Abstract
Background
There was little known on how the interaction effect between obesity and current smoking affected the incidence of hypertension. The aim of this study was to investigate how body mass index (BMI) modified the effect of current smoking on the incidence of hypertension.
Methods
Data were obtained from the China Health and Nutrition Survey (CHNS). According to the WHO recommendations for Chinese people, the normal weight, overweight, and obesity were defined using the BMI cutoff values 18.5 kg/m2, 23.0 kg/m2, and 27.5 kg/m, respectively. Current smokers were defined as having smoked at least 100 cigarettes or electronic cigarettes, 20 cigars, or 20 tobacco pipes and other type of tobacco in the last 30 days preceding the survey. Hypertension was defined as systolic blood pressure (SBP)/ diastolic blood pressure (DBP) ≥ 140/90 mmHg, use of anti-hypertensive medications, or a self-reported diagnosis.
Results
This study included 12,900 subjects. There were interaction effects between obesity and current smoking in females (P = 0.030) and the 50–59 years group (P = 0.049). Current smoking was a significant predictor of incident hypertension only in the total and female populations with normal weight (HR: 1.119 and 1.274; HR 95% CI: 1.013–1.236 and 1.143–1.415; and P = 0.027 and 0.040, respectively). Stratified by age, current smoking affected the development of hypertension only in the 50–59 years subjects with the normal weight (HR: 1.356; HR 95% CI: 1.084–1.697; and P = 0.008).
Conclusions
Current smoking was a significant predictor of incident hypertension only in the female and middle-age populations with normal weight but not in the overweight and obesity as well as the younger and elder populations.
Keywords: The interaction effect, Obesity, Current smoking, The incidence of hypertension
Background
As well known, hypertension, as a main chronic disease, has been the greatest attributable risk factor for death worldwide [1]. Moreover, hypertension is considered as a common risk predictor for cardiovascular disease (CVD) and accounts for approximately 45% of global CVD morbidity and mortality [2, 3]. As a result, there were approximately 7 million hypertension-related deaths each year [4]. In China, the prevalence of hypertension increased from 14.5% in 1991 to 34.0% in 2012 among adult population [5, 6]. As a result, it is an urgent need to take measurements to prevent and control the development of hypertension.
Many previous studies have reported that there is an association of adiposity with hypertension [7–10]. As the major independent risk factors for hypertension, overweight and obesity account for approximately 65–78% of adult hypertension cases [8, 11–13]. On the other hand, smoking has been documented as a common risk factor for many chronic diseases, especially vascular dysfunction [14]. There was a well-established association of smoking with an increased risk of CVD [15, 16]. According to the World Health Organization (WHO) report, smoking is the leading cause of 1.69 million CVD-related deaths [17]. The positive relationship between smoking and hypertension is also well established [18–21]. However, many previous studies reported that there was a long-run effect of smoking cessation on the weight gain [22, 23]. Evenly, there were some economic literatures to report that smoking can reduce BMI [24–26]. Therefore, there might be an interaction effect between obesity and smoking on the risk of hypertension.
However, there was little known on how the interaction effect between obesity and smoking affected the incidence of hypertension. In this study, it could therefore be hypothesized that there was a significant interaction between obesity and current smoking on the incidence of hypertension among adult population. The aim of this study was to investigate how obesity modified the effect of smoking on the incidence of hypertension.
Methods
Study design
This study was based on the China Health and Nutrition Survey (CHNS), which is an open-cohort and national project [27]. The CHNS covers nine provinces, which are representative of the economic development and public resources in China. A multistage stratified random cluster process was employed to extract four counties from each province. A detailed description of the survey design has been published elsewhere [27, 28].
Study population
This study covered all nine waves of the CHNS conducted from 1989 to 2011. The studied subjects should meet the following criterions: who were aged ≥18 years at baseline; who were with complete data on sex, weight, height, current smoking, and blood pressure. The subjects who were pregnant or lactating at the time of survey or with missing and implausible outlying data (e.g., weight > 300 kg or < 20 kg) would be excluded.
