaloupek, & Weathers, 2000) associated with trauma-related symptoms and distress through stimulus generalization (Roemer, Litz, Orsillo, & Wagner, 2001). Specifically, the fear elicited from physiological arousal originally paired with trauma cues may expand to arousing positive emotions over time (Weiss, Dixon-Gordon, et al., 2018). Alternatively, some individuals with PTSD may experience positive emotions as aversive due to negative affect interference, or negative emotional reactions to stimuli that typically elicit positive emotions (Frewen, Dozois, & Lanius, 2012; Frewen, Dozois, Neufeld, & Lanius, 2012). These individuals may exhibit competing negative cognitions in the context of positive emotions (e.g., “I do not deserve to be happy”) that drive feelings of fear, shame, or disgust. Individuals with PTSD who experience positive emotions as aversive may be more likely to control, suppress, or otherwise avoid these emotion states (Roemer et al., 2001). Research of negative emotions suggests that individuals may use alcohol to achieve these effects, consistent with negative reinforcement (Baker, Piper, McCarthy, Majeskie, & Fiore, 2004). Thus, while not yet studied, it is possible that individuals with PTSD may also be motivated to use alcohol to down-regulate positive emotions.
Extending extant literature, the current study sought to explore the roles of positive emotional intensity and positive emotional avoidance in the relation between PTSD symptoms and alcohol misuse in a community sample of US military veterans, which represents a population with highly prevalent rates of PTSD and alcohol misuse, separately and co-occurring (Seal et al., 2011; Smith et al., 2016; Wisco et al., 2014). Further, no studies have examined positive emotion dysfunction in the PTSD-alcohol misuse relation among US military veterans, despite evidence suggesting that this population may be at particular risk for emotion dysfunction. Specifically, the US military socializes individuals to value stoicism and emotional control (Lorber & Garcia, 2010; McAllister, Callaghan, & Fellin, 2019). As a result, US military veterans may be more likely to rely on strategies that facilitate avoidance of emotional experiences that are inconsistent with US military ideals (e.g., intense emotions). Further, PTSD among US military veterans is characterized by heightened arousal (Kimble, Fleming, & Bennion, 2013; Marshall, Schell, Glynn, & Shetty, 2006); thus, veterans may be more likely to experience arousal as distressing, even that stemming from positive emotions (Litz et al., 2000).
To this end, we examined the separate and sequential roles of positive emotional intensity and positive emotional avoidance in the relation between PTSD symptoms and alcohol misuse among US military veterans. To our knowledge, no investigations have examined the role of positive emotional intensity or positive emotional avoidance (separately or sequentially) in the relation between PTSD symptoms and alcohol misuse. The ordering of the variables in the sequential model (i.e., PTSD symptoms to positive emotional intensity to positive emotional avoidance to alcohol misuse) was determined based on the explanation that individuals with more severe PTSD symptoms may perceive intense positive emotions as aversive, increasing levels of positive emotional avoidance, and subsequently alcohol misuse. We hypothesized direct and indirect effects between PTSD symptoms and alcohol misuse through positive emotional intensity and positive emotional avoidance would be significant. Regarding the sequential association, it was expected that PTSD symptoms would be positively related to positive emotional intensity, which was expected to be positively related to positive emotional avoidance, which was expected to be positively related to alcohol misuse.
2. Methods
2.1. Procedure/Participants
US military veterans were recruited from Amazon’s Mechanical Turk (MTurk), an internet-based crowdsourcing platform. MTurk generates reliable data (Buhrmester, Kwang, & Gosling, 2011; Shapiro, Chandler, & Mueller, 2013), and represents the general population in terms of demographics (Mishra & Carleton, 2017) and prevalence of mental health problems (Shapiro et al., 2013), including PTSD (van Stolk-Cooke et al., 2018). To improve data quality, we incorporated validity checks assessing attentive responding and comprehension (4 items; e.g., “I have never brushed my teeth;” Meade & Craig, 2012; Oppenheimer, Meyvis, & Davidenko, 2009; Thomas & Clifford, 2017) and US military-specific knowledge (2 items; e.g., “What is the acronym for the locations where final physicals are taken prior to shipping off for basic training;” Lynn & Morgan, 2016). Participants who failed to correctly respond to any one of the six validity checks were excluded (see Exclusions and Missing Data).
Participants were screened for four inclusionary criteria: 1) ≥18 years old, 2) living in North America (to limit the influence of geographic region on study hypotheses), 3) working knowledge of the English language, and 4) a veteran of the US military (i.e., any former US military member). Eligible participants provided informed consent, completed the survey on Qualtrics data collection platform, and were compensated $2.50. Procedures were approved by the Institutional Review Board at [redacted].
2.2. Exclusions and Missing Data
Of the obtained 2,644 responses, we excluded 997 participants for not meeting inclusionary criteria (remainder n = 1,647), 899 participants who failed any attention/comprehension validity questions (remainder n = 748), 134 participants who failed any US military-specific validity questions (remainder n = 614), and 79 participants who attempted the questionnaire multiple times (remainder n = 535). An additional 67 participants were excluded for not endorsing a traumatic event on the Life Events Checklist for DSM-5 (LEC-5; Weathers, Blake, et al., 2013). Thus, the final sample included 468 participants (see Figure 1 for a schematic flow chart and Table 1 for demographic information).
Figure 1.
