Abstract
Background
Ulcerative colitis is an inflammatory condition affecting the colon, with an annual incidence of approximately 10 to 20 per 100,000 people. The majority of people with ulcerative colitis can be put into remission, leaving a group who do not respond to first‐ or second‐line therapies. There is a significant proportion of people who experience adverse effects with current therapies. Consequently, new alternatives for the treatment of ulcerative colitis are constantly being sought. Probiotics are live microbial feed supplements that may beneficially affect the host by improving intestinal microbial balance, enhancing gut barrier function and improving local immune response.
Objectives
The primary objective was to determine the efficacy of probiotics compared to placebo, no treatment, or any other intervention for the maintenance of remission in people with ulcerative colitis. The secondary objective was to assess the occurrence of adverse events associated with the use of probiotics.
Search methods
We searched CENTRAL, MEDLINE, Embase, and two other databases on 31 October 2019. We contacted authors of relevant studies and manufacturers of probiotics regarding ongoing or unpublished trials that may be relevant to the review, and we searched ClinicalTrials.gov. We also searched references of trials for any additional trials.
Selection criteria
Randomised controlled trials (RCTs) that compared probiotics against placebo or any other intervention, in both adults and children, for the maintenance of remission in ulcerative colitis were eligible for inclusion. Maintenance therapy had to be for a minimum of three months when remission has been established by any clinical, endoscopic,histological or radiological relapse as defined by study authors.
Data collection and analysis
Two review authors independently conducted data extraction and 'Risk of bias' assessment of included studies. We analysed data using Review Manager 5. We expressed dichotomous and continuous outcomes as risk ratios (RRs) and mean differences (MDs) with 95% confidence intervals (CIs). We assessed the certainty of the evidence using the GRADE methodology.
Main results
In this review, we included 12 studies (1473 randomised participants) that met the inclusion criteria. Participants were mostly adults. The studies compared probiotics to placebo, probiotics to 5‐aminosalicylic acid (5‐ASA) and a combination of probiotics and 5‐ASA to 5‐ASA. The studies ranged in length from 12 to 52 weeks. The average age of participants was between 32 and 51, with a range between 18 and 88 years. Seven studies investigated a single bacterial strain, and five studies considered mixed preparations of multiple strains. The risk of bias was high in all except three studies due to selective reporting, incomplete outcome data and lack of blinding. This resulted in low‐ to very low‐certainty of evidence.
It is uncertain if there is any difference in occurrence of clinical relapse when probiotics are compared with placebo (RR 0.87, 95% CI 0.63 to 1.18; 4 studies, 361 participants; very low‐certainty evidence (downgraded for risk of bias, imbalance in baseline characteristics and imprecision)). It is also uncertain whether probiotics lead to a difference in the number of people who maintain clinical remission compared with placebo (RR 1.16, 95% CI 0.98 to 1.37; 2 studies, 141 participants; very low‐certainty evidence (downgraded for risk of bias, imbalance in baseline characteristics and imprecision)).
When probiotics are compared with 5‐ASA, there may be little or no difference in clinical relapse (RR 1.01, 95% CI 0.84 to 1.22; 2 studies, 452 participants; low‐certainty evidence) and maintenance of clinical remission (RR 1.06, 95% CI 0.90 to 1.25; 1 study, 125 participants; low‐certainty evidence). It is uncertain if there is any difference in clinical relapse when probiotics, combined with 5‐ASA are compared with 5‐ASA alone (RR 1.11, 95% CI 0.66 to 1.87; 2 studies, 242 participants; very low‐certainty evidence (downgraded due to risk of bias and imprecision)). There may be little or no difference in maintenance of remission when probiotics, combined with 5‐ASA, are compared with 5‐ASA alone (RR 1.05, 95% CI 0.89 to 1.24; 1 study, 122 participants; low‐certainty evidence).
Where reported, most of the studies which compared probiotics with placebo recorded no serious adverse events or withdrawals due to adverse events. For the comparison of probiotics and 5‐ASA, one trial reported 11/110 withdrawals due to adverse events with probiotics and 11/112 with 5‐ASA (RR 1.02, 95% CI 0.46 to 2.25; 222 participants; very low‐certainty evidence). Discontinuation of therapy was due to gastrointestinal symptoms. One study (24 participants) comparing probiotics combined with 5‐ASA with 5‐ASA alone, reported no withdrawals due to adverse events; and two studies reported two withdrawals in the probiotic arm, due to avascular necrosis of bilateral femoral head and pulmonary thromboembolism (RR 5.29, 95% CI 0.26 to 107.63; 127 participants; very low‐certainty evidence).
Health‐related quality of life and need for additional therapy were reported infrequently.
Authors' conclusions
The effectiveness of probiotics for the maintenance of remission in ulcerative colitis remains unclear. This is due to low‐ to very low‐certainty evidence from poorly conducted studies, which contribute limited amounts of data from a small number of participants. Future trials comparing probiotics with 5‐ASA rather than placebo will better reflect conventional care given to people with ulcerative colitis. Appropriately powered studies with a minimum length of 12 months are needed.
Plain language summary
Probiotics for maintenance of remission in ulcerative colitis
What is the aim of this review?
The aim of this Cochrane Review was to find out whether probiotics can maintain remission in people with ulcerative colitis. We collected and analysed data from 12 studies with a total of 1473 people to answer this question.
Key messages
The question on whether probiotics can maintain remission in people with ulcerative colitis remains unanswered. There were no serious adverse events when probiotics were compared with placebo. However, one study reported similar numbers of serious adverse events in people who had probiotics and those who received 5‐aminosalicylic acid (5‐ASA, an anti‐inflammatory medicine used to treat ulcerative colitis and other conditions. . More information as to what these serious adverse events are, was not provided.
What was studied in the review?
Ulcerative colitis is a chronic disease of the large bowel, which causes inflammation (swelling). Some of the symptoms include tummy pain, diarrhoea and tiredness. Probiotics are living microscopic organisms that are thought to change the growth of bacteria in the bowel and reduce inflammation.
What are the main results of the review?
We searched for randomised controlled trials (RCTs; clinical studies where people are randomly put into one of two or more treatment groups) comparing probiotics with placebo (dummy treatment), probiotics with 5‐ASA and a combination of probiotics and 5‐ASA with 5‐ASA. There were 12 RCTs involving 1473 participants. The trials looked at adult males and females. Only three studies clearly stated that participants were not allowed to take other medication outside of those being compared.
1) There was no clear difference in the number of people who had a clinical relapse when probiotics were compared with placebo.
2) There was also no clear difference in the number of people who had a clinical relapse when probiotics were compared with 5‐ASA.
3) It is uncertain whether probiotics lead to a difference in the number of people who remain in clinical remission compared with placebo because the quality of evidence is very low.
4) There was no clear difference in the number of people who remained in clinical remission when probiotics were compared to 5‐ASA.
5) When probiotics combined with 5‐ASA was compared to 5‐ASA alone, there was no clear difference in the number of people who remained in clinical remission.
6) It is uncertain whether probiotics combined with 5‐ASA lead to a difference in the number of people who have a clinical relapse when compared with 5‐ASA alone.
7) No serious adverse events were reported in the trials which compared probiotics with placebo. One study which compared probiotics with 5‐ASA reported similar numbers of serious adverse events with both treatments. Discontinuation of therapy was due to gastrointestinal disorders, such as bloody stools, nausea, diarrhoea and abdominal pain.
8) There was not enough information from the studies on how probiotics affect people's quality of life and the need for additional therapy when compared to other treatments.
Conclusion
We are uncertain as to whether probiotics can maintain remission in people with ulcerative colitis. This is because the studies had very few participants and were not conducted using reliable methods. With the evidence presented in these studies, we are unable to make strong conclusions into the effectiveness of probiotics; better designed studies with more participants are needed.
How up‐to‐date is this review?
This review is up‐to‐date as of October 2019.
Summary of findings
Background
Description of the condition
Ulcerative colitis is a chronic relapsing disease, with the greatest reported incidence in mainland Europe and Scandinavia of 9.2 to 20.3 per 100,000 people (Loftus 2004), totalling approximately 2.2 million sufferers in Europe alone. The peak incidence of the disease occurs between 15 and 25 years of age, and there is another smaller prevalence at ages 55 to 65. The disease is characterised by abdominal pain, bloody diarrhoea and faecal urgency. The diagnosis of ulcerative colitis is based on medical history, signs and symptoms, and any endoscopic or histopathological findings.
The disease is caused by diffuse inflammation, which starts at the rectum, spreads proximally, and is limited to the colon. The aetiology behind the disease is unknown, but is likely to be multifactorial; consisting of a genetic predisposition, dysregulation of the mucosal and epithelial barrier and lastly dysbiosis, although whether dysbiosis causes or is a result of the disease remains unclear (Ungaro 2016). The genetic component was further evaluated by Cleynen 2016 and a strong association between HLA DRB1 and ulcerative colitis was found. The genetic predisposition creates a four‐fold risk for first‐degree relatives.
Description of the intervention
Probiotics are live micro‐organisms, that when consumed, may provide multiple health benefits. They produce their benefits by altering the gut microbiome through either enhancing the activity, volume or both, of the normal flora. Lactobacillus spp, for example, is one of the more popular probiotics and is thought to secrete bacteriocin, blocking the adherence of translocation of harmful bacteria (Panigrahi 2014).
Lactobacillus rhamnosus GG (Lrhamnosus) produced mixed responses in animal models of colitis (Dieleman 2003; Shibolet 2002), as did Lactobacillus plantarum (Lplantarum) 299V (Dieleman 2003; Kennedy 2000; Schultz 2002). Studies investigating combinations of probiotic species incorporated within De Simone Formulation have demonstrated a partial reduction of colitis in animal models (Madsen 2001; Shibolet 2002). There has been increasing interest in the use of probiotics, as they are considered safe and easily accessible (Ong 2019). It is worth noting that there are a huge number of different preparations available, varying in the specific strains isolated, the use of mixed strains in a single preparation, the form of the preparation and finally the licensing arrangements surrounding the preparations (medicinal versus food products).
How the intervention might work
There is growing evidence looking at the effects of probiotics in the use of inducing remission in ulcerative colitis since a previous Cochrane review (Mallon 2007). Due to the part that dysbiosis plays in ulcerative colitis, there is potential benefit in trying to restore the endogenous flora. Several observations, both on humans and animal models, emphasised the importance of bacterial flora in inflammatory bowel disease pathogenesis, justifying the current interest in antibiotic and probiotic therapies aimed at the manipulation of enteric flora (Cui 2004). The therapeutic efficacy of probiotics has been demonstrated in various models of experimental colitis, including interleukin‐10 deficient mice (Madsen 1999; Schultz 2002), and acetic acid‐induced colitis in rats (Fabia 1993).
Why it is important to do this review
In the UK, National Institute for Health and Care Excellence (NICE) and USA guidelines state that first‐line therapy for maintenance of remission in ulcerative colitis is 5‐aminosalicylic acid (5‐ASA) (NICE 2019). 5‐ASA works by binding to PPAR‐ỿ and reducing cytokine production. Some of the adverse effects associated with 5‐ASA include headache, rash, nausea (common), pancreatitis (uncommon), and agranulocytosis (rare). Due to these side effects, some people are unable to tolerate the drug. If 5‐ASA fails to work then other therapies to maintain remission include immune suppressants, such as anti‐tumour necrosis factor (TNF) monoclonals, vedolizumab and tofacitinib may be used. These drugs work by blocking leukocyte recruitment at the molecular and vascular level (Fiorino 2016), some of the side effects include headache, dizziness and arthralgia.
The relapsing and remitting nature of the disease means that people can be in and out of hospital, experimenting with different drug regimes. The treatment costs Europe between GBP 11 to 26 billion pounds annually, with per patient costs approximately GBP 8011 to 9306 (Cohen 2010). If an alternative, cheaper treatment can be found for ulcerative colitis, then it would greatly benefit not only a budget stricken National Health Service (NHS), but also improve patients' quality of life. Whilst some studies have suggested that probiotics may be useful for maintenance of remission in mild to moderate ulcerative colitis (Kruis 2004; Zocco 2006), others have failed to show any benefit (Kruis 1997; Rembacken 1999). In this review we investigate the available evidence on the use of probiotics for the maintenance of remission in ulcerative colitis.
Objectives
The primary objective was to determine the efficacy of probiotics compared to placebo, no treatment, or any other intervention for the maintenance of remission in people with ulcerative colitis. The secondary objective was to assess the occurrence of adverse events associated with the use of probiotics.
Methods
Criteria for considering studies for this review
Types of studies
We considered randomised controlled trials (RCTs), with a minimum duration of three months, for inclusion in the review.
Types of participants
People of any age with ulcerative colitis in remission, defined as clinical, endoscopic, histological or radiological relapse by study authors.
Types of interventions
Probiotics administered in any form (drink, powder, capsule), orally as a single species, or as a cocktail of multiple species compared to no treatment, placebo or any other intervention.
Types of outcome measures
Primary outcomes
Relapse (clinical, endoscopic, histopathological or radiological), as defined by the authors of the primary studies.
Where studies reported on the number of participants who did not experience a relapse, i.e. those who remained in remission, this was noted under 'maintenance of clinical remission'.
Secondary outcomes
Serious adverse events
Withdrawal due to adverse events
Need for additional therapy
Health‐related quality of life, as measured by a validated quality of life tool
Search methods for identification of studies
Electronic searches
We conducted a comprehensive and systematic search to identify RCTs from inception to 31 October 2019 using the following databases.
Cochrane Inflammatory Bowel Disease (IBD) Specialized Trials Register
Cochrane Central Register of Controlled Trials (CENTRAL)
MEDLINE
Embase
CINAHL
We did not place any restrictions on publication dates (after 1966) or language. See Appendix 1 for the detailed search strategies.
Searching other resources
We inspected the reference lists of all identified studies for more trials. We also contacted leaders in the field and manufacturers of probiotics to identify potentially relevant studies. We also searched ClinicalTrials.gov (clinicaltrials.gov) for ongoing trials (Appendix 1).
Data collection and analysis
We conducted data collection and analysis according to methods stipulated in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011).
Selection of studies
We undertook study selection in Covidence. Using the above search strategy, two review authors (LK, ZIE) identified titles that appeared to be potentially relevant. These were independently screened and in circumstances of disagreement, a third review author (AA) was involved to reach consensus.
There is some evidence that data from abstract publications can be inconsistent with data from published articles (Pitkin 1999), therefore we considered abstract publications, but only if sufficient data were presented to judge inclusion criteria fully and reports of the primary and secondary outcomes were given. If these were not available, we contacted authors directly, and if data were not provided, we excluded such studies.
The review authors, after reading the full texts, independently assessed the eligibility of all trials identified using ad hoc eligibility, based on the inclusion criteria above. Disagreement among review authors was again discussed, and agreement was reached by consensus after involvement of a third review author. We contacted authors of multiple publications, which appeared to report on the same study, for clarification. A flow chart was included (Figure 1).
1.
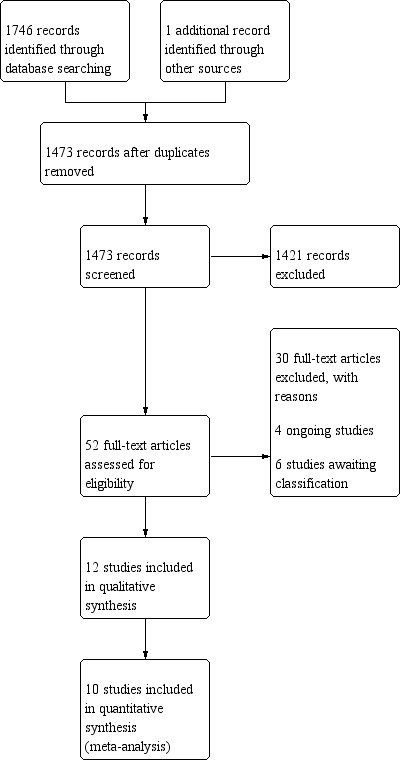
Study flow diagram.
Data extraction and management
We developed a data extraction form and used it to extract information on relevant features and results of included studies. Two review authors (LK, ZIE) independently extracted and recorded data on a predefined checklist. Again, when disagreements occurred, a third review author (AA) was involved and consensus was reached. Extracted data included the following items.
Characteristics of participants: age, sex, disease distribution, disease duration, disease activity index
Total number of participants originally assigned to each intervention group
Intervention: type and dose of probiotic(s)
Control: no intervention, placebo or other interventions
Concurrent medications
Outcomes: time of assessment, length of follow‐up, type of symptom score used or ulcerative colitis activity index, definition of remission and relapse, relapse rates, time to relapse, quality of life assessment, and adverse events
We resolved inconsistencies in data extraction, and transferred the information above into the Characteristics of included studies table.
Assessment of risk of bias in included studies
Two review authors (LK, ZIE) independently assessed risk of bias using the Cochrane 'Risk of bias' tool (Higgins 2011). We assessed the following domains.
-
Selection bias
Sequence generation (i.e. was the allocation sequence adequately generated?)
Allocation sequence concealment (i.e. was allocation adequately concealed?)
Performance bias (i.e. was knowledge of the allocated intervention adequately prevented during the study towards the participants?)
Detection bias (i.e. were outcome assessors blinded adequately?)
Attrition bias (were attritions and exclusions adequately reported?)
Reporting bias: selective outcome reporting (i.e. are reports of the study free of suggestion of selective outcome reporting?)
Other potential sources of bias (i.e. was the study apparently free of other problems that could put it at a high risk of bias?)
We considered subjective outcomes separately in our assessment of blinding and incompleteness of data. We judged studies to be at 'high', 'low' or 'unclear' risk of bias for each domain assessed. We judged the risk of bias across studies as follows.
Low risk of bias (plausible bias unlikely to seriously alter the results) if all domains are at low risk of bias.
Unclear risk of bias (plausible bias that raises some doubt about the results) if one or more domains are at unclear risk of bias.
High risk of bias (plausible bias that seriously weakens confidence in the results) if one or more domains are at high risk of bias.
Disagreements were resolved by consensus. We contacted study authors when insufficient information was provided to determine the risk of bias. Where we obtained information supporting our judgement on risk of bias through correspondence with study authors, we indicated this in the 'Risk of bias' table.
Measures of treatment effect
The measure of treatment effect for dichotomous outcomes was risk ratios (RRs). Where continuous outcomes reported with the same scale, we used mean differences (MDs).
Unit of analysis issues
The unit of analysis was the participant. Where studies assessed more than two interventions which are relevant to the review, we made multiple pair wise comparisons and analysed just the groups of interest. We did not include the same group of participants twice in the same meta‐analysis. We were alert to the unit of analysis issues relating to outcome reporting at different follow‐up times and only reported outcomes at final follow‐up.
Dealing with missing data
We contacted study authors to request missing data. Where authors reported both intention‐to‐treat (ITT) and per protocol analysis, we preferred the former. However, where ITT analysis was not conducted or reported in the studies, we regarded withdrawals as failures. We undertook sensitivity analyses to exclude studies with missing data. We did not impute missing standard deviations (SDs). However, we noted any instances where data were extracted from graphs.
Assessment of heterogeneity
We assessed heterogeneity among trial results by inspection of graphical presentations and by calculating the Chi2 test of heterogeneity; we regarded P = 0.10 as statistically significant. We used the I2 statistic to quantity the effect of heterogeneity (Higgins 2003).
We based our interpretation of the I2 statistic results on those suggested by Higgins 2011 (Section 9.5.2):
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%; may represent substantial heterogeneity;
75% to 100%: considerable heterogeneity.
Assessment of reporting biases
We avoided different reporting biases by conducting an extensive literature search. It was not necessary to generate a funnel plot to investigate publication bias, as there were an insufficient number of studies contributing to the analysis.
Data synthesis
We pooled studies with the same population, intervention, comparator and outcomes; we did not pool studies which were clinically heterogenous. We used Review Manager 5 for data analysis (Review Manager 2014). For dichotomous variables, we calculated RRs and 95% confidence intervals (CIs) based on a random‐effects model. For continuous variables, we calculated the MD and 95% CIs when continuous outcomes were measured using the same units. We used the fixed‐effect model, as I2 = 0. We had planned to use the random‐effects model if I2 had been > 0.
Subgroup analysis and investigation of heterogeneity
Had we included a sufficient number of studies, we would have carried out subgroup analyses based on:
age (below 18 years and above 18 years); and
species of probiotic.
Sensitivity analysis
We carried out the following sensitivity analyses, apart from the exclusion of studies at high risk of bias; this was not possible due to the paucity of data.
Only including participants whose outcome is known (i.e. number of participants who completed the study used as denominator)
Study quality (removing those at highest risk of bias)
Random‐effects versus fixed‐effect models
Summary of findings and assessment of the certainty of the evidence
We used the GRADE approach to assess the certainty of evidence related to all outcomes listed in the Types of outcome measures (Schünemann 2011). The four levels of evidence certainty are 'high', 'moderate', 'low' or 'very low'. Certainty may be downgraded due to study limitations (risk of bias), imprecision, inconsistency, indirectness or publication bias. We derived the optimal information size for the primary outcomes from the included studies.
Two review authors (MG, ZIE) independently produced 'Summary of findings' tables using the GRADEpro GDT software for our main comparisons (GRADEpro GDT 2015). We presented the results for clinical relapse, maintenance of clinical remission, health‐related quality of life, need for additional therapy, serious adverse events, and withdrawal due to serious adverse events.
Results
Description of studies
Results of the search
The literature search returned 1473 unique records after duplicates were removed; we also identified an additional study from another source. After screening 1474 titles and abstracts, we found 52 studies that met our inclusion criteria. We obtained and screened the full‐text copies of these 52 studies. We included 12 studies and excluded 30 studies with reasons. We contacted authors of eight studies for additional information (Bjarnason 2019; Copaci 2014; Shanahan 2006; Wildt 2011; Yasushi 2015; Zocco 2003; Zocco 2006; NCT02361957); we received responses from three authors (NCT02361957; Bjarnason 2019; Wildt 2011). We identified four ongoing studies and six studies are awaiting classification (Characteristics of ongoing studies; Characteristics of studies awaiting classification). The results of the search are presented in the PRISMA flow diagram Figure 1. Full details of the included and excluded studies are available in the Characteristics of included studies and Characteristics of excluded studies tables and are summarised below.
Included studies
Study design and setting
We included 12 studies (Bjarnason 2019; Copaci 2014; Kruis 1997; Kruis 2004; Matsuoka 2018; NCT02361957; Shanahan 2006; Vejdani 2017; Wildt 2011; Yasushi 2015; Zocco 2003; Zocco 2006). These studies were either single centre (Bjarnason 2019; Copaci 2014; NCT02361957; Shanahan 2006; Yasushi 2015; Zocco 2006), or multicentre (Kruis 1997; Kruis 2004; Matsuoka 2018; Vejdani 2017; Wildt 2011) parallel group RCTs. The studies were conducted in hospitals in Italy (Zocco 2003; Zocco 2006), Iran (Vejdani 2017), Ireland (Shanahan 2006), Japan (Yasushi 2015), the Netherlands (NCT02361957), Romania (Copaci 2014), the UK (Bjarnason 2019); multiple centres in Denmark (Wildt 2011) and Japan (Matsuoka 2018); multiple centres across Germany, the Czech Republic, Austria (Kruis 1997) and Germany, the Czech Republic, Austria, Estonia, Latvia, Lithuania, Slovak Republic, Sweden, Switzerland and the UK (Kruis 2004). In two studies (Copaci 2014; Shanahan 2006), where the setting was not explicitly stated, we have assumed this to be the authors' affiliation.
Participants
In five studies reporting mean age, the average age of participants was between 32 years in Zocco 2003 and 51 years in NCT02361957). In five studies reporting on age range, included participants were between 18 in Copaci 2014 and 88 years in Kruis 1997. Only one study (Yasushi 2015), which based on its inclusion criteria may have included paediatric patients (> 13 years). This study had an overall mean age of 43.9 +/‐ 14.8 years, therefore, it is unclear whether children were recruited. Ten out of 11 studies randomised 25 (NCT02361957) to 327 (Kruis 2004) participants. Copaci 2014 included 36 participants, some (number not stated) of which received interventions that are outside the scope of this review. The studies included male and female participants with ulcerative colitis who may or may not have been receiving medication at the time of recruitment, except for Vejdani 2017 who did not report on age and sex, making it unclear whether the study was conducted on adult and/or paediatric female and/or male patients. In 10 studies, participants had the following forms of ulcerative colitis: pancolitis, left‐sided, total colitis, proctitis, proctosigmoiditis, total colitis, subtotal colitis, distal, left colon. However, three studies did not provide any information on the extent of disease (Vejdani 2017; Wildt 2011; Zocco 2003). The length of time participants had been in remission at the point of study entry was not stated in six studies (Bjarnason 2019; Copaci 2014; NCT02361957; Shanahan 2006; Vejdani 2017; Zocco 2003), and unclear in one study (Yasushi 2015). Three studies reported at recruitment, that participants had been in remission between one month in Kruis 1997 and Matsuoka 2018 and 12 years in Kruis 1997.
Intervention
All the included studies had two trial arms, except three studies (Shanahan 2006; Zocco 2003; Zocco 2006), which had three trial arms. Copaci 2014 had three trial arms, however, one arm was excluded for assessing an intervention (prebiotic) that is not relevant to the review. The studies investigated the following comparisons.
Probiotics versus placebo (Bjarnason 2019; Matsuoka 2018; NCT02361957; Vejdani 2017; Wildt 2011; Yasushi 2015)
Probiotics versus 5‐aminosalicylic acid (5‐ASA) (mesalazine) (Kruis 2004)
Probiotics plus 5‐ASA versus 5‐ASA (Copaci 2014)
Probiotics plus 5‐ASA versus 5‐ASA plus placebo (Kruis 1997)
Probiotics versus probiotics versus placebo (Shanahan 2006)
Probiotics versus probiotics plus 5‐ASA versus 5‐ASA (Zocco 2003; Zocco 2006)
In seven studies (Copaci 2014; Kruis 1997; Kruis 2004; Shanahan 2006; Vejdani 2017; Zocco 2003; Zocco 2006), the probiotics contained single bacterial strains and probiotics in five studies contained multiple strains (Bjarnason 2019; Matsuoka 2018; NCT02361957; Wildt 2011; Yasushi 2015). These single bacterial strains include Bifidobacterium longum (B longum) W11 (Copaci 2014), Echerichia coli (E coli) Nissle 1917 (Kruis 1997; Kruis 2004), Lactobacillus salivarius (L salivarius) UCC118 (Shanahan 2006), Bifidobacterium infantis (Binfantis) 35624 (Shanahan 2006), Lactobacilluscasei (L casei) strain ATCC PTA‐3945 (Vejdani 2017), and Lactobacillus GG 18 X 109 (Zocco 2003; Zocco 2006).
In studies with multiple strain probiotics, the following combinations were studied.
Lactobacillus rhamnosus (L rhamnosus) NCIMB 30174, Lactobacillus plantarum (L plantarum) NCIMB 30173, Lactobacillus acidophilus (L acidophilus) NCIMB 30175 and Enterococcus faecium (E faecium) NCIMB 30176 (Bjarnason 2019).
Bifidobacterium bifidum (B bifidum) W23, Bifidobacterium lactis (B lactis) W51, Bifidobacterium lactis (B lactis) W52, L acidophilus W22, L casei W56, Lactobacillus paracasei (L paracasei) W20, Lactobacillus plantarum (L plantarum) W62, L salivarius W24 and Lactococcus lactis (L lactis) W19 (NCT02361957).
Bifidobacteriumbreve (B breve) and L acidophilus (Matsuoka 2018).
L acidophilus strain La‐5 + Bifidobacterium animalis (B animalis) subsp. lactis strain BB‐12 (Wildt 2011).
Streptococcus faecalis (Sfaecalis) T‐110 (lactomin) + Clostridium butyricum TO‐A + Bacillus mesentericus (Yasushi 2015).
Interventions were administered daily for four weeks in Bjarnason 2019 to 52 weeks (Kruis 2004; Shanahan 2006; Wildt 2011; Yasushi 2015; Zocco 2003; Zocco 2006). Concomittant treatments were not allowed in three studies (Kruis 2004; Wildt 2011; Zocco 2006), and in five studies it was not explicitly stated whether concomitant treatments were used or not. In four studies different concomitant treatments were used, such as 5‐aminosalycilic preparation, low‐dose azathioprine (1 mg/kg) and prednisolone < 4 mg/day (Bjarnason 2019), 2.4 g per day of mesalazine (NCT02361957), aminosalicylate (Shanahan 2006), unrestricted mesalazine and salazosulfapyridine plus topical antibiotics were not restricted (Yasushi 2015).
Outcomes
The studies reported data on all outcomes of interest except 'need for withdrawal of therapy'. We summarised outcome data in Table 4.
1. Outcome data table.
| Study ID | Number of relapses | Definition of relapse | Maintenance of remission | Quality of life | Serious adverse events | Withdrawal due to adverse events |
| Bjarnason 2019 | 0 versus 4 | NR | NR | 7.9 +/‐ 2.8 versus 8.0 +/‐ 2.5 | None | None |
| NCT02361957 | 0/13 versus 1/12; 0/13 versus 2/12 |
Relapse was defined as a flare‐up | NR | 3.5 +/‐ 0.7 versus 4.2 +/‐ 1.5 | NR | NR |
| Copaci 2014 | 30% versus 28% | NR | 77% versus 90% | NR | NR | NR |
| Kruis 1997 | 8/50 versus 6/53; 18/60 versus 13/60 |
CAI > 4 | NR | NR | NR | 2/50 versus 1/53 |
| Kruis 2004 | 40/110 versus 38/112; 92/162 versus 91/165 | The presence of all of the following: CAI > 6 (or an increase in CAI of at least 3 points with CAI = 4 being exceeded at the same time); endoscopic index > 4; histological signs of acute inflammation | NR | 24.3 +/‐ 5.2 versus 25.1 +/‐ 3.9 | 7/162 versus 6/165 | 11/110 versus11/112; 63/162 versus 64/165 |
| Matsuoka 2018 | 22/97 versus 19/95 55/98 versus 58/97 |
The persistence of a rectal bleeding score of ≥ 2 on Sutherland DAI score for 3 consecutive days and/or initiation of remission induction therapy for worsening of UC | Reported P = 0.643 | NR | 0* | 0/97 versus 2/95 |
| Shanahan 2006 | NR | Defined as < 3 bowel movements per day (without frank/gross blood) out of 7 | NR | NR | NR | NR |
| Vejdani 2017 | 2/14 versus 4/15; 4/14 versus 7/15 |
An increase in bowel frequency with blood for at least 1 week. A colonoscopy was performed and biopsies were taken to confirm relapse | NR | NR | 0 | NR |
| Wildt 2011 | 15/20 versus 11/12 | SCCAI score > 4 and/or endoscopic changes grade 2–3 | 5/20 versus 1/12 | NR | 0/20 versus 0/12 | 0/20 versus 0/12 |
| Yasushi 2015 | 7/23 versus 10/23; 14/30 versus 17/30 |
CAI ≤ 5 | 16/23 versus 13/23 16/30 versus 13/30 |
NR | 0/23 versus 0/23 | NR |
| Zocco 2003 | 2/12 versus 2/10 versus 4/14 | Defined by clinical and endoscopic features | NR | NR | NR | 0/12 versus 0/10 versus 0/14 |
| Zocco 2006 | 10/65 (Probiotic) versus 12/60 (Mesalazine) versus 10/62 (Probiotic+Mesalazine) | The appearance of UC symptoms or an increase in CAI to more than 4 points | 55/65 versus 48/60 versus 52/62 | NR | 0/65 versus 0/60 versus 0/62 | NR |
*Serious adverse events which occurred were reportedly not related to the intervention (avascular necrosis of bilateral femoral head and pulmonary thromboembolism)
CAI: colitis activity index; DAI: disease activity index; NR: not reported; SCCAI: simple clinical colitis activity index UC: ulcerative colitis
Relapse was reported in all studies (Bjarnason 2019; Copaci 2014; Kruis 1997; Kruis 2004; Matsuoka 2018; NCT02361957; Shanahan 2006; Vejdani 2017; Wildt 2011; Yasushi 2015; Zocco 2003; Zocco 2006). Clinical relapse was reported in six studies (Bjarnason 2019; Kruis 1997; Kruis 2004; Matsuoka 2018; Yasushi 2015; Zocco 2006). In three studies, endoscopic and clinical relapse were not separated out (Vejdani 2017; Wildt 2011; Zocco 2003).
Maintenance of remission (the number of participants who did not have a relapse) was reported in five studies (Copaci 2014; Matsuoka 2018; Wildt 2011; Yasushi 2015; Zocco 2006). Maintenance of clinical remission was reported in three studies (Bjarnason 2019; Yasushi 2015; Zocco 2006).
Health related quality of life was reported in three studies (Bjarnason 2019; Kruis 2004; NCT02361957).
Serious adverse events were reported in seven studies (Bjarnason 2019; Kruis 2004; Matsuoka 2018; Vejdani 2017; Wildt 2011; Yasushi 2015; Zocco 2006), although no full description was provided. Therefore, we were unable to ascertain the severity of the adverse events.
Withdrawal due to adverse events was reported in five studies (Bjarnason 2019; Kruis 1997; Kruis 2004; Wildt 2011; Zocco 2003).
Funding and declaration of interest
The studies were government funded (Yasushi 2015), funded by manufacturing companies (Bjarnason 2019; Kruis 1997; Matsuoka 2018), part funded by industry and a charity (Wildt 2011), and part funded by government and industry (NCT02361957). The funding source was not reported in six studies (Copaci 2014; Kruis 2004; Shanahan 2006; Vejdani 2017; Zocco 2003; Zocco 2006).
Conflict of interest was not fully reported in any of the studies except Copaci 2014, in which the authors reported that they had none. Three studies reported that one author had no conflict of interest (Yasushi 2015), and two authors were funded by manufacturing companies (Bjarnason 2019; Matsuoka 2018). Two studies reported that authors were employed by a manufacturing company (NCT02361957; Wildt 2011). Conflicts of interest were not reported in five studies (Kruis 1997; Kruis 2004; Shanahan 2006; Zocco 2003; Zocco 2006).
Excluded studies
Thirty studies failed to meet the inclusion criteria and we excluded them for the following reasons.
Wrong study design: review (Do 2010), commentary piece (Faubion 2000; Folwaczny 2000), not a RCT (Henker 2008; Venturi 1999).
Wrong population: participants were not in remission at study entry (Fujimori 2009; IRCT20120415009475N5; Li 2013; Liu 2014; Miele 2009; NCT01772615; Rembacken 1999; Sanchez‐Morales 2019; Zhang 2018a), a mixed population of active and inactive ulcerative colitis (Ishikawa 2011), mixed population of ulcerative colitis and Crohn's disease (Ballini 2019; Shadnoush 2013), participants had active ulcerative colitis (NCT00951548; Palumbo 2016; Solovyeva 2014; Tursi 2010), microscopic colitis (Rohatgi 2015).
Wrong intervention (Bamba 2002).
Short duration of follow‐up (Ahmed 2013; Cui 2004).
Insufficient information on study details and no response when authors were contacted (Ishikawa 2002; NCT00268164; NCT00374725; NCT00803829; Pelech 1998).
Risk of bias in included studies
The studies were either at high or unclear risk of bias. The risk of bias for the studies is summarised in Figure 2 and Figure 3. Further details are available in the Characteristics of included studies table.
2.

Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
3.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
Allocation
Random sequence generation
In all the included studies, allocation of participants to intervention or placebo was described as random. The method of randomisation was adequately described in six studies (Bjarnason 2019; Kruis 2004; NCT02361957; Vejdani 2017; Wildt 2011; Yasushi 2015), and not described in six studies (Copaci 2014; Kruis 1997; Matsuoka 2018; Shanahan 2006; Zocco 2003; Zocco 2006). We contacted the authors of these six studies to clarify the method of randomisation, but did not receive further information. We rated these studies as unclear risk of bias for sequence generation.
Allocation concealment
We rated allocation concealment as unclear for all except two studies (Bjarnason 2019; Matsuoka 2018). We contacted the authors to clarify allocation concealment, but did not receive a response. The interventions in Matsuoka 2018 were delivered in identical containers from the central pharmacy, therefore we rated this study as low risk of bias.
Blinding
Nine of the studies were described as double‐blinded (Bjarnason 2019; Kruis 1997; Kruis 2004; Matsuoka 2018; NCT02361957; Shanahan 2006; Vejdani 2017; Wildt 2011; Yasushi 2015), and we rated them at low risk of performance bias. However, only three of these studies provided information (Bjarnason 2019; Kruis 2004; NCT02361957), which suggests that blinding was maintained until after outcome assessment. We rated all three studies at low risk of detection bias, and the remaining as unclear. Copaci 2014 and Zocco 2006 were open‐label studies and we rated them at high risk of bias. There was insufficient information in Zocco 2003 to make a decision, therefore it we rated it at unclear risk of performance and detection bias.
Incomplete outcome data
Ten studies were at low risk of bias for reporting data for all participants (Bjarnason 2019; Zocco 2003; Zocco 2006), conducting full ITT analysis (NCT02361957; Vejdani 2017; Wildt 2011), a combination of low attrition rates and partial ITT analysis (Kruis 1997; Matsuoka 2018), and two studies had attrition rates of > 20% (Kruis 2004; Yasushi 2015), but balanced between both groups. Two studies were at unclear risk of bias (Copaci 2014; Shanahan 2006).
Selective reporting
Trial registrations were available for only three studies (Matsuoka 2018; NCT02361957; Wildt 2011).
Of the seven trials which we rated at low risk of reporting bias, two reported all outcomes which were prespecified in the trial registration (NCT02361957; Wildt 2011), and five had no trial registration, but reported all expected outcomes (Bjarnason 2019; Kruis 1997; Kruis 2004; Yasushi 2015; Zocco 2006). We rated three studies at high risk of bias for reporting more outcomes than specified in the protocol (Matsuoka 2018), failing to report adverse events (Shanahan 2006), and results of biochemical tests (Vejdani 2017), Copaci 2014 and Zocco 2003 failed to provide sufficient information for a judgement to be made (unclear).
Other potential sources of bias
We rated six studies at low risk of bias for not having other apparent biases (Kruis 1997; Kruis 2004; NCT02361957; Vejdani 2017; Yasushi 2015; Zocco 2006). We rated three studies at high risk of bias due to an imbalance in baseline characteristics (Wildt 2011), a posthoc decision to discontinue the trial (Matsuoka 2018), and for being funded by the manufacturer of the probiotic product studied with no justification of the limits or level of involvement (Bjarnason 2019)
Effects of interventions
See: Table 1; Table 2; Table 3
Summary of findings 1. Probiotics compared to placebo for maintenance of remission in ulcerative colitis.
| Probiotics compared to placebo for maintenance of remission in ulcerative colitis | ||||||
| Patient or population: people with ulcerative colitis in remission Setting: hospitals Intervention: probiotics Comparison: placebo | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with placebo | Risk with probiotics | |||||
| Clinical relapse (12 to 52 weeks) |
Study population | RR 0.87 (0.63 to 1.18) | 361 (4 RCTs) | ⊕⊝⊝⊝ Very lowa | Clinical relapse was defined as a flare‐up (NCT02361957), CAI ≤ 5 (Yasushi 2015) and persistence of a rectal bleeding score of ≤ 2 on Sutherland DAI score for 3 consecutive days and/or initiation of remission induction therapy for worsening of ulcerative colitis (Matsuoka 2018), respectively | |
| 554 per 1000 | 493 per 1000 (399 to 609) | |||||
| Maintenance of clinical remission (52 weeks) |
Study population | RR 1.16 (0.98 to 1.37) | 141 (2 RCTs) | ⊕⊝⊝⊝ Very lowa | Maintenance of remission is the number of participants who did not relapse. One additional study reported insufficient data for inclusion in the meta‐analysis, therefore, we did not further analyse the results (reported P = 0.643). | |
| 400 per 1000 | 532 per 1000 (308 to 924) | |||||
| Serious adverse events (48 to 52 weeks) |
See comment | See comment | ‐ | 351 (4 RCTs) | ‐ | Four studies reported that no serious adverse events occurred. |
| Withdrawal due to adverse events | See comment | See comment | ‐ | 113 (2 RCTs) | ‐ | Two studies reported there were no withdrawals due to adverse events. |
| Need for additional therapy | Not reported in any of the studies | |||||
| Health‐related quality of life (12 weeks) |
Mean IBD‐Q score with placebo was 3.5 | MD 0.70 points lower (1.63 lower to 0.23 higher) | ‐ | 25 (1 RCT) | ⊕⊕⊝⊝ Lowb | Scale: IBD‐Q, range 1 ‐7, higher score = better quality of life |
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). CAI: colitis activity index CI: confidence interval; DAI: disease activity index; IBD‐Q: inflammatory bowel disease questionnaire; MD: mean difference; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded three times: risk of reporting bias and other bias due to imbalance in baseline characteristics, imprecision due to small sample size. bDowngraded two times: imprecision due to small sample size from a single study resulting in wide confidence interval.
Summary of findings 2. Probiotics compared to 5‐aminosalicylic acid (5‐ASA) (mesalazine) for maintenance of remission in ulcerative colitis.
| Probiotics compared to 5‐ASA (mesalazine) for maintenance of remission in ulcerative colitis | ||||||
| Patient or population: people with ulcerative colitis in remission Setting: hospitals Intervention: probiotics Comparison: 5‐ASA | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with 5‐ASA | Risk with probiotics | |||||
| Clinical relapse (52 weeks) |
Study population | RR 1.01 (0.84 to 1.22) | 452 (2 RCTs) | ⊕⊕⊝⊝ Lowa | Clinical relapse was based on the presence of all the following: CAI > 6 (or an increase in CAI of at least 3 points with CAI = 4 being exceeded at the same time); endoscopic index > 4; histological signs of acute inflammation (Kruis 2004) and appearance of ulcerative colitis symptoms or an increase in CAI to more than 4 points (Zocco 2006) | |
| 458 per 1000 | 458 per 1000 (380 to 554) | |||||
| Maintenance of clinical remission (52 weeks) |
Study population | RR 1.06 (0.90 to 1.25) | 125 (1 RCT) | ⊕⊕⊝⊝ Lowb | Maintenance of remission is the number of participants who did not relapse. | |
| 800 per 1000 | 848 per 1000 (720 to 1000) | |||||
| Serious adverse events (52 weeks) |
Study population | RR 1.19 (0.41 to 3.46) | 327 (1 RCT) | ⊕⊝⊝⊝ Verylowd | Serious adverse events were not reported in detail | |
| 36 per 1000 | 43 per 1000 (15 to 126) | |||||
| Withdrawal due to adverse events (52 weeks) |
Study population | RR 1.02 (0.46 to 2.25) | 222 (1 study) | ⊕⊝⊝⊝ Very lowe | Discontinuation of therapy was due to gastrointestinal disorders, such as bloody stools, nausea, diarrhoea, mucous secretion and abdominal pain | |
| 98 per 1000 | 100 per 1000 (45 to 221) | |||||
| Need for additional therapy | Not reported in any of the studies | |||||
| Health‐related quality of life (52 weeks) |
Mean IBD‐Q score with 5‐ASA was 24.3 points | MD 0.80 points lower (2.01 lower to 0.41 higher) | 222 (1 RCT) |
⊕⊕⊝⊝ Lowc | Scale: IBD‐Q, range 1 ‐32, higher score = better quality of life | |
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). 5‐ASA: 5‐aminosalicylic acid; CAI: colitis activity index CI: confidence interval; IBD‐Q: inflammatory bowel disease questionnaire; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded two times: risk of attrition bias and other bias due to imbalance in baseline characteristics, imprecision due to sample size not meeting the optimal information size. bDowngraded two times: risk of performance and detection bias from an open‐label study and small number of events. cDowngraded two times: risk of attrition bias and imprecision due to small sample size. dDowngraded three times: risk of attrition bias, imprecision due to small number of events from a single study resulting in wide confidence interval which includes appreciable harm. Serious adverse events were not described in detail.eDowngraded three times: risk of attrition bias, imprecision due to small number of events from a single study resulting in wide confidence interval which includes appreciable harm.
Summary of findings 3. Probiotic + 5‐aminosalicylic acid (5‐ASA) (mesalazine) compared to 5‐ASA (mesalazine) for maintenance of remission in ulcerative colitis.
| Probiotic + 5‐ASA (mesalazine) compared to 5‐ASA (mesalazine) for maintenance of remission in ulcerative colitis | ||||||
| Patient or population: people with ulcerative colitis in remission Setting: hospitals Intervention: probiotic + 5‐ASA Comparison: 5‐ASA | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with 5‐ASA | Risk with probiotic + 5‐ASA | |||||
| Clinical relapse (12 to 52 weeks) |
Study population | RR 1.11 (0.66 to 1.87) | 242 (2 RCTs) | ⊕⊝⊝⊝ Very lowa | Clinical relapse was defined as CAI > 4 (Kruis 1997) and appearance of ulcerative colitis symptoms or an increase in CAI to more than 4 points (Zocco 2006). | |
| 208 per 1000 | 229 per 1000 (144 to 371) | |||||
| Maintenance of clinical remission (24 to 52 weeks) |
Study population | RR 1.05 (0.89 to 1.24) | 122 (1 RCT) | ⊕⊕⊝⊝ Lowb | Maintenance of clinical remission is the number of participants who did not relapse. | |
| 800 per 1000 | 840 per 1000 (712 to 992) | |||||
| Serious adverse events | Not reported in any of the studies | |||||
| Withdrawal due to adverse events (12 to 52 weeks) |
Study population | RR 5.29 (0.26 to 107.63) |
127 (2 RCTs) | ⊕⊝⊝⊝ Very lowc | Two discontinuations in the probiotic arm were due to avascular necrosis of bilateral femoral head and pulmonary thromboembolism. One study (n = 24) reported no events in either arm. |
|
| See comment | See comment | |||||
| Need for additional therapy | Not reported in any of the studies | |||||
| Health‐related quality of life | Not reported in any of the studies | |||||
| *The risk in the intervention group (and its 95% confidence interval) is based on the mean risk in the comparison group and the relative effect of the intervention (and its 95% CI). 5‐ASA: 5‐aminosalicylic acid; CAI: Colitis activity index CI: confidence interval; RCT: randomised controlled trial; RR: risk ratio | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | ||||||
aDowngraded three times: risk of attrition bias, imprecision due to small number of events and confidence interval which includes appreciable harm. bDowngraded two times: risk of performance and detection bias from an open‐label study, imprecision due to small number of events. cDowngraded three times: unclear risk of selection bias (lack of information on sequence generation), imprecision due to small number of events in a single study and confidence interval which include appreciable harm.
Probiotics versus placebo
Seven studies compared probiotics with placebo (Bjarnason 2019; Matsuoka 2018; NCT02361957; Shanahan 2006; Vejdani 2017; Wildt 2011; Yasushi 2015). See Table 1.
Primary outcome
Clinical relapse
We found very low‐certainty evidence that, on average, there was no clear difference in the incidence of clinical relapse between probiotics and placebo (risk ratio (RR) 0.87, 95% confidence interval (CI) 0.63 to 1.18; 4 studies, 361 participants; very low‐certainty evidence; Analysis 1.1, Figure 4). We downgraded the evidence three times for high risk of reporting and other bias due to imbalance in baseline characteristics, and imprecision due to small sample size.
1.1. Analysis.