Measurement and definition of indicators
Weight and height were measured by the trained healthcare workers following standardized protocols. The detailed measurements of weight and height have been described in the previous studies [8, 29]. BMI was calculated as weight in kilograms divided by the square of height in meters. Three measurements were conducted per subject for each indicator. And the average was used to analyze.
According to the WHO recommendations for Chinese people, the normal weight, overweight, and obesity were defined using the BMI cutoff values 18.5 kg/m2, 23.0 kg/m2, and 27.5 kg/m2 [30]. Current smokers were defined as having smoked at least 100 cigarettes or electronic cigarettes, 20 cigars, or 20 tobacco pipes and other type of tobacco (such as chewing betel quid with tobacco, dipping tobacco, and snuff tobacco) in the last 30 days preceding the survey [31, 32]. Nonsmokers were defined as they had never smoked in their lifetime. Former smokers were not mentioned in this study. Current drinking was defined as intake at least 50 g alcohol daily in the last 30 days prior to the survey [33]. Physical activity was defined as no (less than one hour per week) or yes (one or more hours per week). Under calm state, blood pressure measurements were taken with 30 s intervals between cuff inflations using standard mercury sphygmomanometers [34]. Cuff size was selected according to each participant’s arm circumference. When the first and fifth Korotkoff sounds appeared, systolic blood pressure (SBP) and diastolic blood pressure (DBP) were recorded, respectively. The same measurements were conducted for three times and the average was used. Then, hypertension was defined as SBP/DBP ≥ 140/90 mmHg, use of anti-hypertensive medications, or a self-reported diagnosis of hypertension [34, 35].
Statistical analysis
Data are expressed as means ± standard deviations (SDs) for continuous variables and frequencies (percentages) for categorical variables. The differences of the baseline characteristics between the non-hypertension and hypertension groups were compared by t-tests, chi-square tests, and Wilcoxon rank sum tests for continuous normal variables, categorical variables, and ordinal variables, respectively. With hypertension as the end-event, Cox regressions were employed to examine the interaction effects between obesity and smoking as well as the associations of obesity and current smoking with the incidence of hypertension. All models adjusted for death to correct the competing risk. All Cox regression models met the proportional hazard assumption. In the adjusted models, age, sex, current drinking, physical activity, and ethnicity at baseline were adjusted. When the interaction effects appeared, the single effects of obesity and current smoking were tested using Contrast statement in Phreg procedure of SAS with Bonferroni correction for multiple comparison. All analyses were conducted using SAS 9.4 (SAS Institute Inc., Cary, NC, USA.). The two-tailed P ≤ 0.05 was taken as the statistical significance.
Results
This study included 12,900 subjects, 4307 of who were hypertensive and 8593 subjects were non-hypertensive. The average of age was 38.14 years and BMI was 21.78 kg/m2. The median of follow-up period was 8 years. The characteristics of all subjects are shown in Table 1. The differences of all characteristics between the non-hypertension and hypertension groups were significant.
Table 1.
