Abstract
Background
Surgical treatment methods for patients with complex coronary artery disease (CAD) who have undergone vascular reconstruction mainly include coronary artery bypass graft (CABG) and percutaneous coronary intervention (PCI). The purpose of the study aimed to compare a 1-year follow-up for the patient clinical outcomes and costs between PCI and CABG treatment.
Material/Methods
There were 840 patients enrolled in this study from July 2015 to September 2016. Among the study participants, 420 patients underwent PCI treatment and 420 patients underwent off-pump CABG. Patients costs were assessed from the perspective of the China healthcare and medical insurance system. EuroQOL 5-dimension 3 levels (EQ-5D-3L) questionnaire was used to evaluate the general health status, and the Seattle Angina Questionnaire (SAQ) was used to assess the disease-specific health status.
Results
After a 1-year follow-up, the all-cause mortality (P=0.0337), the incidence of major adverse cardiac and cerebrovascular events (P<0.001), and additional revascularization (P<0.001) in PCI group were significantly higher than those in CABG group. Both groups have significant sustained benefits in the SAQ subscale. The CABG group had a higher score on the frequency of angina than the PCI group. In addition, the quality-adjusted life year value of PCI and CABG resulted was 0.8. The average total cost for PCI was $14 643 versus CABG cost of $13 842 (P=0.0492).
Conclusions
In the short-term, among the CAD patients with stable triple-vessel or left-main, costs and clinical outcomes are substantially higher for CABG than PCI. Long-term, economic, and health benefits analysis, is warranted.
MeSH Keywords: Coronary Artery Bypass, Coronary Artery Disease, Costs and Cost Analysis, Percutaneous Coronary Intervention
Background
Complex coronary artery disease (CAD) includes multi-vessel coronary artery and left-main coronary diseases. The disease poses a serious threat to patient health but also exerts a significant financial burden on patients and the healthcare system. The mainstay therapeutic strategies for complex CAD with stable angina are medical treatment (MT) and revascularization treatment (RT), including percutaneous coronary intervention (PCI) and coronary artery bypass graft (CABG) [1,2]. Studies show that CABG is still the standard of treatment for patients with left-main and multiple-coronary disease due to its high safety and effectiveness [3–6]. From a health economics analysis perspective, the different therapeutic strategies have varying costs for initial treatments and long-term management. Previous economic analysis has suggested that CABG, compared to PCI, remains a cost-effective strategy for patients undergoing multi-vessel coronary revascularization [1].
In China, the application of complex CAD and the associated major adverse outcomes is still a significant concern for the public health system. Furthermore, information on costs and clinical outcomes of complex CAD among this population is unknown. Therefore, this study was aimed to compare the PCI and the CABG therapeutic strategies and the economic outcome in complex CAD of Chinese patients.
Material and Methods
Ethical approval
This study was approved by the Institutional Review Board and Ethics committee of Anzhen Hospital, all procedures were carried out by the World Medical Association Declaration of Helsinki. This study provided patients with written informed consent, and all patients signed their consent to participate in the study.
Participants
This study aimed to compare the applications of PCI and CABG with stable triple-vessel or left-main bypass in CAD patients without cardiopulmonary. The primary endpoint events recorded for CAD patients included stroke, myocardial infarction (MI), the combined incidence of overall mortality, and persistent angina requiring additional revascularization. The patients were enrolled in this single-center study at Anzhen hospital from July 2015 to September 2016. The inclusion criteria for this study included patients with proximal multivessel coronary artery stenosis (>70% stenosis) or left-main coronary artery stenosis (>50% stenosis). The exclusion criteria were the patient who unstable angina (UA) or acute MI needed emergency revascularization. The patients were excluded if they had another CABG or PCI contraindication. In this study, all the patients received optimal medical treatment, according to their clinical needs. Therapeutic drugs mainly included angiotensin-converting enzyme inhibitors, beta-blockers, statins, diuretics, calcium channel blockers, and nitrates [7]. In this study, the main stents used for PCI were sirolimus-eluting stents (SES) and paclitaxel-eluting stents (PES), and patients were treated with standard PCI techniques. Furthermore, the patients who received off-pump CABG treatment were treated according to standard techniques.
Follow-up
The patients had outpatient follow-ups at 1, 3, 6, and 12 months during the first year. The major adverse clinical cardiac and cerebral events (MACCE) were recorded, including all-cause of death, MI, stroke, and additional revascularization. The diagnosis of MI was based on an increase in serum creatine kinase-MB levels greater than twice the average reference value, new Q waves on at least 2 electrocardiogram (ECG) readings, and characteristic chest pain symptoms. The diagnosis of stroke is confirmed by brain computed tomography (CT), magnetic resonance imaging (MRI), and clinical manifestations.
