Abstract
Muscle hernias of the extremities most commonly occur in the leg, between the knee and ankle. Symptomatic muscle hernias in the leg are rare cause of chronic leg pain and neuropathy, and not routinely encountered in surgical practice. Although this condition is especially an esthetic problem, with palpable subcutaneous soft tissue mass, it can lead to spontaneous pain, cramp, local tenderness or potentially neuropathic symptoms. Moreover, among leg muscles involved in this process, peroneus brevis is less frequent than tibialis anterior. Magnetic Resonance Imaging is the method of choice in establishing the diagnosis. Symptomatic cases can be treated surgically in different ways, the preferred one is nerve releasing with fasciotomy. The purpose of this case report is to present the Magnetic Resonance findings of a superficial nerve compression due to a peroneus brevis muscle herniation.
Keywords: Peripheral Neuropathy, Muscle Hernia, Magnetic Resonance Imaging, Fasciotomy, Nerve Releasing
CASE REPORT
A 58 year old woman with a tender, slowly enlarging subcutaneous mass on her lower left lateral leg developed over last 6 months, was admitted to our institute in order to perform a MRI exam.
Her primary complaint was numbness in the lower lateral leg and foot associated to mild degree of hyperalgesia that increased with standing, walking, activity and leg dorsiflexion. No associated recent history of trauma, infection or overly exertional activities were reported; the patient reported only that she started taking long walks in the hills the months preceding the development of this finding, without however reporting significant physical efforts.
Physical examination revealed a soft, mildly tender, non-reducible fusiform subcutaneous thickening (longitudinal extension 45mm) on the lateral left lower extremity with occasional paresthesia irradiated to the dorsum of the foot; Tinel’s test was positive.
An ultrasound exam was not carried out and a direct MRI request was done by the family doctor in order to rule out a small parts tumor. MRI (Siemens Magnetom Avanto 1,5T Erlangen, Germany) was performed with a dedicate knee coil with the leg in a mild forced dorsiflexion; a dynamic MRI exam was not performed. Basal sequences were obtained in three standard planes T1w-T2w-PDw fat saturation and an axial T1w fat saturation sequence completed the exam after contrast administration. MRI demonstrated a focal 5mm contour bulging of the peroneus brevis muscle with the same MRI features of the muscle itself, and was interpreted to most likely represent a fascial defect with muscle herniation associated to a little adipose lobulation. This complex measured on the whole 19mm × 9mm × 18mm and determined mild compression and displacement of the superficial peroneal nerve (SPN) just caudally the site where the nerve perforates the deep fascial layer and becomes subcutaneous (Fig 1–2–3). PD fat sat and T1 fat sat enhanced sequences, showed a faint hyperintensity and enhancement of the nerve just close to the adipose-muscular hernia, representing nerve edema and hyperemia consistent with the clinical superficial peripheral neuropathy (Fig 4–5).
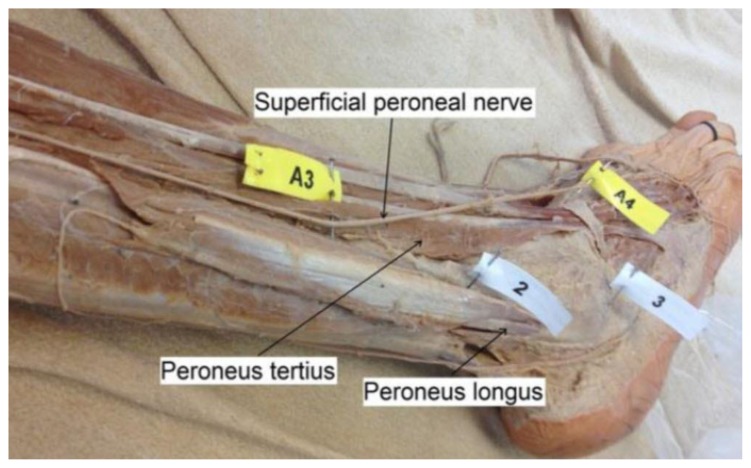
Figure 1.
The superficial peroneal nerve runs between the lateral (flag 2) and anterior muscle compartments, crossing the ankle anterolaterally over peroneus tertius (flag A3) to innervate the dorsum of the foot (flag A4). Flag 3 marks the lateral malleolus. With permission to use by “Asp AR, Marsland D, Elliot RR. The superficial peroneal nerve: A review of its anatomy and surgical relevance. OA Anatomy 2014 Mar 15;2(1):6. [15].
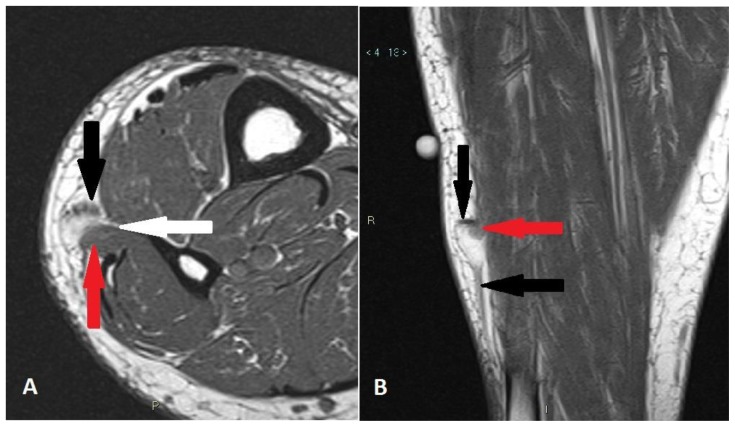
Figure 2.