The characteristics of all subjects at baseline
| Characteristics | All subjects (12900) | Subgroup subjects | t/χ2 | P | |
|---|---|---|---|---|---|
| Non-hypertension (8593) | Hypertension (4307) | ||||
| Age (year)a | 38.14 ± 14.31 | 35.32 ± 13.52 | 43.75 ± 14.19 | −32.320 | < 0.001 |
| BMI (kg/m2)a | 21.78 ± 2.81 | 21.49 ± 2.70 | 22.34 ± 2.95 | −15.810 | < 0.001 |
| Sex | 90.032 | < 0.001 | |||
| Male | 5885 (45.62) | 3667 (42.67) | 2218 (51.50) | ||
| Female | 7015 (54.38) | 4926 (57.33) | 2089 (48.50) | ||
| Current smoking | 153.265 | < 0.001 | |||
| No | 7369 (60.00) | 5126 (64.00) | 2243 (52.50) | ||
| Yes | 4913 (40.00) | 2884 (36.00) | 2029 (47.50) | ||
| Current drinking | 121.351 | < 0.001 | |||
| No | 7123 (57.48) | 4936 (61.05) | 2187 (50.78) | ||
| Yes | 5269 (42.52) | 3149 (38.95) | 2120 (49.22) | ||
| Ethnicity | 59.812 | < 0.001 | |||
| Han | 10,906 (84.54) | 7115 (82.80) | 3791 (88.02) | ||
| Other | 1994 (15.46) | 1478 (17.20) | 516 (11.98) | ||
| Physical activity | 12.581 | < 0.001 | |||
| No | 12,268 (95.10) | 8131 (94.62) | 4137 (96.05) | ||
| Yes | 632 (4.90) | 462 (5.38) | 170 (3.95) | ||
| Obesityb | 14.085 | < 0.001 | |||
| Normal | 9230 (71.55) | 6477 (75.38) | 2753 (63.92) | ||
| Overweight | 3181 (24.66) | 1883 (21.91) | 1298 (30.14) | ||
| Obesity | 489 (3.79) | 233 (2.71) | 256 (5.94) | ||
| Death | 5.096 | 0.024 | |||
| No | 11,935 (92.52) | 7982 (92.89) | 3953 (91.78) | ||
| Yes | 965 (7.48) | 611 (7.11) | 354 (8.22) | ||
aThese variables were analyzed using t test
bThis variable was analyzed using Wilcoxon rank sum test
Table 2 shows the interaction effect between obesity and current smoking on the incidence of hypertension. When adjusting for covariates, there were interaction effects between obesity and current smoking in the total population (P = 0.034), females (P = 0.030), and those aged 50–59 years (P = 0.049). The further analyses were conducted to identify the single effects (Table 3). Without adjusting for covariates, overweight and obesity were associated with the incidence of hypertension despite of current smoking or not (all P < 0.001). While current smoking was the risk factor of hypertension among the normal weight subjects (HR: 1.346; HR 95% CI: 1.248–1.451; and P < 0.001) and the overweight subjects (HR: 1.235; HR 95% CI: 1.105–1.380; and P < 0.001) but not among the obesity subjects (HR: 0.917; HR 95% CI: 0.705–1.192; and P = 0.516). When adjusting for covariates, the effects of overweight and obesity were consistent with the crude results. But current smoking was a significant predictor of incident hypertension only among the normal weight subjects (HR: 1.119; HR 95% CI: 1.013–1.236; and P = 0.027).
Table 2.
The interaction effect between obesity and current smoking on the incidence of hypertension
| The interaction terms | Crude | Adjusteda | ||
|---|---|---|---|---|
| β | P | β | P | |
| Total population | ||||
| obesity ×current smoking | − 0.172 | 0.001 | −0.113 | 0.034 |
| Males | ||||
| obesity ×current smoking | − 0.219 | 0.007 | − 0.089 | 0.273 |
| Females | ||||
| obesity ×current smoking | −0.406 | 0.002 | −0.280 | 0.030 |
| Aged 18–29 years | ||||
| obesity ×current smoking | −0.084 | 0.551 | −0.095 | 0.499 |
| Aged 30–49 years | ||||
| obesity ×current smoking | −0.110 | 0.180 | −0.111 | 0.180 |
| Aged 50–59 years | ||||
| obesity ×current smoking | −0.216 | 0.034 | −0.202 | 0.049 |
| Aged 60~93 years | ||||
| obesity ×current smoking | 0.115 | 0.418 | 0.120 | 0.398 |
aIn adjusted model, age, gender, current drinking, ethnicity, physical activity, and death were adjusted
Table 3.
