Abstract
Context
Postoperative recovery rooms have existed since 1847, however, there is sparse literature investigating interventions undertaken in recovery, and their impact on patients after recovery room discharge.
Objective
This review aimed to investigate the organisation of care delivery in postoperative recovery rooms; and its effect on patient outcomes; including mortality, morbidity, unplanned intensive care unit (ICU) admission and length of hospital stay.
Data sources
NCBI PubMed, EMBASE and Cumulative Index to Nursing and Allied Health Literature.
Study selection
Studies published since 1990, investigating health system initiatives undertaken in postoperative recovery rooms. One author screened titles and abstracts, with two authors completing full-text reviews to determine inclusion based on predetermined criteria. A total of 3288 unique studies were identified, with 14 selected for full-text reviews, and 8 included in the review.
Data extraction
EndNote V.8 (Clarivate Analytics) was used to manage references. One author extracted data from each study using a data extraction form adapted from the Cochrane Data Extraction Template, with all data checked by a second author.
Data synthesis
Narrative synthesis of data was the primary outcome measure, with all data of individual studies also presented in the summary results table.
Results
Four studies investigated the use of the postanaesthesia care unit (PACU) as a non-ICU pathway for postoperative patients. Two investigated the implementation of physiotherapy in PACU, one evaluated the use of a new nursing scoring tool for detecting patient deterioration, and one evaluated the implementation of a two-track clinical pathway in PACU.
Conclusions
Managing selected postoperative patients in a PACU, instead of ICU, does not appear to be associated with worse patient outcomes, however, due to the high risk of bias within studies, the strength of evidence is only moderate. Four of eight studies also examined hospital length of stay; two found the intervention was associated with decreased length of stay and two found no association.
PROSPERO registration number
This protocol is registered on the International Prospective Register of Systematic Reviews (PROSPERO) database, registration number CRD42018106093.
Keywords: post operative care, post anaesthetic care, recovery room, post anaesthetic care unit (PACU), anaesthetics, health services administration & management
Strengths and limitations of this study.
This is the first systematic review to provide a summary of the organisation of care delivery in recovery rooms and the impact on patient outcomes. It is a current area of interest for many hospitals/health networks, due to the frequency and cost of postoperative complications.
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement was strictly adhered to, with a broad search strategy in an attempt to capture all relevant publications.
The variation in study designs and primary outcome measures meant that we were unable to combine data for aggregate analysis or meta-analysis.
Narrative synthesis of key results may introduce bias; however, steps were taken to minimise this, including the review of all data by a second author.
Introduction
Rationale
The concept of a postoperative recovery room or postanaesthesia care unit (PACU) was first described in 1847,1 and the progression of surgical and anaesthetic techniques has seen marked advances in their form and function. However, there is a striking paucity of literature investigating the interventions undertaken in recovery, and their impact on patients after recovery room discharge. An editorial by C. Aps in 2004, discussed the concept of overnight intensive recovery; where patients can be managed in the PACU for up to 24 hours,2 to avoid unnecessary intensive care unit (ICU) admissions and decrease cancellations due to lack of bed availability. This concept was introduced in the 1990s at St Thomas’ Hospital, London2; and despite its apparent success, has not spawned further research surrounding such a model of care. Swart et al retrospectively examined the impact of the loss of access to a high-dependency unit (HDU) for postoperative management of medium risk patients, and showed a significant increase in emergency laparotomies and unplanned critical care admissions.3 However, the use of HDU for postoperative patients has also been associated with an increase in postoperative respiratory complications.4 The concept of extended 6-hour recovery, followed by a monitored ward bed instead of an elective ICU admission postoperatively, has also shown to be safe, with no worsening in patient outcomes.5 This review focuses on health services research, also known as health systems research; investigating models of care delivery, rather than single therapeutic interventions. Health systems research is a multidisciplinary field that examines access to, and the use, cost, quality, delivery, organisation, financing and outcomes of healthcare services. This is used to identify new knowledge about the structure, processes and effect of health systems for individuals and populations.6 This is the first systematic review to provide a summary of the organisation of care delivery in recovery, and its impact on patient outcomes after recovery room discharge. In presenting these finding, we hope to highlight the need for further research to help improve the care of patients in the postoperative period.
Objectives
The objective of this systematic review was to investigate any health system initiatives undertaken in operating suite recovery rooms, in the postoperative period, that have been shown to improve outcomes after PACU discharge, for adult, non-cardiac surgical patients. Important outcomes included mortality, morbidity, return to theatre, unplanned ICU admission and length of hospital stay. Prospective and retrospective randomised control trials, cohort studies, case–control studies and comparison studies were included for analysis.
Methods
Protocol and registration
A review protocol was developed in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement by the author team prior to commencing the systematic review. This protocol is registered on the International Prospective Register of Systematic Reviews (PROSPERO) database, registration number CRD42018106093.