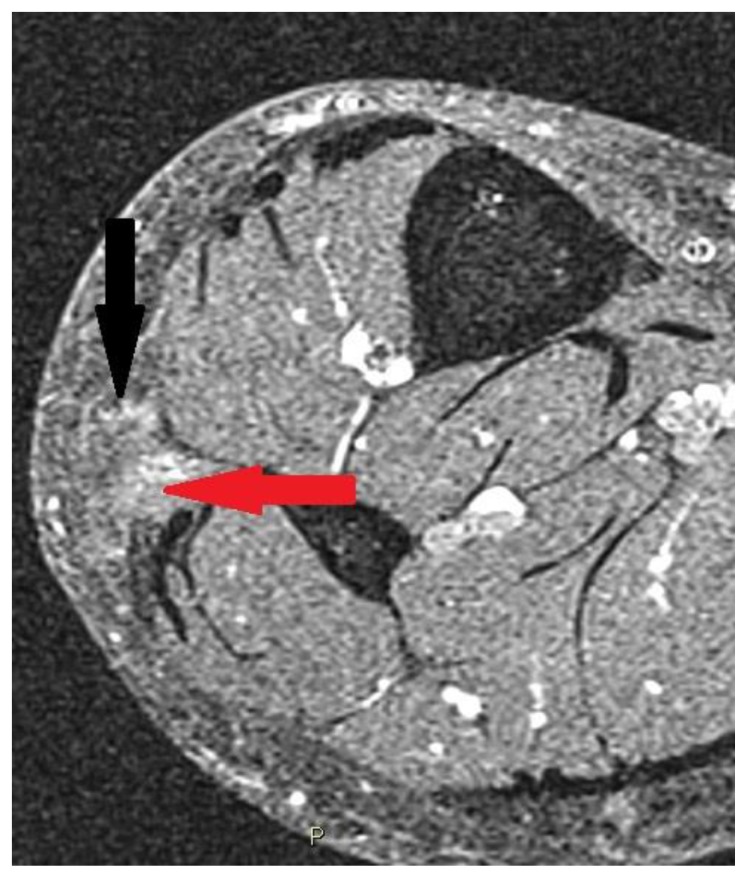
58 year old woman with a superficial peroneal nerve compression due to peroneus brevis muscle herniation.
Findings: axial (A) and coronal (B) T1-weighted sequences show a focal peroneus brevis muscle herniation (red arrows) through a fascial layer defect (white arrow) associated to a little adipose lobule determining compression and neuropathy of the superficial peroneal nerve (black arrows). In B cutaneous marker localized cranially to palpable mass.
Technique: Siemens 1.5T Magnetic Resonance System. Turbo Spin Echo axial T1-weighted sequence A (slice thickness 3mm - TR: 500 - TE: 20) and coronal T1-weighted sequence B (slice thickness 3mm - TR: 500 - TE: 18).
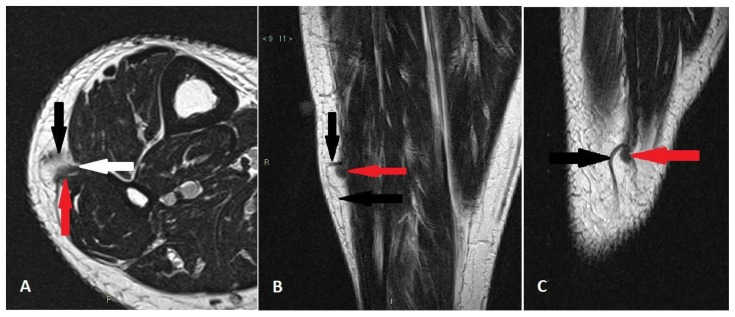
Figure 3.
58 year old woman with a superficial peroneal nerve compression due to peroneus brevis muscle herniation.
Findings: axial (A), coronal (B) and sagittal (C)T2-weighted sequences show a focal peroneus brevis muscle herniation (red arrows) through a fascial layer defect (white arrow) associated to a little adipose lobule determining compression and neuropathy of the superficial peroneal nerve (black arrows). In B cutaneous marker localized cranially to palpable mass.
Technique: Siemens 1.5T Magnetic Resonance System. Turbo Spin Echo axial T2-weighted sequence A (slice thickness 3mm - TR: 4600 - TE: 96), coronal T2-weighted sequence B (slice thickness 3mm - TR: 4600 - TE: 98) and sagittal T2-weighted sequence C (slice thickness 3mm - TR: 4190 - TE: 102).