The single effects of obesity and current smoking on the incidence of hypertension in total population
| Crude | Adjusteda | |||||
|---|---|---|---|---|---|---|
| HR | HR 95% CI | P | HR | HR 95% CI | P | |
| Overweight and nonsmoking | 2.480 | 1.870–3.288 | < 0.001 | 1.990 | 1.500–2.640 | < 0.001 |
| Obesity and nonsmoking | 3.700 | 3.148–4.349 | < 0.001 | 2.872 | 2.441–3.378 | < 0.001 |
| Overweight and current smoking | 2.276 | 1.642–3.154 | < 0.001 | 1.878 | 1.354–2.604 | < 0.001 |
| Obesity and current smoking | 3.396 | 2.792–4.131 | < 0.001 | 2.710 | 2.227–3.299 | < 0.001 |
| Current smoking and normal weight | 1.346 | 1.248–1.451 | < 0.001 | 1.119 | 1.013–1.236 | 0.027 |
| Current smoking and overweight | 1.235 | 1.105–1.380 | < 0.001 | 1.056 | 0.930–1.198 | 0.400 |
| Current smoking and obesity | 0.917 | 0.705–1.192 | 0.516 | 0.893 | 0.683–1.167 | 0.406 |
aIn adjusted model, age, sex, current drinking, ethnicity, physical activity, and death were adjusted
In Cox regression models stratified by sex, there was no interaction effect between obesity and current smoking in males. Therefore, the single effects were displayed only in females (Table 4). As adjusting for covariates, overweight and obesity were the significant predictors of hypertension despite of current smoking or not (HR: 2.726, 3.074, 2.377, and 2.681; HR 95% CI: 1.541–4.821, 2.570–3.678, 1.161–4.867, and 1.909–3.764; and P < 0.001, < 0.001, 0.018, and < 0.001, respectively). However, current smoking was associated with hypertension only in the normal weight subjects (HR: 1.274; HR 95% CI: 1.143–1.415; and P = 0.040), but not in the overweight (P = 0.851) and obesity subjects (P = 0.090).
Table 4.
The single effects of obesity and current smoking on the incidence of hypertension in females
| Crude | Adjusteda | |||||
|---|---|---|---|---|---|---|
| HR | HR 95% CI | P | HR | HR 95% CI | P | |
| Overweight and nonsmoking | 3.345 | 1.893–5.912 | < 0.001 | 2.726 | 1.541–4.821 | < 0.001 |
| Obesity and nonsmoking | 3.827 | 3.203–4.571 | < 0.001 | 3.074 | 2.570–3.678 | < 0.001 |
| Overweight and current smoking | 2.623 | 1.282–5.364 | 0.008 | 2.377 | 1.161–4.867 | 0.018 |
| Obesity and current smoking | 3.000 | 2.139–4.207 | < 0.001 | 2.681 | 1.909–3.764 | < 0.001 |
| Current smoking and normal weight | 1.864 | 1.563–2.225 | < 0.001 | 1.274 | 1.143–1.415 | 0.040 |
| Current smoking and overweight | 1.462 | 1.147–1.862 | 0.002 | 1.024 | 0.802–1.405 | 0.851 |
| Current smoking and obesity | 0.795 | 0.474–1.334 | 0.386 | 0.639 | 0.381–1.072 | 0.090 |
aIn adjusted model, age, current drinking, ethnicity, physical activity, and death were adjusted
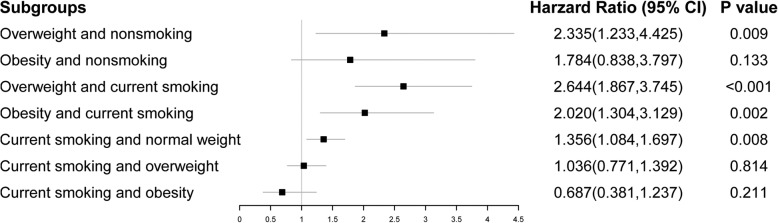
The single effects of obesity and current smoking on the incidence of hypertension in the 50–59 years group are displayed in Fig. 1. Overweight and obesity were the predictors of hypertension except in the obesity subjects with nonsmoking (HR: 1.784; HR 95% CI: 0.838–3.797; and P = 0.133). And current smoking was a predictor of hypertension only among the normal weight subjects (HR: 1.356; HR 95% CI: 1.084–1.697; and P = 0.008).
Fig. 1.