Patient and public involvement
As this is a systematic review of pre-existing literature, patients and the public were not involved in study design. However, this systematic review forms part of a broader research topic on postoperative care, and how to face the challenge of increasing postoperative complication rates. In 2012, the WHO estimated the global volume of surgery to be 312.9 million operations, an increase of 38.2% compared with 2004, resulting in a mean global surgical rate of 4469 operations per 100 000 people per year.7 With an ageing population and increasing prevalence of comorbidities, postoperative complications are now at pandemic levels.8 Investigating alternative healthcare systems and care delivery models is paramount to combatting this issue. It should be a priority for both patients and service providers, as it has the potential to provide great benefit to the broader population.
Eligibility criteria
Included studies investigated health system initiatives in the PACU, in the postoperative period, up to 48 hours postoperatively. Adult patient groups were the primary focus, however, studies that included a small cohort of children were not automatically excluded. Studies that explored the relationship between interventions in recovery and mortality, morbidity, hospital length of stay, unplanned ICU admission and return to theatre were included. Varying study designs were eligible for inclusion; such as randomised control trials, cohort studies, case–control studies and before and after studies. Cross-sectional studies and case reports were excluded. Only studies published from 1990 onwards were included, to focus on up to date clinical practice and minimise the inclusion of irrelevant data. Studies published in a language other than English, grey literature and studies focusing solely on ambulatory surgery were excluded.
Information sources and search strategy
Medical Subject Heading terms were generated from the NCBI (National Center for Biotechnology Information) PubMed advanced search area with the assistance of the University of Adelaide Health Sciences librarian. Logic grids were used as a tool, to replicate the search throughout the three databases; NCBI PubMed, EMBASE and Cumulative Index to Nursing and Allied Health Literature. The full electronic search strategy for the PubMed database is presented in online supplementary appendix 1. This search strategy was used across the three databases from 23 March 2018 to 8 April 2018 to yield the articles screened for inclusion in the review.
bmjopen-2018-027262supp001.pdf (20.6KB, pdf)
Study selection
Search results from each data base were recorded, and imported into EndNote V.8 (Clarivate Analytics, Boston, USA). Key word searching was also performed to identify new studies that had not yet been assigned indexing terms for the databases. Reference lists from key articles were also reviewed to identify further papers that may have been relevant to the review. Titles and abstracts were screened by one reviewer (CL), who was not blinded to journal titles or to the study authors or institutions. Articles selected for full-text review were reviewed by two reviewers (CL and GL), and any discrepancies arising regarding the relevance of a study were resolved by consulting a third party. The list of references for inclusion was sent to all authors to ensure consensus.
Data collection process
The Cochrane Data Extraction Template for Included Studies from their consumers and communication page was used as a base for our data extraction form. This form was piloted on two initial studies for usability, with no further modifications required. One reviewer extracted the initial data from each study (CL), and these data were confirmed by a second reviewer (GL) before inclusion in the review. One study only included data in pictorial form, and an attempt was made to contact the authors to obtain the raw data. Unfortunately, this was unsuccessful.
Data items
Data items extracted from each study included patient population and characteristics, intervention aims and methods, comparison groups and outcome measures. These data items are presented in the Characteristics of Included Studies Tables.
Risk of bias in individual studies
Risk of bias in individual studies was assessed by two reviewers (CL and GL) using Gate-Lite and Robins-I (previously known as A Cochrane Risk of Bias Assessment Tool: for Non-Randomized Studies of Interventions). Narrative synthesis of data placed more weight on higher quality studies; however, all studies and their results are presented, with caveats to highlight the individual biases that will affect interpretations of results.
Summary measures and planned methods of analysis
Narrative synthesis of data was the principle summary measure. This was due to the differing study designs and variable outcome measures in each study. Meta-analysis was not appropriate for the data in this systematic review. All data are presented individually, in relation to each study, with further narrative synthesis to summarise results. Results from studies were unable to be combined due to the variation in primary and secondary outcome measures, and differences in study design. No additional analysis or subgroup analysis was performed during this systematic review.
Risk of bias across studies
Risk of bias across studies was assessed by two reviewers (CL and GL), using the Cochrane Risk of Bias Tool, and discussing any evident publication bias or selective reporting.
