Abstract
PURPOSE:
For most people, the benefits of physical activity far outweigh the risks. Research has suggested exercise preparticipation questionnaires might refer an unwarranted number of adults for medical evaluation before exercise initiation, creating a potential barrier to adoption. The new American College of Sports Medicine (ACSM) prescreening algorithm relies on current exercise participation; history and symptoms of cardiovascular, metabolic or renal disease; and desired exercise intensity to determine referral status. Our purpose was to compare the referral proportion of the ACSM algorithm to that of previous screening tools using a representative sample of US adults.
METHODS:
Based on responses to health questionnaires from the 2001–2004 National Health and Nutrition Examination Survey, we calculated the proportion of adults aged 40 years or older who would be referred for medical clearance before exercise participation based on the ACSM algorithm. Results were stratified by age and sex and compared to previous results for the ACSM/American Heart Association Preparticipation Questionnaire and the Physical Activity Readiness Questionnaire.
RESULTS:
Based on the ACSM algorithm, 2.6% of adults would be referred only before beginning vigorous exercise and 54.2% of respondents would be referred before beginning any exercise. Men were more frequently referred before vigorous exercise and women were more frequently referred before any exercise. Referral was more common with increasing age. The ACSM algorithm referred a smaller proportion of adults for preparticipation medical clearance than the previously examined questionnaires.
CONCLUSIONS:
Although additional validation is needed to determine if the algorithm correctly identifies those at risk for cardiovascular complications, the revised ACSM algorithm referred fewer respondents than other screening tools. A lower referral proportion may mitigate an important barrier of medical clearance from exercise participation.
Keywords: Population, Exercise safety, Cardiovascular screening, physician exam
Introduction
The benefits of regular participation in physical activity are well-established and consistently outweigh the risks of participation (10). Musculoskeletal injuries are the most common adverse event associated with physical activity participation, and are seldom severe (10). An individual bout of activity also carries an elevated risk of acute myocardial infarction (AMI) or sudden cardiac death (SCD). While severe, these events are rare and most commonly occur among habitually inactive people performing vigorous-intensity activity (3, 8, 10); the risk of AMI or SCD during activity is sharply attenuated by progressive, regular physical activity participation (10). Among adults, occlusive coronary artery disease is usually the underlying cause of activity-associated AMI and SCD (7). Because of this, attempts to identify adults at risk for activity associated AMI or SCD have often included cardiovascular disease (CVD) risk factor assessment (1).
The American College of Sports Medicine (ACSM) recently released an updated exercise preparticipation screening algorithm (henceforth: ACSM algorithm) that focuses on 1) the respondent’s current exercise participation 2) the presence of signs/symptoms or known history of cardiovascular diseases and 3) the desired exercise intensity, and in contrast to previous screening tools, does not assess cardiovascular risk factors (11). These changes came about in part because of indications that CVD risk factor-based screening may be overly conservative and unnecessarily refer adults for medical clearance before exercise participation (15). Using data from the 2001–2004 National Health and Nutrition Examination Survey (NHANES), the ACSM/American Heart Association Preparticipation Questionnaire (AAPQ) could potentially refer 95% of all US adults aged 40 years or older to a medical provider before beginning an exercise program (15), and 68% of US adults aged 40 years or older could be referred using the Physical Activity Readiness Questionnaire (PAR-Q) (15).
Additionally, The AAPQ and PAR-Q predate the 2008 Physical Activity Guidelines for Americans, which, like the ACSM algorithm, focus not on CVD risk factors, but on history of chronic diseases, the symptoms thereof, and current activity levels to inform the need for medical involvement (13). To date, referral estimates for the new ACSM algorithm are not available, so its performance relative to the AAPQ and PAR-Q is unknown. Therefore, the purpose of this research was to estimate the proportion of US adults aged 40 years or older that would be referred for preparticipation medical clearance using the ACSM algorithm in order to place this tool in context with previous findings.
Methods
Data Source
To ensure comparability across the three screening measures, a dataset from previous work was used that included health history interview responses from US adults aged 40 years or older from the 2001–2004 NHANES (15). Accordingly, the number of respondents and demographic characteristics of the samples are identical with the previous report (15). This dataset was limited to adults aged 40 years and older because of 1) the importance of underlying CVD as a causative factor for exercise-associated SCD and MI in adults and 2) age restrictions in many of the CVD questionnaire items in the data source. Complete information regarding NHANES methods are publically available from the Centers for Disease Control and Prevention (9) and are only summarized here. NHANES is an ongoing public health surveillance system that uses multistaged, stratified, probability sampling methods to achieve a representative sample of the US, non-institutionalized population. Among all individuals screened to participate, 84% in 2001–2002 and 79% in 2003–2004 completed questionnaires (9). Data are continuously collected and are prepared for release every two years. All NHANES data collection activities are approved by the research ethics review board of the National Center for Health Statistics and include informed consent for all participants.
Referral for medical clearance
The ACSM algorithm (Figure 1) first classifies respondents as active or inactive based on the presence or absence of exercise in the past 3 months, with exercise defined as planned, structured physical activity at least 30 min at moderate intensity on at least 3 days per week. Next, respondents are classified based on presence or absence of known cardiovascular, metabolic, or renal disease and presence or absence of signs or symptoms of these conditions (Figure 1, footnote). Recommendations for medical clearance are then made based on the desired intensity of exercise:
Figure 1: 2015 ACSM Preparticipation Screening Algorithm, reproduced with permission from Riebe, et al (11).