The single effects of obesity and current smoking on the incidence of hypertension in the 50–59 years group
Discussion
By now, there were few studies to investigate the interaction effect between obesity and current smoking on incident hypertension. This study was based on the CHNS, a 22-year national cohort study, and attempted to examine the interaction effect. The results implied that there were significant interaction effects between obesity and current smoking in females and the 50–59 years population. Despite of current smoking or not, obesity was a significant predictor of incident hypertension. However, current smoking was associated with hypertension only in the female and middle-aged subjects with the normal weight. When subjects were overweight or obesity, current smoking was ineffective on the incidence of hypertension.
Although previous studies reported that acute effect of smoking could temporarily raise blood pressure [17, 36, 37], several population-based studies have shown that there was no or a negative relationship between chronic smoking and hypertension [38–40]. Perhaps obesity, as a confounding factor, covered the effect of smoking. Notably, the prevalence of smoking and hypertension have been decreasing, but accompanied with a simultaneous increase in obesity [41]. As a result, the effect of smoking on hypertension might reduce or disappear but the effect of obesity on hypertension would be more significant. However, the mechanism of the interaction effect between obesity and smoking is unknown and should be further investigated in the future study.
This study showed that current smoking was a significant risk factor for hypertension in females but not in males. It was consistent with the previous studies [19, 42]. A season might be the different characteristics between males and females. The characteristics of male smokers were smoking for a long time and heavy smoking but relatively lower proportion of smokers and hypertension in females [43].
Limitations and strengths
This study was based on a 22-year follow-up national population-based cohort study. As a result, the conclusion would be more comprehensive and convictive. Furthermore, it was the first study to examine the interaction effect between obesity and current smoking on the incidence of hypertension. The results would provide a new insight for prevention and control of hypertension. However, the limitations of this study should be stated. First, in this study, smoking status was obtained according to the self-reported questionnaire. There might be misclassification error and recall bias. Second, since the information of former smoking was unavailable, the former smoking was not considered in this study. Third, since the sodium intake is not available due to the limitation of the CHNS and the family history of hypertension is not collected in the CHNS, the diet intake and the family history of hypertension were not adjusted in this study.
Conclusions
Overweight and obesity were associated with the higher incident hypertension both in the smokers and the non-smokers. However, current smoking was a significant predictor of the incidence of hypertension only in the female and middle-aged populations with the normal weight but not in the overweight and obesity as well as the younger and elder populations. Therefore, different public health interventional measurements should be made for different populations.
Acknowledgements
Not applicable.
Abbreviations
- CHNS
China Health and Nutrition Survey
- CVD
Cardiovascular disease
- SDs
Standard deviations
- WHO
World Health Organization
Authors’ contributions
YC designed the study and wrote the draft, FY revised the manuscript and improved the language, WL analyzed the data, RZ interpreted the results, and XH and GL edited and reviewed the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (81903416) and the Science and Innovation Bureau Project of Baoan District, Shenzhen (2017JD150). The funding bodies did not play roles in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript. Furthermore, we thank the National Institute for Nutrition and Health, China Center for Disease Control and Prevention, Carolina Population Center (P2C HD050924, T32 HD007168), the University of North Carolina at Chapel Hill, the NIH (R01-HD30880, DK056350, R24 HD050924, and R01-HD38700) and the NIH Fogarty International Center (D43 TW009077, D43 TW007709) for financial support for the CHNS data collection and analysis files from 1989 to 2015 and future surveys, and the China-Japan Friendship Hospital, Ministry of Health for support for CHNS 2009, Chinese National Human Genome Center at Shanghai since 2009, and Beijing Municipal Center for Disease Prevention and Control since 2011.
Availability of data and materials
The datasets analyzed during the current study are available in the China Health and Nutrition Survey (CHNS) on the site: https://www.cpc.unc.edu/projects/china.
Ethics approval and consent to participate
This study was approved by the IRB of the National Institute for Nutrition and Food Safety, China Center for Disease Control and Prevention, and University of North Carolina at Chapel Hill. All subjects provided the written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Feifei Yao and Wenfeng Liu contributed equally to this work.