Results
Study selection
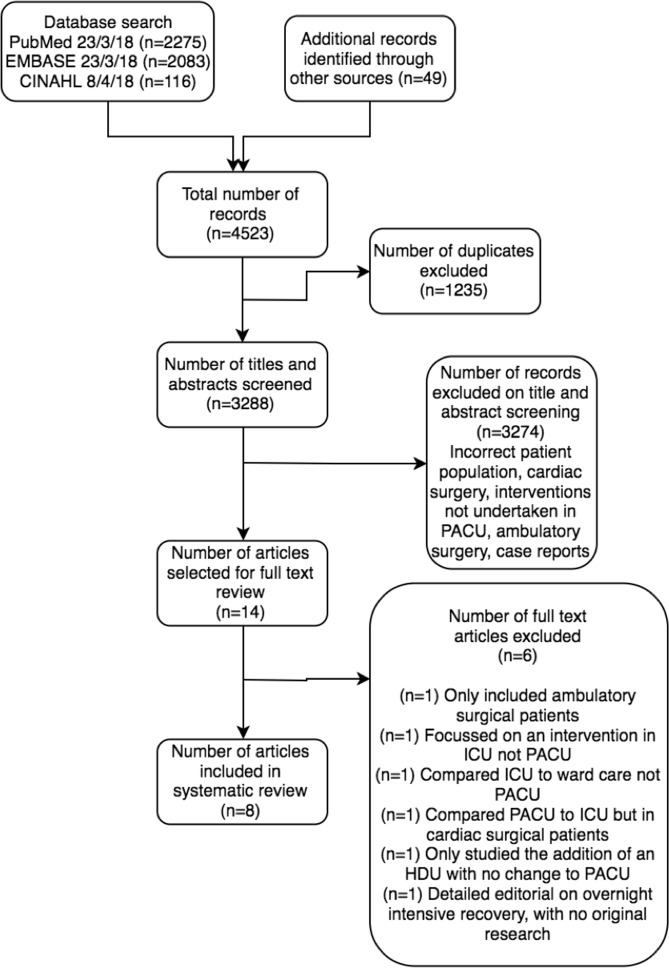
Database results and numbers of studies screened are presented in the flow diagram (figure 1). All references were imported into EndNote V.8 for title and abstract screening. One reviewer (CL) screened all titles and abstracts, with ambiguous studies included for full text review. Fourteen studies were selected for full-text review. Full-text reviews were completed by two reviewers (CL and GL), and eight studies were selected for inclusion in the review. A summary of included and excluded studies was sent to the third and fourth authors for consensus.
Figure 1.
Flow diagram for selection of studies included in review. ICU, intensive care unit; PACU, post anaesthesia care unit.
Study characteristics
Of the eight studies included, four of the included studies were retrospective cohort studies,9–12 two were observational cohort studies,13 14 one was a prospective non-randomised pre–post intervention study15 and one was a prospective randomised cohort study.16 Study characteristics for each of the included studies are outlined in the Characteristics of Included Studies Summary Table (table 1). Four studies investigated the use of PACU as a non-ICU pathway for postoperative patients.9 11 13 14 Two investigated the implementation of physiotherapy in PACU, and the impact on patient outcomes.12 16 One evaluated the use of a new nursing scoring tool, and its impact on recognition of patient deterioration in PACU,15 and one evaluated the implementation of a two-track clinical pathway in PACU and the effect on patient outcomes.10 All studies focused primarily on adults, but one included a small cohort of children.11 Common outcome measures included in-hospital mortality, PACU length of stay and hospital length of stay. Further details regarding patient population characteristics, study methodology and outcome measures are also outlined in the supplementary tables published online (online supplementary file).
Table 1.
Characteristics of included studies summary table
| Source | Aim | Study design | Number of arms/groups | Population | Intervention | Comparison group | Outcome measures |
| Callaghan et al9 (n=178) |
To determine the safety of introducing non-ICU pathways for selected patients. And evaluate the effect on cost, ICU beds availability and cancellation rates of elective surgery. | Retrospective cohort study. | Intervention group: patients selected for OIR. Comparison group: patients booked for an elective ICU admission. | All patients undergoing elective open aortic surgery between 1 January 1998 and 31 December 2002. | (n=152) Introduction of OIR |
(n=26) Elective postoperative ICU bed |
In-hospital mortality In-hospital morbidity Postoperative length of stay ICU length of stay |
| Eichenberger et al10 (n=6375) |
To assess the impact of a clinical pathway implemented in a postanaesthesia care unit on postoperative outcomes. | Retrospective cohort study based on electronic patient records. | Fast track: nurse driven, ASA 1–2. Slow track: physician driven, ASA 3–5 who have undergone minor or major surgery, or developed postoperative complications. Comparison group: Pre-existing PACU conditions without the clinical pathway. |
All elective and non-elective inpatients, who underwent a surgical or endoscopic procedure under anaesthesia during the study period. | (n=3345) Introduction of a two-track clinical pathway that clearly defined and coordinated medical and nursing interventions. |
(n=3030) Pre-existing PACU conditions without the clinical pathway. |
PACU length of stay In-hospital mortality Unplanned ICU admissions after PACU stay. |
| Fraser and Nair13 (n=119) |
To assess if elective surgical patients were stable enough to return to the general ward after a stay in Extended Recovery instead of being routinely admitted to ICU. | Observational cohort study. | One arm. No control group | Elective surgical patients who would have previously been booked for level two care postoperatively. | (n=119) Opening of an extended recovery unit. |
Nil | Discharge destination after extended recovery unit admission |
| Kastrup et al11 (n=51 090) |
To evaluate the effect of around-the-clock intensivist PACU coverage on the structure of ICU, and to demonstrate the economic effect on the hospital. | Retrospective cohort study. | Intervention group: after the introduction of 24 hours intensivist coverage. Comparison group: prior to introduction of 24 hours intensivist coverage. | All patients undergoing a surgical procedure (adults and children) between 1 January 2008 and 30 April 2011. | (n=26 118) Introduction of 24 hours intensivist coverage in PACU |