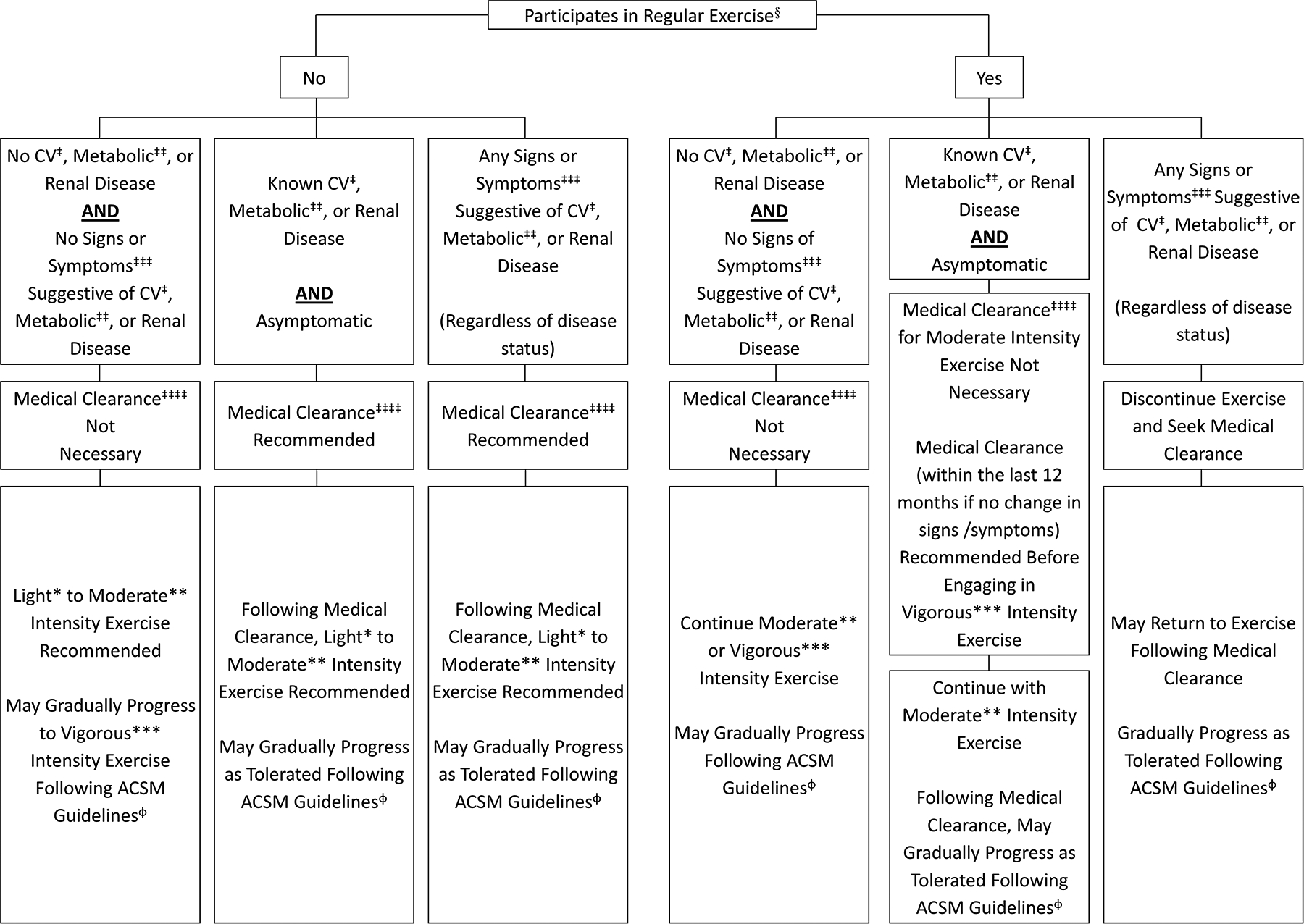
§Exercise Participation Performing planned, structured physical activity at least 30 min at moderate intensity on at least 3 d∙wk−1 for at least the last 3 months.
*Light Intensity Exercise: 30% to <40% HRR or VO2R, 2 to <3 METs, 9–11 RPE, an intensity that causes slight increases in HR and breathing
**Moderate Intensity Exercise 40% to <60% HRR or VO2R, 3 to <6 METs, 12–13 RPE, an intensity that causes noticeable increases in HR and breathing
***Vigorous Intensity Exercise ≥60% HRR or VO2R, ≥6 METs, ≥14 RPE, an intensity that causes substantial increases in HR and breathing
‡ Cardiovascular (CV) Disease Cardiac, peripheral vascular, or cerebrovascular disease.
‡‡Metabolic Disease Type 1 and 2 diabetes mellitus.
‡‡‡Signs and Symptoms At rest or during activity; includes pain, discomfort in the chest, neck, jaw, arms, or other areas that may result from ischemia; shortness of breath at rest or with mild exertion; dizziness or syncope; orthopnea or paroxysmal nocturnal dyspnea; ankle edema; palpitations or tachycardia; intermittent claudication; known heart murmur; or unusual fatigue or shortness of breath with usual activities.