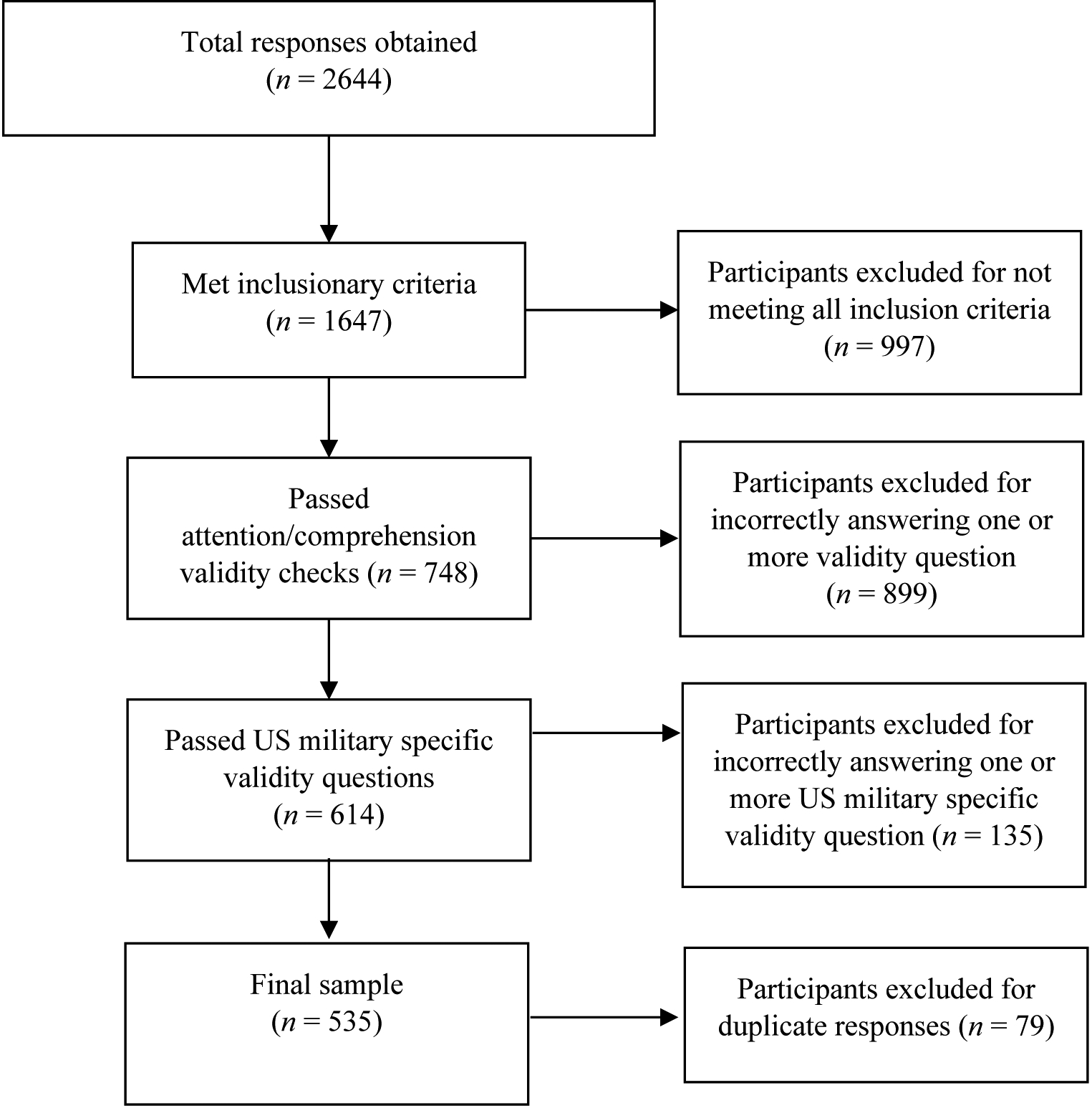
Flow Diagram for Sample Selection
Table 1.
Descriptive Characteristics of the Sample
| Full Sample (n = 468) | |
|---|---|
| Variables | Mean (SD) |
| Age | 37.74 (11.41) |
| PTSD Symptoms | 29.76 (23.22) |
| Positive Emotional Intensity | 29.89 (9.27) |
| Positive Emotional Avoidance | 12.09 (5.97) |
| Alcohol Misuse | 9.74 (9.85) |
| n (%) | |
| Gender | |
| Female | 135 (29.1%) |
| Male | 327 (70.5%) |
| Female to Male Transgender | 2 (.4%) |
| Race | |
| White | 323 (69.0%) |
| Black | 109 (23.3%) |
| Asian | 28 (6.0%) |
| American Indian/Alaska Native | 15 (3.2%) |
| Native Hawaiian/Other Pacific Islander | 6 (1.3%) |
| Not Listed | 4 (0.9%) |
| Ethnicity | |
| Hispanic or Latino/a | 115 (25.2%) |
| Not Hispanic or Latino/a | 341 (74.8%) |
| Employment Status | |
| Employed Full-time | 394 (85.7%) |
| Employed Part-time | 41 (8.9%) |
| Not in Labor Force (student, homemaker) | 14 (3.0%) |
| Unemployed | 11 (2.4%) |
| Family Annual Income | |
| < $15,000 | 234 (50.0%) |
| $15,000 – $24,999 | 16 (3.4%) |
| $25,000 – $34,999 | 23 (4.9%) |
| $35,000 – $49,999 | 51 (10.9%) |
| $50,000 – $64,999 | 64 (13.7%) |
| $65,000 – $79,999 | 30 (6.4%) |
| $80,000 or higher | 50 (10.7%) |
| Branch of Service | |
| Army | 301 (64.4%) |
| Navy | 44 (9.4%) |
| Air Force | 88 (18.8%) |
| Marines | 29 (6.2%) |
| Coast Guard | 6 (1.3%) |
| Number of Deployments | |
| None | 94 (20.8 %) |
| One | 121 (26.8%) |
| Two | 106 (23.5%) |
| Three or more | 130 (28.9%) |
| Involved in Combat Operations | |
| Yes | 235 (70.1%) |
| No | 100 (29.9%) |
| Probable Diagnoses | |
| Probable PTSD | 224 (47.9%) |
| Probable Alcohol Use Disorder | 215 (45.9%) |
Note. All reported percentages are valid percentages to account for missing data. PTSD = posttraumatic stress disorder. Respondents could endorse more than one racial category.