(n=24 972) Pre-existing PACU with no intensivist coverage |
PACU LOS ICU LOS Preoperative days Hospital LOS Casemix index Cost |
| Schweizer et al14 (n=933) |
To assess the impact of a new PACU on ICU utilisation, hospital length of stay and complications following major non-cardiac surgery. | Observational cohort study. | Intervention group: after opening of a new PACU. Control group: before opening of the new PACU | Adult patients undergoing abdominal aortic reconstruction or resection of lung cancer during the study periods. | (n=485) Opening of a new PACU (PACT) |
(n=448) Pre-existing PACU |
Mortality Reoperation Secondary admission to ICU Postoperative complications Hospital LOS |
| Street et al15 (n=1417) |
To evaluate whether use of a discharge criteria tool for nursing assessment of patients in PACU would enhance nurses' recognition and response to patients at-risk of deterioration and improve patient outcomes. | Prospective non-randomised pre–post intervention study. | Intervention group: after the implementation of the Postanaesthetic Care Tool (PACT) Comparison group: prior to the implementation of PACT. |
All adult patients undergoing elective surgery on days of data collection. | (n=694) Implementation of a PACT |
(n=723) Standard PACU care without PACT |
Nursing management of symptoms Rates of adverse events Mortality PACU LOS Hospital LOS Health service usage and healthcare costs |
| Tayrose et al12 (n=900) |
To address the impact of rapid rehabilitation beginning in the recovery room on length-of-stay after primary hip and knee arthroplasty. | Retrospective cohort study. | Intervention group: rapid rehabilitation group. Comparison group: standard rehabilitation protocol |
900 consecutive hip and knee arthroplasty patients. | (n=331) Rapid rehabilitation pilot programme where the first two cases of the day were mobilised in the recovery room. |
(n=569) Remainder of cases received standard rehabilitation protocol starting on the morning of postoperative day one. |
Overall hospital LOS Hip arthroplasty subgroup LOS Knee arthroplasty subgroup LOS |
| Zoremba et al16 (n=60) |
To evaluate the impact of short-term respiratory physiotherapy during the PACU stay, on postoperative lung function tests and pulse oximetry values in obese adults after minor surgery. | Prospective randomised cohort study | Intervention group: physical therapy treatment group that performed incentive spirometry in the PACU Control group: patients who did not undergo physical therapy |
60 obese adult patients (BMI 30–40) ASA 2–3, scheduled for minor peripheral surgery. | (n=30) Patients performed incentive spirometry in the PACU. |
(n=30) Not instructed to do any breathing exercises or spirometry. |
Pulse oximetry and spirometry at 1, 2, 6 and 24 hours postoperatively |
ASA, American Society of Anaesthesiologists physical status classification; BMI, body mass index; ICU, intensive care unit; LOS, Length of stay; OIR, overnight intensive recovery; PACU, postanaesthesia care unit.
bmjopen-2018-027262supp002.pdf (183.8KB, pdf)
Risk of bias within studies
The overall risk of bias within studies was serious. Critical risk of bias was identified in two studies,12 13 serious risk of bias in three studies,9 14 15 moderate risk of bias in one study11 and low risk of bias in two studies.10 16 Significant patient selection and allocation bias was the most common identified cause9 11 12 14 15; as patients in these studies were not randomly allocated to their postoperative level of care. The most clinically unwell patients were sent to ICU automatically, and only the lower risk patients, as deemed by the treating teams, were allowed a trial of care in the PACU. The relatively small numbers of participants in each study, with the exception of Kastrup et al, also introduced a significant risk of bias; as these studies were not adequately powered to assess critical outcomes such as mortality and other serious postoperative complications. Articles, which were considered as being of serious and critical risk of bias, were still included in the review, due to the sparse literature available. The risk of bias summary table (table 2) provides further analysis, and comment regarding the risk of bias within individual studies.
Table 2.
