Abstract
A 52-year-old female presented with an asymptomatic cyst-like lesion on her right labia majora present for several years. Excision revealed a 3-mm cystic lesion containing complex networks of thin fronds of clear apocrine cells and basaloid cells, features characteristic of hidradenoma papilliferum (HP). In contrast to the medical literature, the lesion was connected to the overlying epithelium by a straight duct, a feature characteristic of apocrine glands. Searching of six different dermatopathology study sets revealed 11 cases diagnosed as HP. Histological review of the eight available cases for review revealed none that were diagnosed correctly. Six were syringocystadenoma papilliferum and two were trichoepithelioma. HP is a fascinating lesion that needs further study and requires better diagnostic criteria.
KEY WORDS: Hidradenoma papilliferum, labia majora, syringocystadenoma papilliferum, trichoepithelioma
Introduction
Hidradenoma papilliferum (HP) is a rare, benign tumor of apocrine gland that typically presents in the anogenital region of 30–49-year-old females.[1] Clinically, HP presents as an isolated dermal or subcutaneous nodule, said to have no connection to the epidermis.[2] Interestingly, the lack of communication with the overlying epithelium is accepted by some as criterion for diagnosis.[2] Histologically, HP is a cystic lesion that presents with tall, papillary fronds, and tubules.[1] The bilayered epithelium is composed of an outer myoepithelial layer and an inner columnar layer with decapitation secretion.[1] HP has estrogen and progesterone receptors, possibility providing an explanation for its female prevalence.[3] Treatment is surgical excision.[4] We here, report a case histologically and a search of similar past cases gave rise to pathological fallacies related to the condition.
Case Report
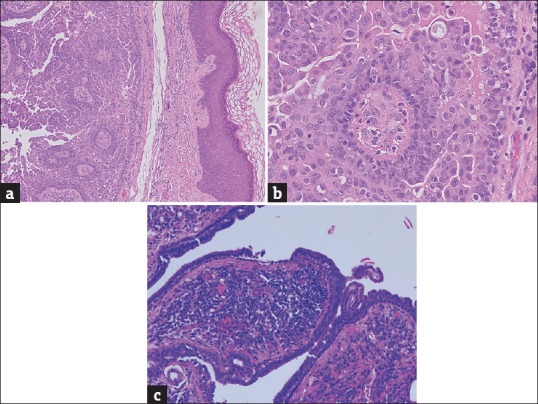
A 52-year-old Caucasian woman presented with an asymptomatic 3-mm cystic lesion on the right labia majora of several years duration. Excision was carried out [Figure 1a-c]. The patient was well with no complaints following the procedure. Histologically, the lesion was composed of complex thin fronds of relatively clear cells showing apocrine “decapitation” secretion and basaloid cells. There was a clear connection to the overlying epidermis via a duct with no spiraling, indicative of apocrine duct changes [Figure 1a-c].
Figure 1.

(a) Case 1: Hidradenoma papilliferum: 3-mm asymptomatic lesion on the labium majora of a 52-year-old female (H and E, ×24). (b) Case 1. Hidradenoma papilliferum: Higher power view showing thin strands of relatively clear cells with sparse stroma (the “papilliferum” component of the lesion). Note the apocrine (“decapitation”) secretion of the cells (H and E, ×240). (c) Case 1. Hidradenoma papilliferum: View shows clearly that the tumor is connected to the epidermis (H and E, ×60)
A search of 142,966 cases in six different medical center databases was performed to investigate the frequency of HP. Eleven cases were found in the database as HP, with eight cases available for histological analysis. All the eight diagnosed cases were mislabeled, with reanalysis showing six cases of syringocystadenoma papilliferum [Figure 2a-c] and two of trichoepithelioma [Figure 3a-c]. Of the six syringocystadenoma papilliferum cases, three arose in the axilla and three in the perineum. The syringocystadenoma papilliferum cases from the axilla and perineum comprise one female and two males in each group.
Figure 2.
(a) An example of a syringocystadenoma papilliferum found in a dermatopathology reference file mislabeled as hidradenoma papilliferum. This lesion was from the perineum of a 49-year-old female. The lesion was asymptomatic. Note the bulbous shape of the papillae and their abundant stroma in contrast to the thin stromas of the hidradenoma papilliferum seen in Figures 1a and b. Note the apocrine secretion and the denser appearance of the cells than in Figures 1a and b. Note also the absence of an inflammatory infiltrate in the stroma of these papillae (H and E, ×60). (b) Same case as in Figure 2a, high-power view. Again note the absence of an inflammatory infiltrate within the papilla shown (H and E, ×240). (c) An example of a syringocystadeoma papilliferum occurring in a nevus sebaceous of Jadassohn. Note the intense infiltrate of plasma cells in the papilla shown (H and E, ×120)
Figure 3.