Economic analysis
The cumulative costs of each treatment strategy in the CABG group and PCI group during the study period were compared using an economic analysis. The cost of hospitalization was directly obtained from the medical records of Anzhen Hospital, including the cost of antibacterial drugs, proprietary Chinese medicines, and Chinese herbal medicines. The following interventions were charged at standard fee rates, which included anesthesia, interventional treatment, surgery, care, vital signs monitoring, mechanical ventilation, and oxygenation. Other treatment costs involved clinical physical treatment, special treatment, rehabilitation treatment, psychotherapy, and Chinese traditional medicine treatment. The cardiovascular tests included echocardiogram, treadmill exercise test, radioisotope examination, single-photon emission CT, radiography, and coronary arteriography; the costs associated with these tests were considered patient examination and pathological examination fees. Additional costs were incurred for laboratory tests, blood transfusion, albumin and globulin products, coagulation factors, and cytokines; disposable medical materials, and bed fees. The follow-up costs include cardiovascular and brain hospital costs, other surgery-related costs, and medication costs. The follow-up cost=the number of events by median costs per the endpoint event+the costs of medicines. The diagnostically related group price in the Medicare claims data were from the Beijing Medical Insurance Center as unit cost estimates and the costs of repeated were estimated by using the cost of on-pump CABG. All expenses of patients were measured in the Renminbi (RMB). Costs of resources in Beijing Area are: $16 963 for CABG; $11 369 for PCI; $9 424 for hospitalization due to MI; $2659 for hospitalization due to stroke [8]; $3 for clopidogrel cost per day; $2 for statins cost per day, $0.8 for beta-blocker cost per day, and $0.1 for aspirin cost per day. In our primary analysis, estimates of follow-up costs depend on Medicare claims from the Beijing Medical Insurance Center, and we also calculated the follow-up costs to compare the data from the Guangzhou and Xining Medical Insurance Centers. The follow-up costs were adjusted follow to the Guangzhou and Xining consumer price indexes, as appropriate according to 2012. For this period, 1000 RMB was approximately $156.60.
Measurement of health status
The general health status was evaluated using the EuroQOL 5-dimension 3 level questionnaire (EQ-5D-3L) health status instrument for each enrolled patient at baseline, as well as at follow-up intervals of 1, 6, and 12 months after initial treatment [9]. In this study, the EQ-5D-3L data was used to weighting for the health state utility (range 0–1, high scores indicate healthier patients). The Seattle Angina Questionnaire (SAQ) was used to assess the disease-specific health status.
Statistical analysis
The population baseline characteristics were described using percentages (%, categorical variables) and mean±standard deviation (SD, continuous variables). Categorical variables were tested using Fisher’s exact test. For continuity data, the skewness and kurtosis tests were first used to evaluate whether the data conformed to the normal distribution; then, the Student’s t-test was used to compare the data of the normal distribution, and the Mann-Whitney U test was used to compare the data of the non-normal distribution. Compared with the traditional significance test, the standardized difference has a lower sensitivity to the sample size, which helps to identify meaningful differences. Typically, standardization differences >0.2 are considered significant.
We used a type of propensity score analysis to inverse probability of treatment weighting (IPW) methods to address the confounding effects of observed covariates. Two different sets of IPW-adjusted analyses were used in this study, respectively, and the weights are based on results from a treatment selection model. Logistic regression was used to estimate the different treatments as the dependent variable and the baseline characteristics including age, sex, body mass index (BMI), previous angina, previous MI, previous heart failure, previous arrhythmia, previous stroke, peripheral artery disease, diabetes mellitus, hypertension, dyslipidemia, chronic renal failure, chronic obstructive pulmonary disease (COPD), current smoking status, glomerular filtration rate (GFR), left ventricular ejection fraction (LVEF), left main artery disease, SYNergy between PCI with TAXUS™ and Cardiac Surgery (SYNTAX) score, and EuroSCORE-as independent variables. Core lab SYNTAX score calculations were performed by Corelab (CCRF, Beijing) Inc. and cardiologists at Yale-New Heaven Hospital. According to the standard operation procedure, each angiogram was reviewed by 2 doctors independently. If the difference between the 2 SYNTAX scores was >5, a third doctor confirmed the ultimate score. Both the exact data from every lesion and the total score were collected. Subsequently, the degree of every stenosis was also recorded by core-lab for inclusion criteria adjudication. Moreover, we calculated the weights in each patient as the inverse of the probability that the patient receives treatment under the observed covariates [10–12]. The collated data was weighted at first, then the categorical variables were tested by using χ2 test, and the continuous variables were calculated by mean±SD, and t-test was used to evaluate the characteristics of the baseline data between the 2 groups. P-values <0.05 were considered the difference is statistically significant. Cumulative costs of the patient’s hospitalization were compared based on the intention-to-treat. Statistical analysis of the study data was performed using SAS 9.1 software (SAS, Institute Inc., Cary, NC, USA).
In addition, a 1-year follow-up period of each patient about quality-adjusted life-year (QALY) was estimated as the time-weighted average of the patient’s utility value. The time from recruitment to the procedure was defined as the baseline utility, and through the midpoint between the 1- and 6-month follow-ups was defined as the 1-month utility value. In the study, missing the data of the experiment was less than 1% in our analysis, and the missing utility value was replaced by the last observed value of the previous utility value.
Results
Patient characteristics
From the 840 patients, equal numbers underwent PCI and CABG. The PCI group patients were slightly younger than the CABG group (mean age; 60.2 years versus 61.6 years), were more often female (indicate percentages for comparison) and smokers (indicate rates for comparison). In the CABG group, the patients were more likely to have a history of left-main, heart failure, and diabetes mellitus. Moreover, in the SYNTAX scores ≥32, the proportion of patients was more significant in the group CABG than the group PCI (Table 1). In the baseline characteristics, there were no significant differences between the 2 groups after applying inverse probability weights (Table 2).