Comparison 1: Probiotics versus placebo, Outcome 1: Clinical relapse
4.

Forest plot of comparison: 1 Probiotics versus placebo, outcome: 1.1 Clinical relapse.
Two other studies also reported on relapse (Vejdani 2017; Wildt 2011). In these studies, relapse data appear to have included a mix of endoscopic and clinical relapse. Vejdani 2017 defines relapse as: an increase in bowel frequency with blood for at least one week and a colonoscopy and biopsies to confirm relapse. Wildt 2011 defines relapse as: simple clinical colitis activity index (SCCAI) score > 4 and/or endoscopic changes grade 2 to 3. Due to concerns about clinical heterogeneity, we did not analyse the data. Number of relapses in the probiotics compared to the placebo group were 4/14 (28.6%) versus 7/15 (46.7%) in Vejdani 2017 and 15/20 (75%) versus 11/12 (91.7%) in Wildt 2011.
Maintenance of clinical remission
The number of participants who remained in clinical remission, i.e. did not have a relapse, was reported in three studies. It is uncertain whether probiotics lead to a difference in maintenance of remission when compared with placebo (RR 1.16, 95% CI 0.98 to 1.37; 2 studies, 141 participants; very low‐certainty of evidence; Analysis 1.2). We downgraded the evidence three times for high risk of bias and imprecision due to wide CIs, which includes appreciable harm. One additional study with 205 participants (Matsuoka 2018), reported insufficient data for inclusion in the meta‐analysis; we did not analyse the results further.
1.2. Analysis.

Comparison 1: Probiotics versus placebo, Outcome 2: Maintenance of clinical remission
Wildt 2011 reported on the number of participants who remained in remission, however, the definition of the relapse suggests that the data potentially includes participants in endoscopic and clinical remission. The number of people on probiotics who remained in remission compared to those on placebo were 5/20 (25%) versus 1/12 (8.3%), respectively.
Secondary outcomes
Serious adverse events
In four studies with 351 participants which reported on serious adverse events, no events were recorded (Analysis 1.3, Figure 5).
1.3. Analysis.

Comparison 1: Probiotics versus placebo, Outcome 3: Serious adverse events
5.

Forest plot of comparison: 1 Probiotics versus placebo, outcome: 1.3 Serious adverse events.
Withdrawal due to adverse events
Two studies with 113 participants indicated that there were no withdrawals as a result of adverse events (Bjarnason 2019; Wildt 2011).
Need for additional therapy
This outcome was not reported.
Health‐related quality of life
Health‐related quality of life was reported in two studies and measured using the inflammatory bowel disease questionnaire (IBD‐Q) scale in one of them (NCT02361957), and the UK IBD‐Q in the other one (Bjarnason 2019). The IBD‐Q scale ranges from 1 to 7, with a higher score representing better quality of life. We found low‐certainty evidence that, on average, probiotics made no clear difference in health‐related quality of life compared with placebo (mean difference (MD) ‐0.70, 95% CI ‐1.63 to 0.23; 1 study, 25 participants; low‐certainty evidence; Analysis 1.5). We downgraded the evidence twice for imprecision due to inadequate sample size from a single study with wide CIs. The UK IBD‐Q is similar, however, the authors that used it reported separately on the five overall parameters of the questionnaire (emotional symptoms, bowel function‐1, social function, bowel function‐2, systemic function). As there was no overall score reported, we could not include a quality of life value in our meta‐analysis.
1.5. Analysis.

Comparison 1: Probiotics versus placebo, Outcome 5: Health‐related quality of life
Probiotics versus 5‐aminosalicylic acid (5‐ASA) (mesalazine)
Three trials compared probiotics with 5‐ASA (Kruis 2004; Zocco 2003; Zocco 2006). See Table 2.
Primary outcome
Clinical relapse
We found low‐certainty evidence that, on average, there was no clear difference in the incidence of relapse between probiotics and 5‐ASA (RR 1.01, 95% CI 0.84 to 1.22; 2 studies, 452 participants; low‐certainty evidence; Analysis 2.1). We downgraded the evidence twice for high risk of bias and imprecision due to the inadequate sample size.
2.1. Analysis.

Comparison 2: Probiotics versus 5‐aminosalicylic acid (5‐ASA) (mesalazine), Outcome 1: Clinical relapse
In Zocco 2003, relapse was defined "by clinical and endoscopic features". Due to the heterogeneity, we decided not to analyse the data. The number of relapses in the probiotics versus placebo group were 2/12 (16.7%) versus 2/10 (20%), respectively.
Maintenance of clinical remission
We found low‐certainty evidence that, on average, probiotics showed no clear difference in maintenance of clinical remission when compared with 5‐ASA (RR 1.06, 95% CI 0.90 to 1.25; 1 study, 125 participants; low‐certainty evidence; Analysis 2.2). We downgraded the evidence twice for high risk of bias and imprecision due to a small number of events.
2.2. Analysis.

Comparison 2: Probiotics versus 5‐aminosalicylic acid (5‐ASA) (mesalazine), Outcome 2: Maintenance of clinical remission
Secondary outcomes
Serious adverse events
It is uncertain whether probiotics lead to a difference in serious adverse events when compared with 5‐ASA (RR 1.19, 95% CI 0.41 to 3.46; 1 study, 327 participants; very low‐certainty evidence; Analysis 2.3). We downgraded the evidence three times for high risk of bias and imprecision due to the small number of events and wide confidence interval, which includes appreciable harm.
2.3. Analysis.

Comparison 2: Probiotics versus 5‐aminosalicylic acid (5‐ASA) (mesalazine), Outcome 3: Serious adverse events
Withdrawal due to adverse events
It is uncertain whether probiotics lead to a difference in serious adverse events when compared with 5‐ASA (RR 1.02, 95% CI 0.46 to 2.25; 1 study, 222 participants; very low‐certainty evidence; Analysis 2.4). We downgraded the evidence three times for high risk of bias and imprecision due to the small number of events in a single study and wide confidence interval, which includes appreciable harm.
2.4. Analysis.

Comparison 2: Probiotics versus 5‐aminosalicylic acid (5‐ASA) (mesalazine), Outcome 4: Withdrawal due to adverse events
Need for additional therapy
This outcome was not reported.
Health‐related quality of life
One study reported quality of life scores at 12 months based on the IBDQ scale, ranging from 0 to 32, with a higher score representing a better quality of life (Kruis 2004). We found low‐certainty evidence that there was no clear difference in health‐related quality of life between probiotics and 5‐ASA (MD ‐0.80, 95% CI ‐2.01 to 0.41; 1 study, 222 participants; low‐certainty evidence Analysis 2.5). We downgraded the evidence twice for high risk of bias and imprecision due to small sample size.
2.5. Analysis.

Comparison 2: Probiotics versus 5‐aminosalicylic acid (5‐ASA) (mesalazine), Outcome 5: Health‐related quality of life
Probiotic + 5‐ASA (mesalazine) versus 5‐ASA (mesalazine)
Four trials compared a probiotic plus 5‐ASA with 5‐ASA alone (Copaci 2014; Kruis 1997; Zocco 2003; Zocco 2006). See Table 3.
Primary outcome
Clinical relapse
It is uncertain whether probiotics combined with 5‐ASA leads to a difference in the incidence of relapse when compared with 5‐ASA alone (RR 1.11, 95% CI 0.66 to 1.87; 2 studies, 242 participants; very low‐certainty evidence; Analysis 3.1). We downgraded the evidence three times for high risk of bias and imprecision due to the small number of events and confidence interval, which includes appreciable benefit or harm.
3.1. Analysis.

Comparison 3: Probiotic + 5‐aminosalicylic acid (5‐ASA) (mesalazine) versus 5‐ASA (mesalazine), Outcome 1: Clinical relapse
In Zocco 2003, relapse was defined "by clinical and endoscopic features". Due to the heterogeneity, we were unable to analyse the data. The number of relapses which occurred in the probiotics and 5‐ASA group compared to 5‐ASA alone was 4/14 (28.6%) versus 2/10 (20%).
Maintenance of clinical remission
The number of participants who remained in remission, i.e. did not have a relapse, was reported in two studies. We found low‐certainty evidence that, on average, probiotics combined with and 5‐ASA showed no clear difference in maintenance of remission compared with 5‐ASA alone (RR 1.05, 95% CI 0.89 to 1.24; 1 study, 122 participants; Analysis 3.2). We downgraded the evidence twice for high risk of bias and imprecision due to the small number of events.
3.2. Analysis.

Comparison 3: Probiotic + 5‐aminosalicylic acid (5‐ASA) (mesalazine) versus 5‐ASA (mesalazine), Outcome 2: Maintenance of clinical remission
Secondary outcomes
Serious adverse events
This outcome was not reported.
Withdrawal due to adverse events
It is uncertain whether probiotics combined with 5‐ASA leads to a difference in withdrawal due to adverse events compared with 5‐ASA alone because the certainty of the evidence is very low. One study reported there were no withdrawals due to adverse events and one study reported two withdrawals in the probiotics combined with 5‐ASA group (RR 5.29, 95% CI 0.26 to 107.63; 2 studies, 127 participants; very low‐certainty evidence; Analysis 3.3). We downgraded the evidence three times for unclear risk of selection bias, small number of events and wide confidence interval, which includes appreciable harm.
3.3. Analysis.