2.3. Measures
2.3.1. Life Events Checklist for DSM-5 (LEC-5; Weathers, Blake, et al., 2013).
The LEC-5 is a 17-item self-report measure assessing lifetime exposure to DSM-5 Criterion A traumatic events (American Psychiatric Association, 2013) using a 6-point scale: happened to me, witnessed it, learned about it, part of my job, not sure, and does not apply. The LEC has good psychometric properties (Gray, Litz, Hsu, & Lombardo, 2004).
2.3.2. PTSD Checklist for DSM-5 (PCL-5; Weathers, Litz, et al., 2013).
The PCL-5 is a 20-item self-report measure assessing DSM-5 criteria for PTSD in response to the most distressing traumatic event endorsed on the LEC-5. Participants indicated how bothersome symptoms have been over the past month using a scale ranging from 0 (not at all) to 4 (extremely). Total scores ranged from 0–80. The PCL-5 has good psychometric properties (Blevins, Weathers, Davis, Witte, & Domino, 2015; Bovin et al., 2016; Wortmann et al., 2016). Cronbach’s α was .98 in the current sample.
2.3.3. The Short Affect Intensity Scale-Positive (SAIS-P; Geuens & De Pelsmacker, 2002).
The SAIS-P is an 8-item self-report measure assessing positive emotional intensity (e.g., “My happy moods are so strong that I feel like I’m in heaven”). Responses are given on a 6-point Likert scale ranging from 1 (strongly disagree) to 6 (strongly agree), with total scores ranging from 8–48. This scale has good psychometric properties (Geuens & De Pelsmacker, 2002). Cronbach’s α was .93 in the current sample.
2.3.4. Emotional Avoidance Questionnaire-Positive (EAQ-Positive; Taylor, Laposa, & Alden, 2004).
The EAQ-Positive is a 5-item self-report measure assessing avoidance of positive emotions (e.g., “If I start feeling strong positive emotions, I prefer to leave the situation”). Responses are given on a 5-point Likert-type scale ranging from 1 (not true of me) to 5 (very true of me), with total scores ranging from 5–25. The EAQ-Positive has good psychometric properties. Cronbach’s α was .91 in the current sample.
2.3.5. Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993).
The AUDIT is a 10-item self-report measure assessing alcohol use and problems. Items are rated on a scale between 0 and 4 with total scores ranging from 0–40. The AUDIT has good psychometric properties (Searle et al., 2015). Cronbach’s α was .92 in the current sample.
2.4. Data Analysis
Preliminary analyses were first conducted to examine associations between the dependent (i.e., alcohol misuse) and independent (i.e., PTSD symptom severity) variables and potential demographic (i.e., age) and deployment (i.e., deployment number, combat exposure) covariates. These specific demographic and deployment characteristics were examined given previously established associations with the dependent variable (Jacobson et al., 2008). Per recommendations set forth by Miller and Chapman, (2001), demographic and deployment characteristics that were significantly related to the dependent variable were included as covariates if they were not significantly related to the independent variable (inclusion of covariates significantly associated with the independent variable in nonrandomized designs may remove a portion of the variance attributed to the independent variable and thus negatively affect its construct validity).
Descriptive information and intercorrelations were examined for primary variables. Serial mediation was then used to examine the multiple mediating pathways between PTSD symptoms and alcohol misuse through positive emotional intensity and positive emotional avoidance. Serial mediation allows multiple mediators to be examined while simultaneously controlling for collinearity and mediational effects. This model was examined using the PROCESS SPSS macro (Model 6; Hayes, 2013) using bootstrapping methodology, which is a nonparametric resampling procedure that is considered the most powerful and effective method for estimating the significance of indirect effects, does not assume normal distribution, and is robust against Type 1 errors (Preacher & Hayes, 2004). Bootstrapping was done with 5,000 random samples generated from the observed covariance matrix to estimate 95% confidence intervals (CIs) and significance values. Mediation is considered to be significant if the upper and lower bounds of the 95% confidence interval does not contain zero (Preacher & Hayes, 2004).
3. Results
Approximately half of the sample met diagnostic criteria for probable PTSD (47.9%) and alcohol use disorder (45.9%). Intercorrelations among primary variables are presented in Table 2. All variables were significantly positively associated with one another.
Table 2.
Intercorrelations among Primary Variables
| 1 | 2 | 3 | 4 | |
|---|---|---|---|---|
| 1. PTSD Symptoms | -- | -- | -- | -- |
| 2. Positive Emotional Intensity | .18** | -- | -- | -- |
| 3. Positive Emotional Avoidance | .57** | .25** | -- | -- |
| 4. Alcohol Misuse | .50** | .13* | .37** | -- |
Note. PTSD = posttraumatic stress disorder.
p < .01.
p < .001.
Next, demographic and deployment characteristics were examined as potential covariates. Age (r = .05, p = .28) and deployment number (r = −.03, p = .51) were not significantly associated with the dependent variable. Combat exposure was significantly associated with both the independent (r = .26, p < .001) and dependent (r = .21, p < .001) variables, and thus was not included as a covariate (see Chapman & Miller, 2001).
The serial mediation model (see Figure 2 and Table 3) revealed a significant positive association between PTSD symptoms and alcohol misuse (c path; B = 0.21, SE = .02, t = 12.20, p < .001, 95% CI [0.18, 0.24]). PTSD symptoms were significantly positively associated with both positive emotional intensity (a1 path; B = 0.07, SE = .02, t = 3.82, p < .001, 95% CI [0.03, 0.11]) and positive emotional avoidance (a2 path; B = 0.14, SE = .01, t = 14.20, p < .001, 95% CI [0.12, 0.16]). Further, positive emotional intensity was significantly positively associated with positive emotional avoidance (a3 path; B = 0.10, SE = .02, t = 4.07, p < .001, 95% CI [0.05, 0.15]), but not alcohol misuse (b1 path; B = 0.05, SE = .04, t = 1.04, p = .30, 95% CI [−0.04, 0.13]). Lastly, positive emotional avoidance was significantly associated with alcohol misuse (b2 path; B = 0.20, SE = .08, t = 2.43, p = .02, 95% CI [.04, 0.36]).