Table 1.
Baseline characteristics of CABG and PCI patients.
| Baseline characteristics | Treatment | P-value | Standardized difference | |
|---|---|---|---|---|
| PCI (N=420) | CABG (N=420) | |||
| Female sex | 119 (28.4%) | 93 (22.2%) | 0.0386 | 0.143 |
| Age (years) | 60.19±10.27 | 61.63±8.66 | 0.0283 | 0.152 |
| Age >65 years | 130 (31%) | 134 (32.0%) | 0.7661 | 0.021 |
| BMI (kg/m2) | 25.78±3.54 | 25.47±4.47 | 0.2613 | 0.022 |
| Previous angina | 394 (94%) | 394 (94%) | 1.000 | 0.000 |
| Previous MI | 136 (32.5%) | 147 (35.1%) | 0.4217 | 0.058 |
| Previous HF | 2 (0.5%) | 9 (2.1%) | 0.0272 | 0.147 |
| Previous arrhythmia | 56 (13.4%) | 52 (12.4%) | 0.68 | 0.028 |
| Stroke | 55 (13.1%) | 52 (12.4%) | 0.7562 | 0.035 |
| TIA | 3 (0.7%) | 0 (0%) | 0.0412 | 0.063 |
| PAD | 4 (1%) | 7 (1.7%) | 0.3595 | 0.120 |
| Diabetes mellitus | 137 (32.7%) | 168 (40.1%) | 0.0259 | 0.154 |
| Hypertension | 320 (76.4%) | 319 (76.1%) | 0.7212 | 0.025 |
| Dyslipidemia | 320 (76.4%) | 319 (76.1%) | 0.9353 | 0.006 |
| Chronic renal failure | 0 | 0 | NA | 0 |
| COPD | 7 (1.7%) | 4 (1%) | 0.3575 | 0.063 |
| Venous thromboembolism | 2 (0.5%) | 0 (0%) | 0.0956 | 0.098 |
| Current smoke | 152 (36.3%) | 140 (33.4%) | 0.0393 | 0.176 |
| Cr (mg/dL) | 75.64±16.68 | 76.67±17.61 | 0.3849 | 0.06 |
| Cr >133 mg/dL | 3 (0.7%) | 1 (0.2%) | 0.3085 | 0.069 |
| LVEF (%) | 73.87±102.02 | 62±46.84 | 0.0307 | 0.15 |
| NYHA | 0.387 | 0.118 | ||
| III | 18 (4.3%) | 22 (5.3%) | ||
| IV | 1 (0.2%) | 4 (1%) | ||
| Left main artery disease | 89 (21.2%) | 187 (44.6%) | 0.0000 | 0.514 |
| CTO | 0.47±0.66 | 0.82±0.83 | 0.0000 | 0.463 |
| SYNTAX score | 0.0000 | 0.550 | ||
| Low risk | 244 (58.2%) | 150 (35.8%) | ||
| Median risk | 139 (33.2%) | 163 (38.9%) | ||
| High risk | 36 (8.6%) | 106 (25.3%) | ||
| EuroSCORE | 2.35±2.05 | 2.26±1.86 | 0.5141 | 0.045 |
PCI – percutaneous coronary intervention; CABG – coronary artery bypass surgery; BMI – body mass index; MI – myocardial infarction; HF – heart failure; TIA – transient ischemic attack; PAD – peripheral artery disease; COPD – chronic obstructive pulmonary disease; Cr – creatinine; LVEF – left ventricular ejection fraction; NYHA – New York Heart Association Functional Classification; CTO – chronic total occlusion.
Table 2.
Baseline characteristics of CABG and PCI patients after application of inverse probability weights.