‡‡‡‡Medical Clearance Approval from a healthcare professional to engage in exercise.
ɸACSM Guidelines See ACSM’s Guidelines for Exercise Testing and Prescription, 9th edition, 2014
- Among those not currently exercising:
- Asymptomatic respondents with no history of the specified diseases are recommended to begin light to moderate intensity physical exercise without clearance, and gradually progress per ACSM guidelines
- Asymptomatic respondents with a positive history of the specified diseases are recommended to seek medical clearance before beginning exercise of any intensity
- Symptomatic respondents, regardless of history, are recommended to seek medical clearance before beginning exercise of any intensity
- Among those currently exercising:
- Asymptomatic respondents with no history of the specified diseases are encouraged to continue moderate or vigorous intensity exercise without clearance, and gradually progress per ACSM guidelines
- Asymptomatic respondents with a positive history of the specified diseases are encouraged to continue light to moderate intensity exercise without clearance, but should have medical clearance before progressing to vigorous intensity exercise
- Symptomatic respondents, regardless of history, are recommended to seek medical clearance before continuing exercise of any intensity
Linking NHANES to the ACSM Algorithm, AAPQ, and PAR-Q
The health questionnaires from NHANES 2001–2004 provide much of the information needed to complete the ACSM algorithm. A matrix of algorithm components and their corresponding NHANES items is presented in Table 1. To determine current exercise participation (based on the algorithm’s definition noted previously), the weekly frequency of each selected leisure activity (bouts per week) was estimated by dividing reported monthly frequency by 4.286. The weekly frequency was then multiplied by the reported duration (minutes per bout) and NHANES-assigned metabolic equivalent value (METs), which is a measure of exercise intensity. This provided estimated weekly exercise volume in MET*minutes/week. A value of ≥270 MET*minutes/week was classified as current regular exercise (30 minutes * 3 times per week * ≥3 METs). Several items in the ACSM algorithm were not available in NHANES. Regarding CVD history, we were unable to determine if respondents had a previous diagnosis of peripheral vascular disease, but patients could report pain in the lower legs when walking, which may capture intermittent claudication. Regarding signs and symptoms of CVD, we were unable to ascertain presence of orthopnea or paroxysmal nocturnal dyspnea (PND), ankle edema, palpitations or tachycardia, murmur, or unusual fatigue. Sensitivity analyses suggested that signs and symptoms we were able to assess tended to occur jointly (few reported only one symptom). For example, of the 816 respondents that reported chest pain, fully 88% reported ≥1 additional assessed symptom; of the 2,478 that reported breathlessness, 60% reported ≥1 additional symptom. Three of five omitted symptoms relate to heart failure (orthopnea and PND, ankle edema, and unusual fatigue) and often cluster together (14), which would lessen the impact of each symptom’s omission.
Table 1:
Itemized components of the 2015 ACSM preparticipation screening algorithm and their corresponding items from the National Health and Nutrition Examination Survey, 2001–2004.
| ACSM Algorithm Item | National Health and Nutrition Examination Survey | |||
|---|---|---|---|---|
| Section | Variable | Prompt | Classification Criteria | |
| Regular Exercise | PAQIAF | PADACTIVE | Over the past 30 days, what moderate/vigorous activities did you do? | Reported exercise volume was calculated as: (monthly frequency/4.286)*duration in minutes)*(intensity in metabolic equivalents [METs]). Those reporting ≥270 MET*minutes/week were classified as currently exercising (30 minutes * 3 times per week * ≥3 METs). |
| PADLEVEL | Reported intensity level of activity | |||
| PADTIMES | How many times did you do this activity? | |||
| PADDURAT | On average, about how long did you do this activity each time? | |||
| PADMETS | Assigned MET score | |||
| Disease History | ||||
| Cardiovascular disease | ||||
| Cardiac | MCQ | MCQ160E | Has a doctor or other health professional ever told you that you had a heart attack (aka MI)? | Those reporting ‘yes’ to either question were classified as having a history of cardiovascular disease |
| MCQ | MCQ160C | Has a doctor or other health professional ever told you that you had coronary heart disease? | ||
| Peripheral vascular | n/a | n/a | n/a | |
| Cerebrovascular | MCQ | MCQ160F | Has a doctor or other health professional ever told you that you had a stroke? | Those reporting ‘yes’ were classified as having a history of cerebrovascular disease |
| Metabolic Disease | ||||
| Type I / II Diabetes | DIQ | DIQ010 | (Other than during pregnancy) have you ever been told by a doctor or health professional that you have diabetes or sugar diabetes? | Those reporting ‘yes’ were classified as having a history of diabetes |
| Renal Disease | KIQ_U | KIQ022 | Have you ever been told by a doctor or other health professional that you have weak or failing kidneys? Do not include kidney stones, bladder infections, or incontinence. | Those reporting ‘yes’ were classified as having a history of renal disease |
| Signs/Symptoms | ||||
| Pain/discomfort in chest, neck, jaw, arms, or other areas (ischemia) | CDQ | CDQ001 | Have you ever had any pain or discomfort in your chest? | Those reporting chest pain when walking uphill in a hurry or walking at an ordinary pace on level ground were classified as having pain that might be related to ischemia |