References
- 1.Attard SM, Herring AH, Zhang B, Du S, Popkin BM, Gordon-Larsen P. Associations between age, cohort, and urbanization with systolic and diastolic blood pressure in China: a population-based study across 18 years. J Hypertens. 2015;33(5):948. doi: 10.1097/HJH.0000000000000522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ezzati M, Vander Hoorn S, Lawes CM, Leach R, James WPT, Lopez AD, et al. Rethinking the “diseases of affluence” paradigm: global patterns of nutritional risks in relation to economic development. PLoS Med. 2005;2(5):e133. doi: 10.1371/journal.pmed.0020133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gać P, Poręba M, Mazur G, Poręba R. The aortic mechanical properties in patients with the essential hypertension environmentally exposed to cigaret smoke. Inhal Toxicol. 2015;27(13):717–723. doi: 10.3109/08958378.2015.1103337. [DOI] [PubMed] [Google Scholar]
- 4.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ, Group CRAC Selected major risk factors and global and regional burden of disease. Lancet. 2002;360(9343):1347–1360. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 5.Wu X, Duan X, Gu D, Hao J, Tao S, Fan D. Prevalence of hypertension and its trends in Chinese populations. Int J Cardiol. 1995;52(1):39–44. doi: 10.1016/0167-5273(95)02443-Z. [DOI] [PubMed] [Google Scholar]
- 6.Li D, Lv J, Liu F, Liu P, Yang X, Feng Y, et al. Hypertension burden and control in mainland China: analysis of nationwide data 2003–2012. Int J Cardiol. 2015;184:637–644. doi: 10.1016/j.ijcard.2015.03.045. [DOI] [PubMed] [Google Scholar]
- 7.Chandra A, Neeland IJ, Berry JD, Ayers CR, Rohatgi A, Das SR, et al. The relationship of body mass and fat distribution with incident hypertension: observations from the Dallas heart study. J Am Coll Cardiol. 2014;64(10):997–1002. doi: 10.1016/j.jacc.2014.05.057. [DOI] [PubMed] [Google Scholar]
- 8.Chen Y, Liang X, Zheng S, Wang Y, Lu W. Association of body fat mass and fat distribution with the incidence of hypertension in a population-based Chinese cohort: a 22-year follow-up. J Am Heart Assoc. 2018;7(6):e007153. doi: 10.1161/JAHA.117.007153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen Y, Liang X, Zheng S, Wang Y, Lu W. The comparison of percent body fat estimated by different anthropometrics to predict the incidence of hypertension. J Hum Hypertens. 2020;34(1):51–58. doi: 10.1038/s41371-019-0240-9. [DOI] [PubMed] [Google Scholar]
- 10.Wang S, Liu Y, Li F, Jia H, Liu L, Xue F. A novel quantitative body shape score for detecting association between obesity and hypertension in China. BMC Public Health. 2015;15(1):7. doi: 10.1186/s12889-014-1334-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Garrison RJ, Kannel WB, Stokes J, 3rd, Castelli WP. Incidence and precursors of hypertension in young adults: the Framingham offspring study. Prev Med. 1987;16(2):235–251. doi: 10.1016/0091-7435(87)90087-9. [DOI] [PubMed] [Google Scholar]
- 12.Rahmouni K, Correia ML, Haynes WG, Mark AL. Obesity-associated hypertension: new insights into mechanisms. Hypertension. 2005;45(1):9–14. doi: 10.1161/01.HYP.0000151325.83008.b4. [DOI] [PubMed] [Google Scholar]
- 13.Xie D, Bollag WB. Obesity, hypertension and aldosterone: is leptin the link? J Endocrinol. 2016;230(1):F7–F11. doi: 10.1530/JOE-16-0160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li N, Li Z, Chen S, Yang N, Ren A, Ye R. Effects of passive smoking on hypertension in rural Chinese nonsmoking women. J Hypertens. 2015;33(11):2210–2214. doi: 10.1097/HJH.0000000000000694. [DOI] [PubMed] [Google Scholar]