| Baseline characteristics | Treatment | P-value | Standardized difference | |
|---|---|---|---|---|
| PCI (N=420) | CABG (N=420) | |||
| Female sex | 27.1% | 25.8% | 0.6679 | 0.03 |
| Age (years) | 61.6±10.41 | 61.2 ±8.96 | 0.5472 | 0.042 |
| Age >65 years | 34.6% | 32.3% | 0.4641 | 0.051 |
| BMI (kg/m2) | 25.67±3.12 | 25.77±3.19 | 0.6527 | 0.031 |
| Previous angina | 93.9% | 93.8% | 0.9645 | 0.003 |
| Previous MI | 36.7% | 34.5% | 0.5141 | 0.045 |
| Previous HF | 3% | 1.4% | 0.1111 | 0.109 |
| Previous arrhythmia | 13.1% | 14.1% | 0.761 | 0.021 |
| Stroke | 12.8% | 12.3% | 0.8333 | 0.015 |
| TIA | 0.4% | 0% | 0.1518 | 0.008 |
| PAD | 1.4% | 1.3% | 0.9109 | 0.084 |
| Diabetes mellitus | 37.5% | 35.9% | 0.64 | 0.032 |
| Hypertension | 82.7% | 82.9% | 0.9256 | 0.006 |
| Dyslipidemia | 75.2% | 76.2% | 0.732 | 0.024 |
| Chronic renal failure | 0 | 0 | NA | 0 |
| COPD | 1.4% | 1.4% | 0.9292 | 0.006 |
| Venous thromboembolism | 0.2% | 0% | 0.242 | 0.069 |
| Current smoke | 35.4% | 35.3% | 0.9567 | 0.017 |
| Cr (mg/dL) | 76.08±16.04 | 75.94 ±17.6 | 0.9051 | 0.008 |
| Cr >133 mg/dL | 0.5% | 0.2% | 0.3457 | 0.064 |
| LVEF (%) | 67.96±76.2 | 65.67±70.61 | 0.6523 | 0.031 |
| NYHA | 0.7426 | 0.077 | ||
| III | 6.1% | 4.7% | ||
| IV | 0.3% | 0.6% | ||
| Left main artery disease | 33.7% | 33.20% | 0.8717 | 0.011 |
| CTO | 0.64±0.74 | 0.64±0.77 | 0.866 | 0.012 |
| SYNTAX score | 0.8511 | 0.04 | ||
| Low risk | 45.9% | 46.7% | ||
| Median risk | 35.3% | 36% | ||
| High risk | 18.8% | 17.3% | ||
| EuroSCORE | 2.45±2.2 | 2.32±1.88 | 0.3612 | 0.063 |
PCI – percutaneous coronary intervention; CABG – coronary artery bypass surgery, BMI – body mass index; MI – myocardial infarction; HF – heart failure; TIA – transient ischemic attack; PAD – peripheral artery disease; COPD – chronic obstructive pulmonary disease; Cr – creatinine; LVEF – left ventricular ejection fraction; NYHA – New York Heart Association Functional Classification; CTO – chronic total occlusion.
One-year clinical outcome and medical resource use
The patient follow-up was conducted to 1 year, and the major adverse cardiovascular and cerebral events (MAACE) are demonstrated in Figure 1. The patient’s follow-up rate achieved 99%, only 2 patients in the bypass group were lost, and 3 patients in the PCI group were lost. After inverse weighting for the probability, the rates of all-cause mortality (3.6% versus 1.3%; P=0.0337), the MACCE (11.3% versus 4.1%; P=0.0001), and the additional revascularization (8.3% versus 1.2%; P<0.0001) were significantly higher in group PCI than group CABG. Notably, there was no significant between in PCI group and CABG group for the cumulative incidence of stroke (0.3% versus 1.5%; P=0.0546) and MI (0.2% versus 0%; P=0.3218). The detailed medical resource usage of the study listed in Table 3.
Figure 1.
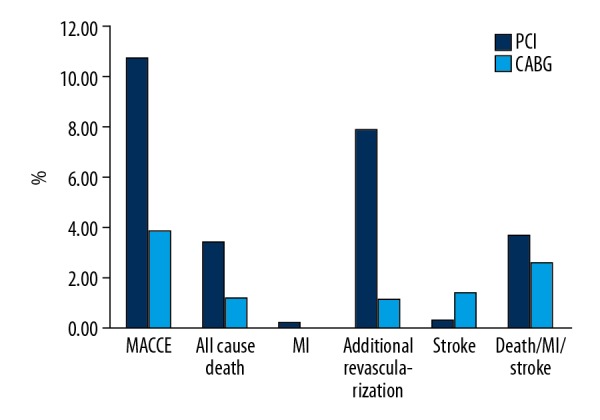
Major adverse cardiac and cerebral events between CABG and PCI groups at a 1-year follow-up (adjusted). CABG – coronary artery bypass surgery; PCI – percutaneous coronary intervention.
Table 3.
One-year medical resource use.
| Variable | PCI (N=420) | CABG (N=420) | P-value |
|---|---|---|---|
| Initial hospital length of stay | 7 (5.11) | 19 (15.24) | <0.0001 |
| Number of stents | 2.07±1.21 | Null | NA |
| Number of grafts | Null | 3.11±1.22 | NA |
| Follow-up revascularization procedures | 33 (7.9%) | 5 (1.2%) | <0.0001 |
| Follow-up PCI | 32 (7.6%) | 2 (0.5%) | <0.0001 |
| Follow-up CABG | 1 (0.2%) | 3 (0.7%) | 0.3052 |
PCI – percutaneous coronary intervention; CABG – coronary artery bypass surgery; NA – not applicable.
Utility weights and quality-adjusted life years (QALYs)
The EQ-5D-3L value was used to assess the general health status of including patients, which are summarized in Table 4. After a 1-year follow-up, the utility weights improved substantially for both group PCI and group CABG. Moreover, the SAQ value was used to assess the disease-specific health status, and the significant and sustained benefits were evident across each of the subscales for both groups, more details are shown in Table 5. After 1-, 6-, and 12-month intervals, the frequency for angina was significantly higher with the CABG group than the PCI group for the scores of the subscales. In addition, an increasing trend at 1 month for the scores of the physical limitations subscales in the PCI group. However, after 1 month, there was no apparent difference in this parameter between the groups. Notably, the scores of the angina stability, treatment satisfaction, and the disease perception were no statistical differences between the 2 groups.
Table 4.