| CDQ002 | Do you get it when you walk up hill or in a hurry? (per 001) | |||
| CDQ003 | Do you get it when you walk at an ordinary pace on level ground? (per 001) | |||
| Shortness of breath at rest or with mild exertion | CDQ | CDQ010 | Have you had shortness of breath either when hurrying on the level or walking up a slight hill? | Those reporting ‘yes’ were classified as having shortness of breath with mild exertion |
| Dizziness or syncope | BAQ | BAQ010 | During the past 12 months, have you had dizziness, difficulty with balance, or difficulty with falling? | Those reporting ‘yes’ were classified as having dizziness or syncope |
| Orthopnea or PND | n/a | n/a | n/a | |
| Ankle edema | n/a | n/a | n/a | |
| Palpitations or tachycardia | n/a | n/a | n/a | |
| Intermittent claudication | DIQ | DIQ140 | Do you ever get pain in either leg while walking? | Those reporting ‘yes’ were classified as having intermittent claudication |
| Heart murmur | n/a | n/a | n/a | |
| Unusual fatigue | n/a | n/a | n/a | |
Abbreviations: MET – Metabolic equivalent; PND – Paroxysmal nocturnal dyspnea
NHANES section abbreviations: PAQIAF – Physical activity individual activities; MCQ – Medical conditions; DIQ – Diabetes; KIQ_U – Kidney conditions, urology; CDQ – Cardiovascular health; BAQ - Balance
For each participant, binary variables for each component of the ACSM algorithm were created. The value of this variable was determined by the value of the corresponding NHANES item(s) (Table 1). These binary variables were used to classify respondents into the six possible groups in the algorithm. Next, the referral status based on algorithm classification was assigned: 1) no clearance needed, 2) clearance needed before vigorous-intensity exercise only, and 3) clearance needed before any exercise. As noted previously (15), this method of algorithm completion and scoring operates under the assumption that respondents will answer a preparticipation questionnaire in the same manner that they answer the health history items in NHANES.
A similar process was used to complete the AAPQ and PAR-Q based on NHANES responses. These methods have been previously published (15) and are only summarized here. Following the AAPQ instructions, a participant was classified as referred if he or she responded ‘yes’ to any of the history and symptoms of CVD items or “other health issues” items, or responded yes to two or more CVD Risk factor items (see Table, SDC 1, Items from the AAPQ and their corresponding items from NHANES 2001–2004). Following the PAR-Q instructions, a respondent was classified as referred if he or she were aged >69 years and reported less than the equivalent of 10 minutes per day of combined transportation, household/occupational, or leisure time physical activity of at least moderate intensity, or responded ‘yes’ to any of the PAR-Q items for which NHANES corollaries were available (see Table, SDC 2, PAR-Q items and their corresponding items from NHANES 2001–2004).
Statistical Analyses
Referral proportions with 95% confidence intervals were calculated for the sample as a whole, and stratified by sex and age group. A cross-tabulation of referral status comparing the ACSM algorithm to the AAPQ and PAR-Q was also conducted. Differences in referral proportions were assessed with Wald tests with a Bonferroni correction for multiple comparisons; α=0.5.
Post-hoc analyses were done to investigate the prevalence of reported symptoms of CVD. A Monte Carlo simulation was conducted to determine the sensitivity of the algorithm to the most prevalent symptom. In 500 replications, 10% of those reporting ‘no’ for the most prevalent symptom were randomly reassigned to ‘yes’ and the referral criteria were applied to the resulting dataset. This process was also used to change 10% of those originally reporting ‘yes’ for the most prevalent symptom to ‘no’. The average of the 500 referral proportions under each condition (10% higher and 10% lower prevalence) was then compared to the original referral proportions. All analyses used sampling and analytic weights supplied by NHANES. Variance estimation was by Taylor series linearization. Survey commands within Stata version 13.1 were used for all analyses.
Results
The descriptive characteristics for this sample have been previously described (15) and are summarized here. Complete questionnaire responses were available for 3459 women (97.9% of total) and 3326 men (98.5% of total), accordingly, the demographic characteristics were quite similar to the general adult population over 40 years of age in the US from this time period. Based on the algorithm definition above, 47.1% reported enough leisure time activity to be classified as current exercisers.
The distribution of the population across the six categories of the 2015 ACSM algorithm and the total referral proportions are presented in Table 2. Among those reporting no current exercise, 18.0% reported no history or current symptoms, 3.0% reported a positive history but no current symptoms, and 32.0% reported current symptoms. Among those currently exercising, 25.1% reported no history or current symptoms, 2.6% reported a positive history but no current symptoms, and 19.3% reported current symptoms. With this distribution across categories, 43.1% of the population would receive no referral for medical clearance before beginning or continuing exercise, 2.6% would be referred for medical clearance before engaging in vigorous intensity exercise, and 54.2% would be referred for medical clearance before beginning or continuing any exercise.