- 15.Berry JD, Dyer A, Cai X, Garside DB, Ning H, Thomas A, et al. Lifetime risks of cardiovascular disease. N Engl J Med. 2012;366(4):321–329. doi: 10.1056/NEJMoa1012848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lloyd-Jones DM, Leip EP, Larson MG, d’Agostino RB, Beiser A, Wilson PW, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006;113(6):791–798. doi: 10.1161/CIRCULATIONAHA.105.548206. [DOI] [PubMed] [Google Scholar]
- 17.Lee Whanhee, Hwang Sung-Hee, Choi Hayoung, Kim Ho. The association between smoking or passive smoking and cardiovascular diseases using a Bayesian hierarchical model: based on the 2008-2013 Korea Community Health Survey. Epidemiology and Health. 2017;39:e2017026. doi: 10.4178/epih.e2017026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dochi M, Sakata K, Oishi M, Tanaka K, Kobayashi E, Suwazono Y. Smoking as an independent risk factor for hypertension: a 14-year longitudinal study in male Japanese workers. Tohoku J Exp Med. 2009;217(1):37–43. doi: 10.1620/tjem.217.37. [DOI] [PubMed] [Google Scholar]
- 19.Bowman TS, Gaziano JM, Buring JE, Sesso HD. A prospective study of cigarette smoking and risk of incident hypertension in women. J Am Coll Cardiol. 2007;50(21):2085–2092. doi: 10.1016/j.jacc.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 20.Niskanen L, Laaksonen DE, Nyyssönen K, Punnonen K, Valkonen V-P, Fuentes R, et al. Inflammation, abdominal obesity, and smoking as predictors of hypertension. Hypertension. 2004;44(6):859–865. doi: 10.1161/01.HYP.0000146691.51307.84. [DOI] [PubMed] [Google Scholar]
- 21.Mann SJ, James GD, Wang RS, Pickering TG. Elevation of ambulatory systolic blood pressure in hypertensive smokers: a case-control study. JAMA. 1991;265(17):2226–2228. doi: 10.1001/jama.1991.03460170080037. [DOI] [PubMed] [Google Scholar]
- 22.Flegal KM, Troiano RP, Pamuk ER, Kuczmarski RJ, Campbell SM. The influence of smoking cessation on the prevalence of overweight in the United States. N Engl J Med. 1995;333(18):1165–1170. doi: 10.1056/NEJM199511023331801. [DOI] [PubMed] [Google Scholar]
- 23.Travier N, Agudo A, May AM, Gonzalez C, Luan J, Wareham NJ, et al. Longitudinal changes in weight in relation to smoking cessation in participants of the EPIC-PANACEA study. Prev Med. 2012;54(3–4):183–192. doi: 10.1016/j.ypmed.2011.09.003. [DOI] [PubMed] [Google Scholar]
- 24.Kasteridis P, Yen ST. Smoking cessation and body weight: evidence from the behavioral risk factor surveillance survey. Health Serv Res. 2012;47(4):1580–1602. doi: 10.1111/j.1475-6773.2012.01380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kasteridis P, Yen ST. Occasional smoking and body weight among adults. Appl Econ Perspect Policy. 2014;36(3):479–503. doi: 10.1093/aepp/ppu008. [DOI] [Google Scholar]
- 26.Amialchuk A, Bornukova K, Ali MM. Will a decline in smoking increase body weights? Evidence from Belarus. East Econ J. 2018;44(2):190–210. doi: 10.1057/s41302-016-0071-0. [DOI] [Google Scholar]
- 27.Popkin BM, Du S, Zhai F, Zhang B. Cohort profile: the China health and nutrition survey—monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol. 2010;39(6):1435–1440. doi: 10.1093/ije/dyp322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhao R, Duan X, Wu Y, Zhang Q, Chen Y. Association of exposure to Chinese famine in early life with the incidence of hypertension in adulthood: a 22-year cohort study. Nutr Metab Cardiovasc Dis. 2019;29(11):1237–1244. doi: 10.1016/j.numecd.2019.07.008. [DOI] [PubMed] [Google Scholar]
- 29.Chen Y, Yang Y, Jiang H, Liang X, Wang Y, Lu W. Associations of BMI and waist circumference with all-cause mortality: a 22-year cohort study. Obesity. 2019;27(4):662–669. doi: 10.1002/oby.22423. [DOI] [PubMed] [Google Scholar]