EQ-5D utility scores and QALY in CABG and PCI groups after application of inverse probability weights.
| Time point | Treatment | P-value | |
|---|---|---|---|
| PCI (N=420) | CABG (N=420) | ||
| Baseline | 0.78±0.12 | 0.78±0.11 | 0.8528 |
| 1-month | 0.78±0.08 | 0.74±0.11 | <0.0001 |
| 6-month | 0.81±0.05 | 0.82±0.06 | 0.0351 |
| 12-month | 0.82±0.06 | 0.82±0.07 | 0.21 |
| 1-year QALY | 0.8±0.06 | 0.8±0.06 | 0.2299 |
PCI – percutaneous coronary intervention; CABG – coronary artery bypass surgery; QALY – quality-adjusted life year.
Table 5.
SAQ subscales in CABG and PCI groups after application of inverse probability weights.
| Scores on SAQ subscales | PCI (N=420) | CABG (N=420) | P-value |
|---|---|---|---|
| Physical limitation | |||
| Baseline | 68.62±25.11 | 69.48±23.14 | 0.6063 |
| 1 month | 95.45±12.54 | 89.91±18.95 | <0.001 |
| 6-month | 95.95±9.4 | 94.66±12.08 | 0.0848 |
| 12-month | 95.22±9.76 | 95.35±10.52 | 0.8558 |
| Angina stability | |||
| Baseline | 15.64±24.63 | 15.95±23.94 | 0.8501 |
| 1 month | 90.49±23.54 | 92.04±20.46 | 0.3095 |
| 6-month | 90.54±24.01 | 90.56±22.49 | 0.9911 |
| 12-month | 94.78±19.99 | 95.99±16.55 | 0.3367 |
| Angina frequency | |||
| Baseline | 65.77±27.09 | 62.68±27.43 | 0.1019 |
| 1 month | 93.86±14.31 | 96.90±11.38 | 0.0007 |
| 6-month | 93.41±14.5 | 96.52±12.25 | 0.0008 |
| 12-month | 94.03±13.97 | 96±13.49 | 0.0376 |
| Treatment satisfaction | |||
| Baseline | 77.91±18.44 | 79.4±19.38 | 0.2535 |
| 1 month | 87.54±11.49 | 88.09±11.34 | 0.4906 |
| 6-month | 87.91±12.03 | 88.72±11.5 | 0.3221 |
| 12-month | 87.7±10.82 | 87.41±10.51 | 0.7017 |
| Disease perception | |||
| Baseline | 51.09±22.56 | 48.25±22.20 | 0.0664 |
| 1-month | 81.32±14.12 | 82.03±13.78 | 0.4659 |
| 6-month | 82.3±14.05 | 84.83±12.76 | 0.0066 |
| 12-month | 82.7±13.5 | 84.14±12.33 | 0.1285 |
PCI – percutaneous coronary intervention; CABG – coronary artery bypass surgery.
Costs outcomes and sensitivity analyses
The costs in-hospital of the risk-adjusted median in group PCI was significantly lower than that in group CABG ($12 499 versus $13 626, respectively; P=0.0031, Table 6). In PCI patients, the risk-adjusted total costs, including both in-hospital and during follow-up were much higher than those in CABG patients ($14 643 versus $13 842; P=0.0492).
Table 6.
One-year cost-effectiveness outcomes for CABG and PCI groups after application of inverse probability weights*.
| Entry | Treatment | P-value | |
|---|---|---|---|
| PCI (N=420) | CABG (N=420) | ||
| In-hospital cost | 12.499±5.291 | 13.626±5.600 | 0.0031 |
| 1-year total cost | 14.643±5.950 | 13.842±5.710 | 0.0492 |
| 1-year event free cost | 16.509±6.708 | 14.434±5.944 | <0.0001 |
| Cost/QALY | 18.261±7.466 | 17.521±7.960 | 0.1690 |
Cost is given in US Dollars.
PCI – percutaneous coronary intervention; CABG – coronary artery bypass surgery; QALY – quality-adjusted life year.
At a 1-year follow-up, the MAACE-free costs were $16 509 and $14 434 for the PCI groups and CABG groups, respectively. The median cumulative costs for each patient during a 1-year follow-up were represented by the figures. The event-free costs were a significant difference between the 2 groups (P<0.0001), more details are shown in Table 6. Sensitivity analysis was used to recalculate the unit cost data from the local medical insurance centers in Xining and Guangzhou.
Discussion
As far as we know, this is the first direct comparison of economic and clinical outcomes between the PCI and the CABG for CAD patient treatment with triple-vessel and left main coronary artery in China. Our results reveal that in the short-term, CABG costs less than PCI and has a better prognosis among CAD patients with stable triple-vessel or left-main. This result of the study was consistent with some randomized clinical trials (RCT) and observational studies reported by previous economic and clinical outcomes [13–15].
The QALY score was lower with the CABG than PCI group (0.74 versus 0.78, P<0.0001) in the first month after the respective procedures. However, this difference did not hold during subsequent follow-up visits; after 1 year, the quality of life in the CABG treatment group was similar to the PCI treatment group. This trend in utility weight demonstrated that CABG surgery was more invasive than the PCI procedure and that patients in CABG groups required more recovery time to improve their quality of life. In this study, the EQ5D generally assessed the patients’ health status only. For the CAD patients with triple-vessel and left-main, using the SAQ may be a better option. Concerning disease-specific health status, the SAQ scores with the revascularization for angina stability, treatment satisfaction, angina frequency, and disease perception were higher than medication. Moreover, the scores on the subscales for angina frequency with the CABG group were higher than that of the PCI group.