(a) Trichoepithelioma. Note the basophilic cells in which are imbedded collagenous structures resembling immature hair papillae. These changes are diagnostic of this entity (H and E, ×100). (b) Trichoepithelioma combined with hair follicle lining epithelium, producing a cyst-like structure (H and E, ×80). (c) Trichoepithelioma combined with hair follicle lining epithelium, producing a papillary structure with diagnostic changes of trichoepithelioma projecting into a cyst-like structure composed of hair follicular epithelium (H and E, ×60)
Discussion
Syringocystadenoma papilliferum is a benign hamartomatous apocrine tumor that may appear as a solitary plaque or as one or multiple papules.[5,6] This tumor is most commonly associated with the nevus sebaceous of Jadassohn.[7] A review of 145 cases found this tumor presents in the head and neck region (75%), trunk (20%), or extremities (5%).[6,7] Surgical excision is the primary method of treatment, either to remove the small risk of malignant transformation or to address a cosmetic concern.[5]
Syringocystadenoma papilliferum is diagnosed histopathologically, as clinical examination is not sufficient.[5] Histologically, syringocystadenoma papilliferum presents as a cystic lesion with papillary rounded cabbage-like fronds. The bilayered epithelium is made of an outer layer of cuboidal cells and an inner layer of columnar cells with decapitation secretion.[7]
Syringocystadenoma papilliferum tumors arising in sebaceous of Jadassohn are usually exposed to the outside environment. This outside exposure contributes to the secondary histological changes. The most prominent of these is an infiltrate of overmature plasma cells that fill the characteristic cabbage-like fronds within the tumor [Figure 2c]. These secondary changes are, therefore, commonly noted on histological examination and are considered by some to comprise part of the definition of a syringocystadenoma papilliferum. However, this is an incorrect notion.
The six cases misdiagnosed as HP that were later diagnosed as syringocystadenoma papilliferum were obtained from the axilla and perineum, two relatively rare locations that are also unexposed to the outside environment. Therefore, in these two locations, a syringocystadenoma papilliferum may present without any secondary changes, and our direct examination also showed a lack of secondary changes in these mislabeled slides [Figures 2b and c]. The lack of associated secondary changes may lead pathologists to attribute another diagnosis to the lesion. In these cases, the lesion was misdiagnosed as an HP. In addition, four of the six cases were found in males, which makes the diagnosis of HP even more unlikely.
Two cases of trichoepithelioma, both from the head, were also misdiagnosed as HP. Trichoepithelioma is a benign tumor of the hair follicle, which commonly presents on the face and scalp.[8] Histologically, trichoepithelioma shows a nodular process composed of basaloid cells within which are dermal masses showing changes characteristic of hair papillae. These changes are similar to the structure of a hair bulb. In addition, adjacent to hair bulb, the hair follicle consists of lining epithelium, and in those unusual cases in which the trichoepithelioma shows differentiation toward both processes, the nodular process described above may appear in association with a cystic process which represents hair epithelium differentiation.[8] In one case, the trichoepithelioma showed differentiation of hair bulbs and one adjacent hair follicle lining [Figure 3a and b]. The second case of trichoepithelioma showed a large cyst-like cavity into which fronds of tissue with foci of hyaline and basaloid cells, diagnostic of trichoepithelioma, projected [Figure 3c]. These histological presentations gave the trichoepithelioma a cystic appearance, which may have been interpreted by error as HP.
We found that the current case was clearly connected to the overlying epithelium via a straight nonsyringoid duct, typical of apocrine gland. Since some authors have defined HP as not having such a duct, this paper also serves to redefine this entity. We believe that other cases have failed to show this connection because of differences in the plane of sectioning.
Altogether, we present a model histological case of a HP of the labia majora. Through our investigation, we found that HP may be commonly misdiagnosed in dermatopathology. Due to this misdiagnosis, HP may currently have an overrepresented and misrepresented prevalence in dermatopathology.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Kambil SM, Bhat RM, D'Souza DC. Hidradenoma papilliferum of the vulva. Indian Dermatol Online J. 2014;5:523–4. doi: 10.4103/2229-5178.142541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nishie W, Sawamura D, Mayuzumi M, Takahashi S, Shimizu H. Hidradenoma papilliferum with mixed histopathologic features of syringocystadenoma papilliferum and anogenital mammary-like glands. J Cutan Pathol. 2004;31:561–4. doi: 10.1111/j.0303-6987.2004.00176.x. [DOI] [PubMed] [Google Scholar]
- 3.Offidani A, Campanati A. Papillary hidradenoma: Immunohistochemical analysis of steroid receptor profile with a focus on apocrine differentiation. J Clin Pathol. 1999;52:829–32. doi: 10.1136/jcp.52.11.829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duhan N, Kalra R, Singh S, Rajotia N. Hidradenoma papilliferum of the vulva: Case report and review of literature. Arch Gynecol Obstet. 2011;284:1015–7. doi: 10.1007/s00404-010-1784-7. [DOI] [PubMed] [Google Scholar]
- 5.Chandramouli M, Sarma D, Tejaswy K, Rodrigues G. Syringocystadenoma papilliferum of the scalp arising from a nevus sebaceous. J Cutan Aesthet Surg. 2016;9:204–6. doi: 10.4103/0974-2077.191656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mammino JJ, Vidmar DA. Syringocystadenoma papilliferum. Int J Dermatol. 1991;30:763–6. doi: 10.1111/j.1365-4362.1991.tb04780.x. [DOI] [PubMed] [Google Scholar]
- 7.Yap FB, Lee BR, Baba R. Syringocystadenoma papilliferum in an unusual location beyond the head and neck region: A case report and review of literature. Dermatol Online J. 2010;16:4. [PubMed] [Google Scholar]
- 8.Heller J, Roche N, Hameed M. Trichoepithelioma of the vulva: Report of a case and review of the literature. J Low Genit Tract Dis. 2009;13:186–7. doi: 10.1097/LGT.0b013e31818e0c57. [DOI] [PubMed] [Google Scholar]