Comparison 3: Probiotic + 5‐aminosalicylic acid (5‐ASA) (mesalazine) versus 5‐ASA (mesalazine), Outcome 3: Withdrawal due to serious adverse events
Need for additional therapy
This outcome was not reported.
Health‐related quality of life
This outcome was not reported.
Sensitivity analysis
We carried out sensitivity analyses using an available case analysis versus intention‐to‐treat (ITT) analysis as well as fixed‐effect versus random‐effects models. We did not find any differences between either set of analyses. See full data in Table 5.
2. Sensitivity analysis.
| Outcome | Fixed‐effect | Random‐effects |
| Probiotics versus placebo | ||
| Clinical relapse | RR 0.85, 95% CI 0.68 to 1.05 | RR 0.87, 95% CI 0.63 to 1.18 |
| Maintenace of clinical remission | RR 1.16, 95% CI 0.98 to 1.37 | RR 1.11, 95% CI 0.99 to 1.24 |
| Probiotics versus 5‐ASA | ||
| Clinical relapse | RR 1.00, 95% CI 0.83 to 1.21 | RR 1.01, 95% CI 0.84 to 1.22 |
| Maintenace of clinical remission | RR 1.06, 95% CI 0.90 to 1.25 | RR 1.06, 95% CI 0.90 to 1.25 |
| Probiotics + 5‐ASA versus 5‐ASA | ||
| Clinical relapse | RR 1.10, 95% CI 0.69 to 1.78 | RR 1.11, 95% CI 0.66 to 1.87 |
| Maintenance of clinical remission | RR 1.05, 95% CI 0.89 to 1.24 | RR 1.05, 95% CI 0.89 to 1.24 |
5‐ASA: 5‐aminosalicylic acid; CI: confidence interval; RR: risk ratio
Discussion
Summary of main results
This review included 11 parallel group randomised controlled trials (RCTs) assessing the effectiveness of probiotics for the maintenance of remission in ulcerative colitis. All the studies, except two (Copaci 2014; Shanahan 2006), provided sufficient data for inclusion in a meta‐analysis. The comparisons assessed by the studies were probiotics versus placebo, probiotics versus 5‐aminosalicylic acid (5‐ASA) and probiotic plus 5‐ASA versus 5‐ASA. We analysed and summarised data from nine studies (1031 participants): Table 1; Table 2; Table 3. It is uncertain if there is any difference in occurrence of clinical relapse when probiotics are compared with placebo (very low‐certainty evidence). When probiotics were compared with 5‐ASA, there was no clear difference in relapse (low‐certainty evidence). It is uncertain whether probiotics lead to a difference in maintenance of remission when compared with placebo because the certainty of the evidence is very low. There is no clear difference in maintenance of remission when probiotics are compared with 5‐ASA, neither is there a difference when probiotics combined with 5‐ASA is compared with 5‐ASA alone (low‐certainty evidence). It is uncertain whether probiotics combined with 5‐ASA leads to a difference in the incidence of relapse when compared with 5‐ASA alone because the certainty of the evidence is very low.
The studies comparing probiotics with placebo reported that no serious adverse events occurred. One study comparing probiotics and 5‐ASA reported on similar numbers of serious adverse events in both groups. Further details were not provided on these serious adverse events.
No difference in efficacy was found between probiotics and placebo, which could reflect the clinical truth of no efficacy regarding these agents. However, no difference was found between probiotics and 5‐ASA either. This is key, as 5‐ASA are generally used as standard first‐line interventional therapy, with their efficacy well demonstrated in previous systematic reviews (Wang 2016). As such, given the lack of efficacy of probiotics compared with placebo, it would be expected that they would be inferior to 5‐ASA as standard therapy, which has not been demonstrated. We do not have enough evidence in this current synthesis to demonstrate the efficacy of probiotics, but feel these inconsistencies raise genuine questions for clinicians, researchers and users in the field.
Overall completeness and applicability of evidence
The capricious body of evidence synthesised in this review is highly heterogenous in terms of population and intervention, and as such, significantly limits its applicability to guide decision making. In considering application of the evidence, clinicians and patients require not just statistically significant results; the results need to reflect specific clinical contexts and problems for which they can apply these solutions. It is particularly striking that on updating this review after almost 10 years, the body of evidence has grown but is still far from complete and unable to be applied to practice.
The studies involved a wide range of people who had been in remission for various lengths (> 1 month to 12 years), but as recruiting studies ubiquitously made such judgements on clinical grounds, with the addition of activity scores, consideration of concepts, such as 'deep remission', which are key in practice, is completely absent from the discourse in these trials. The weaknesses of the primary studies have not allowed exploration of such wide ranging participant characteristics through subgroup analysis, which would be key for implementation of any findings from such a review.
There was minimal consideration of children in included studies, with all except Yasushi 2015 recruiting only adults. Based on its inclusion criteria, Yasushi 2015 attempted to recruit both adult and paediatric patients, but it is not clear if they actually achieved this, treating them as one population. As such, the applicability of this evidence to paediatric patients is a significant concern. Furthermore, almost half of the studies excluded participants who were receiving immunosuppressants at the point of recruitment, suggesting a preference for people with mild disease severity. This should be considered in applying the evidence in practice.
Study participants received probiotics which had either single or multiple strains for a maximum period of 12 to 52 weeks. Whilst it is common for reviews within Cochrane and the wider field to synthesis evidence that considers probiotics as a single interventional group, subgroup analysis is key for what are effectively a disparate family of interventional agents, and once again the limitations of the evidence in this review has not allowed this to be completed.
Relapse and maintenance of remission were reported in most of the studies. However, most of the secondary outcomes were not sufficiently reported. Serious adverse events were reported, however, this outcome was not described at all in any of the studies. Health‐related quality of life and withdrawal due to adverse events were rarely reported. Need for withdrawal of therapy was not reported in any of the included studies. The effect of probiotics on these secondary outcomes remains unclear.
Certainty of the evidence
The certainty of evidence was either low or very low due to risk of bias and imprecision. Eight studies were at high risk of bias and three studies were at unclear risk of bias. Most of the studies failed to provide sufficient information on allocation concealment. Though the studies which used double‐blinding had clearly included placebo or provided control which was identical to the study intervention to prevent performance bias, it was not explicitly stated whether outcome assessment was blinded or not. Indicating that a study was double‐blinded without explicitly stating who (participants, caregiver, outcome assessor, etc.) the blinding was applied to is usually not helpful in 'Risk of bias' assessment. Five studies were published as abstracts and were at unclear risk of bias for most domains.
The studies had sample sizes of between 25 and 327 participants. We downgraded for imprecision as the trials either had small numbers of events or small sample sizes which were insufficient to meet the optimal information size, thus resulting in wide confidence intervals. Whilst power calculations were used, they were often based on estimates of effect, rather than previous trial data, and therefore this raises the question as to whether these studies were adequately powered. The definition of relapse reported in some of the studies suggests that people with endoscopic and clinical relapse or remission may have been lumped together. We carried out a narrative synthesis of such studies since they were dissimilar to the studies which clearly reported on clinical relapse only. This reduced the amount of data that were pooled for the outcome of clinical relapse/remission and increased imprecision.
Most of the analyses involved single studies. Where there was sufficient data for pooling, there was no heterogeneity (I2 = 0%). Therefore, there was no reason to downgrade for inconsistency.
There was no indirectness, as the included studies all addressed the objectives of the review and fit within the scope. The number of studies included in the meta‐analysis was insufficient to assess for publication bias.
The inconsistency within results has already been discussed, with no difference between probiotics and placebo nor probiotics and 5‐ASA (a standard treatment with proven superiority over placebo). This point is highlighted in the context of the quality issues raised, given that all but one study comparing probiotics and placebo was at high risk of bias. It is therefore likely that this is the source of the inconsistency and is a key message for future researchers.
Potential biases in the review process
We are aware of the biases that could arise from missing data and made efforts to contact authors for additional information and clarifications. However, most of the authors we contacted failed to reply. To minimise bias, we included such studies in our narrative synthesis and carried out sensitivity analyses, where possible, to provide a conservative estimate of effect. We aim to include any data which become available from authors in future updates.
Other limitations in the review process are to do with risk of bias of individual studies. Three of the included studies are only available as abstracts. This meant that the studies had to be marked at unclear risk of bias for most of the domains. Given that we did not carry out sensitivity analyses to examine their impact on the results due to the insufficient number of studies included in each meta‐analysis, the inclusion of these abstracts may further influence the validity of the data.
Finally, we are aware of the possible impact of industry funding on the validity of trial results. Funding from probiotic manufacturing companies or inclusion of company staff in the author team was noted in some of the studies and we considered the impact of this information on the 'Risk of bias' assessment of the studies and GRADE assessment of the evidence. Given that none of the studies showed a clear difference in favour of probiotics, we assumed that industry funding is unlikely to have compromised the results of this review.
Agreements and disagreements with other studies or reviews
There is currently no other known evidence‐based guidance or systematic review around the use of probiotics for the maintenance of remission in ulcerative colitis, apart from the previous version of this review (Naidoo 2011). The European Crohn's and Colitis Organisation (ECCO) and European Society of Paediatric Gastroenterology, Hepatology and Nutrition (ESPHGAN) guideline briefly described the evidence on the efficacy of probiotics and made no recommendation regarding its use for the maintenance of remission (Turner 2018). The current National Institute for Health and Care Excellence (NICE) guideline does not cover probiotics either (NICE 2013). This review has found insufficient evidence on the effect of probiotics for maintenance of remission in ulcerative colitis, and therefore retains the same conclusion from Naidoo 2011.
Authors' conclusions
Implications for practice.
The effectiveness of probiotics for the maintenance of remission in ulcerative colitis remains unclear. This is due to low‐ to very low‐certainty evidence from poorly conducted studies, which contribute limited amounts of data from a small number of participants. It is uncertain whether probiotics lead to a difference in clinical relapse and the maintenance of remission when compared with placebo (very low‐certainty evidence). Probiotics were compared with 5‐aminosalicylic acid (5‐ASA) (conventional therapy) and there was no clear difference in relapse or maintenance of remission (low‐certainty evidence). There were no serious adverse events in all but one study, which reported similar numbers across the probiotics and 5‐ASA groups, however, no further details were reported. Health‐related quality of life and withdrawal due to adverse events were rarely reported.
Implications for research.
This review highlights the need for further well‐designed randomised controlled trials (RCTs) to investigate the efficacy and safety of probiotics for the maintenance of remission in ulcerative colitis. However, we believe it is key to define contextually what the attributes of such trials should be. The majority of the trials compared probiotics with placebo. Future trials comparing probiotics with 5‐ASA would reflect conventional care given to people with ulcerative colitis. Additionally, the length of follow‐up of most studies in this review is much less than in studies assessed by other published reviews on maintenance therapy. Maintenance studies investigating treatment effects for less than 12 months are simply too short to inform clinical practice, where the attrition rates from remission are such that a minimum of one year should be considered for study. We would also strongly suggest that study investigators work to ensure the homogenous nature of their baseline populations from a disease activity standpoint, as we believe it is difficult to consider patients in remission for one month on recruitment the same as those who are 12 years into their remission. The question of sample size is also a major concern, with a minimal use of power calculations using expected effect sizes which were estimated in wide ranging ways and have led to 11 studies with a little over 1000 participants. Given other studies exhibited in other reviews in the field, particularly the high placebo response rate seen (Jairath 2017), we believe it is likely that such calculations were too optimistic in projected effect sizes, and as such, may have been underpowered to appropriately investigate the agents under study. Considering the ongoing trials, none of these appears to be of the statistical power or length of follow up to address these issues.
What's new
| Date | Event | Description |
|---|---|---|
| 4 May 2020 | Amended | Correction: Three of the included studies in this review assessed a probiotic formulation known as VSL#3. The probiotic formulation that was assessed in these studies is now known by the generic name ’De Simone Formulation’. To the best of our knowledge, there are no randomized trials that have assessed the current product known as VSL#3 in people with UC. The current product known as VSL#3 is not the same formulation as the original product invented by Professor De Simone. De Simone Formulation is available under the brand names Visbiome in the USA and Vivomixx in the EU. |
History
Protocol first published: Issue 4, 2008 Review first published: Issue 12, 2011
| Date | Event | Description |
|---|---|---|
| 29 November 2019 | New citation required but conclusions have not changed | There remains insufficient evidence for the use of probiotics in maintaining remission in ulcerative colitis. Further research against placebo is unlikely to provide useful data, and instead comparisons to other therapies is proposed. |
| 31 October 2019 | New search has been performed | We updated the searches in December 2017 and reran them in October 2019; we added eight new studies to this update. |
| 8 May 2018 | Amended | ZIE, LK and PB were added to the author team |
Acknowledgements
Partial funding for Cochrane Inflammatory Bowel Disease (IBD) (1 April 2016 to 31 March 2018) has been provided by Crohn's and Colitis Canada (CCC).
Funding for Zipporah Iheozor‐Ejiofor and partial funding for Morris Gordon was provided through the National Institute for Health Research (NIHR) Cochrane Programme Grant.
Yuhong Yuan, Information Specialist, Cochrane Upper Gastrointestinal and Pancreatic Diseases (UGPD) reran the search strategies in October 2019.
Appendices
Appendix 1. Search strategies
EMBASE
1. random$.tw.
2. factorial$.tw.
3. (crossover$ or cross over$ or cross‐over$).tw.
4. placebo$.tw.
5. single blind.mp.
6. double blind.mp.
7. triple blind.mp.
8. (singl$ adj blind$).tw.
9. (double$ adj blind$).tw.
10. (tripl$ adj blind$).tw.
11. assign$.tw.
12. allocat$.tw.
13. crossover procedure/
14. double blind procedure/
15. single blind procedure/
16. triple blind procedure/
17. randomized controlled trial/
18. or/1‐17
19. exp ulcerative colitis/
20. colitis.mp.
21. inflammatory bowel disease.mp.
22. IBD.mp.
23. UC.mp.
24. Or/19‐23
25. exp Probiotics/
26. exp Synbiotics/
27. probiotic*.tw.
28. synbiotic*.tw.
29. exp Lactobacillus/
30. lactobacill*.tw.
31. bacill*.tw.
32. exp Bifidobacterium/
33. (bifidus or bifidobacter*).tw.
34. exp Streptococcus thermophilus/
35. streptococcus thermophilus.tw.
36. streptococc*.tw.
37. exp Lactococcus/
38. lactococc*.tw.
39. Bacillus subtilis/
40. bacillus subtilis.tw.
41. exp Enterococcus/
42. exp Enterococcus faecium/ or Enterococcus faecalis/
43. exp Saccharomyces/
44. saccharomyc*.tw.
45. leuconostoc.tw.
46. pediococc*.tw.
47. bulgarian bacillus.tw.
48. (beneficial adj3 bacter*).tw.
49. (Escherichia coli or "E. coli").tw.
50. Yeast.tw.
51. (fungus or fungi).tw.
52. (VSL# 3 or VSL 3).tw.
53. Or/25‐52
54. 18 and 24 and 53
Medline
random$.tw.
factorial$.tw.
(crossover$ or cross over$ or cross‐over$).tw.
placebo$.tw.
single blind.mp.
double blind.mp.
triple blind.mp.
(singl$ adj blind$).tw.
(double$ adj blind$).tw.
(tripl$ adj blind$).tw.
assign$.tw.
allocat$.tw.
randomized controlled trial/
or/1‐13
exp ulcerative colitis/
colitis.mp.
inflammatory bowel disease.mp.
IBD.mp.
UC.mp.
Or/15‐19
exp Probiotics/
exp Synbiotics/
probiotic*.tw.
synbiotic*.tw.
exp Lactobacillus/
lactobacill*.tw.
bacill*.tw.
exp Bifidobacterium/
(bifidus or bifidobacter*).tw.
exp Streptococcus thermophilus/
streptococcus thermophilus.tw.
streptococc*.tw.
exp Lactococcus/
lactococc*.tw.
Bacillus subtilis/
bacillus subtilis.tw.
exp Enterococcus/
exp Enterococcus faecium/ or Enterococcus faecalis/
exp Saccharomyces/
saccharomyc*.tw.
leuconostoc.tw.
pediococc*.tw.
bulgarian bacillus.tw.
(beneficial adj3 bacter*).tw.
(Escherichia coli or "E. coli").tw.
Yeast.tw.
(fungus or fungi).tw.
(VSL# 3 or VSL 3).tw.
Or/21‐48
14 and 20 and 49
Cochrane CENTRAL
#1 MeSH descriptor: [Probiotics] explode all trees
#2 MeSH descriptor: [Synbiotics] explode all trees
#3 probiotic*
#4 synbiotic*
#5 MeSH descriptor: [Lactobacillus] explode all trees
#6 lactobacill*
#7 bacill*
#8 MeSH descriptor: [Bifidobacterium] explode all trees
#9 (bifidus or bifidobacter*)
#10 MeSH descriptor: [Streptococcus thermophilus] explode all trees
#11 streptococcus thermophilus
#12 streptococc*
#13 MeSH descriptor: [Lactococcus] explode all tree
#14 lactococc*
#15 MeSH descriptor: [Bacillus subtilis] explode all trees
#16 bacillus subtilis
#17 MeSH descriptor: [Enterococcus] explode all trees
#18 enterococcus faec*
#19 MeSH descriptor: [Saccharomyces] explode all trees
#20 saccharomyc*
#21 leuconostoc*
#22 pediococc*
#23 bulgarian bacillus
#24 (Escherichia coli or "E. coli").tw.
#25 Yeast.tw.
#26 (fungus or fungi).tw.
#27 Or/ #1‐ #26
#28 MeSH: [Ulcerative colitis] explode all trees
#29 UC
#30 Inflammatory bowel disease
#31 IBD
#32 #28 or #29 #30 and #31
#33 #27 and #32
The Cochrane IBD/FBD Review Specialised Trials Register
1. Probiotics and Inflammatory bowel disease
2. Probiotics and Ulcerative colitis
3. Synbiotics and Inflammatory bowel disease
4. Synbiotics and Ulcerative colitis
CINAHL
1. (TI probiotic* or AB probiotic*) OR (TI synbiotic* or AB synbiotic*) OR (TI probiotics* or AB probiotics*) OR (TI lactobacill* or AB lactobacill*) OR (TI bacill* or AB bacill*) OR (TI bifidobacter* or AB bifidobacter*) OR (TI bifidus* or AB bifidus*) OR (TI streptococc* or AB streptococc*) OR (TI lactococc* or AB lactococc*) OR (TI enterococcus* or AB enterococcus*) OR (TI saccharomyc* or AB saccharomyc*) OR (TI leuconostoc* or AB leuconostoc*) OR (TI pediococc* or AB pediococc*) OR (TI *coli or AB *coli) OR (TI yeast* or AB yeast*) OR (TI fung* or AB fung*) OR (TI VSL* or AB VSL*)
2. (TI Inflammatory bowel disease or AB Inflammatory bowel disease) OR (TI Ulcerative colitis or AB Ulcerative colitis) OR (TI UC or AB UC) OR (TI IBD or AB IBD)
3. 1 and 2
Clinical trials.gov
1. Probiotics and inflammatory bowel disease (37)
2. Probiotics and Ulcerative colitis (23)
3. Synbiotic and inflammatory bowel disease (3)
4. Synbiotic and Ulcerative colitis (1)
Data and analyses
Comparison 1. Probiotics versus placebo.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Clinical relapse | 4 | 361 | Risk Ratio (M‐H, Random, 95% CI) | 0.87 [0.63, 1.18] |
| 1.2 Maintenance of clinical remission | 2 | 141 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.16 [0.98, 1.37] |
| 1.3 Serious adverse events | 4 | 351 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.4 Withdrawal due to adverse events | 2 | 113 | Risk Ratio (M‐H, Fixed, 95% CI) | Not estimable |
| 1.5 Health‐related quality of life | 1 | 25 | Mean Difference (IV, Fixed, 95% CI) | ‐0.70 [‐1.63, 0.23] |
1.4. Analysis.