Currently studying, only 1 randomized trial (MASS II) is compared to these 3 therapeutic strategies for long-term economic outcomes of CAD patients with multi-vessel [16]. The results of MASS II demonstrated that, at the 5-year follow-up period, the event-free costs of PCI were $19 967, and the CABG was $18 263. There was a significant difference favoring the use of medicine versus PCI (P<0.01) and CABG (P<0.01) in the paired comparison of the event-free costs, and there are also differences between CABG and PCI (P<0.01) [1]. In addition, other studies do compare PCI with MT, or CABG with MT [17,18]. Besides, it is demonstrated that there was significantly higher in the cumulative cost of the PCI group compared with MT, which was confirmed by the study of Sculpher et al. [19] and the Weintraub et al. [20]. Most recently, the medical costs were higher for surgical revascularization than for medical therapy in our study, which demonstrated by the Hlatky study ($20 300; P=0.0001) [21]. In our study, the event-free costs were $15 203 for RT; $16 509 for PCI; and $14 434 for CABG after 1-year follow-up. These observations compared with what has been reported for other countries regarding the treatment of complex CAD.
The cost-effective analysis was examining by compared the Bypass Angioplasty Revascularization Investigation (BARI) trial and CABG with conventional balloon angioplasty [22]. After a mean of 11.4 years follow-up, their findings revealed that CABG was a more cost-effective strategy for patients with complex CAD or diabetes mellitus. However, since the BARI trial, improvements in surgical and percutaneous revascularization techniques have affected the comparison of short-term and long-term clinical outcomes involving 2 revascularization strategies. Most recently, the Future Revascularization Evaluation in Patients with Diabetes Mellitus trial [Optimal Management of Multi-vessel Disease (FREEDOM)] after long-term follow-up also demonstrated that compared to DES-PCI (drug-eluting stent), CABG is a cost-effective revascularization strategy for treating patients with diabetes and multi-vessel CAD [23–25]. Moreover, CABG remains a cost-effective strategy suggested by BARI or other economic-based observational studies that conducted up to 1-year follow-up [25–29]. Therefore, the findings of our study agree with those of others, as described earlier.
After the initial hospitalization, the cost of PCI groups (without stents) was 9% lower than the CABG groups. After a 1-year follow-up, however, CABG proved to be more cost-effective in preventing composite primary endpoints. In this study, we found the cost of CABG in the Beijing area to be $16 963, yet the total in-hospital cost for the CABG group in Anzhen hospital was only $12 917. Although a little surprising, this attests to the rigorous medical quality and costs control in Anzhen hospital. Moreover, an interesting find was that the costs at hospital discharge and 1-year were lower with CABG than PCI in the study. It is noteworthy that this observation is quite different from what emerged in the analysis of FREEDOM and SYNTAX and deserves further investigation. The underlining reason for this difference is that the cost of stents, which were responsible for a more significant percentage of the total costs in the PCI group, is much higher in China. Given that clinical outcomes are better with CABG than PCI at 1-year and will likely become even better with longer follow-up, which is consisted of the study of Yang et al. [30]. Thus, we think that this finding has significant implications for the way patients should be treated in China.
This is the first observational study that compares the economic outcomes of these 2 therapeutic strategies for CAD patients with stable triple-vessel or left main in China. Undoubtedly, China is the largest developing country in the world, with entirely different healthcare and medical insurance systems compared to other developed countries. Notably, the prevalence of complex CAD is rising annually in China. This high-cost disease consumes significant proportions of healthcare resources, posing financial strain to the healthcare system and patients. We thought that this study would provide valuable information for the cost-effective management of CAD.
Conclusions
In the short-term, among the CAD patients with stable triple-vessel or left-main, costs and clinical outcomes were substantially higher for CABG than for PCI. And it necessary for a long-term economic analysis of these interventions.
Limitations
There are some limitations that should be acknowledged in our study. First, performing cost analysis is a challenging task [31,32]. Previous studies have reported various methods used to calculate the total cost of different treatments according to feasibility. However, considering the status of healthcare and the medical insurance system in China, we could only obtain the cost, mainly including the in-hospital cost and median cost per endpoint event. Therefore, the patient’s follow-up costs are calculated by multiplying the median cost of each endpoint event and the number of events. Despite some inevitable biases, the cost analysis conducted may be used as a guide to describe the real status of expenditure of triple-vessel and left-main of CAD patients in China. Second, in this observational study, the baseline characteristics of the 2 treatment groups were unmatched. This study is not a randomized controlled study, the patient’s baseline data may be disequilibrium, and the potential differences cannot be completely avoided. Considering the population size and statistical methodology, we used the inverse probability of treatment weighting methods to address confounding by observed covariates.
Footnotes
Source of support: Departmental sources
Conflict of interest
None.