Figure 2.
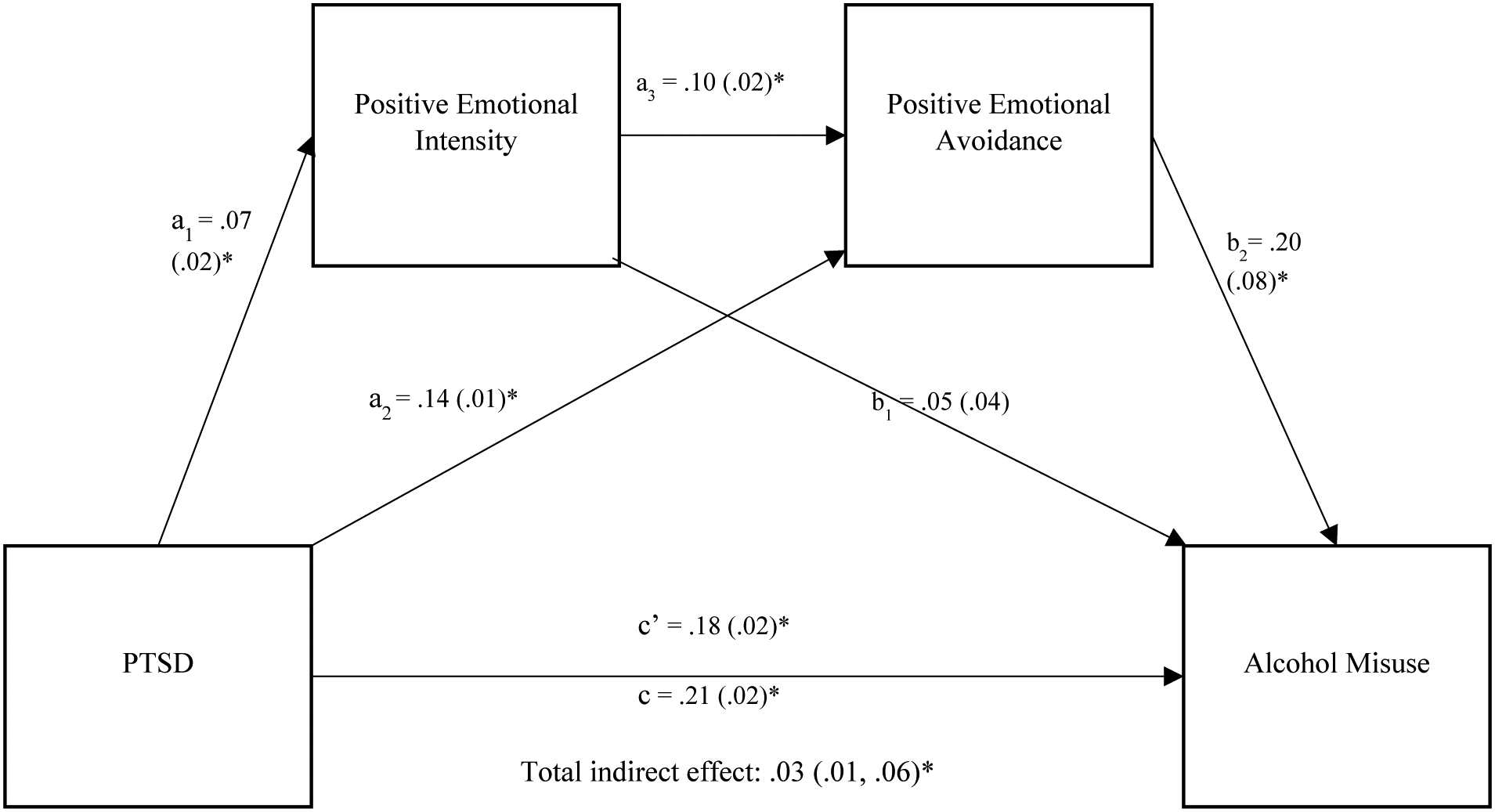
Direct Paths among Study Variables
Note. In this model, the a path represents the association between the predictor (PTSD symptoms) and mediator (positive emotional intensity and positive emotional avoidance) variables and the b path represents the association between the mediators and outcome (alcohol misuse) variables. The total effect (c path) refers to the association between PTSD symptoms and alcohol misuse without controlling for mediators. The direct effect (c’ path) is the relation between PTSD symptoms and alcohol misuse after controlling for the effect of the mediators. The specific indirect effects reflect the influence of a specific mediator on the relation between PTSD symptoms and alcohol misuse, and the total indirect effect is the sum of the specific indirect effects. This model estimated two simple specific indirect effects (PTSD symptoms → positive emotional intensity → alcohol misuse and PTSD symptoms → positive emotional avoidance → alcohol misuse) and one serial indirect effect (PTSD symptoms → positive emotional intensity → positive emotional avoidance → alcohol misuse). *represent significant results at p < .05.
Table 3.
Model Estimates for Indirect Effects, Standard Errors, and Confidence Intervals
| PTSD Symptoms on Alcohol Misuse via: | B | SE | 95%CI |
|---|---|---|---|
| Positive Emotional Intensity | .003 | .003 | −.003, .01 |
| Positive Emotional Avoidance | .03 | .01 | .005, .05* |
| Positive Emotional Intensity → Positive Emotional Avoidance | .001 | .001 | .0001, .003* |
Note.
represents significant results at the level of p < .05.