Comparison 1: Probiotics versus placebo, Outcome 4: Withdrawal due to adverse events
Comparison 2. Probiotics versus 5‐aminosalicylic acid (5‐ASA) (mesalazine).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 2.1 Clinical relapse | 2 | 452 | Risk Ratio (M‐H, Random, 95% CI) | 1.01 [0.84, 1.22] |
| 2.2 Maintenance of clinical remission | 1 | 125 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.06 [0.90, 1.25] |
| 2.3 Serious adverse events | 1 | 327 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.19 [0.41, 3.46] |
| 2.4 Withdrawal due to adverse events | 1 | 222 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.02 [0.46, 2.25] |
| 2.5 Health‐related quality of life | 1 | 222 | Mean Difference (IV, Fixed, 95% CI) | ‐0.80 [‐2.01, 0.41] |
Comparison 3. Probiotic + 5‐aminosalicylic acid (5‐ASA) (mesalazine) versus 5‐ASA (mesalazine).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 3.1 Clinical relapse | 2 | 242 | Risk Ratio (M‐H, Random, 95% CI) | 1.11 [0.66, 1.87] |
| 3.2 Maintenance of clinical remission | 1 | 122 | Risk Ratio (M‐H, Random, 95% CI) | 1.05 [0.89, 1.24] |
| 3.3 Withdrawal due to serious adverse events | 2 | 127 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.29 [0.26, 107.63] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bjarnason 2019.
| Study characteristics | ||
| Methods | RCT, double‐blind, single centre Setting: King's College Hospital Gastroenterology Clinic, London Study duration: November 2010 to October 2014 |
|
| Participants | 81 patients with UC, 61 patients with CD (total IBD = 142) Inclusion criteria: patients attending routine clinical review with established UC and CD, age 18 to 70 years, diagnosed at least 6 months prior to the trial; patients were required to have stable inactive clinical disease, as defined by < 5 points on Harvey Bradshaw (which corresponded to a score of ≤ 4 on the Truelove‐Witts criteria for UC, without a change in medication for 4 months. Patients on no treatment, maintenance treatment with a 5‐aminosalycilic preparation or low‐dose azathioprine (1 mg/kg) were eligible for inclusion in the trial. Exclusion criteria: patients on steroids (prednisolone > 4 mg/day) and biologics were excluded from the study; patients having undergone intestinal resection, patients with serious comorbidity including neurological, rheumatological, respiratory, nephrological, cardiovascular, psychiatric disease, patients with alcohol or drug addiction or dependency problems (within the last 5 years) and pregnant or lactating women; patients with previous intolerance or adverse reactions to probiotics or the use of these products within the preceeding 3 months were excluded. Age (mean +/‐ SD): probiotic UC 47.3 +/‐ 14.4, placebo UC: 43.4 +/‐ 12.1; probiotic CD: 41.2 +/‐ 13.0, placebo CD: 39.0 +/‐ 13.0 Sex: not specified Site of disease: probiotics UC: proctosigmoid 16, left‐sided 9, pancolonic 12; placebo UC: proctosigmoid 21, left‐sided 10, pancolonic 9 probiotics CD: small bowel 14, colon 11, small and large bowel 9; placebo CD: small bowel 14, colon 7, small and large bowel 7 Use of medication: probiotics UC: 5‐ASA 31, azathioprine 2, prednisolone 1, none 7 placebo UC: 5‐ASA 33, azathioprine 2, prednisolone 0, none 6 probiotics CD: 5‐ASA 15, azathioprine 4, prednisolone 1, none 13 placebo CD: 5‐ASA 12, azathioprine 2, prednisolone 0, none 15 Length of time remission at study entry: not specified Number randomised: total probiotic: 73, total placebo: 70; probiotic UC: 40, placebo UC: 41; probiotic CD: 33, placebo CD: 29 Number assessed: all randomised completed the study Postrandomisation exclusion: 0 No significant side effects were reported and the probiotic was well‐tolerated by everyone |
|
| Interventions | Follow‐up: 4 weeks IV: Symprove (Symprove Ltd. Farnham, Surrey UK), a dietary food supplement which contains 4 strains of bacteria (Lactobacillus rhamnosus NCIMB 30174, Lactobacillus plantarum NCIMB 30173, Lactobacillus acidophilus NCIMB 30175 and Enterococcus faecium NCIMB 30176), in a water‐based suspension of barley extract with each 50 mL/dose containing about 10 billion live bacteria. Control: patients received placebo, which was an identical liquid in appearance and taste, containing water and flavouring and was provided in identical packaging supplied by the manufacturers identified by a trial batch and code number only. Patients were asked to keep the study medication refrigerated between 2 °C and 7 °C and to self‐administer 1 mL/kg each morning on a fasting stomach. Foods and fluids were allowed 20 min later. Missed does could be taken later during the day provided that no food had been consumed during the preceding 3 hours. |
|
| Outcomes |
Primary efficacy outcome: difference in overall change in the IBD QoL questionnaire results at week 4 Secondary measures: the differences in clinical disease activity scores between active and placebo treatment and changes in laboratory measures including FCAL (Ek‐CAL, Buhlmann, Switzerland) |
|
| Notes | Funding and conflict of interest: supported by an unreserved research grant from Symprove Limited, the manufacturers of the probiotic Symprove to King's College Hospital. They also provided the probiotic used in the trial and a matching placebo free of charge. Prof Bjarnason has received financial support from Symprove Ltd for travel expenses to scientific meetings. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Study participants were randomised using a two‐stage computerised randomisation protocol provided by the Department of Pharmacy at King's College Hospital" |
| Allocation concealment (selection bias) | Low risk | It is explained that preparations were identical liquids in appearance and taste, provided in identical packaging supplied by the manufacturers, identified by a trial batch and code number only, however no other information on allocation concealment are provided |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Blinding of allocation to treatment was maintained until the completed study database was locked and passed over to an independent study statistician". Double‐blinding. Preparations were identical liquids in appearance and taste, provided in identical packaging supplied by the manufacturers, identified by a trial batch and code number only |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Blinding of allocation to treatment was maintained until the completed study database was locked and passed over to an independent study statistician" |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All reported |
| Selective reporting (reporting bias) | Low risk | All reported |
| Other bias | High risk | The study was funded by the manufacturers of the probiotics product studied in this article and the lead author has received financial support from the same company. |
Copaci 2014.
| Study characteristics | ||
| Methods | Open‐label, parallel group, randomised clinical trial (abstract only) Setting: not stated, however authors' affiliation ‐ Fundini clinical institute, Bucharest, Romania Study period: not stated |
|
| Participants |
Inclusion criteria: people with UC in remission for over 3 months Exclusion criteria: not stated Age (range): 18 to 65 years Sex: not stated Site of disease: ? (total colitis), ? (left‐sided colitis) Use of medication: not stated Length of time remission at study entry: not stated Number randomised (n = 36):? (probiotic + mesalamine)/? (mesalamine + prebiotic)*/? (mesalamine) Number assessed: ? (probiotic + mesalamine)/? (mesalamine + prebiotic)*/? (mesalamine) Postrandomisation exclusion: not stated |
|
| Interventions |
|
|
| Outcomes |
Duration of follow‐up: 24 weeks
|
|
| Notes |
Funding source: not stated Declaration of interest: reported, none declared *Disregarded prebiotic data for not being within the scope of the review |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Open‐label, parallel group, randomized clinical trial". Comment: not adequately described |
| Allocation concealment (selection bias) | Unclear risk | Not adequately described |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Open‐label, parallel group, randomized clinical trial" Comment: there was no blinding of participants and personnel |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Open‐label, parallel group, randomized clinical trial" Comment: no blinding |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Not adequately reported |
| Selective reporting (reporting bias) | Unclear risk | Symptoms were monitored using a gastrointestinal symptom rating scale, however, the results were not fully reported |
| Other bias | Unclear risk | Not adequately described |
Kruis 1997.
| Study characteristics | ||
| Methods | Double‐blind, multicentre RCT Setting: outpatient hospitals and private practices in Germany, the Czech Republic and Austria Study period: not stated |
|
| Participants |
Inclusion: age > 17 years; presence of chronic UC currently in remission (defined by CAI score) Exclusion: active UC, infectious colitis, existing or intended pregnancy, any other medication for UC besides the study drugs, antibiotics or suphonamides, substantial cardiac, hepatic or renal disease, major operations on the bowels, and known intolerance to salicylates Age* (range): 19 to 88 years Sex* (M/F): 55/48 Site of disease*: 28 (proctitis); 40 (proctosigmoiditis); 19 (left‐sided colitis); 18 (total/subtotal colitis) Use of medication*: 82 (salicylates); 25 (corticosteroids) Length of time remission at study entry: 14 (1 to 147 (probiotic)/12 (1 to 60) months (mesalazine) Number randomised (n = 120): 60? (probiotics)/60? (mesalazine) Number assessed: 50 (probiotics)/53 (mesalazine) Postrandomisation exclusion: 2 ‐ not started taking study medication, 15 ‐ had CAI of > 4 (8 versus 7) |
|
| Interventions |
|
|
| Outcomes |
Duration of follow‐up: 12 weeks (in one centre the total study period was 24 weeks)
|
|
| Notes |
Funding source: supported by Ardeypharm GmbH, Herdecke, Germany Declaration of interest: not reported. *Baseline characteristics reported do not account for participants who were excluded postrandomisation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were reportedly randomised, however, the method of randomisation was not adequately described |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Described as double‐blind double‐dummy. Both intervention arms included placebos. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Described as double‐blind double‐dummy, however, there was no specific information as to whether outcome assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis (modified ITT) was partially applied as it failed to account for participants who were excluded postrandomisation. However, number and reasons for postrandomisation exclusion appear to have been equal across groups (16% versus 11%) |
| Selective reporting (reporting bias) | Low risk | Trial registration was not available, however, all expected outcomes were reported |
| Other bias | Low risk | No other apparent biases |
Kruis 2004.
| Study characteristics | ||
| Methods | Double‐blind, multicentre RCT Setting: 60 hospitals and private settings in 10 European countries (Austria, Czech Republic, Estonia, Germany, Latvia, Lithuania, Slovak Republic, Sweden, Switzerland, UK) Study period: not stated |
|
| Participants |
Inclusion: age 18 to 70; UC in remission (CAI ≤ 4, endoscopic index ≤ 4 and no sign of acute inflammation on histological examination); at least two acute attacks of UC prior to study; time since last relapse: < 12 months Exclusion: active UC; proctitis with up to 10 cm proximal spread; Crohn's disease, infectious colitis; severe accompanying illnesses or major colonic surgery; use of antibiotics, sulphonamides, steroids or other therapies for UC at entry into trial; administration of study intervention drug within the previous six months before trial entry; known intolerance to salicylates Age: 19 to 82 years Sex (M/F): 179/148 Site of disease: 61 (sub/total); 62 (left‐sided); 190 (distal) Use of medication: 235 (oral salicylates ‐ partly combined with steroids) Length of time remission at study entry: < 4 (probiotic)/< 3 months (mesalazine) Number randomised (n = 327): 162 (probiotic)/165 (mesalazine) Number assessed: 162 (probiotic)/165 (mesalazine) Postrandomisation exclusion*: 2 ‐ deterioration of disease excluding relapse; 6 ‐ newly emerged exclusion criterion during study; 22 ‐ patient's request; 9 ‐ adverse events; 12 ‐ insufficient patient compliance; 9 ‐ insufficient patient co‐operation; 7 ‐ dropped out; 3 ‐ other; premature discontinuation ‐ 39 |
|
| Interventions |
No concomitant medication for UC was allowed throughout the study |
|
| Outcomes |
Duration of follow‐up: 12 months
|
|
| Notes |
Funding source: not stated Declaration of interest: not reported *some participants may have had multiple reasons for being excluded |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Randomisation was carried out in a double blind manner in blocks of four patients using 1:1 allocation to the two treatment groups. Only complete blocks of random numbers were used for each centre. If patients were eligible for study entry, they were assigned to random numbers ( = patient numbers) in ascending order within each centre according to the chronological order of their randomisation and were given the corresponding study medication." Comment: adequately described |
| Allocation concealment (selection bias) | Unclear risk | Confirmed via correspondence (quote): "Since Mutaflor and Mesalazine have a different dosage form (capsule vs. tablet), the double‐dummy method was used to ensure double‐blindness, i.e. a patient allocated to the test group was given Mutaflor verum and Mesalazine placebo, whereas a patient allocated to the control group was given Mesalazine verum and Mutaflor placebo)" Comment: unclear whether study interventions were provided in identical sequentially numbered containers |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Described as double‐blind and double‐dummy |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Before unblinding the study, a steering committee assessed protocol violations in 105/327 (32.1%) patients." Comment: blinding appears to have been maintained until after outcomes were assessed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | High attrition, but balanced between the two groups. |
| Selective reporting (reporting bias) | Low risk | Trial registration not available, however, all measured outcomes were reported |
| Other bias | Low risk | Quote: "The two patient groups were matched with regard to demographic, clinical, and pretreatment characteristics" Comment: no other apparent biases |
Matsuoka 2018.
| Study characteristics | ||
| Methods | Double‐blind, parallel group, Multicentre RCT Setting: Keio University School of Medicine; Tokyo Yamate Medical Center, Center for Infammatory Bowel Disease; Toho University Medical Center, Sakura Hospital; Kitasato University Hospital; Yokohama City University Medical Center, Infammatory Bowel Disease Center; Kannai‐Suzuki Clinic; and Matsushima Clinic, Japan Study period: April 2012 to September 2013 |
|
| Participants |
Inclusion: diagnosed with UC, in remission, age 20 to 70, worsening symptoms within 2 years, defined as one or more of the following criteria:
Exclusion:
Age: 20 to 70 years Sex (M/F): 100/92 Site of disease: 100 (pancolitis); 92 (left‐sided colitis) Use of medication: 190 (5‐ASA) Length of time remission at study entry (mean/range): 362.7 (54 to 750) ‐ probiotic/378.6 (41 to 846) days ‐ placebo Number randomised (n = 195)*: 98 (probiotics)/97 (placebo) Number assessed: 97 (probiotics)/95 (placebo) Postrandomisation exclusion**: 67 ‐ discontinuation of protocol specified treatment, 10 ‐ prohibited concomitant treatment, 2 ‐ adverse events, 13 ‐ discontinuation of study beverage, 1 ‐ other |
|
| Interventions |
All participants received their allocated treatment for 48 Weeks |
|
| Outcomes |
Duration of follow‐up: 48 weeks
|
|
| Notes |
Funding source: "This work was supported by Yakult Honsha Co., Ltd." Declaration of interest: reported; Takanori Kanai received a financial donation from Yakult. Yasuo Suzuki, Toshifumi Hibi, Yukari Uemura, Kaoru Yokoyama, Naoki Yoshimura, Reiko Kunisaki, and Katsuyoshi Matsuoka have no conflicts of interest to declare *Statistical power calculated 300 in each intervention arm needed. However, study split into Period 1 and Period 2. Only period 1 conducted ‐ this used 97 in intervention and 95 in control **Some participants discontinued for multiple reasons |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patient data were sent to the registration center via facsimile, where randomization was implemented by the central registration method. A statistician determined the algorithm of allocation. Patients were randomly allocated to the BFM group or placebo group at a ratio of 1:1 by dynamic allocation with the following randomization factors: age (≥ 40 years/12 weeks), study site (each study site), and compliance with 5‐ASA" Comment: algorithm was determined by a statistician based on age, study site and compliance with 5‐ASA as opposed to a computer |
| Allocation concealment (selection bias) | Low risk | Quote: "The study beverage and placebo beverage were packaged to be indistinguishable in appearance from each other and were delivered from the distribution center based on the allocation results at the time of enrolment. The distribution center, which was not informed of the groups to which patients were allocated, delivered the study beverage according to the provided numbers; this maintained blindness of the study." Comment: participants and personnel could not foresee assignment |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "BFM and placebo consisted of 100 mL of an opaque white liquid that were identical" Comment: similar opaque liquid used |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The trial was described as double‐blinded, however, it is not clear if this includes blind outcome assessment. Though there was an independent data monitoring committee, the trial did not specifically report that they were blinded. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Data analysed based on the "full study set". This full study set does not include all participants who were randomised, however, the difference (1 versus 1) across groups and reasons appear to be balanced |
| Selective reporting (reporting bias) | High risk | Trial registration available (UMIN000007593), however, there were more outcomes reported in the trial than prespecified |
| Other bias | High risk | Quote: "The interim analysis results showed that the Bayesian predictive power was 3.7%, which was markedly lower than the reference range for study continuation (20–25%). Based on this, the Independent Data Monitoring Committee recommended discontinuation of the study, so the study was discontinued" Comment: a posthoc decision was made to discontinue the study. This was not prespecified in the protocol. |
NCT02361957.
| Study characteristics | ||
| Methods | Double‐blind, single centre RCT Setting: Hospital Gelderse Valei (Ede, The Netherlands) Study period: not stated |
|
| Participants |
Inclusion: age 18 to 65; left‐sided UC or pancolitis in clinical remission (serum concentrations of C‐reactive protein of < 10 mg/L, which was checked with a point‐of‐care CRP test, and calprotectin of < 100 μg/g during their last medical check‐up) Exclusion: history of GI surgery, diabetes mellitus, cancer; use of antibiotics during the last 3 months; current use of corticosteroids; alcohol consumption ≥ 21 servings a week for men and ≥ 14 for women; hypersensitivity to milk protein, gluten, or soy protein; currently pregnant or breastfeeding Age (mean ± SD): 51.5 ± 12.4 years Sex (M/F): 13/12 Site of disease:? (left‐sided), ? (pancolitis) Use of medication: not stated Length of time remission at study entry: not stated Number randomised (n = 25): 13 (probiotic)/12 (placebo) Number analysed: 13 (probiotic)/12 (placebo); ITT principle applied Postrandomisation exclusion: 1 ‐ prednisone prescribed for a flare‐up; 1 ‐ personal reasons |
|
| Interventions |
Duration of follow‐up: 12 weeks
Mesalazine with a maximum dose of 2.4 g/day was the only medication for UC that was permitted during the study |
|
| Outcomes |
Duration of follow‐up:
|
|
| Notes |