References
- 1.Vieira RD, Hueb W, Hlatky M, et al. Cost-effectiveness analysis for surgical, angioplasty, or medical therapeutics for coronary artery disease: 5-year follow-up of medicine, angioplasty, or surgery study (MASS) II trial. Circulation. 2012;126(11 Suppl 1):S145–50. doi: 10.1161/CIRCULATIONAHA.111.084442. [DOI] [PubMed] [Google Scholar]
- 2.Hlatky MA, Boothroyd DB, Bravata DM, et al. Coronary artery bypass surgery compared with percutaneous coronary interventions for multivessel disease: A collaborative analysis of individual patient data from ten randomised trials. Lancet. 2009;373(9670):1190–97. doi: 10.1016/S0140-6736(09)60552-3. [DOI] [PubMed] [Google Scholar]
- 3.Viana MDS, Lopes F, Cerqueira Junior AMDS, et al. Incremental prognostic value of the incorporation of clinical data into coronary anatomy data in acute coronary syndromes: SYNTAX-GRACE score. Arq Bras Cardiol. 2017;109(6):527–32. doi: 10.5935/abc.20170160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kappetein AP, Feldman TE, Mack MJ, et al. Comparison of coronary bypass surgery with drug-eluting stenting for the treatment of left main and/or three-vessel disease: 3-year follow-up of the SYNTAX trial. Eur Heart J. 2011;32(17):2125–34. doi: 10.1093/eurheartj/ehr213. [DOI] [PubMed] [Google Scholar]
- 5.Mohr FW, Morice MC, Kappetein AP, et al. Coronary artery bypass graft surgery versus percutaneous coronary intervention in patients with three-vessel disease and left main coronary disease: 5-year follow-up of the randomized, clinical SYNTAX trial. Lancet. 2013;381(9867):629–38. doi: 10.1016/S0140-6736(13)60141-5. [DOI] [PubMed] [Google Scholar]
- 6.Serruys PW, Unger F, Sousa JE, et al. Comparison of coronary-artery bypass surgery and stenting for the treatment of multivessel disease. N Engl J Med. 2001;344(15):1117–24. doi: 10.1056/NEJM200104123441502. [DOI] [PubMed] [Google Scholar]
- 7.Lai HM, Aronow WS, Mercando AD, et al. The impact of statin therapy on long-term cardiovascular outcomes in an outpatient cardiology practice. Med Sci Monit. 2011;17(12):CR683–86. doi: 10.12659/MSM.882126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hu S, Zheng Z, Yuan X, et al. Increasing long-term major vascular events and resource consumption in patients receiving off-pump coronary artery bypass: A single-center prospective observational study. Circulation. 2010;121(16):1800–8. doi: 10.1161/CIRCULATIONAHA.109.894543. [DOI] [PubMed] [Google Scholar]
- 9.Shaw JW, Johnson JA, Coons SJ. US valuation of the EQ-5D health states: Development and testing of the D1 valuation model. Med Care. 2005;43(3):203–20. doi: 10.1097/00005650-200503000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Yang D, Dalton JE. SAS Global Forum 2012: Statistics and Data Analysis. 2012. A unified approach to measuring the effect size between two groups using SAS®; pp. 335–2012. [Google Scholar]
- 11.Hernandez AF, Mi X, Hammill BG, et al. Associations between aldosterone antagonist therapy and risks of mortality and readmission among patients with heart failure and reduced ejection fraction. JAMA. 2012;308(20):2097–107. doi: 10.1001/jama.2012.14795. [DOI] [PubMed] [Google Scholar]
- 12.Curtis LH, Hammill BG, Eisenstein EL, et al. Using inverse probability-weighted estimators in comparative effectiveness analyses with observational databases. Med Care. 2007;45(10 Suppl 2):S103–7. doi: 10.1097/MLR.0b013e31806518ac. [DOI] [PubMed] [Google Scholar]
- 13.Cohen DJ, Lavelle TA, Hout BV, et al. Economic outcomes of percutaneous coronary intervention with drug-eluting stents versus bypass surgery for patients with left main or three-vessel coronary artery disease: One-year results from the SYNTAX trial. Catheter Cardiovasc Interv. 2012;79(2):198–209. doi: 10.1002/ccd.23147. [DOI] [PubMed] [Google Scholar]
- 14.Javanbakht M, Bakhsh RY, Mashayekhi A, et al. Coronary bypass surgery versus percutaneous coronary intervention: Cost-effectiveness in Iran: A study in patients with multivessel coronary artery disease. Int J Technol Assess Health Care. 2014;30(04):366–73. doi: 10.1017/S0266462314000439. [DOI] [PubMed] [Google Scholar]
- 15.Thibaut C, Sandrine K, Catherine S, et al. Treatment for stable coronary artery disease: A network meta-analysis of cost-effectiveness studies. PLos One. 2014;9(6):e98371. doi: 10.1371/journal.pone.0098371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vieira RD, Hueb W, Hlatky M, et al. Cost-effectiveness analysis for surgical, angioplasty, or medical therapeutics for coronary artery disease: 5-year follow-up of medicine, angioplasty, or surgery study (MASS) II trial. Circulation. 2012;126(11 Supp1.):S145–50. doi: 10.1161/CIRCULATIONAHA.111.084442. [DOI] [PubMed] [Google Scholar]