Risk of bias summary table
| Source | Bias due to confounding | Bias in selection and allocation of participants | Bias in measurement of interventions | Bias due to departures from intended interventions | Bias due to missing data | Bias in measurement of outcomes | Bias in selection of reported Results | Overall risk of bias judgement | Comments |
| Callaghan et al9 | Low | Serious | Low | sModerate | Low | Moderate | Low | Serious | Significant selection bias of lower risk patients who were sent to OIR. Used predictive values for mortality (based on POSSUM variables) as a comparison measure. |
| Eichenberger et al10 | Low | Low | Low | Low | Low | Low | Low | Low | High-quality study. No specific concerns from review authors. |
| Fraser and Nair13 | Low | Moderate | Moderate | Moderate | Critical | Serious | Moderate | Critical | Over 25% of data missing. No clear objective stated, no explanation of methodology. Poorly defined selection criteria. |
| Kastrup et al11 | Low | Serious | Low | Moderate | Low | Low | Low | Moderate | Significant selection bias of patients allocated to PACU, intermediate care unit or ICU by intensive care physician. This study also included a population of children (numbers not given). |
| Schweizer et al14 | Critical | Serious | Low | Low | Low | Low | Low | Serious | Introduction of preoperative risk assessment guidelines (AHA/ACC) with increased antiadrenergic administration preoperatively confounds results. Significant selection bias, no admission criteria stated for PACU or ICU. Patient allocation was determined by treating clinician. |
| Street et al15 | Low | Serious | Low | Moderate | Low | Serious | Critical | Serious | Power analysis included all patients (including day surgery) when investigating postoperative outcomes after PACU discharge, giving inaccurate results. Poor objective (with different objectives stated in the abstract and the article). |
| Tayrose et al12 | Low | Critical | Serious | Moderate | Low | Serious | Low | Critical | Patients who were deemed too unwell to be mobilised in recovery, were included in analysis for the standard recovery group. Operative order bias, by including the first two cases of the day. No methods reported for data collection. |
| Zoremba et al16 | Low | Low | Low | Low | Low | Low | Low | Low | Good-quality study. However, does not address the longer-term outcomes of interest. |
ACC, American College of Cardiology; AHA, American Heart Association; ICU, intensive care unit; PACU, postanaesthesia care unit; POSSUM, Physiological and operative severity score for the enumeration of mortality and morbidity.
Results of individual studies
The results of each individual study are presented in the results of included studies table (table 3). Four studies9 11 13 14 investigated non-ICU pathways for care of postoperative patients, and these pathways were not associated with increased mortality rates in three of the included studies.9 11 14 However, it must be noted that due to sample size, only one study11 was adequately powered to show a reliable difference in mortality rates, and one study13 did not investigate mortality as an outcome measure. Admission criteria for PACU care instead of ICU care postoperatively were only stated in two of the included studies.9 11 Callaghan et al outlined contraindications to use of overnight intensive recovery; including significantly impaired renal function, technically difficult or prolonged surgery expected, poor exercise tolerance or likelihood of requiring postoperative ventilation. However, the selection of patients was ultimately at the discretion of the attending anaesthetist and vascular surgeon. Kastrup et al only listed planned length of stay <24 hours as their admission criteria to PACU instead of ICU or the intermediate care unit. Fraser et al did not mention their admission criteria for extended recovery care,13 and Schweizer et al admitted patients to PACU instead of ICU purely at the discretion of the attending anaesthetist.14 Four of eight studies also examined hospital length of stay,9 11 12 14 and two found the intervention was associated with decreased length of stay and two found no association (table 3). Kastrup et al demonstrated a significant decrease in length of stay for all surgical patients after their introduction of 24 hours intensivist coverage to the PACU.11 Tayrose et al also demonstrated a decreased length of stay for patients who received early mobilisation in PACU.12 However, Callaghan et al and Schweizer et al did not demonstrate any statistically significant decrease in length of stay.9 14 PACU length of stay was another common outcome measure in three of the included studies.10 11 15 Eichenberger et al demonstrated a decreased PACU length of stay for ASA (American Society of Anaesthesiologists physical status classification) 1–2 patients, but no difference for ASA3-5, while Kastrup et al and Street et al both demonstrated an increase in PACU length of stay following their interventions.11 15 Due to the variations in study designs, we were unable to combine the data for further aggregate analysis.
Table 3.