The specific indirect effects through just positive emotional intensity (a1b1; B = 0.003, SE = .003, p > .05, 95% CI [−0.003, 0.01]) were non-significant, but the specific indirect effects through positive emotional avoidance (a2b2; B = 0.03, SE = .01, p < .05, 95% CI [0.004, 0.05]) were significant. The serial indirect effects of PTSD symptoms on alcohol misuse through both positive emotional intensity and positive emotional avoidance were significant (a1a3b2; B = 0.001, SE = .001, 95% CI [0.0002, 0.003]). The total indirect effect (i.e., the sum of the specific indirect effects) was significant (B = 0.03, SE = .01, 95% CI [0.007, 0.06]). Further, the relation between PTSD symptoms and alcohol misuse remained significant after controlling for the indirect relations in the model (c’ path; B = 0.18, SE = .02, t = 8.49, p < .001, 95% CI [0.14, 0.22]). Therefore, positive emotional avoidance, separately, and positive emotional intensity and positive emotional avoidance, sequentially, mediated the relation between PTSD symptoms and alcohol misuse.1
4. Discussion
The present study sought to begin to clarify the role of positive emotions in the association between PTSD symptomatology and alcohol misuse. Using cross-sectional data, we tested the separate and sequential roles of positive emotional intensity and positive emotional avoidance in the relation between PTSD symptoms and alcohol misuse. Partially consistent with study hypotheses, positive emotional avoidance (but not positive emotional intensity) partially accounted for the association between PTSD symptoms and alcohol misuse. In addition, evidence for the sequential role of positive emotional intensity and positive emotional avoidance in the relation between PTSD symptoms and alcohol misuse was obtained. Specifically, greater severity of PTSD symptoms was related to greater positive emotional intensity, which was related to greater positive emotional avoidance, which was related to greater alcohol misuse. These findings advance theory on the role of positive emotion dysfunction in the co-occurrence of PTSD and alcohol misuse and highlight important avenues for future research focused on this co-occurrence. If replicated using longitudinal data, our results may inform treatment efforts for co-occurring PTSD-alcohol misuse.
Preliminary (i.e., cross-sectional) evidence of sequential mediation advances research in this area by beginning to clarify the mechanism through which positive emotional intensity stemming from PTSD symptoms is related to alcohol misuse. Specifically, our results point to the potentially key role of positive emotional avoidance in these associations, suggesting that individuals with greater severity of PTSD symptoms may be more likely to use avoidance strategies in the context of intense positive emotional experience, which in turn may increase their risk for alcohol misuse. This finding is consistent with theoretical explanations, such that individuals with PTSD may avoid positive emotional experiences (Roemer et al., 2001) because they elicit physiological arousal (Litz et al., 2000) and/or negative emotional reactions (Frewen, Dozois, & Lanius, 2012; Frewen, Dozois, Neufeld, et al., 2012) that are distressing (Weiss, Dixon-Gordon, et al., 2018). In line with research on the functional roles of alcohol use (Baker et al., 2004), individuals with PTSD may sometimes use alcohol to alleviate or distract from positive emotions that are perceived as aversive.
It warrants mention that evidence for the separate role of positive emotional intensity in the association between PTSD symptoms and alcohol misuse in our cross-sectional data was not found, suggesting that intense positive emotions may not, by themselves, be problematic among individuals with PTSD. Indeed, work on positive emotions supports their protective nature in reducing risk for deleterious health outcomes following traumatic exposure. Folkman (1997, 2008) identified positive emotions as a crucial component of the coping process among individuals exposed to traumatic stress. Positive emotions can counteract negative emotions during traumatic stressors (Fredrickson, Tugade, Waugh, & Larkin, 2003; Tugade & Fredrickson, 2004) and restore physiological, psychological, and social resources following traumatic stress (Fredrickson, 1998, 2001). While positive emotions may be generally adaptive, there is growing evidence to suggest that they may, at times, confer negative consequences, including risk for alcohol misuse (Coskunpinar, Dir, & Cyders, 2013; Cyders et al., 2010; Weiss, Forkus, et al., 2018; Weiss et al., 2019; Weiss, Tull, Dixon-Gordon, & Gratz, 2018). Our findings suggest that positive emotions may be more likely to be linked to alcohol misuse following traumatic stress if individuals utilize strategies to avoid them, perhaps indicative of their aversive nature (Weiss, Gratz, & Lavender, 2015).
While preliminary in nature, the findings of the current study could have important clinical implications if replicated using longitudinal data. First, they may suggest the potential utility of assessing for positive emotional avoidance among trauma-exposed populations. Trauma-exposed individuals who are high in positive emotional avoidance may be at heightened risk for alcohol misuse. For these individuals, primary (for those without a current alcohol misuse) or secondary/tertiary (for those with a current alcohol misuse) preventions may be recommended. Second, our results could highlight positive emotional avoidance as a potentially important factor in the treatment of co-occurring PTSD-alcohol misuse. Counter to general practice, the goal of PTSD-alcohol misuse treatment may not be to simply increase positive emotions. Instead, clinicians may first need to address the presence of aversive physiological, cognitive, and affective reactions to positive emotions. For instance, given evidence here for the potential role of positive emotional avoidance, treatment may include exposure to positive emotions without efforts to control, suppress, or otherwise avoid these emotion states, perhaps drawing from acceptance-based therapies (e.g., acceptance and commitment therapy for PTSD; Walser & Westrup, 2007). If replicated in longitudinal studies, future research would benefit from assessing the utility of addressing positive emotional avoidance in treatments targeting the co-occurrence of PTSD and alcohol misuse.
These results also have important implications for future research. Our findings extend conceptual models of the relations among trauma, positive emotions, and alcohol use. In particular, results suggest that using avoidance to manage intense positive emotions may be linked to alcohol misuse among trauma-exposed individuals. Future research is needed to test and expand this conceptual model, including replication among populations for which the co-occurrence of PTSD and alcohol misuse is elevated (e.g., clinical samples). Further, examination of the relations among PTSD symptoms, positive emotional intensity, positive emotional avoidance, and alcohol misuse using study designs (e.g., longitudinal) and methods (e.g., ecological momentary assessment) that speak to temporal and causal associations are warranted. Investigations should also examine other potential mechanisms that may explain the role of positive emotional intensity in the PTSD-alcohol misuse relation. One relevant factor may be the ability to inhibit prepotent responses, or control or suppress an automatic response, shown to be impaired in emotional contexts (Billieux, Gay, Rochat, & Van der Linden, 2010) and associated with alcohol misuse (Noël et al., 2001). Likewise, individuals may exhibit difficulties taking into account the future consequences of an action in emotional contexts (Billieux et al., 2010), which might underlie alcohol use following positive emotions (Dolan, Bechara, & Nathan, 2008). Further, research would benefit examining the role of positive emotional avoidance in the inability to experience positive emotions among individuals with PTSD (i.e., D7 criterion; American Psychiatric Association, 2013). Specifically, studies are needed to better understand the extent to which positive emotional experiences are restricted in PTSD as a result of autonomic, passive processes versus conscious, active processes. Lastly, given evidence that the experience of positive and negative emotions often co-occur (Watson, Clark, & Tellegen, 1988), it is important for future studies to tease apart the contributions of positive emotion dysfunction to alcohol misuse beyond those of negative emotion dysfunction.