Funding source: funding was provided by the Dutch Ministry of Economy Affairs (IPCSFV2900) and Winclove Probiotics BV Declaration of interest: IBvdV is employee of Winclove Probiotics. Winclove develops, researches and markets probiotic food supplements |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization scheme was computer generated by Winclove using permuted blocks with block size equal to 4" Comment: adequate randomisation |
| Allocation concealment (selection bias) | Unclear risk | Quote: "It was impossible for research personnel involved with participants to adjust randomization or discern what product participants were receiving, ensuring true allocation concealment" Comment: method of allocation concealment was not adequately described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "It was impossible for research personnel involved with participants to adjust randomization or discern what product participants were receiving..." Comment: study was referred to as double‐blinded. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "It was impossible for research personnel involved with participants to adjust randomization or discern what product participants were receiving..." Comment: study was placebo‐blinded and quality of life data were recorded by the participants |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis applied |
| Selective reporting (reporting bias) | Low risk | Trial registration is available (NCT02361957) and all prespecified outcomes were reported |
| Other bias | Low risk | No other apparent biases |
Shanahan 2006.
| Study characteristics | ||
| Methods | Double‐blind, single centre RCT (abstract only) Setting: not stated Study period: not stated |
|
| Participants |
Inclusion: within one month of achieving clinical remission of UC following a documented relapse that required steroids to induce remission. Remission was defined as < 3 bowel movements/day (without frank/gross blood) out of 7, while off all steroids Exclusion: not stated Age: not stated, however, patients' demographic characteristics were similar across the three treatment groups Sex: not stated, however, patients' demographic characteristics were similar across the three treatment groups Site of disease: not stated, however, the extent of colitis which was similar across the groups was left‐sided in about one‐third, limited (proctitis) in one‐third and pancolitis in one‐third Use of medication: not stated, however, patients' demographic characteristics were similar across the three treatment groups Length of time remission at study entry: not stated Number randomised (n = 157): not stated (52/52/53?), however, there were similar numbers (52 to 53) per group Number analysed: not stated Postrandomisation exclusion: not stated |
|
| Interventions |
Each intervention was administered as a rehydrated blended yogurt powder (109 daily for one year). A stable dose of aminosalicylate was the only permitted concomitant medication for colitis |
|
| Outcomes |
Duration of follow‐up: 1 year
|
|
| Notes |
Funding source: University College Cork Declaration of interest: not stated Emailed on 7 March 2018 ‐ awaiting reply |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "a prospective, balanced, randomised, parallel group, double blind, placebo‐controlled trial..." Comment: not adequately described |
| Allocation concealment (selection bias) | Unclear risk | Not adequately described |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "...double blind, placebo‐controlled trial" |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not adequately described |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Insufficient information to make a judgement |
| Selective reporting (reporting bias) | High risk | Not adequately described; adverse events mentioned but not gone into detail. Trial registration was available (NCT00510978) |
| Other bias | Unclear risk | Insufficient information to support judgement as study was published as an abstract. |
Vejdani 2017.
| Study characteristics | ||
| Methods | Multicentre, double‐blind, randomised, placebo‐controlled trial Setting: Multicentre, Iran, private practices Study period: not stated |
|
| Participants |
Inclusion criteria: between 15 and 65 years of age, newly diagnosed or recently relapsed UC, based on clinical, endoscopic, and histological findings and had a mild to moderately active UC according to Truelove and Witts criteria and CAI ≥ 4 and ≤ 12. Additional external participants included in the maintenance of remission phase had to be in remission for less than 3 months. Exclusion criteria: substantial cardiac, renal or hepatic diseases, severe immunocompromised patients, existing or intended pregnancy or breastfeeding, regular treatment with NSAID drugs, intestinal major operation, steroid dependency, known intolerance to sulphate free preparations of mesalazine, UC exacerbated by infectious colitis, toxic megacolon, use of antibiotic within 14 days prior to first visit for more than 1 week, use of corticosteroid injection within the last 30 days, use of immunosuppressive treatment within the last 90 days and use of mesalazine enema or corton enema within the last 14 days Age (mean ± SD): not stated Sex (M/F): not stated Site of disease: not stated Use of concurrent medication: conventional medical treatment for active UC Treatment before study: not stated Length of time remission at study entry:less than three months Number randomised: 14 (probiotic), 15 (placebo) Number analysed: 14 (probiotic), 15 (placebo) Postrandomisation exclusion: 2 ‐ lost to follow‐up, 1 ‐ concurrent illness, 1 ‐ poor compliance, 1 ‐ taking antibiotics |
|
| Interventions |
Participants also received conventional medical treatment for active UC according to the severity and extension of their disease. Participants with mild proctitis, received mesalazine or sulfasalazine tablets after remission. In participants with moderate proctitis, mesalazine suppositories were stopped after remission. The rest of the drugs and their doses were kept unchanged. |
|
| Outcomes |
Duration of follow‐up: 4 months
|
|
| Notes |
Funding source: not stated Conflicts of interests: not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: “Randomisations were done using a random number table with odd numbers for probiotic and even numbers for placebo; randomisation was stratified according to the use of mesalazine or sulfasalazine and to the clinical severity of disease (mild or moderate)" Comment: use of random number table |
| Allocation concealment (selection bias) | Unclear risk | No mention in the text |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote 'Placebos were indistinguishable from the L Casei preparation' |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | The study was reportedly double‐blinded however, there is no indication that outcome assessment was blinded |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Attrition rate was over 26%, but balanced in both groups |
| Selective reporting (reporting bias) | High risk | Trial registration not available, however, biochemical tests were recorded both at entry, remission and relapse, but not reported. |
| Other bias | Low risk | Quote: "There was not a significant difference between the two groups in factors such as age, sex, disease duration and extent, smoking, education taken and clinical activity index” Comment: baseline characteristics were balanced across groups and there were no other apparent risks of bias |
Wildt 2011.
| Study characteristics | ||
| Methods | Double‐blinded, multicentre RCT Setting*: "two participating centers in Denmark" Study period: June 2004 to March 2006 |
|
| Participants |
Inclusion: age ≥ 18 years; established diagnosis of UC left‐sided disease (endoscopic changes distally to the splenic flexure) ‐ including proctitis; time since relapse > 4 weeks during stable monotherapy with 5‐ASA or no medication at all; ≥ 1 relapse within the last year. Exclusion: pregnancy (postive urine HCG) or breastfeeding; chronic liver or kidney disease; severe chronic disease of vascular or cardiopulmonary aetiology, malignancies; immunosuppressive disease or treatment; inflammatory bowel diseases besides UC, malabsorption syndromes, and former surgical procedures involving the gastrointestinal tract — with the exception of appendectomy. Treatment with azathioprine, 6‐mercaptopurine, biological immunomodifiers, and treatment with steroids within 1 month of entry. Sex (M/F): 10/22 Age (median/range): 37.5 (23 to 68) years Site of disease (location from anal valve ‐ cm): 20 (5 to 70) ‐ probiotic/22.5 (5 to 60) ‐ placebo Use of medication: 24 (5‐ASA orally, rectally and both); 1 (salazopyrine) Length of time remission at study entry: 4 (2 to 9) ‐ probiotic/5 (2 to 11) months ‐ placebo Number randomised: 20 (probiotics)/12 (placebo) Number analysed: 20 (probiotics)/12 (placebo) Postrandomisation exclusion: 1 ‐ pregnancy, however, ITT principle was applied |
|
| Interventions |
|
|
| Outcomes |
Duration of follow‐up: 52 weeks
|
|
| Notes |
Funding source: "The study was supported by grants from Chr. Hansen A/S, Hoersholm, Denmark and by grants received from P. Carl Petersens Foundation and The Danish Crohn Colitis Organisation." Declaration of interest: "one of the authors (EB) is employed at the laboratory at Chr. Hansen A/S" *Presumably Gentofte and Hvidovre Hospital, University of Copenhagen Denmark judging by authors' affiliation |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "...randomised in blocks of 6 according to a table‐generated randomisation list to receive either Probio‐Tec AB‐25 (two capsules three times daily, resulting in a total delivery of 1.5 X 10 11 CFU daily) or to receive placebo (two capsules three times daily) in a 2:1 ratio" Comment: adequate randomisation |
| Allocation concealment (selection bias) | Unclear risk | Correspondence with author: "At inclusion in the study an enclosed envelope was drawn from a batch of 6 envelopes ‐ and the randomization revealed." Comment: no information as to whether envelopes were opaque and numbered |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Placebo medication […] was identical in appearance, size and taste" Comment: adequate blinding |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Trial was referred to as double‐blinded placebo study, however, there were no details on blind outcome assessment |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | ITT analysis was applied |
| Selective reporting (reporting bias) | Low risk | Study protocol available (NCT00268164) and all prespecified outcomes were reported |
| Other bias | High risk | Comment: imbalance in baseline characteristics ‐ there were more participants receiving medication at inclusion in the intervention group compared to the control group (reported P = 0.018). |
Yasushi 2015.
| Study characteristics | ||
| Methods | Double‐blind, placebo‐controlled, single centre RCT Setting: Sakura Medical Center, Toho University, Japan Study period: not stated |
|
| Participants |
Inclusion: patients with UC in remission who were receiving treatment on an outpatient basis (UC was diagnosed in accordance with the diagnostic criteria proposed by the Survey Research Group of Intractable Inflammatory Intestinal Disorders/Specified Diseases, Japanese Ministry of Health, Labour and Welfare); 13 years or older in whom the CAI was maintained at 5 or less while receiving drugs such as mesalazine, salazosulfapyridine, or steroids, with no change in treatment regimens within 4 weeks before study entry. Exclusion: serious cardiac disease, serious renal disease, hypotension (systolic blood pressure, ≤ 80 mmHg), a history of shock during extracorporeal circulation, serious infections such as sepsis or pneumonia, or a serum haemoglobin concentration of less than 10 g/dL; newly began treatments such as leukocytapheresis, granulocyte adsorptive apheresis, or immunosuppressant therapy with drugs such as 6‐mercaptopurine, azathioprine, and cyclosporine to improve symptoms, having milk allergy or a CAI of 6 or higher; pregnant women Age (mean ± SD): 43.9 ± 14.8 years* Sex (M/F): 28/18 Site of disease: 15 (left colon), 11 (proctosigmoiditis), 20 (total/subtotal) Use of medication: 24 (pentasa), 19 (salazopyrin), 1 (pentasa + salazopyrin), 2 (nothing) Length of time remission at study entry: unclear Number randomised (n = 60): 30 (probiotic)/30 (placebo) Number analysed: 23 (probiotic)/23 (probiotic) Postrandomisation exclusions: 14 (7 in each group) ‐ prohibited use of drug and lack of consent |
|
| Interventions |
All participants received 3 tablets 3 x daily for 12 months. As concomitant medication, the use of mesalazine and salazosulfapyridine was unrestricted, but steroids could not be used as remission maintenance therapy. The use of drugs with similar effects as the study drug, potentially affecting the evaluation of effectiveness (i.e. other active live microbial preparations, laxatives, etc.) was prohibited from 1 week before study entry to the completion of the study. In principle, the use of oral antibiotics was also prohibited, but the use of topical antibiotics other than oral preparations was not particularly restricted. If a participant received a new treatment in addition to their basic therapy with drugs such as mesalazine or salazosulfapyridine, relapse was diagnosed, and the study treatment and faecal sample collection were discontinued. |
|
| Outcomes |
Duration of follow‐up: 12 months
|
|
| Notes |
Funding source: This study was supported in part by a grant from the Japan Ministry of Health and Welfare. Declaration of interest: partially reported (YY ‐ none, other authors ‐ not reported) **Reported for the two intervention groups and pooled using an online calculator (www.statstodo.com/CombineMeansSDs_Pgm.php) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "At the start of the study, 30 outpatients were randomly assigned to the Bio‐Three group and 30 to the placebo group by means of a computer‐generated scheme." Comment: adequately described |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Placebo tablets were identical to Bio‐Three tablets and could not be distinguished from the active preparation on the basis of appearance. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Overall attrition rate was over 20%, but balanced between the two groups |
| Selective reporting (reporting bias) | Low risk | Trial registration not available, however, all expected outcomes appear to have been reported |
| Other bias | Low risk | Quote: "After randomization, the baseline characteristics of sex, age, age at disease onset, disease duration, disease extent, and concomitant treatment did not differ between the groups" Comment: no other apparent biases |
Zocco 2003.
| Study characteristics | ||
| Methods | RCT (abstract only) Setting: not stated Study period: not stated |
|
| Participants |
Inclusion: inactive UC and quiescent Crohn's disease* Exclusion: not stated Age (mean): 32 years Sex (M/F): 20/16 Site of disease: not stated Use of medication: not stated Length of time remission at study entry: not stated Number randomised (n = 36): 12 (probiotic)/10 (mesalazine)/14 (probiotic + mesalazine) Number assessed: 12 (probiotic)/10 (mesalazine)/14 (probiotic + mesalazine) Postrandomisation exclusion: none |
|
| Interventions |
|
|
| Outcomes |
Duration of follow‐up: 12 months
|
|
| Notes |
Funding source: not stated Declaration of interest: not reported Data from participants with CD were discarded due to the limited scope of the review. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were reportedly randomised, however, no further details were available |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not stated |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not stated |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants appear to have been accounted for |
| Selective reporting (reporting bias) | Unclear risk | The study was published as an abstract. Insufficient information to make a judgement |
| Other bias | Unclear risk | The study was published as an abstract. Insufficient information to make a judgement |
Zocco 2006.
| Study characteristics | ||
| Methods | Open‐label, single centre RCT Setting: Inflammatory Bowel Diseases Centre of the Catholic University, Rome, Italy Study period: June 2001 to December 2004 |
|
| Participants |
Inclusion: UC in clinical (CAI < 4), laboratory and endoscopic remission; time since last relapse: < 12 months Exclusion: patients with active disease or complications, severe accompanying illness or major colonic surgery, gastrointestinal infections, serious concomitant diseases (renal or hepatic failure, severe hypertension), diabetes mellitus, immunosuppressive treatment being administered currently or in the month before enrolment, mesalazine intolerance, and pregnant or lactating woman Age (mean ± SD): 33 ± 5.8 years* Sex (M/F): 104/83 Site of disease: 35 (proctosigmoiditis), 25 (left colon), 12 (total/subtotal) Use of medication: not stated Length of time remission at study entry: ≤ 4 weeks in 12% (probiotic)/11% (probiotic + mesalazine)/10% (mesalazine); ≤ 3 months in 26% (probiotic)/25% (probiotic +mesalazine)/26% (mesalazine) Number randomised (n = 187): 65 (probiotic)/62 (probiotic + mesalazine)/60 (mesalazine) Number analysed: 65 (probiotic)/62 (probiotic + mesalazine)/60 (mesalazine) Postrandomisation exclusion: none (premature discontinuation of the study for reasons other than relapse did not occur) |
|
| Interventions |
Participants were treated for 12 months. Treatment was interrupted in case of disease relapse, occurrence of side effects, poor compliance and inability to attend follow‐up visit. Oral or rectal treatment with antibiotic or steroid medications, apart from the study drugs, was not allowed during the trial. Full clinical evaluation with symptoms assessment and physical examination was performed at baseline and every 3 months for all the 12‐month study period. |
|
| Outcomes |
Duration of follow‐up: 12 months
|
|
| Notes |
Funding source: no external funding Declaration of interests: not reported *Reported for the three intervention groups and pooled using an online calculator (www.statstodo.com/CombineMeansSDs_Pgm.php) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Participants were reportedly randomised, however, no further details were provided |
| Allocation concealment (selection bias) | Unclear risk | Not stated |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | The study was an open‐label study |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The study was an open‐label study |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All participants were accounted for |
| Selective reporting (reporting bias) | Low risk | Trial registration not available, however, all participants were accounted for |
| Other bias | Low risk | Quote: "Demographic and prestudy clinical characteristics did not differ significantly among the three groups" Comment: no other apparent biases |
5‐ASA: 5‐aminosalicylic acid; CAI: colitis activity Index; CD: crohn's disease; CFU: colony forming units; CRP; C‐reactive protein; DAI: disease activity index; FCAL: fecal calprotectin; GI: gastrointestinal HCG: human chorionic gonadotropin; IBD: inflammatory bowel disease; IBD‐Q: inflammatory bowel disease questionnaire; ITT: intention to treat IV: intervention; NSAID: non steroidal ant‐inflammatory drugs; QoL; quality of life; RCT: randomised controlled trial; SCCAI: simple clinical colitis activity index; SD: standard deviation; UC: ulcerative colitis
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ahmed 2013 | Insufficient duration of follow‐up, i.e. less than 3 months; (quote): "if this could be altered with one months treatment with synbiotics" |
| Ballini 2019 | Wrong patient population and not maintenance study |
| Bamba 2002 | Wrong intervention, i.e. uses prebiotic; (quote): "A new prebiotic from germinated barley..." |
| Cui 2004 | Insufficient duration of follow‐up; (quote): "the patients were evaluated ....after 2 mo of treatment..." |
| Do 2010 | Wrong study design, i.e. review article |
| Faubion 2000 | Wrong study design, i.e. commentary piece |
| Folwaczny 2000 | Wrong study design, i.e. not randomised |
| Fujimori 2009 | Wrong patient population, i.e. patients were not in remission, so not maintenance trial |
| Henker 2008 | Wrong study design, i.e. not randomised |
| IRCT20120415009475N5 | Wrong study type |
| Ishikawa 2002 | Insufficient information: emailed author for clarification, no reply |
| Ishikawa 2011 | Wrong patient population: data from patients in remission presented together with those not in remission, unable to differentiate data |