- 17.Tanihata S, Nishigaki K, Kawasaki M, et al. Outcomes of patients with stable low-risk coronary artery disease receiving medical-and PCI-preceding therapies in Japan. Circ J. 2006;70(4):365–69. doi: 10.1253/circj.70.365. [DOI] [PubMed] [Google Scholar]
- 18.Velazquez EJ, Williams JB, Yow E, et al. Long-term survival of patients with ischemic cardiomyopathy treated by coronary artery bypass grafting versus medical therapy. Ann Thorac Surg. 2012;93(2):523–30. doi: 10.1016/j.athoracsur.2011.10.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sculpher M, Smith D, Clayton T, et al. Coronary angioplasty versus medical therapy for angina. Health service costs based on the second Randomized Intervention Treatment of Angina (RITA-2) trial. Eur Heart J. 2002;23(16):1291–300. doi: 10.1053/euhj.2001.3075. [DOI] [PubMed] [Google Scholar]
- 20.Weintraub WS, Barnett P, Chen S, et al. Economics methods in the clinical outcomes utilizing percutaneous coronary revascularization and aggressive guideline-driven drug evaluation (COURAGE) trial. Am Heart J. 2006;151(6):1180–85. doi: 10.1016/j.ahj.2005.07.035. [DOI] [PubMed] [Google Scholar]
- 21.Hlatky MA, Boothroyd DB, Melsop KA, et al. Economic outcomes of treatment strategies for type 2 diabetes mellitus and coronary artery disease in the Bypass Angioplasty Revascularization Investigation 2 Diabetes trial. Circulation. 2009;120(25):2550–58. doi: 10.1161/CIRCULATIONAHA.109.912709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hlatky MA, Rogers WJ, Johnstone I, et al. Medical care costs and quality of life after randomization to coronary angioplasty or coronary bypass surgery. Bypass Angioplasty Revascularization Investigation (BARI) Investigators. N Engl J Med. 1997;336(2):92–99. doi: 10.1056/NEJM199701093360203. [DOI] [PubMed] [Google Scholar]
- 23.Magnuson EA, Farkouh ME, Fuster V, et al. Cost-effectiveness of percutaneous coronary intervention with drug eluting stents versus bypass surgery for patients with diabetes mellitus and multivessel coronary artery disease: results from the FREEDOM trial. Circulation. 2013;127(7):820–31. doi: 10.1161/CIRCULATIONAHA.112.147488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hlatky MA, Boothroyd DB, Melsop KA, et al. Medical costs and quality of life 10 to 12 years after randomization to angioplasty or bypass surgery for multivessel coronary artery disease. Circulation. 2004;110(14):1960–66. doi: 10.1161/01.CIR.0000143379.26342.5C. [DOI] [PubMed] [Google Scholar]
- 25.Abizaid A, Costa MA, Centemero M, et al. Clinical and economic impact of diabetes mellitus on percutaneous and surgical treatment of multivessel coronary disease patients: Insights from the Arterial Revascularization Therapy Study (ARTS) trial. Circulation. 2001;104(5):533–38. doi: 10.1161/hc3101.093700. [DOI] [PubMed] [Google Scholar]
- 26.Cohen DJ, Lavelle TA, Van Hout B, et al. Economic outcomes of percutaneous coronary intervention with drug-eluting stents versus bypass surgery for patients with left main or three-vessel coronary artery disease: One-year results from the SYNTAX trial. Catheter Cardiovasc Interv. 2012;79(2):198–209. doi: 10.1002/ccd.23147. [DOI] [PubMed] [Google Scholar]
- 27.Weintraub WS, Mahoney EM, Zhang Z, et al. One-year comparison of costs of coronary surgery versus percutaneous coronary intervention in the stent or surgery trial. Heart. 2004;90(7):782–88. doi: 10.1136/hrt.2003.015057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weintraub WS, Boden WE, Zhang Z, et al. Cost-effectiveness of percutaneous coronary intervention in optimally treated stable coronary patients. Circ Cardiovasc Qual Outcomes. 2008;1(1):12–20. doi: 10.1161/CIRCOUTCOMES.108.798462. [DOI] [PubMed] [Google Scholar]
- 29.Farkouh ME, Domanski M, Sleeper LA, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med. 2012;367(25):2375–84. doi: 10.1056/NEJMoa1211585. [DOI] [PubMed] [Google Scholar]
- 30.Yang M, Xiao LB, Gao ZS, et al. Clinical effect and prognosis of off-pump minimally invasive direct coronary artery bypass. Med Sci Monit. 2017;23:1123–28. doi: 10.12659/MSM.902940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guerre P, Laaboub N, Colin C, et al. Quality assessment of reporting of economic evaluation in cardiac sugery: Has it improved? Int J Technol Assess Health Care. 2019;35(1):45–49. doi: 10.1017/S0266462318003768. [DOI] [PubMed] [Google Scholar]
- 32.Ardati AK, Cohen DJ. Transradial percutaneous coronary intervention: works great! less billing! Circ Cardiovasc Qual Outcomes. 2018;11(5):e004667. doi: 10.1161/CIRCOUTCOMES.118.004667. [DOI] [PubMed] [Google Scholar]