Results should be considered within the context of study limitations. First, the cross-sectional and correlational nature of the data precludes causal determination of the associations examined. Future research is needed to investigate the nature and direction of these relations through prospective, longitudinal investigations. Second, this study relied exclusively on self-report measures, which may be influenced by one’s willingness and/or ability to report accurately. Future investigations should include objective (e.g., behavioral, physiological) measures of emotional responding (Gratz, Rosenthal, Tull, Lejuez, & Gunderson, 2006; Vasilev, Crowell, Beauchaine, Mead, & Gatzke-Kopp, 2009). Third, prior research indicates that levels of the primary study variables may vary as a function of sex (male vs. female) and military (veteran vs. civilian) status (Grant et al., 2015; Kilpatrick et al., 2013; Weiss et al., 2015). Unfortunately, the current sample is not large enough to examine moderated sequential mediation, and does not include civilians. Future research with larger samples and both civilian and military participants is necessary. Fourth, collecting data via the internet has disadvantages that may limit generalizability of results, such as sample biases and lack of control over the research environment (Kraut et al., 2004). Further, while MTurk has been shown to generate reliable data (Buhrmester, Kwang, & Gosling, 2011; Shapiro, Chandler, & Mueller, 2013) and represent the general population in terms of demographics (Mishra & Carleton, 2017) and prevalence of mental health problems (Shapiro et al., 2013), including PTSD (van Stolk‐Cooke et al., 2018), we are not aware of any studies that have demonstrated the reliability and validity of MTurk in military populations. Future research that integrates other data collection methods and examines the utility of MTurk in military samples is necessary. Lastly, to our knowledge, this is the first study to examine the roles of positive emotional intensity or positive emotional avoidance (separately or sequentially) in the relation between PTSD symptoms and alcohol misuse. As such, replication among other military (e.g., clinical) or trauma-exposed (e.g., civilian) populations is warranted (e.g., to see if the strength and directionality of findings generalizes to other samples). For instance, while a community-based recruitment approach captures a larger segment of the population and thus is a strength of our study, our findings may not generalize to clinical samples of US military veterans who likely have more severe PTSD symptoms and greater alcohol misuse. Further, this study did not address unique military subgroup differences, such as in branches of the military or active duty versus reserve veteran populations.
Despite these limitations, results of the current study extend our understanding of the roles of positive emotional intensity and positive emotional avoidance in the association between PTSD symptoms and alcohol misuse. Specifically, findings provided support for the separate role of positive emotional avoidance in the PTSD symptoms-alcohol misuse relation, such that higher levels of positive emotional avoidance accounted for this association. Moreover, results highlighted the sequential role of positive emotional intensity and positive emotional avoidance in the relation between PTSD symptoms and alcohol misuse. In particular, greater severity of PTSD symptoms was related to greater positive emotional intensity, which was related to greater positive emotional avoidance, which was related to greater alcohol misuse. These findings have important implications for our understanding of positive emotional experiences, indicating contexts in which they may be deleterious. Future research and clinical practice should consider the potentially adverse consequences of positive emotional experiences.
Highlights.
More severe PTSD symptoms were related to greater alcohol misuse
PTSD was indirectly related to alcohol misuse through positive emotional avoidance
Positive emotional intensity did not explain the PTSD to alcohol misuse relation
Positive emotional intensity and positive emotional avoidance were sequential mediators
Targeting positive emotional avoidance may reduce the PTSD-alcohol misuse relation
Role of Funding Sources:
This work was supported by the National Institute on Drug Abuse (K23DA039327). NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Work on this paper by the first author (NHW) was supported by National Institute on Drug Abuse grant K23DA039327.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors declare that they have no conflicts of interest.
Declarations of interest: none.