Table 2:
Percent of respondents aged ≥40 years that would be referred for medical clearance based on the 2015 ACSM preparticipation screening algorithm, National Health and Nutrition Examination Survey, 2001–2004
| No current exercise | Yes current exercise | |||||
|---|---|---|---|---|---|---|
| No Disease History No Symptoms |
Yes Disease History No Symptoms |
Yes Symptoms | No Disease History No Symptoms |
Yes Disease History No Symptoms |
Yes Symptoms | |
| Referral Status |
None | Before Any | Before Any | None | Before Vigorous | Before Any |
| Percent (95% CI) |
18.0% (16.7–19.4) |
3.0% (2.5–3.5) |
32.0% (29.5–34.5) |
25.1% (22.7–27.7) |
2.6% (2.3–3.0) |
19.3% (18.0–20.7) |
| Totals for Each Class of Referral Status | ||||||
| Not Referred | Before Vigorous | Before Any | ||||
| 43.1% (40.6–45.7) |
2.6% (2.3–3.0) |
54.2% (51.6–56.8) |
||||
The referral proportions stratified by sex and age group are presented in Table 3. Across four of the seven age groups and for the sample as a whole, women would be referred for medical clearance before any exercise more frequently than men (all p<0.05). The differences between men and women across age groups was less clear for referral before vigorous intensity exercise, but no group exceeded a 7% referral proportion for this outcome.
Table 3:
Percent of respondents (with 95% confidence interval) aged ≥40 years that would be referred for medical clearance based on the 2015 ACSM preparticipation screening algorithm, stratified by sex and age, National Health and Nutrition Examination Survey, 2001–2004
| Age Categories (Years) | ||||||||
|---|---|---|---|---|---|---|---|---|
| 40–44 | 45–49 | 50–54 | 55–59 | 60–64 | 65–69 | 70+ | Overall | |
| WOMEN | n=447 | n=394 | n=370 | n=268 | n=420 | n=348 | n=1138 | n=3385 |
| Referred Vigorous | 1.2% (0.4–3.4) |
1.5% (0.6–3.7) |
2.1% (0.9–4.7) |
2.0% (0.7–5.2) |
3.2% (1.7–5.7) |
3.0% (1.3–6.6) |
1.8% (1.1–2.9) |
1.9% (1.5–2.5) |
| Referred Any |
49.8% (42.4–57.2) |
51.9% (45.9–58.0) |
56.1% (47.7–64.2) |
61.9% (55.1–68.2) |
57.9% (50.1–65.2) |
66.3% (59.8–72.2) |
74.6% (71.2–77.7) |
59.8% (56.3–63.2) |
| MEN | n=447 | n=406 | n=386 | n=261 | n=384 | n=341 | n=1051 | n=3276 |
| Referred Vigorous | 2.5% (1.1–5.6) |
2.2% (1.3–3.6) |
3.1% (1.6–5.9) |
2.0% (0.7–5.4) |
3.9% (21.−7.2) |
7.0% (4.2–11.4) |
5.5% (3.9–7.7) |
3.4% (3.0–4.0) |
| Referred Any | 36.1% (31.3–41.2) |
34.4% (30.8–38.3) |
50.8% (46.0–55.7) |
49.1% (42.4–55.9) |
57.0% (48.6–65.0) |
57.1% (48.6–65.1) |
65.7% (62.3–68.9) |
48.1% (45.7–50.5) |
Values for women in bold are significantly different than the comparable value among men (Bonferroni-adjusted p<0.05)
Combined results from the ACSM algorithm, the AAPQ, and the PAR-Q are presented in Figure 2, stratified by age group. Across all age groups, the AAPQ would refer more respondents (94.5%) than either the PAR-Q (68.4%) or the ACSM algorithm, including those referred only before vigorous exercise (2.6%) and those referred before any exercise (54.2%). When considering those referred before any exercise, the ACSM algorithm and the PAR-Q performed similarly in the 40–44 year age group (42.9% and 48.8% referred, respectively), then the referral proportions diverged with increasing age. For those aged 70 years or older, the ACSM algorithm would refer 70.9% before any exercise and the PAR-Q would refer 93.2%.
Figure 2: Comparison of predicted referral proportions for the 2015 ACSM algorithm, AAPQ, and PAR-Q.