Results of included studies
| Source | Intervention | Mortality | Other key results |
| Callaghan et al9 | Introduction of overnight intensive recovery | No significant difference between groups. Overall in hospital mortality was 2%. fewer than predicted patients died (observed mortality 3 vs predicted 95% CI 8 to 21). | Morbidity: No significant difference between groups. Overall, fever than predicted patients experienced one or more complications (observed 101 vs predicted morbidity 103%–125% 95% CI) Hospital length of stay: No significant difference between groups |
| Eichenberger et al10 | Introduction of a two-track clinical pathway that clearly defined and coordinated medical and nursing interventions. | Overall in-hospital mortality decreased significantly from 68 patients (1.5%) to 39 patients (0.8%) (p<0.001). In ASA 3–5 patients, mortality was nearly halved (adjusted OR 0.40) (p<0.001). | Unplanned ICU admission: Total number of unplanned ICU admissions after stay in PACU decreased from 113 (2.5%) to 90 (1.9%) (adjusted OR 0.70) (p=0.70) PACU length of stay: After adjustment for differenced in patients and procedures. Statistically significant decrease in PACU length of stay for ASA 1–2 patients (adjusted p<0.001). There was no difference for ASA 3–5 patients (adjusted p=0.768) |
| Fraser and Nair13 | Opening of an extended recovery unit. | Not investigated | Discharge destination after extended recovery unit admission: Data from the first 119 patients admitted to the extended recovery unit were collected. 76 patients (63.9%) who would have otherwise gone to critical care were able to go back to the ward. |
| Kastrup et al11 | Introduction of 24 hours intensivist coverage in PACU | No difference between groups | Hospital length of stay: Overall length of stay decreased significantly for all surgical patients. From 8.3 (±11.8) days to 7.71 (±10.99) days. PACU length of stay: More patients were treated in the PACU for a longer period of time. Mean LOS increased from 0.27 (±0.2) days to 0.45 (±0.41) days Cases treated in ICU: Mean number of cases treated in the ICU per month decreased significantly from 164.7 (±14.37) to 133.8 (±19.42) (p=<0.001) ICU treatment days: Mean number of treatment days per month did not change. Relative number of patients with longer LOS (>7 days) increased after introduction of PACU, whereas average number of patients staying <24 hours in the ICU decreased by ~50%. |
| Schweizer et al14 | Opening of a new PACU | No difference between study periods | Morbidity: Vascular patients had decreased rates of myocardial infarction (6.4% vs 1.3% p=0.009) and decreased rates of pulmonary oedema (5.1% vs 1.7% p=0.08) Reoperation: No difference between study periods Hospital length of stay: Total hospital length of stay did not change over time |
| Street et al15 | Implementation of a Postanaesthesia Care Tool (PACT) | No significant difference between groups. | Patient management in PACU: More requests for medical review 19% vs 30% (p=<0.001), more patients with MET criteria modified by an anaesthetist 6.5% vs 13.8% (p<0.001), higher rates of analgesia administration37.3% vs 54.2% (p=0.001). Adverse events in PACU: More adverse events recorded in PACU in phase 2, 29.4% vs 21.2% (p<0.001). May represent a greater recognition of adverse events in PACU after implementation of PACT. Adverse events after PACU: Significant decrease in rates of clinical deterioration and significant decrease in cardiovascular events after PACU discharge. PACU length of stay: Increase in median PACU length of stay from 45 min in phase 1 to 53 min in phase 2 (p<0.001) |
| Tayrose et al12 | Rapid rehabilitation pilot programme where the first two cases of the day were mobilised in the recovery room. | Not investigated | Overall hospital length of stay: Rapid rehabilitation had significantly decreased length of stay that patient who began therapy on postoperative day 1 (p<0.001). Hip arthroplasty subgroup length of stay: Decreased length of stay for rapid rehab patients in the hip arthroplasty subgroup (p<0.001). Knee arthroplasty subgroup length of stay: Decreased LOS for rapid rehab patients in the knee arthroplasty subgroup (p=0.16). |
| Zoremba et al16 | Patients performed incentive spirometry in the PACU. | Not investigated | Pulse oximetry: Significantly improved pulse oximetry values at 1 and 2 hours in PACU, and at 6 hours postmobilisations (p<0.0001), and significant improvement in pulse oximetry values at 24 hours postoperative (p<0.0001). Spirometry results: Incentive spirometry group recovered lung function faster in during the PACU stay (p<0.0001). Lung function had almost reached baseline at 6 hours in the incentive spirometry group, however, the control group were up to 25% below baseline (p<0.0001). Overall difference in lung function between groups had decreased 24 hours after surgery, but significant differences still remained (p=0.0040). |
ASA, American Society of Anaesthesiologists physical status classification; ICU, intensive care unit; LOS, Length of stay; MET, Medical emergency team; PACU, postanaesthesia care unit.