| Li 2013 | Wrong patient population: patients not in remission, so not maintenance trial |
| Liu 2014 | Wrong patient population: translated from Chinese and confirmed not maintenance study |
| Miele 2009 | Wrong patient population: patients not in remission, so not maintenance study |
| NCT00268164 | Insufficinet information: university replied 26 February 2018 ‐ no access to full paper |
| NCT00374725 | Insufficient information: no reply from author ‐ emailed 15 January 2018 |
| NCT00803829 | Insufficient information: author passed away ‐ no access to full paper |
| NCT00951548 | Insufficient information: emailed author for classification on 15 January 2018, replied and confirmed not maintenance trial |
| NCT01772615 | Wrong patient population: author replied with full paper ‐ patients not in remission so not maintenance study |
| Palumbo 2016 | Wrong patient population: patients being induced, so not maintenance study |
| Pelech 1998 | Insufficient information: emailed author for classification, no reply |
| Rembacken 1999 | Includes both an induction and maintenance phase, however, participants were only randomised for induction. The maintenance phase was an observational study. |
| Rohatgi 2015 | Wrong patient population: patient cohort have microscopic colitis so not ulcerative colitis study |
| Sanchez‐Morales 2019 | Induction study |
| Shadnoush 2013 | Wrong patient population: study uses patients with inflammatory bowel disease ‐ does not differentiate between ulcerative colitis and Crohn's |
| Solovyeva 2014 | Wrong patient population: patients being induced, so not maintenance trial |
| Tursi 2010 | Wrong patient population: patients being induced, so not maintenance trial |
| Venturi 1999 | Wrong study design: this study was not a randomised controlled trial |
| Zhang 2018a | Induction study |
Characteristics of studies awaiting classification [ordered by study ID]
Fan 2019.
| Methods | RCT, single centre Setting: The First Affiliated Hospital of Fujian Medical University Study duration: January 2015 to June 2016 |
| Participants | 40 with IBD randomised (19 control group, 21 observation group) UC total: 31, CD total: 9; UC control 15, CD IV 4; CD control 4, CD IV 5 Inclusion: confirmed IBD diagnosis with mild to moderate symptoms as per the current standards in China; no previous probiotic treatment; no allergy to drugs used in the present study; cognisance of the purpose of the present study and willingness to sign an informed consent Exclusion: severe heart, liver, kidney and other systemic diseases; pregnancy or lactation; unresponsive to medical treatment and with complications; immune system disorders Sex (M/F): 10/9 control group; 10/11 observation group Age (mean +/‐ SD): 39.97 +/‐ 8.68 control group; 42.56 +/‐ 7.58 observation group Site of disease: not specified Use of medication: not specified Length of time remission at study entry: not specified Number randomised: 40 Number assessed: not specified Postrandomisation exclusion: not specified Follow‐up: 40 days |
| Interventions |
IV: pentasa (mesalazine extended action tablet) as in the control regimen + probiotics (2 tablets Bifico once and three times/day + "a largely liquid‐based high nutrition diet" Control: 1 to 2 pentasa tablets once and three times/day and a maintenance dose of 1 tablet once and three times/day |
| Outcomes |
|
| Notes | Mixed: contacted author for UC data This work was supported by the Fujian Province Natural Science Fund Project The authors declare that there are no conflicts of interest |
Fang 2018.
| Methods | RCT, multicentre Setting: Chunan County First People's Hospital and Taizhou Hospital Study duration: February 2016 to September 2017 |
| Participants | 84 patients with UC (42 control, 42 IV) Control: 18 mild, 24 moderate; IV: 19 mild, 23 moderate Inclusion: met the relevant diagnostic criteria for UC, confirmed by colonoscopy, barium enema, etc; course of disease ≥ 4 weeks; accompanied by persistent or recurrent diarrhoea, haemorrhagic stool with abdominal pain, acute aftermath etc; age ≥ 18 years; volunteer to participate in this study and sign informed consent Exclusion: those with allergies; combined with infectious colitis such as amoebiasis, bacterial disease, intestinal tuberculosis, chronic schistosomiasis; severe intestinal perforation, intestinal obstruction, toxic colonic dilatation etc; people with unconsciousness, serious insufficiency of important organs such as heart and kidney; people with radiation colitis, ischaemic colitis, Crohn's disease, mental illnesses, history of drug and alcohol abuse; pregnant, lactating women Sex (M/F): 26/16 control; 28/14 IV Age: 45.12 +/‐ 6.21 control; 45.13 +/‐ 6.2 IV Site of disease: control: whole colon 15, right half colon 19, left half colon 8; IV: whole colon 16, right half colon 17, left half colon 9 Use of medication: not specified Length of time remission at study entry: not specified Number randomised: 84 Number assessed: not specified Postrandomisation exclusion: not specified Follow‐up: 2 months |
| Interventions | IV: mesalazine + gold bifid Control: mesalazine only |
| Outcomes |
|
| Notes | Disease activity to be clarified. 95 versus 76% effective rate Main article in Chinese. Google translate was used for the translation. Funding and conflict of interest were not discussed in the article. |
Huang 2018.
| Methods | RCT, single centre Study duration: May 2014 to February 2018 Setting: Bai'an Affiliation Sanxia Central Hospital of Chongqing |
| Participants | Abstract: 120 UC patients (control 60, IV 60) Main text: 360 UC patients (control 180, IV 180) ??? Inclusion: not specified Exclusion: not specified Sex (M/F): 81/99 control; 90/90 IV Age (mean +/‐ SD): 41.5 +/‐ 8.3 control; 42.2 +/‐ 9.4 IV Site of disease: not specified Use of medication: not specified Length of time remission at study entry: not specified Number randomised: 120 or 360 Number assessed:not stated Postrandomisation exclusion: not stated Follow‐up: 8 weeks |
| Interventions | Control: mesalazine only IV: mesalazine + bifid triple viable capsules enteric‐coated tablet of mesalazine (Sunflower Group Jiamusi Luling Pharmaceutical Co, Ltd, 0.25 g/tablet, batch No.: 13001830), four tablets oral administration before meal, 3 times/day. Those in the research group would additionally take two bifid triple viable capsules (Jincheng Haisi Pharmaceutical Co, Ltd, 0.21 g/capsule, Batch No.: 13012365) prior to meal, 3 times/day |
| Outcomes |
|
| Notes | Unclear whether active or inactive UC ‐ emailed authors. Effectiveness rate = 90 versus 72% Funding and conflict of interest not discussed in the article. |
Shi 2018.
| Methods | RCT, single centre Setting: Department of Gastroenterology, Anji County People's Hospital of Huzhou City Study duration: August 2014 to November 2016 |
| Participants | 86 UC patients (43 control, 43 IV) Inclusion criteria: all who met the diagnosis of ulcerative colitis in the "Consensus Opinions on the Diagnosis and Treatment of Inflammatory Bowel Diseases in China" formulated by the Collaborative Group of Inflammatory Bowel Diseases of the Chinese Medical Association Gastroenterology Branch Criterion, with typical clinical manifestations (diarrhoea, mucus, pus, blood, stool, etc.) and colonoscopy (continuous, diffuse distribution of ulcer surface); Patients agreed to the study and signed informed consent Exclusion: those who used contraindications to the study; those who had poor compliance during treatment; other reasons were not suitable for inclusion in the study Sex (M/F): IV: 14/27; control: 17/24 Age (mean +/‐ SD): IV: 47.1 +/‐ 4.9; control: 47.3 +/‐ 6.2 Site of disease: not specified Use of medication: not specified Length of time remission at study entry: not specified Number randomised: 86 Number assessed: not specified Postrandomisation exclusion: not specified Follow‐up: treatment 2 months + 6 months |
| Interventions | IV: Bacillus subtilis and Enterococcus faecium + mesalazine Control: mesalazine only Mesalazine enteric‐coated tablets (Sunflower Pharmacy, Chinese Medicine Standard: H19980148, (specification: 0.25 g/tablet), oral, 1 g/time, 6 h/time; the observation group was combined with the Bacillus subtilis double live enteric‐coated capsules (trade name: Mei Changan, Beijing Hanmei Pharmaceutical Co, Ltd. based on the control group). Company, National Medicine Standard: S20030087, specification: 250 mg/capsule), 500 mg, orally, 3 times/day; two groups of patients were continuously taking medication for 2 months. |
| Outcomes |
|
| Notes | Disease activity to be clarified. 93% versus 76% effective rate Article in Chinese. Google Translate was used for the translation. Funding and conflict of interest were not discussed in the article. |
Yilmaz 2019.
| Methods | RCT, single centre, prospective, open‐label Study duration: May 2015 to December 2016 |
| Participants | 45 IBD patients (25 IV, 20 control) UC = 15, CD = 10 Inclusion/exclusion: "Patients with IBD participated in the study. In the trial, CD Activity Index for CD and Truelove‐Witts scoring systems for UC were used for disease assessment scores. If the score was <450, patients with CD were admitted to the study. If the score was higher, patients with UC were not admitted to the study. Volunteers also had to be >18 years old. Patients with alcohol consumption > 20 g/day, allergies or intolerance to milk, antibiotic treatment within the last 1 month, column or bowel operation history up to 3 months before the start of the study, and the presence of active infection within 1 month prior to the start of the study or during the study were excluded from the study. In addition, if a patient requested to leave on his/her own will, or if kefir was not consumed continuously for 2 weeks, the trial protocol was assessed and was not approved." Sex (M/F): IV: total 13/12, UC 9/6, CD: 4/6, control: total 10/10, UC: 4/6, CD: 6/4 Age (median): IV: 33, control: 43 Site of disease: IV: UC colon 15, CD colon 1, Ileum 6, colon + Ileum 3; control: UC colon 10, CD Ileum 10 Use of medication: not specified Length of time remission at study entry: not specified Number randomised: 45? Number assessed: 45 Postrandomisation exclusion: either 0 or 3. Authors mention 3 patients left the trial willingly, however participant and completers number are the same (n = 45) Follow‐up: 4 weeks |
| Interventions |
IV: 400 mL/day kefir x 2 day Control: ??? "The control group did not consume placebo because it was not possible to prepare a control product with a similar flavor, texture, and taste as those of kefir. Ayran and yogurt were similar to kefir, but they also have Lactobacillus and can affect the microbiota results." |
| Outcomes |
|
| Notes | Disease activity not clear. 96% versus 85% effective rate The authors declare no conflict of interest and that this study has received no financial support. |
Zhang 2018b.
| Methods | RCT, single centre Setting: Department of Gastroenterology, Longyou County People's Hospital, Luzhou, Zhejiang Province Study duration: October 2016 to November 2017 |
| Participants | 110 UC patients (55 control (38 UC, 17 CD); 55 observation (36 UC, 19 CD)) Inclusion: in accordance with the diagnostic criteria of the "Consensus on the diagnosis and treatment of inflammatory bowel disease in China" formulated by the Chinese Medical Association; no significant abnormalities in liver and kidney function; no other severe chronic diseases; informed consent Exclusion: severe liver and kidney diseases; intestinal diseases such as intestinal tuberculosis, Crohn's disease, intestinal tumours; hormones, 5‐aminosalicylic acid, and intestinal probiotics for nearly 4 weeks; patients taking other drugs; patients who are allergic to drugs such as mesalazine, Bifidobacterium quadruplex, etc.; pregnant and lactating women; patients with mental illness; patients who do not co‐operate with treatment; younger than 18 years old Sex (M/F): IV 29/26; control 32/23 Age (mean +/‐ SD): IV: 44.6 +/‐ 5.8; control 45.3 +/‐ 5.5 Site of disease: not specified Use of medication: not specified Length of time remission at study entry: not specified Number randomised: 110 Number assessed: not specified Postrandomisation exclusion: not specified Follow‐up: 2 months |
| Interventions |
IV: Bifidobacterium quadruplex bacteria tablets + mesalazine Control: mesalazine Both groups were given mesalazine enteric‐coated tablets (trade name: Huidi, Manufacturer: Sunflower Pharmaceutical Group Jiamusi Luling Pharmaceutical Co, Ltd, National Medicine Standard H19980148, 0.25 g/tablet), oral, 1 g/3 times/day. The observation group was given a Bifidobacterium quadruple live bacteria tablets (brand name: Siliankang, manufacturer: Hangzhou Longda Xinke Biopharmaceutical Co, Ltd, National Medicine Standard) S20060010, 0.5 g/tablet), oral, 1.5 g/3 times/day |
| Outcomes |
|
| Notes | Article in Chinese. Google Translate was used for the translation. Funding and conflict of interest were not discussed in the article. |
CD: crohn's disease; COX‐2: cyclooxygenase‐2; DAI: disease activity index; IBD: inflammatory bowel disease; IL: interleukin; IV: intervention; MDA: malondialdehyde; NF‐κβ: nuclear factor kappa beta; RCT; randomised controlled trial; sIL‐2R: soluble interleukin 2 receptor; SOD: superoxide dismutase; TNF‐ α: tumor necrosis factor alpha; UC: ulcerative colitis
Characteristics of ongoing studies [ordered by study ID]
NCT03415711.
| Study name | PRObiotic VSL#3® for maintenance of clinical and endoscopic REMission in Ulcerative Colitis (PROREM UC) |
| Methods | RCT, double‐blind, parallel assignment |
| Participants | 39 UC participants |
| Interventions |
|
| Outcomes |
|
| Starting date | April 2017 |
| Contact information | Antonino Amato clinicaltrialcentre@policlinicogemelli.it |
| Notes | Sponsors and collaborators: VSL pharmaceuticals, Actial Farmaceutica S.r.l. |
NCT03565939.
| Study name | Probiotic Treatment of Ulcerative Colitis with Trichuris Suis Ova (PROCTO) |
| Methods | RCT, parallel assignment, double‐blind, comparative, exploratory phase II proof of concept trial |
| Participants | 120 UC participants |
| Interventions |
IV: trichuris suis ova Control: placebo |
| Outcomes |
Primary outcome measures
Secondary outcome measures
|
| Starting date | May 2018 |
| Contact information | Contact: Michelle V Prosberg, MD, mailto:michelle.vernstroem.prosberg%40regionh.dk?subject=NCT03565939, PROCTO, Probiotic Treatment of Ulcerative Colitis With Trichuris Suis Ova (TSO) Contact: Andreas M Petersen, MD, Ph.D mailto:andreas.munk.petersen%40regionh.dk?subject=NCT03565939, PROCTO, Probiotic Treatment of Ulcerative Colitis With Trichuris Suis Ova (TSO) |
| Notes | Sponsors and collaborators: ParaTech A/S |
NCT03798210.
| Study name | Lactobacillus reuteri ATCC PTA 4659 in ulcerative colitis (COLUS) |
| Methods | RCT, triple‐blind, parallel assignment |
| Participants | 40 UC patients |
| Interventions | Lactobacillus reuteri versus placebo |
| Outcomes |
Primary outcome measures
Secondary outcome measures
Other outcome measures
|
| Starting date | January 2017 |
| Contact information | Contact: Per M Hellström, Prof +46 70 3727423 mailto:per.hellstrom%40medsci.uu.se?subject=NCT03798210, ATCC PTA 4659, Lactobacillus Reuteri ATCC PTA 4659 in Ulcerative Colitis; Peter Benno, MD, PhD +46 70 5795554 mailto:peter.benno%40endoskopienheten.se?subject=NCT03798210, ATCC PTA 4659, Lactobacillus Reuteri ATCC PTA 4659 in Ulcerative Colitis |
| Notes | Sponsors and collaborators: Uppsala University |
NCT04006977.
| Study name | Multistrain probiotics reduces UC depression and anxiety scores |
| Methods | RCT, double‐blind, parallel assignment |
| Participants | 60 UC patients |
| Interventions |
IV: multistrain probiotic product (DSF) Control: placebo |
| Outcomes |
Primary outcome measures
Secondary outcome measures
Adverse events (time frame: 4 weeks, 8 weeks, 12 weeks, 16 weeks). Adverse events were assessed at weeks 8 and 16 by participant survey. |
| Starting date | October 2019 |
| Contact information | Prof Jie Liang liangjie@fmmu.edu.cn |
| Notes | Sponsors and collaborators: Xijing Hospital of Digestive Diseases, MENDES SA |
5‐ASA: 5‐aminosalicylic acid; CRP; C‐reactive protein; DSF: Disulfiram HADS: hospital anxiety and depression scale; TSO: trichuris suis ova; UC: ulcerative colitis
Differences between protocol and review
We made a posthoc decision not to collect data on biochemical markers of inflammation as an outcome. Biochemical markers as surrogate endpoints are unlikely to provide results which are helpful to clinicians or patients.
Since the previous review, we have updated the search strategy, 'Risk of bias' reporting and use of GRADE to current Cochrane standards.
Contributions of authors
Zipporah Iheozor‐Ejiofor co‐ordinated the review; extracted data and contacted authors; checked the quality of data extraction; analysed and interpreted data; undertook and checked quality assessment; performed statistical analysis; checked the quality of the statistical analysis; produced the first draft of the review; contributed to writing and editing the review; made an intellectual contribution to the review; and approved the final review prior to submission.
Lakhbir Kaur performed screening of titles and abstracts and full‐text articles, extracted data and contacted authors; contributed to writing and editing the review; made an intellectual contribution to the review; and approved the final review prior to submission.
Morris Gordon performed screening of titles and abstracts and full‐text articles, extracted data and contacted authors, analysed and interpreted data; contributed to writing and editing the review; made an intellectual contribution to the review; contributed to previous versions of the review; made final changes to the review, including the update search prior to publication and peer review changes; and approved the final review prior to submission.
Patricia Baines contributed to writing and editing the review; made an intellectual contribution to the review; approved the final review prior to submission
Vasiliki Sinopoulou made update changes to all sections of the review following peer review and repeated searches; and approved the final review.
Anthony Akobeng initiated and conceptualised the review; contributed to previous versions of the review; and approved the final review prior to submission.
Sources of support
Internal sources
School of Medicine, University of Central Lancashire, UK
External sources
-
National Institute for Health Research, UK
This project was supported by the National institute for Health Research, via Cochrane Infrastructure and Cochrane Programme Grant funding (NIHR Cochrane Program Grant 16/114/13 ‐ A programme of Cochrane systematic reviews to investigate optimal treatment strategies using emerging pharmacological interventions, dietary therapies and interventions to manage pain in inflammatory bowel disease) to the University of Central Lancashire (UCLAN). The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, National Health Service (NHS) or the Department of Health.
Declarations of interest
Zipporah Iheozor‐Ejiofor: my employment at the University of Central Lancashire is funded by the National Institute for Health Research (NIHR) UK and focuses on high priority Cochrane Reviews in Inflammatory Bowel Disease.
Lakhbir Kaur: none known
Morris Gordon: received travel grants from various companies to attend scientific meetings in the last three years, including Biogaia, Synergy, Tillots, Ferring and Allergan. None of these companies have had any involvement in the planning, completion, analysis or write up of this or any other reviews. This review has been completed as part of a UK funded National Institute for Health Research (NIHR) Cochrane Programme grant, with some time funded.
Patricia Baines: none known
Vasiliki Sinopoulou: none known
Anthony Akobeng: none known
Edited (no change to conclusions)
References
References to studies included in this review
Bjarnason 2019 {published data only}
- Bjarnason I, Sission G, Hayee B. A randomised, double-blind, placebo controlled trial of a multi-strain probiotic in patients with asymptomatic ulcerative colitis and Crohn's disease. Inflammopharmacology 2019;27:465-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
Copaci 2014 {published data only}
- Copaci I, Chiriac G. Maintenance of remission of ulcerative colitis: prebiotics and dietary fiber. United European Gastroenterology Journal 2014;1:A375. [Google Scholar]
Kruis 1997 {published data only}