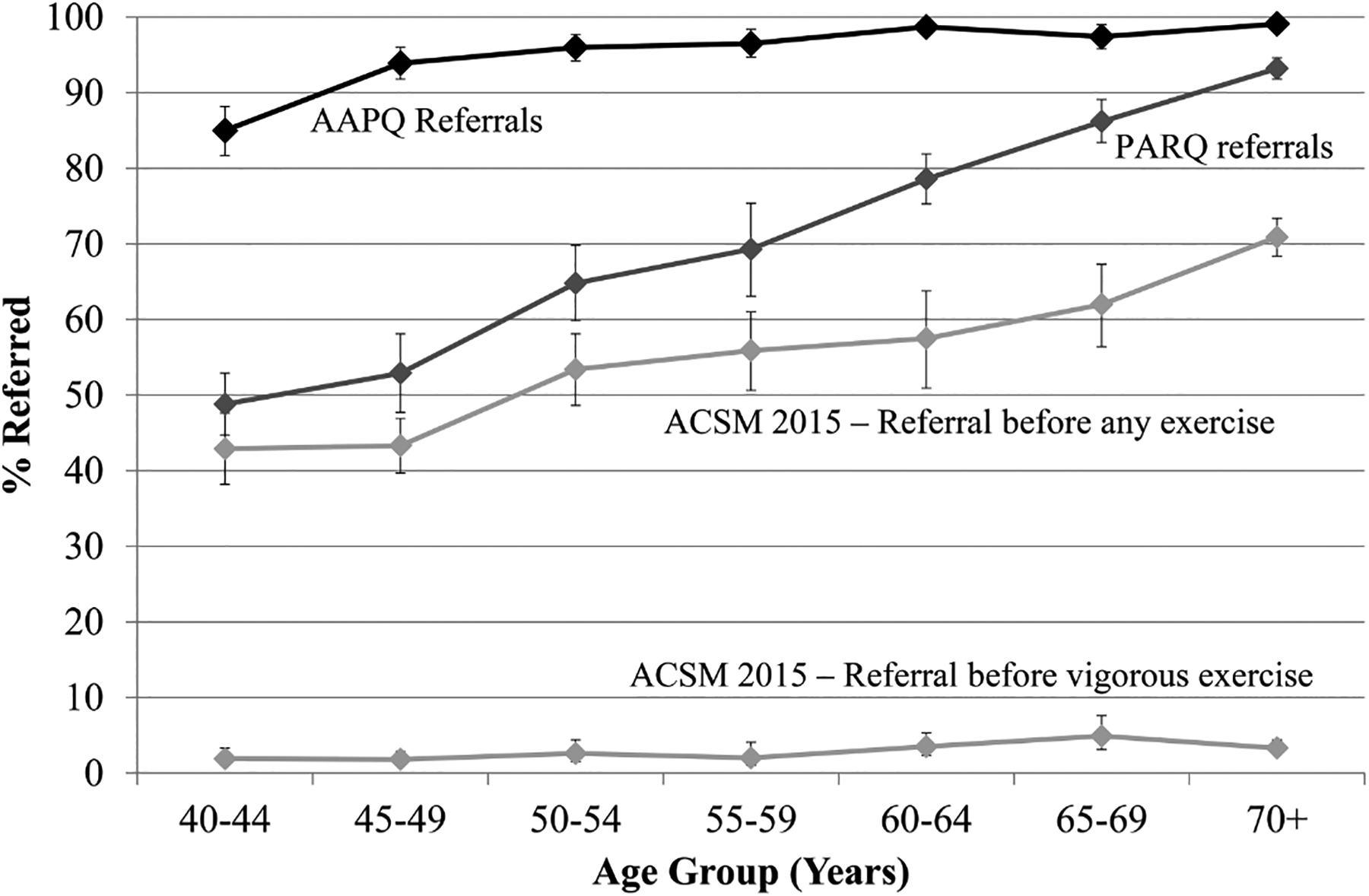
Results for the AAPQ and PAR-Q have been previously published (15)
Abbreviations: ACSM: American College of Sports Medicine; AAPQ: ACSM/American Heart Association Preparticipation Questionnaire; PAR-Q: Physical Activity Readiness Questionnaire; PA: Physical Activity
According to the cross-tabulation presented in Table 4, 37.7% of respondents were referred by the AAPQ but were not referred by the ACSM algorithm. Only one respondent (<0.1% of the weighted total) was not referred based on the AAPQ but was referred before vigorous-intensity exercise based on the ACSM algorithm. Further, 19.0% of respondents were referred based on the PAR-Q but were not referred based on the ACSM algorithm. Only 7.4% of respondents were not referred based on the PAR-Q but were referred based on the ACSM algorithm (0.5% before vigorous-intensity exercise only, 6.9% before any exercise).
Table 4:
Cross-tabulation of the percent of respondents (with 95% confidence interval) aged ≥40 years that would be referred for medical clearance by three screening tools, National Health and Nutrition Examination Survey, 2001–2004
| AAPQ Referral Status | PAR-Q Referral Status | |||
|---|---|---|---|---|
| ACSM Algorithm Referral Status | Not Referred | Referred | Not Referred | Referred |
| Not Referred | 5.5% (4.6–6.5) |
37.7% (35.3–40.1) |
24.1% (22.4–25.9) |
19.0% (17.5–20.7) |
| Referred-Vigorous | <0.1% (<0.1–0.1) |
2.6% (2.3–3.0) |
0.5% (0.4–0.8) |
2.1% (1.8–2.5) |
| Referred-Any | 0% | 54.2% (51.7–56.8) |
6.9% (6.2–7.8) |
47.3% (44.5–50.1) |
ACSM: American College of Sports Medicine
AAPQ: ACSM/American Heart Association Preparticipation Questionnaire
PAR-Q: Physical Activity Readiness Questionnaire
The proportion that reported any current symptoms was higher than expected (54.2%) and further investigated. Shortness of breath was the most commonly reported symptom: 72.0% of those with any symptom reported shortness of breath. It is likely that many reported cases of shortness of breath are due to benign causes other than worsening CVD. Monte Carlo-based sensitivity analyses suggested shortness of breath was an important referral trigger. When the prevalence of shortness of breath was randomly increased 10% in the sample, the proportion referred for clearance before any exercise increased 9% (five percentage points) from 54% to 59%. When the prevalence was decreased by 10%, the proportion referred before any exercise decreased 2% (one percentage point) to 53% (not shown).