Synthesis of results
The overall quality of studies was poor, with significant selection and allocation bias; however, managing postoperative patients outside of the ICU is not associated with worse patient outcomes, especially in an extended recovery setting. There was no increase in mortality rates identified in three of the studies investigating non-ICU pathways for postoperative patients,9 11 14 and the fourth did not investigate mortality as an outcome measure.13 Use of extended recovery also meant that ward discharge was usual, bypassing the ICU.9 13 Kastrup et al showed that the addition of intensivist coverage to PACU was associated with decreased length of hospital stay, and Tayrose et al demonstrated that early mobilisation in PACU was associated with decreased length of hospital stay, but significant preselection bias for early mobilisation of arthroplasty patients confounds results.12 Other changes to the PACU environment, including the opening of a new PACU14 and introduction of overnight intensive recovery,9 did not appear to have any effect on hospital length of stay. The use of a two-track pathway for nurse-driven and physician-driven PACU management and discharge, appears to be beneficial in reducing PACU length of stay, and improving outcomes after discharge from PACU, including a significant decrease in postoperative mortality.10 However, introduction of a Post Anaesthetic Care Tool, and introduction of 24 hour intensivist coverage in PACU was associated with increased length of stay in PACU.11 15 While incentive spirometry in PACU did improve pulse oximetry values and lung function for the first 24 hours postoperatively, there were no long-term positive effects investigated or identified.16 It must be noted that the risk of bias of the included studies modifies results. Critical risk of bias was identified in two studies,12 13 serious risk of bias in three studies,9 14 15 moderate risk of bias in one study11 and low risk of bias in two studies.10 16 Only one of the included studies was adequately powered,11 and reliable conclusions cannot be drawn from single studies with such small datasets.
Risk of bias across studies and additional analyses
Risk of bias across studies for the key common outcome measures of mortality, hospital length of stay and PACU length of stay was high due to the study designs, with no level I or II evidence available. There was no additional analysis required for this review.
Discussion
Summary of evidence
Of the eight studies included in this systematic review, only one was a prospective randomised cohort study,16 and one was a prospective non-randomised pre–post intervention study.15 The rest were observational and retrospective cohort studies.9–14 There was no level I or level II evidence available for inclusion in this review. Common outcome measures identified, included mortality, hospital length of stay and PACU length of stay. Despite the poor quality of evidence, we found that managing selected higher risk postoperative patients in the PACU instead of ICU was not associated with worse outcomes,9 11 13 14 and may be associated with decreased unnecessary ICU admissions, with potential large cost savings. However, due to study types, small participant numbers, and the significant selection and allocation bias of patients within these studies, the overall strength of evidence is only moderate. Unfortunately, only two of the included studies stated the admission criteria for PACU care instead of ICU care postoperatively,9 11 making the use of this finding to guide care difficult, with further research into risk stratification of patients needed. The addition of intensivist coverage to PACU was associated with deceased hospital length of stay in one study,11 as was the rapid mobilisation of arthroplasty patients.12 However, the introduction of overnight intensive recovery and the opening of a new PACU had no effect on hospital length of stay.9 14 The introduction of a two-track clinical pathway appeared to be associated with a decreased PACU length of stay,10 however, the introduction of a Post Anaesthesia Care Tool and introduction of intensivist coverage was associated with increased PACU length of stay.11 15 Only one of the included studies was adequately powered,11 and we are unable to draw accurate conclusions from single studies with such small participant numbers. This has significant implications for future research and health resource allocation. Further studies that prospectively randomly allocate patients to a treatment arm would be of great value, however, we acknowledge that due to the risk profile and care requirements of surgical patients, this may not be possible until further safety is proven.
Limitations
The protocol development and search strategy for this review were developed in accordance with the PRISMA statement. With help from experienced health science research librarians, we attempted to ensure that all references were captured; however, it is possible that studies were missed. Due to the variation in study design and primary outcome measures, we were unable to combine data for aggregate analysis or meta-analysis. The narrative synthesis of key results may introduce bias; however, steps were taken to minimise this, including the review of all data by a second author. The most significant limitation of this systematic review was the high risk of bias within the individual studies included in the review. Selection and allocation bias, missing data, inclusion of inappropriate patient groups such as day surgery, and lack of fidelity assessment were some of the key flaws within each study. However, the thorough risk of bias assessment and its implications on reported results allows readers to interpret the data appropriately.
Conclusions
Managing selected postoperative patients in PACU instead of ICU does not appear to be associated with worse patient outcomes, however, due to study design, and the high risk of bias within studies, the strength of evidence is moderate at best. The addition of intensivist coverage to PACU and early mobilisation were associated with decreased hospital length of stay. While the use of a two-track clinical pathway decreased PACU length of stay, however, there is no evidence of this improving patients’ overall outcomes. This is the first systematic review to investigate the health system initiatives undertaken in recovery rooms and their impact on patient outcomes after PACU discharge. There is a striking paucity of literature on this topic, with very few high-quality studies; and further research is required to evaluate and improve the care of postoperative patients in the recovery room setting.