- Kruis W, Schutz E, Fric P, Fixa B, Judmaier G, Stolte M. Double-blind comparison of an oral Escherichia coli preparation and mesalazine in maintaining remission of ulcerative colitis. Alimentary Pharmacology and Therapeutics 1997;11(5):853-8. [DOI] [PubMed] [Google Scholar]
Kruis 2004 {published data only}
- Kruis W, Fric P, Pokrotnieks J, Lukas M, Fixa B, Kascak M, et al. Maintaining remission of ulcerative colitis with the probiotic Escherichia coli Nissle 1917 is as effective as with standard mesalazine. Gut 2004;53(11):1617-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
Matsuoka 2018 {published data only}
- Matsuoka K, Uemura Y, Kanai T. Efficacy of Bifidobacterium breve fermented milk in maintaining remission of ulcerative colitis. Digestive Diseases and Sciences 2018;ns:1-10. [org/10.1007/s10620-018-4946-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
NCT02361957 {unpublished data only}
- NCT02361957. The Effect of the Multispecies Probiotic Ecologic 825 Versus Placebo in Ulcerative Colitis Patients (CUPIDO). clinicaltrials.gov/ct2/show/NCT02361957 first posted 12 February 2015.
Shanahan 2006 {published data only}
- Shanahan F, Guarner F, Von Wright A, Vilpponen-Salmela T, O'Donoghue, D, Kiely B, et al. A one year, randomised, double-blind, placebo controlled trial of a Lactobacillus or a Bidifobacterium probiotic for maintenance of steroid-induced remission of ulcerative colitis. Gastroenterology 2006;130(4 Suppl 2):A44. [Google Scholar]
Vejdani 2017 {published data only}
- Vejdani R, Bahari A, Zadeh AM, Azmi M, Ebrahimi-Daryani N, Hashtroudi AA, et al. Effects of lactobacillus casei probiotic on mild to moderate ulcerative colitis: A placebo controlled study. Indian Journal of Medical Sciences January-March 2017;69(1):24-8. [Google Scholar]
Wildt 2011 {published data only}
- Wildt S, Nordgaard I, Hansen U, Brockmann E, Rumessen JJ. A randomised double-blind placebo-controlled trial with Lactobacillus acidophilus La-5 and Bifidobacterium animalis subsp. lactis BB-12 for maintenance of remission in ulcerative colitis. Journal of Crohn's and Colitis 2011;5(2):115-21. [DOI] [PubMed] [Google Scholar]
Yasushi 2015 {published data only}
- Yasushi Y, Akihiro Y, Ryuichi F, Koji S, Aisaku O, Kentaro N, et al. Effectiveness of probiotic therapy for the prevention of relapse in patients with inactive ulcerative colitis. World Journal of Gastroenterology 2015;21(19):5985-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zocco 2003 {published data only}
- Zocco MA, dal Verme LZ, Armuzzi A, Nista EC, Papa A, Candelli M. Comparison of Lactobacillus GG and mesalazine in maintaining remission of ulcerative colitis and Crohn's disease. Gastroenterology 2003;124(4):A201. [Google Scholar]
Zocco 2006 {published data only}
- Zocco MA, dal Verme LZ, Cremonini F, Piscaglia AC, Nista EC, Candelli M, et al. Efficacy of Lactobacillus GG in maintaining remission of ulcerative colitis. Alimentary Pharmacology and Therapeutics 2006;23(11):1567-74. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ahmed 2013 {published data only}
- Ahmed J, Reddy BS, Molbak L, Leser TD, Macfie J. Impact of probiotic on colonic microflora in patients with colitis: A prospective double blind randomised crossover study. International Journal of Surgery 2013;11(10):1131-6. [DOI] [PubMed] [Google Scholar]
Ballini 2019 {published data only}
- Ballini A, Santacroce L, Cantore S, Bottalico L, Dipalma G, Tope S, et al. Probiotics efficacy on oxidative stress values in inflammatory bowel disease: a randomized double-blinded placebo-controlled pilot study. Endocrine, Metabolic & Immune Disorders - Drug Targets 2019;19(3):1-8. [DOI] [PubMed] [Google Scholar]
Bamba 2002 {published data only}
- Bamba T, Kanauchi O, Andoh A, Fujiyama Y. A new prebiotic from germinated barley for nutraceutical treatment of ulcerative colitis. Journal of Gastroenterology and Hepatology 2002;17(8):818-24. [DOI] [PubMed] [Google Scholar]
Cui 2004 {published data only}
- Cui HH, Chen CL, Wang JD, Yang YJ, Cun Y, Wu JB, et al. Effects of probiotics on intestinal mucosa of patients with ulcerative colitis. World Journal of Gastroenterology 2004;10(10):1521-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Do 2010 {published data only}
- Do VT, Baird BG, Kockler DR. Probiotics for maintaining remission of ulcerative colitis in adults. Annals of Pharmacotherapy 2010;44(3):565-71. [DOI] [PubMed] [Google Scholar]
Faubion 2000 {published data only}
- Faubion WA, Sandborn WJ. Probiotic therapy with E. Coli for ulcerative colitis: take the good with the bad. Gastroenterology 2000;118(3):630-1. [DOI] [PubMed] [Google Scholar]
Folwaczny 2000 {published data only}
- Folwaczny C. Probiotics for prevention of ulcerative colitis recurrence: alternative medicine added to standard treatment. Zeitschfrift de Gastroenterologie 2000;38(6):547-50. [PubMed] [Google Scholar]
Fujimori 2009 {published data only}
- Fujimori S, Gudis K, Mitsui K, Seo T, Yonezawa M, Tanaka S, et al. Randomized controlled trial on the efficacy of synbiotic versus probiotic or prebiotic treatment to improve the quality of life in patients with ulcerative colitis. Nutrition 2009;25(5):520-5. [DOI] [PubMed] [Google Scholar]
Henker 2008 {published data only}
- Henker J, Müller S, Laass MW, Schreiner A, Schulze J. Probiotic Escherichia coli Nissle 1917 (EcN) for successful remission maintenance of ulcerative colitis in children and adolescents: an open-label pilot study. Zeitschrift fur Gastroenterologie 2008;46(9):874-5. [DOI] [PubMed] [Google Scholar]
IRCT20120415009475N5 {published data only}
- IRCT20120415009475N5. Evaluation of the effects of Saccharomyces Boulardii on pain and quality of life in children with Inflammatory Bowel Disease (IBD) [Evaluation of the effects of lyophilized Saccharomyces Boulardii capsules on quality of life and clinical outcomes in children with inflammatory bowel disease (IBD)]. www.irct.ir/trial/32179 (registration date 10 October 2018). [IRCT: https://www.irct.ir/trial/32179]
Ishikawa 2002 {published data only}
- Ishikawa H, Akedo I, Umesaki Y, Tanaka R, Imaoka A, Otani T. Randomized controlled trial of the effect of bifidobacteria-fermented milk on ulcerative colitis. Journal of the American College of Nutrition 2002;22(1):56-63. [DOI] [PubMed] [Google Scholar]
Ishikawa 2011 {published data only}
- Ishikawa H, Matsumoto S, Ohashi Y, Imoaka A, Setoyama H, Umesaki Y, et al. Beneficial effects of probiotic bifidobacterium and galacto-oligosaccharide in patients with ulcerative colitis: A randomized controlled study. Digestion 2011;84(2):128-33. [DOI] [PubMed] [Google Scholar]
Li 2013 {published data only}
- Li K, Zhang CF, Xia YH, Li Z J, Han Y. Efficacy of probiotics on ulcerative colitis and its mechanism. Zhonghua Weichang Waike Zazhi 2013;16(4):336-9. [PubMed] [Google Scholar]
Liu 2014 {published data only}
- Liu P, Sun L, Zhang ZH, Zhang P, Zhang J. Clinical efficacy of Salofalk combined with beneficial bacteria in patients with ulcerative colitis. World Chinese Journal of Digestology 2014;22(22):3344-8. [Google Scholar]
Miele 2009 {published data only}
- Miele E, Pascarella F, Giannetti E, Quaglietta L, Baldassano RN, Staiano A. Effect of a probiotic preparation (VSL#3) on induction and maintenance of remission in children with ulcerative colitis. American Journal of Gastroenterology 2009;104(2):437-43. [DOI] [PubMed] [Google Scholar]
NCT00268164 {published data only}
- NCT00268164. Lactobacilus acidophilus and Bifidobaceterium animalis subsp. Lactis maintenance treatment in ulcerative colitis. clinicaltrials.gov/show/NCT00268164 First received 22 December 2005.
NCT00374725 {published data only}
- NCT00374725. Treatment of Ulcerative Colitis With a Combination of Lactobacillus Rhamnosus and Lactobacillus Acidophilus. clinicaltrials.gov/show/NCT00374725 First posted 11 September 2006.
NCT00803829 {published data only}
- NCT00803829. Sunbiotic treatment of ulcerative colitis patients. clinialtrials.gov/show/NCT00803829 First posted 8 December 2008.
NCT00951548 {published data only}
- NCT00951548. Food Supplementation With VSL#3 as a Support to Standard Pharmaceutical Therapy in Ulcerative Colitis. clinicaltrials.gov/show/NCT00951548 First posted 4 August 2009.
NCT01772615 {published data only}
- NCT01772615. Treatment of ulcerative colitis with ciprofloxacin and E. Coli Nissle. clinicaltrials/gov/show/NCT01772615 First posted 21 january 2013.
Palumbo 2016 {published data only}
- Palumbo VD, Romeo M, Marino Gammazza A, Carini F, Damiani P, Damiano G et al. The long-term effects of probiotics in the therapy of ulcerative colitis: A clinical study. Biomedical Papers of the Medical Faculty of the University Palacky, Olomouc, Czechoslovakia 2016;160(3):372-7. [DOI] [PubMed] [Google Scholar]
Pelech 1998 {published data only}
- Pelech T, Fric P, Fixa B, Komarkova O. Comparison of mutaflor and mesalazine in the maintenance treatment of inactive ulcerative colitis. Prakticky Lekar 1998;78(10):556-8. [Google Scholar]
Rembacken 1999 {published data only}
- Rembacken BJ, Snelling AM, Hawkey PM, Chalmers DM, Axon AT. Non-pathogenic Escherichia coli versus mesalazine for the treatment of ulcerative colitis: a randomised trial. Lancet 1999;354(9179):635-9. [DOI] [PubMed] [Google Scholar]
Rohatgi 2015 {published data only}
- Rohatgi S, Ahuja V, Makharia GK, Rai T, Das P, Dattagupta S, et al. VSL#3 induces and maintains short-term clinical response in patients with active microscopic colitis: a two-phase randomised clinical trial. BMJ Open Gastroenteroilogy 2015;2(1):e000018. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sanchez‐Morales 2019 {published data only}
- Sanchez-Morales A, Perez-Ayala MF, Cruz-Martinez M, Arenas-Osuna J, Ramirez-Mendoza P, Ceniceros RA, et al. Efectividad de probioticos sobre sintomas, histologia, y tolerancia alimentaria en colitis ulcerativa. Revista Medica del Instituto Mexicano del Seguro Social 2019;57(1):9-14. [PubMed] [Google Scholar]
Shadnoush 2013 {published data only}
- Shadnoush M, Hosseini RS, Mehrabi Y, Delpisheh A, Alipoor E, Faghfoori Z, et al. Probiotic yogurt affects pro- and anti-inflammatory factors in patients with inflammatory bowel disease. Iranian Journal of Pharamceutical Research 2013;12(4):929-36. [PMC free article] [PubMed] [Google Scholar]
Solovyeva 2014 {published data only}
- Solovyeva O. Probiotics can extend remission of ulcerative colitis. Journal of Crohn's and Colitis 2014;8:221. [Google Scholar]
Tursi 2010 {published data only}
- Tursi A, Brandimarte G, Papa A, Giglio A, Elisei W, Giorgetti GM, et al. Treatment of relapsing mild-to-moderate ulcerative colitis with the probiotic VSL3 as adjunctive to a standard pharmaceutical treatment: A double-blind, randomized, placebo-controlled study. American Journal of Gastroenterology 2010;105(10):2218-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
Venturi 1999 {published data only}
- Venturi A, Gionchetti P, Rizzello F, Johansson R, Zucconi E, Brigidi P, et al. Impact on the composition of the faecal flora by a new probiotic preparation: preliminary data on maintenance treatment of patients with ulcerative colitis. Alimentary Pharmacology and Therapeutics 1999;13(8):1103-8. [DOI] [PubMed] [Google Scholar]
Zhang 2018a {published data only}
- Zhang J. Effects of Bifidobacterium quadruplex live bacteria tablets on Mayo score and hs-CRP, IL-4, IL-8 in patients with mild to moderate ulcerative colitis. World Chinese Journal of Digestology 2018;26(6):373-7. [Google Scholar]
References to studies awaiting assessment
Fan 2019 {published data only}
- Fan H, Du J, Liu X, Zheng WW, Zhuang ZH, Wang CD, et al. Effects of pentasa-combined probiotics on the microflora structure and prognosis of patients with inflammatory bowel disease. Turkish Journal of Gastroenterology 2019;30(8):680-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fang 2018 {published data only}
- Fang W, Cai Q. Effect of mesalazine combined with bifid on inflammatory response and rectal-anal dynamics in patients with ulcerative colitis. World Chinese Journal of Digestology 2018;26(10):594-600. [Google Scholar]
Huang 2018 {published data only}
- Huang M, Chen Z, Lang C, Chen J, Yang B, Xue L, et al. Efficacy of mesalazine in combination with bifid triple viable capsules on ulcerative colitis and the resultant effect on the inflammatory factors. Pakistan Journal of Pharmaceutical Sciences 2018;31(6):2891-5. [PubMed] [Google Scholar]
Shi 2018 {published data only}
- Shi XH, Tan FP, Jiang WH. Bacillus subtilis and Enterococcus faecium enteric-coated capsules combined with mesalazine for treatment of patients with ulcerative colitis: Efficacy and impact on serum levels of SOD, MDA, interleukins, and TNF-α. World Chinese Journal of Digestology 2018;26(12):748-54. [Google Scholar]
Yilmaz 2019 {published data only}
- Yilmaz I, Dolar ME, Özpinar H. Effect of administering kefir on the changes in fecal microbiota and symptoms of inflammatory bowel disease: a randomized controlled trial. Turkish Journal of Gastroenterology 2019;30(3):242-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2018b {published data only}
- Zhang Y, Wu M, Chen Y. Effects of adjuvant therapy with bifidobacterium quadruplex on lipid peroxidation injury indices, inflammatory factors and immune function in patients with ulcerative colitis. World Chinese Journal of Digestology 2018;26(22):1348-54. [Google Scholar]
References to ongoing studies
NCT03415711 {published data only}
- NCT03415711. PRObiotic VSL#3® for Maintenance of Clinical and Endoscopic REMission in Ulcerative Colitis (PROREM UC). clinicaltrials.gov/ct2/show/NCT03415711 First posted 30 January 2018.
NCT03565939 {published data only}
- NCT03565939. Probiotic Treatment of Ulcerative Colitis With Trichuris Suis Ova (TSO) (PROCTO). clinicaltrials.gov/ct2/show/NCT03565939 First posted 21 June 2018.
NCT03798210 {published data only}
- NCT03798210. Lactobacillus Reuteri ATCC PTA 4659 in Ulcerative Colitis (COLUS). clinicaltrials.gov/ct2/show/NCT03798210 First posted 9 January 2019.
NCT04006977 {published data only}
- Liang J. Multistrain Probiotics Reduces UC Depression and Anxiety Scores. clinicaltrials.gov/ct2/show/NCT04006977 First posted 5 July 2019.
Additional references
Baron 1964
- Baron JH, Connell AM, Lenard-Jones JE. Variation between observers in describing mucosal appearances in proctocolitis. British medical journal 1964;1:89-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cleynen 2016
- Cleynen I. Inherited determinants of Crohn's disease and ulcerative colitis phenotypes: a genetic association study. Lancet 2016;387(10014):156-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 2010
- Cohen RD. Systematic review: the costs of ulcerative colitis in Western countries. Alimentary Pharmaology and Therapeutics 2010;31(7):693-707. [DOI] [PubMed] [Google Scholar]
Dieleman 2003
- Dieleman LA, Goerres MS, Arends A, Sprengers D, Torrice C, Hoentjen F, et al. Lactobacillus GG prevents recurrence of colitis in HLA-B27 transgenic rats after antibiotic treatment. Gut 2003;52(3):370-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Fabia 1993
- Fabia R, Ar'Rajab A, Johansson ML, Willen R, Andersson R, Molin G, et al. The effect of exogenous administration of Lactobacillus reuteri R2LC and oat fiber on acetic-induced colitis in the rat. Scandinavian Journal of Gastroenterology 1993;28(2):155-62. [DOI] [PubMed] [Google Scholar]
Fiorino 2016
- Fiorino G. The clinical potential of etrolizumab in ulcerative colitis: hypes and hopes. Therapeutic Advances in Gastroenerology 2016;9(4):503-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT 2015 [Computer program]
- McMaster University GRADEpro GDT: GRADEpro Guideline Development Tool. McMaster University, 2015 (developed by Evidence Prime, Inc.).Available from gradepro.org.
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JP, Altman DG, Sterne JA, editor(s). Chapter 8: Assessing risk of bias in included studies. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Jairath 2017
- Jairath V, Zou GY, Parker CP, MacDonald JK, AlAmeel T, Al Beshir M et al. Placebo response and remission rates in randomised trials of induction and maintenance therapy for ulcerative colitis. Cochrane Database of Systematic Reviews 2017, Issue 9. [DOI: 10.1002/14651858.CD011572.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kennedy 2000
- Kennedy RJ, Hoper M, Deodhar K, Kirk SJ, Gardiner KR. Probiotic therapy fails to improve gut permeability in a hapten model of colitis. Scandinavian Journal of Gastroenterology 2000;35(12):1266-71. [DOI] [PubMed] [Google Scholar]
Loftus 2004
- Loftus EV. Clinical epidemiology of inflammatory bowel disease: Incidence, prevalence, and environmental influences. Gastroenterology 2004;126(6):1504-17. [DOI] [PubMed] [Google Scholar]
Madsen 1999
- Madsen KL, Doyle JS, Jewell LD, Tavernini MM, Fedorak RN. Lactobacillus species prevents colitis in interleukin 10 gene-deficient mice. Gastroenterology 1999;116(5):1107-14. [DOI] [PubMed] [Google Scholar]
Madsen 2001
- Madsen K, Cornish A, Soper P, McKaigney C, Jijon H, Yachimec C, et al. Probiotic bacteria enhance murine and human intestinal epithelial barrier function. Gastroenterology 2001;121(3):580-91. [DOI] [PubMed] [Google Scholar]
Mallon 2007
- Mallon P, McKay D, Kirk S, Gardiner K. Probiotics for induction of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2007, Issue 10. [DOI: 10.1002/14651858.CD005573.pub2] [DOI] [PubMed] [Google Scholar]
NICE 2019
- National Institute for Health and Care Excellence. Ulcerative Colitis Mangagement NG130. https://www.nice.org.uk/guidance/ng130 2019. [PubMed]
Ong 2019
- Ong TG, Gordon M, Banks SS, Thomas MR, Akobeng AK. Probiotics to prevent infantile colic. Cochrane Database of Systematic Reviews 2019, Issue 3. [DOI: 10.1002/14651858.CD012473.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Panigrahi 2014
- Panigrahi P. Probiotics and prebiotics in neonatal necrotizing enterocolitis: new opportunities for translational research. Pathophysiology 2014;21(1):35-46. [DOI] [PubMed] [Google Scholar]
Pitkin 1999
- Pitkin RM, Branagan MA, Burmeister LF. Accuracy of data in abstracts of published research articles. JAMA 1999;281:1110-1. [DOI] [PubMed] [Google Scholar]
Review Manager 2014 [Computer program]
- The Cochrane Collaboration The Nordic Centre. Copenhagen: The Cochrane Collaboration, 13th June 2014.Available at https://community.cochrane.org/help/tools-and-software/revman-5.
Schultz 2002
- Schultz M, Veltkamp C, Dieleman LA, Grenther WB, Wyrick PB, Tonkonogy SL, et al. Lactobacillus plantarum 299V in the treatment and prevention of spontaneous colitis in interleukin-10-deficient mice. Inflammatory Bowel Diseases 2002;8(2):71-80. [DOI] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann HJ, Oxman AD, Higgins JP, Vist GE, Glasziou P, Guyatt GH. Chapter 11: Presenting results and 'Summary of findings' tables. In: Higgins JP, Green S, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from handbook.cochrane.org.
Shibolet 2002
- Shibolet O, Karmeli F, Eliakim R, Swennen E, Brigidi P, Gionchetti P, et al. Variable response to probiotics in two models of experimental colitis in rats. Inflammatory Bowel Diseases 2002;8(6):399-406. [DOI] [PubMed] [Google Scholar]
Truelove 1956
- Truelove SC, Richards WC. Biopsy studies in ulcerative colitis. British medical journal 1956;1:1315-1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
Turner 2018
- Turner D, Ruemmele FM, Orlanski-Meyer E, Griffiths AM, Carpi JM, Bronsky J, et al. Management of paediatric ulcerative colitis, Part 1: ambulatory care—an evidence-based guideline From European Crohn's and Colitis Organization and European Society of Paediatric Gastroenterology, Hepatology and Nutrition. Journal of Pediatric Gastroenterology and Nutrition 2018;67(2):257-91. [DOI: 10.1097/mpg.0000000000002035] [DOI] [PubMed] [Google Scholar]
Ungaro 2016
- Ungaro R, Mehandru S, Allen PB, Peyrin-Biroulet L, Colombel JF. Ulcerative colitis. Lancet 2016;389(10080):1756-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2016
- Wang Y, Parker CE, Feagan BG, MacDonald JK. Oral 5-aminosalicylic acid for maintenance of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2016, Issue 5. [DOI: 10.1002/14651858.CD000544.pub4] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Fagbemi 2008
- Fagbemi AO, Thomas AG, Akobeng AK. Probiotics for maintenance of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2008, Issue 4. [DOI: 10.1002/14651858.CD007443] [DOI] [PubMed] [Google Scholar]
Naidoo 2011
- Naidoo K, Gordon M, Fagbemi AO, Thomas AG, Akobeng AK. Probiotics for maintenance of remission in ulcerative colitis. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD007443.pub2] [DOI] [PubMed] [Google Scholar]