Discussion
Using the same methods and assumptions as a previous evaluation (15), the ACSM algorithm would refer fewer US adults aged 40 years or older for medical clearance than either the AAPQ or the PAR-Q. Previous research suggested that 95% of this demographic group would be referred for a physician visit under the AAPQ scoring criteria. While additional validation is needed, this analysis suggests 37.7% of adults in this age range that would be referred based on the AAPQ would not be referred based on the ACSM algorithm. This reduction in referrals may mitigate a potentially important barrier to exercise adoption.
The lower referral proportion in the ACSM algorithm is likely attributable to the removal of CVD risk factors from the prescreening criteria. Because of the widespread prevalence of CVD risk factors (4) and the rarity of exercise-associated CVD events (12), CVD risk factor assessment is likely a poor predictor of these events. For example, the CDC estimates that 70 million American adults have high blood pressure, compared to 600,000 who die of CVD each year (0.9% of 70 million) (5, 6), and only a small percent of these CVD deaths occur during exercise (12). Assessment of CVD risk factors therefore may overestimate the proportion of people at risk for exercise-associated CVD complications. The removal of CVD risk factors also aligns the ACSM algorithm with the 2008 Physical Activity Guidelines for Americans, which place focus on diagnosed chronic diseases and symptoms thereof:
“People without diagnosed chronic conditions (such as diabetes, heart disease, or osteoarthritis) and who do not have symptoms (such as chest pain or pressure, dizziness, or joint pain) do not need to consult a health-care provider about physical activity.” (13)
As with the ACSM algorithm, the Guidelines also consider a person’s initial level of activity, progression of activity, and development of symptoms when considering medical involvement:
“Inactive people who gradually progress over time to relatively moderate-intensity activity have no known risk of sudden cardiac events, and very low risk of bone, muscle, or joint injuries. A person who is habitually active with moderate-intensity activity can gradually increase to vigorous intensity without needing to consult a health-care provider. People who develop new symptoms when increasing their levels of activity should consult a health-care provider.” (13)
While designed primarily for fitness professionals, the ACSM algorithm is more aligned with the public health recommendations set forth in the Physical Activity Guidelines than previous screening tools.
The ACSM algorithm differentiates referrals based on the desired exercise intensity of the respondent, and the proportion that would be referred before any exercise was much higher than the proportion that would be referred only before vigorous intensity exercise. This is likely attributed to two factors. First, a recommendation for clearance only before vigorous exercise is given to one highly specific group in the algorithm: those who have previously had cardiovascular, metabolic, or renal disease, but have recovered or stabilized to the point that they now perform regular exercise and are free of symptoms. They warrant referral under the algorithm only before increasing to vigorous intensity. Second, in contrast to the very specific group previously mentioned, three of the six categories in the algorithm receive a recommendation for clearance before any exercise. These include any respondents that report a current symptom (both physically active and inactive) and those that are currently inactive and have a history of cardiovascular, metabolic, or renal disease. Among adults aged 40 years and older, this includes a considerable proportion of the population. Samples with more diverse age ranges would likely exhibit different referral proportions.
Using the present methods, the referral proportion of the ACSM algorithm was more similar to the PAR-Q than the AAPQ, which was likely because of the similarity of these two instruments. For example, both the ACSM algorithm and PAR-Q place emphasis on a history of CVD, current chest pain, and dizziness or lack of balance. Further, the ACSM algorithm does not consider age and the PAR-Q only considers age as important if the person is currently inactive. The 19.0% of respondents that were referred based on the PAR-Q but not referred based on the ACSM algorithm is likely due to the inclusion of bone and joint issues and medication use for hypertension in the PAR-Q, neither of which are considered in the ACSM algorithm.
This report has several strengths. First, the exact methods and dataset from a previous evaluation of the AAPQ and PAR-Q were used, allowing comparison of referral proportions under identical assumptions (15). Second, the NHANES dataset is representative of the non-institutionalized US population over 40 years of age; this study provides information about referral performance in the general public. Finally, this method allows for rapid comparison of screening tools at low cost. Several limitations should also be noted. First, several symptoms on the ACSM algorithm could not be assessed, but analyses suggested that assessed symptoms tended to cluster together, which could limit the impact of unassessed symptoms. Nevertheless, omission of symptoms could cause an underestimation of referral proportion. Second, we were unable to assess referral proportions in adults under 40 years of age. Third, as with the previous report (15), this method assumes that people will answer a pre-screening questionnaire the same way they answered comprehensive health interview questions, and the validity of this assumption is unknown. Finally, the criteria for participating in regular exercise in the ACSM algorithm is different from the 2008 Physical Activity Guidelines (13), but a post-hoc analysis that defined regular exercise as 150 minutes per week of at least moderate intensity leisure-time activity instead of 90 minutes per week suggested little impact on referral status (43.1% not referred [43.1% originally], 2.3% referred before vigorous exercise [2.6% originally], and 54.6% referred before any exercise [54.2% originally]).
In conclusion, the revised ACSM algorithm referred fewer NHANES respondents for medical clearance compared to the AAPQ. Definitive confirmation of this finding would require comparison of referral proportions in actual practice in exercise facilities. While additional validation is needed to determine how well the algorithm identifies those at risk for CVD complications during exercise, a lower referral proportion may mitigate an important barrier to exercise adoption, especially among those who undergo a preparticipation screening program based on ACSM recommendations. Considering that 73% of ACSM-certified Health Fitness Specialists report performing some type of preparticipation screening (2), the potential use of this new algorithm is considerable.