Supplementary Material
Footnotes
Contributors: CL developed the review protocol, completed all title and abstract screening, full-text reviews and data analysis. She completed the risk of bias assessment with GL. CL also drafted and revised the manuscript. GL developed the initial review question, and assisted writing the review protocol. He also completed the full-text reviews, reviewed all data of included studies and completed the risk of bias assessment with CL. He also critically appraised the draft manuscript. DS assisted with developing the initial review question, and reviewed all included articles for consensus. He also critically appraised the draft manuscript and assisted with revisions. GM reviewed all included articles for consensus, and critically appraised the manuscript. All authors have given final approval for publication. There were no other contributors.
Funding: This systematic review was undertaken as part of a Masters of Clinical Sciences with the University of Adelaide, funded by the Australian Government's Research Training Program (Commonwealth funded).
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: There was no new data produced by this research. Data extracted from the original studies is available in the online supplementary tables.
References
- 1.Zuck D. Anaesthetic and postoperative recovery rooms. Some notes on their early history. Anaesthesia 1995;50:435–8. 10.1111/j.1365-2044.1995.tb06001.x [DOI] [PubMed] [Google Scholar]
- 2.Aps C. Surgical critical care: the overnight intensive recovery (OIR) concept. Br J Anaesth 2004;92:164–6. 10.1093/bja/aeh041 [DOI] [PubMed] [Google Scholar]
- 3.Swart M, Carlisle JB, Goddard J. Using predicted 30 day mortality to plan postoperative colorectal surgery care: a cohort study. Br J Anaesth 2017;118:100–4. 10.1093/bja/aew402 [DOI] [PubMed] [Google Scholar]
- 4.Bellomo R, Goldsmith D, Uchino S, et al. A before and after trial of the effect of a high-dependency unit on post-operative morbidity and mortality. Crit Care Resusc 2005;7:16–21. [PubMed] [Google Scholar]
- 5.Katz SG, Kohl RD. Selective use of the intensive care unit after nonaortic arterial surgery. J Vasc Surg 1996;24:235–9. 10.1016/S0741-5214(96)70098-8 [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine (US) Committee on Health Services Research: Training and Work Force Issues Thaul S, Lohr KN, Tranquada RE, Health services research: opportunities for an expanding field of inquiry: an interim statement. Washington, DC: National Academies Press (US), 1994. [PubMed] [Google Scholar]
- 7.Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet 2008;372:139–44. 10.1016/S0140-6736(08)60878-8 [DOI] [PubMed] [Google Scholar]
- 8.Ludbrook G. Hidden pandemic of postoperative complications-time to turn our focus to health systems analysis. Br J Anaesth 2018;121:1190–2. 10.1016/j.bja.2018.08.011 [DOI] [PubMed] [Google Scholar]
- 9.Callaghan CJ, Lynch AG, Amin I, et al. Overnight intensive recovery: elective open aortic surgery without a routine ICU bed. Eur J Vasc Endovasc Surg 2005;30:252–8. 10.1016/j.ejvs.2005.03.004 [DOI] [PubMed] [Google Scholar]
- 10.Eichenberger A-S, Haller G, Cheseaux N, et al. A clinical pathway in a post-anaesthesia care unit to reduce length of stay, mortality and unplanned intensive care unit admission. Eur J Anaesthesiol 2011;28:859–66. 10.1097/EJA.0b013e328347dff5 [DOI] [PubMed] [Google Scholar]
- 11.Kastrup M, Seeling M, Barthel S, et al. Effects of intensivist coverage in a post-anaesthesia care unit on surgical patients' case mix and characteristics of the intensive care unit. Crit Care 2012;16:R126 10.1186/cc11428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tayrose G, Newman D, Slover J, et al. Rapid mobilization decreases length-of-stay in joint replacement patients. Bull Hosp Jt Dis 2013;71:222–6. [PubMed] [Google Scholar]
- 13.Fraser C, Nair A. Reducing critical care admissions after elective surgery by opening an extended recovery unit at the Northern General Hospital, Sheffield. Anaesthesia 2016;71:50.26444149 [Google Scholar]
- 14.Schweizer A, Khatchatourian G, Höhn L, et al. Opening of a new postanesthesia care unit: impact on critical care utilization and complications following major vascular and thoracic surgery. J Clin Anesth 2002;14:486–93. 10.1016/S0952-8180(02)00403-8 [DOI] [PubMed] [Google Scholar]
- 15.Street M, Phillips NM, Mohebbi M, et al. Effect of a newly designed observation, response and discharge chart in the post anaesthesia care unit on patient outcomes: a quasi-expermental study in Australia. BMJ Open 2017;7:e015149 10.1136/bmjopen-2016-015149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zoremba M, Dette F, Gerlach L, et al. Short-term respiratory physical therapy treatment in the PACU and influence on postoperative lung function in obese adults. Obes Surg 2009;19:1346–54. 10.1007/s11695-009-9922-7 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-027262supp001.pdf (20.6KB, pdf)
bmjopen-2018-027262supp002.pdf (183.8KB, pdf)