- 30.Expert Consultation WHO. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–163. doi: 10.1016/S0140-6736(03)15268-3. [DOI] [PubMed] [Google Scholar]
- 31.Wang J, Li C, Jia C, Liu Y, Liu J, Yan X, et al. Smoking, smoking cessation and tobacco control in rural China: a qualitative study in Shandong Province. BMC Public Health. 2014;14(1):916. doi: 10.1186/1471-2458-14-916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sinha D, Palipudi K, Jones C, Khadka B, Silva P, Mumthaz M, et al. Levels and trends of smokeless tobacco use among youth in countries of the World Health Organization South-East Asia region. Indian J Cancer. 2014;51(5):50. doi: 10.4103/0019-509X.147472. [DOI] [PubMed] [Google Scholar]
- 33.Wu L, Feng X, He A, Ding Y, Zhou X, Xu Z. Prenatal exposure to the great Chinese famine and mid-age hypertension. PLoS One. 2017;12(5):e0176413. doi: 10.1371/journal.pone.0176413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chobanian AV. Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure; National Heart, Lung, and Blood Institute; National High Blood Pressure Education Program Coordinating Committee: seventh report of the joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 35.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 36.Yarlioglues M, Kaya MG, Ardic I, Calapkorur B, Dogdu O, Akpek M, et al. Acute effects of passive smoking on blood pressure and heart rate in healthy females. Blood Press Monit. 2010;15(5):251–256. doi: 10.1097/MBP.0b013e32833e439f. [DOI] [PubMed] [Google Scholar]
- 37.Schiess R, Senn O, Fischler M, Huber LC, Vatandaslar S, Speich R, et al. Tobacco smoke: a risk factor for pulmonary arterial hypertension?: a case-control study. Chest. 2010;138(5):1086–1092. doi: 10.1378/chest.09-2962. [DOI] [PubMed] [Google Scholar]
- 38.Thuy AB, Blizzard L, Schmidt MD, Luc PH, Granger RH, Dwyer T. The association between smoking and hypertension in a population-based sample of Vietnamese men. J Hypertens. 2010;28(2):245–250. doi: 10.1097/HJH.0b013e32833310e0. [DOI] [PubMed] [Google Scholar]
- 39.Wang W, Lee ET, Fabsitz RR, Devereux R, Best L, Welty TK, et al. A longitudinal study of hypertension risk factors and their relation to cardiovascular disease: the strong heart study. Hypertension. 2006;47(3):403–409. doi: 10.1161/01.HYP.0000200710.29498.80. [DOI] [PubMed] [Google Scholar]
- 40.Primatesta P, Falaschetti E, Gupta S, Marmot MG, Poulter NR. Association between smoking and blood pressure: evidence from the health survey for England. Hypertension. 2001;37(2):187–193. doi: 10.1161/01.HYP.37.2.187. [DOI] [PubMed] [Google Scholar]
- 41.Smith CY, Bailey KR, Emerson JA, Nemetz PN, Roger VL, Palumbo PJ, et al. Contributions of increasing obesity and diabetes to slowing decline in subclinical coronary artery disease. J Am Heart Assoc. 2015;4(4):e001524. doi: 10.1161/JAHA.114.001524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Burke GM, Genuardi M, Shappell H, D'Agostino RB, Sr, Magnani JW. Temporal associations between smoking and cardiovascular disease, 1971 to 2006 (from the Framingham heart study) Am J Cardiol. 2017;120(10):1787–1791. doi: 10.1016/j.amjcard.2017.07.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim BJ, Han JM, Kang JG, Kim BS, Kang JH. Association between cotinine-verified smoking status and hypertension in 167,868 Korean adults. Blood Press. 2017;26(5):303–310. doi: 10.1080/08037051.2017.1344539. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed during the current study are available in the China Health and Nutrition Survey (CHNS) on the site: https://www.cpc.unc.edu/projects/china.