Consistent with recommendations by Winer et al. 2016 we examined the alternative sequential mediation model (i.e., PTSD symptoms to positive emotional avoidance to positive emotional intensity to alcohol misuse). The serial indirect effect through both positive emotional avoidance and positive emotional intensity was nonsignificant.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author. [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychol Rev, 111, 33–51. doi: 10.1037/0033-295X.111.1.33 [DOI] [PubMed] [Google Scholar]
- Billieux J, Gay P, Rochat L, & Van der Linden M (2010). The role of urgency and its underlying psychological mechanisms in problematic behaviours. Behav Res Ther, 48, 1085–1096. [DOI] [PubMed] [Google Scholar]
- Blevins CA, Weathers FW, Davis MT, Witte TK, & Domino JL (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and initial psychometric evaluation. J Trauma Stress, 28, 489–498. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychol Assess, 28, 1379–1391. [DOI] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon’s Mechanical Turk: A new source of inexpensive, yet high-quality, data? Perspectives on Psychological Science, 6, 3–5. [DOI] [PubMed] [Google Scholar]
- Coskunpinar A, Dir AL, & Cyders MA (2013). Multidimensionality in impulsivity and alcohol Use: a meta-analysis using the UPPS model of impulsivity. Alcoholism: Clinical and Experimental Research, 37, 1441–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cyders MA, Zapolski TCB, Combs JL, Settles RF, Fillmore MT, & Smith GT (2010). Experimental effect of positive urgency on negative outcomes from risk taking and on increased alcohol consumption. Psychology of Addictive Behaviors, 24, 367–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dolan SL, Bechara A, & Nathan PE (2008). Executive dysfunction as a risk marker for substance abuse: The role of impulsive personality traits. Behavioral Sciences & the Law, 26, 799–822. [DOI] [PubMed] [Google Scholar]
- Driessen M, Schulte S, Luedecke C, Schaefer I, Sutmann F, Ohlmeier M, Kemper U, Koesters G, Chodzinski C, Schneider U, Broese T, Dette C, & Havemann-Reinicke U (2008). Trauma and PTSD in patients with alcohol, drug, or dual dependence: A multi-center study. Alcoholism: Clinical and Experimental Research, 32, 481–488. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL (1998). What good are positive emotions? Review of General Psychology, 2, 300–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL (2001). The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist, 56, 218–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredrickson BL, Tugade MM, Waugh CE, & Larkin GR (2003). What good are positive emotions in crisis? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. Journal of Personality and Social Psychology, 84, 365–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen PA, Dozois DJA, & Lanius RA (2012). Assessment of anhedonia in psychological trauma: Psychometric and neuroimaging perspectives. European Journal of Psychotraumatology, 3, 8587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frewen PA, Dozois DJA, Neufeld RWJ, & Lanius RA (2012). Disturbances of emotional awareness and expression in posttraumatic stress disorder: Meta-mood, emotion regulation, mindfulness, and interference of emotional expressiveness. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 152–161. [Google Scholar]
- Geuens M, & De Pelsmacker P (2002). Developing a short affect intensity scale. Psychological Reports, 91, 657–670. [DOI] [PubMed] [Google Scholar]
- Grant BF, Goldstein RB, Saha TD, Chou SP, Jung J, Zhang H, … & Hasin DS (2015). Epidemiology of DSM-5 alcohol use disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA psychiatry, 72, 757–766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, Rosenthal MZ, Tull MT, Lejuez CW, & Gunderson JG (2006). An experimental investigation of emotion dysregulation in borderline personality disorder. J Abnorm Psychol, 115, 850–855. [DOI] [PubMed] [Google Scholar]
- Gray MJ, Litz BT, Hsu JL, & Lombardo TW (2004). Psychometric properties of the Life Events Checklist. Assessment, 11, 330–341. [DOI] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis. New York, NY: Guilford Press. [Google Scholar]
- Jacobson IG, Ryan MA, Hooper TI, Smith TC, Amoroso PJ, Boyko EJ, … & Bell NS (2008). Alcohol use and alcohol-related problems before and after military combat deployment. JAMA, 300, 663–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpatrick DG, Resnick HS, Milanak ME, Miller MW, Keyes KM, & Friedman MJ (2013). National estimates of exposure to traumatic events and PTSD prevalence using DSM-IV and DSM-5 criteria. Journal of Traumatic Stress, 26, 537–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimble MO, Fleming K, & Bennion KA (2013). Contributors to hypervigilance in a military and civilian sample. J Interpers Violence, 28, 1672–1692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraut R, Olson J, Banaji M, Bruckman A, Cohen J, & Couper M (2004). Psychological research online: Report of Board of Scientific Affairs’ Advisory Group on the Conduct of Research on the Internet. American Psychologist, 59, 105–117. [DOI] [PubMed] [Google Scholar]
- Litz BT, Orsillo SM, Kaloupek D, & Weathers F (2000). Emotional processing in posttraumatic stress disorder. J Abnorm Psychol, 109, 26–39. doi: 10.1037/0021-843X.109.1.26 [DOI] [PubMed] [Google Scholar]
- Lorber W, & Garcia HA (2010). Not supposed to feel this: Traditional masculinity in psychotherapy with male veterans returning from Afghanistan and Iraq. Psychotherapy: Theory, Research, Practice, Training, 47, 296–305. [DOI] [PubMed] [Google Scholar]
- Marshall GN, Schell TL, Glynn SM, & Shetty V (2006). The role of hyperarousal in the manifestation of posttraumatic psychological distress following injury. J Abnorm Psychol, 115, 624–628. [DOI] [PubMed] [Google Scholar]
- McAllister L, Callaghan JE, & Fellin LC (2019). Masculinities and emotional expression in UK servicemen: ‘Big boys don’t cry’? Journal of Gender Studies, 28, 257–270. [Google Scholar]
- Meade AW, & Craig SB (2012). Identifying careless responses in survey data. Psychological Methods, 17, 437–455. [DOI] [PubMed] [Google Scholar]
- Mills KL, Lynskey M, Teesson M, Ross J, & Darke S (2005). Post-traumatic stress disorder among people with heroin dependence in the Australian treatment outcome study (ATOS): Prevalence and correlates. Drug and Alcohol Dependence, 77, 243–249. [DOI] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Ross J, & Peters L (2006). Trauma, PTSD, and substance use disorders: Findings from the Australian National Survey of Mental Health and Well-Being. American Journal of Psychiatry, 163, 652–658. [DOI] [PubMed] [Google Scholar]
- Mishra S, & Carleton RN (2017). Use of online crowdsourcing platforms for gambling research. International Gambling Studies, 17, 125–143. [Google Scholar]
- Noël X, Paternot J, Van der Linden M, Sferrazza R, Verhas M, Hanak C, Kornreich Charles, Martin P, De Mol J, Pelc I, & Verbanck P (2001). Correlation between inhibition, working memory and delimited frontal area blood flow measured by 99MTC–bicisate spect in alcohol–dependent patients. Alcohol and Alcoholism, 36, 556–563. [DOI] [PubMed] [Google Scholar]