Supplementary Material
SDC 2: Table: PAR-Q items and their corresponding items from NHANES 2001–2004
SDC 1: Table: Items from the AAPQ and their corresponding items from NHANES 2001–2004
Acknowledgements
No outside funds were used for this study. The results of the study are presented clearly, honestly, and without fabrication, falsification, or inappropriate data manipulation.
Footnotes
Publisher's Disclaimer: Disclaimer
Publisher's Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, nor do they constitute endorsement by ACSM.
Conflict of Interest
The authors have participated in development of the ACSM preparticipation screening algorithm and the Guidelines for Exercise Testing and Prescription. Other than travel compensation, no financial support was received.
References
- 1.American College of Sports Medicine. Preparticipation Health Screening In: Pescatello LS Arena R, Riebe D, Thompson P, editors. ACSM’s guidelines for exercise testing and prescription. 9th ed Philadelphia, PA: Lippincott Williams & Wilkins; 2014. p. 23–31. [Google Scholar]
- 2.Craig AC, Eickhoff-Shemek J. Adherence to ACSM’s Pre-Activity Screening Procedures in Fitness Facilities: a National Investigation. J Phys Ed Sports Mgmt. 2015;2(2):120–137. [Google Scholar]
- 3.Dahabreh IJ, Paulus JK. Association of episodic physical and sexual activity with triggering of acute cardiac events: systematic review and meta-analysis. JAMA. 2011;305:1225–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heart Disease Risk Factors [Internet]. Atlanta, GA: Centers for Disease Control and Prevention; [Cited 2016 December 1]. Available from: http://www.cdc.gov/heartdisease/risk_factors.htm. [Google Scholar]
- 5.Heart Disease Statistics and Maps [Internet]. Atlanta, GA: Centers for Disease Control and Prevention; [Cited 27 October 2016]. Available from: http://www.cdc.gov/heartdisease/statistics_maps.htm. [Google Scholar]
- 6.High Blood Pressure [Internet]. Atlanta, GA: Centers for Disease Control and Prevention; [Cited 27 October 2016]. Available from: http://www.cdc.gov/bloodpressure/index.htm. [Google Scholar]
- 7.Kohl HW 3rd, Powell KE, Gordon NF, Blair SN, Paffenbarger RS Jr. Physical activity, phyical fitness, and sudden cardiac death. Epidemiol Rev. 1992;14:37–58. [DOI] [PubMed] [Google Scholar]
- 8.Mittleman MA, Maclure M, Tofler GH, Sherwood JB, Goldberg RJ, Muller JE. Triggering of acute myocardial infarction by heavy physical exertion. Protection against triggering by regular exertion. Determinants of Myocardial Infarction Onset Study Investigators. N Engl J Med. 1993;329(23):1677–83. [DOI] [PubMed] [Google Scholar]
- 9.National Health and Nutrition Examination Survey; Questionnaires, Datasets, and Related Documentation [Internet]. Atlanta, GA: Centers for Disease Control and Prevention; [Cited 27 October 2016]. Available from: http://www.cdc.gov/nchs/nhanes/nhanes_questionnaires.htm. [Google Scholar]
- 10.Physical Activity Guidelines Advisory Committee Physical Activity Guidelines Advisory Committee Report. 2008. Washington, DC: U.S. Department of Health and Human Services; 2008. [DOI] [PubMed] [Google Scholar]
- 11.Riebe D, Franklin BA, Thompson PD, Garber CE, Whitfield GP, Magal M, Pescatello LS. Updating ACSM’s Recommendations for Exercise Preparticipation Health Screening. Med Sci Sports Exerc. 2015;47(11):2473–9. [DOI] [PubMed] [Google Scholar]
- 12.Thompson PD, Franklin BA, Balady GJ, et al. Exercise and acute cardiovascular events placing the risks into perspective: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism and the Council on Clinical Cardiology. Circulation. 2007;115(17):2358–68. [DOI] [PubMed] [Google Scholar]
- 13.United States Department of Health and Human Services Physical Activity Guidelines for Americans, Chapter 6: Safe and Active. Washington, DC: U.S. Department of Health and Human Services; 2008. Pgs 35–40. Available from: https://health.gov/paguidelines/guidelines/chapter6.aspx. [Cited 20 December 2016]. [Google Scholar]
- 14.Warning Signs of Heart Failure [Internet]. Dallas, TX: American Heart Association; [Cited: 11 May 2017]. Available from: http://www.heart.org/HEARTORG/Conditions/HeartFailure/WarningSignsforHeartFailure/Warning-Signs-of-Heart-Failure_UCM_002045_Article.jsp#.WRSrCU1dBD8. [Google Scholar]
- 15.Whitfield GP, Pettee Gabriel KK, Rahbar MH, Kohl HW 3rd. Application of the American Heart Association/American College of Sports Medicine Adult Preparticipation Screening Checklist to a nationally representative sample of US adults aged >=40 years from the National Health and Nutrition Examination Survey 2001 to 2004. Circulation. 2014;129(10):1113–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
SDC 2: Table: PAR-Q items and their corresponding items from NHANES 2001–2004
SDC 1: Table: Items from the AAPQ and their corresponding items from NHANES 2001–2004