- Oppenheimer DM, Meyvis T, & Davidenko N (2009). Instructional manipulation checks: Detecting satisficing to increase statistical power. Journal of Experimental Social Psychology, 45, 867–872. [Google Scholar]
- Ouimette PC, Wolfe J, & Chrestman KR (1996). Characteristics of posttraumatic stress disorder—Alcohol abuse comorbidity in women. Journal of Substance Abuse, 8, 335–346. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36, 717–731. doi: 10.3758/BF03206553 [DOI] [PubMed] [Google Scholar]
- Riggs DS, Rukstalis M, Volpicelli JR, Kalmanson D, & Foa EB (2003). Demographic and social adjustment characteristics of patients with comorbid posttraumatic stress disorder and alcohol dependence: Potential pitfalls to PTSD treatment. Addictive Behaviors, 28, 1717–1730. [DOI] [PubMed] [Google Scholar]
- Roemer L, Litz BT, Orsillo SM, & Wagner AW (2001). A preliminary investigation of the role of strategic withholding of emotions in PTSD. J Trauma Stress, 14, 149–156. [Google Scholar]
- Saladin ME, Brady KT, Dansky BS, & Kilpatrick DG (1995). Understanding comorbidity between PTSD and substance use disorders: Two preliminary investigations. Addictive Behaviors, 20(5), 643–655. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88, 791–804. [DOI] [PubMed] [Google Scholar]
- Schick MR, Weiss NH, Contractor A, Dixon-Gordon KL, & Spillane N (in press). Depression and risky alcohol use: An examination of the role of difficulties regulating positive emotions in trauma-exposed individuals. The American Journal of Drug and Alcohol Abuse. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, & Ren L (2011). Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug and Alcohol Dependence, 116, 93–101. [DOI] [PubMed] [Google Scholar]
- Searle AK, Van Hooff M, McFarlane AC, Davies CE, Fairweather-Schmidt AK, Hodson SE, Benassi H, & Steele N (2015). The validity of military screening for mental health problems: diagnostic accuracy of the PCL, K10 and AUDIT scales in an entire military population. International Journal of Methods in Psychiatric Research, 24, 32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro DN, Chandler J, & Mueller PA (2013). Using Mechanical Turk to study clinical populations. Clinical Psychological Science, 1(2), 213–220. [Google Scholar]
- Smith SM, Goldstein RB, & Grant BF (2016). The association between post-traumatic stress disorder and lifetime DSM-5 psychiatric disorders among veterans: data from the National Epidemiologic Survey on Alcohol and Related Conditions-III (NESARC-III). J Psychiatr Res, 82, 16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor CT, Laposa JM, & Alden LE (2004). Is avoidant personality disorder more than just social avoidance? J Pers Disord, 18, 571–594. [DOI] [PubMed] [Google Scholar]
- Thomas KA, & Clifford S (2017). Validity and mechanical turk: An assessment of exclusion methods and interactive experiments. Comput Human Behav, 77, 184–197. [Google Scholar]
- Tugade MM, & Fredrickson BL (2004). Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology, 86, 320–333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Stolk-Cooke K, Brown A, Maheux A, Parent J, Forehand R, & Price M (2018). Crowdsourcing trauma: Psychopathology in a trauma-eposed sample recruited via Mechanical Turk. J Trauma Stress, 31, 549–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasilev CA, Crowell SE, Beauchaine TP, Mead HK, & Gatzke-Kopp LM (2009). Correspondence between physiological and self-report measures of emotion dysregulation: A longitudinal investigation of youth with and without psychopathology. Journal of Child Psychology and Psychiatry, 50, 1357–1364. [DOI] [PubMed] [Google Scholar]
- Walser RD, & Westrup D (2007). Acceptance and commitment therapy for the treatment of post-traumatic stress disorder and trauma-related problems: A practitioner’s guide to using mindfulness and acceptance strategies. Oakland, CA: New Harbinger. [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology, 54, 1063–1070. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The Life Events Checklist for DSM-5 (LEC-5).
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5).
- Weiss NH, Contractor AA, Forkus SR, Goncharenko S, & Raudales AM (in press). Positive emotion dysregulation among community individuals: The role of traumatic exposure and posttraumatic stress disorder. J Trauma Stress. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Dixon-Gordon KL, Peasant C, & Sullivan TP (2018). An examination of the role of difficulties regulating positive emotions in posttraumatic stress disorder. J Trauma Stress, 31, 775–780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Forkus SR, Contractor AA, & Schick MR (2018). Difficulties regulating positive emotions and alcohol and drug misuse: A path analysis. Addictive Behaviors, 84, 45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Gratz KL, & Lavender J (2015). Factor structure and initial validation of a multidimensional measure of difficulties in the regulation of positive emotions: The DERS-Positive. Behav Modif, 39, 431–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Nelson R, Contractor AA, & Sullivan TP (in press). Emotion dysregulation and posttraumatic stress disorder: A test of the incremental role of difficulties regulating positive emotions Anxiety, Stress, & Coping. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Risi MM, Bold KW, Sullivan TP, & Dixon-Gordon KL (in press). Daily relationship between positive affect and drinking to cope: The moderating role of difficulties regulating positive emotions. The American Journal of Drug and Alcohol Abuse. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Schick MR, Contractor AA, & Dixon-Gordon KL (2019). Posttraumatic stress disorder and substance use: Identifying the underlying role of difficulties regulating positive emotions. Addictive Behaviors, 96, 119–126. [DOI] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Dixon-Gordon KL, & Gratz KL (2018). Assessing the negative and positive emotion-dependent nature of risky behaviors among substance dependent patients. Assessment, 25, 702–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Sullivan TP, Dixon-Gordon KL, & Gratz KL (2015). Posttraumatic stress disorder symptoms and risky behaviors among trauma-exposed inpatients with substance dependence: The influence of negative and positive urgency. Drug and Alcohol Dependence, 155, 147–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisco BE, Marx BP, Holowka DW, Vasterling JJ, Han SC, Chen MS, … Keane TM (2014). Traumatic brain injury, PTSD, and current suicidal ideation among Iraq and Afghanistan US veterans. J Trauma Stress, 27, 244–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, Foa EB, Young-McCaughan S, Yarvis JS, Hembree EA, Mintz J, Peterson AL Hembree EA (2016). Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychol Assess, 28, 1392–1403. [DOI] [PubMed] [Google Scholar]