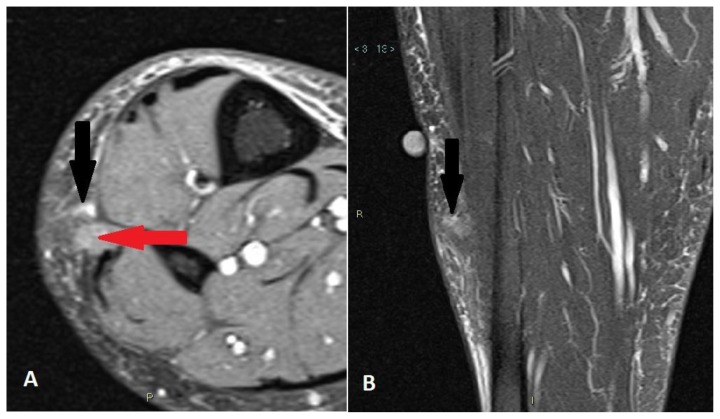
Figure 4.
58 year old woman with a superficial peroneal nerve compression due to peroneus brevis muscle herniation.
Findings: axial (A) and coronal (B) PD-weighted sequences with fat saturation show a focal peroneus brevis muscle herniation (red arrow) through a fascial layer defect associated to a little adipose lobule determining compression and neuropathy of the superficial peroneal nerve. Neuropathy is shown by mild hyperintensity of the nerve near herniation (black arrows). In B cutaneous marker localized cranially to palpable mass.
Technique: Siemens 1.5T Magnetic Resonance System. Turbo Spin Echo axial PD-weighted sequence with fat saturation A (slice thickness 3mm - TR: 3540 - TE: 10) and coronal PD-weighted sequence with fat saturation B (slice thickness 3mm - TR: 3130 - TE: 51).
Figure 5.
58 year old woman with a superficial peroneal nerve compression due to peroneus brevis muscle herniation.
Findings: axial T1-weighted sequence with fat saturation after contrast administration shows a focal peroneus brevis muscle herniation (red arrow) through a fascial layer defect associated to a little adipose lobule determining compression and mild neuropathic hyperemia of the superficial peroneal nerve (black arrow).
Technique: Siemens 1.5T Magnetic Resonance System. Turbo Spin Echo T1-weighted sequence with fat saturation (slice thickness 3mm - TR: 606 - TE: 21). Gadolinium 12 ml iv bolus.
The patient was treated conservatively by resting, avoiding excessive strain on the leg and compression stockings. After about 2 months from the interruption of the walks the symptomatology has regressed, although the small swelling was still moderately appreciable. Therefore, in agreement with the patient and in consideration of the regression of symptoms, further surgical approaches were avoided.
DISCUSSION
Etiology & Demographics
Muscle herniation is defined as a portion of muscle through acquired or congenital fascial layer defects. Tibialis anterior muscle herniation is the most common, because its fascia is the most vulnerable to trauma. Herniations of peroneus longus, brevis, extensor and flexor digitorum longus and gastrocnemius muscles have also been described. Even upper limbs can be involved, but less frequently. Patients are usually adolescents or young adults [1].
Muscle herniation of the extremities is a rare clinical entity, frequently misdiagnosed as a soft tissue tumor and commonly occurs as acquired (post-traumatic or post-surgical) or congenital fascial defects. Congenital causes may be an overall general weakness in the muscular fascia (mesodermal insufficiency), or may occur at sites of perforating nerves and vessels. Acquired causes are usually secondary to trauma. Traumatic examples include penetrating trauma, closed fractures causing a fascial tear (direct trauma), or force applied to contracted muscle causing acute fascial rupture (indirect trauma). Herniation is potentiated by increases in intracompartmental pressures such as muscle hypertrophy or chronic exertional compartment syndrome (CECS). For perspective, regular cardiovascular exercise and physical activity can lead to muscle hypertrophy with a 20% increase in muscle volume. CECS is defined as a reversible form of abnormally increased intramuscular pressure during exercise or physical exertion secondary to noncompliance of osteofascial tissues to exercise-induced increases in muscle volume. Athletic men, such as military soldiers, athletes, mountain climbers, skiers, and those partaking in similar occupational and sporting activities, are the demographic population believed to be at the highest risk [2].
Clinical & Imaging findings
Patients usually present with a palpable soft-tissue mass that becomes more firm and prominent after the contraction of the affected limb. Most of the masses are painless and asymptomatic; however, in some cases, they may become painful after prolonged exercises due to focal muscle entrapment and resultant ischemia. Although this condition is especially an esthetic problem, it can lead to spontaneous pain, cramp, local tenderness or potentially neuropathic symptoms. The presence of pain is an important indicator for treatment of symptomatic muscle herniation [3]. A physical examination can also reveal if there is a positive Tinel’s sign present at the region of the palpable lump and muscle hernia.
Ultrasound and MRI are considered the methods of choice for detecting fascial defects and muscle hernias. The sonographer, with light probe pressure, can scan dynamically to determine the presence of a fascial defect during muscle contraction and positional manipulation. The appearance of a muscle hernia can be extremely subtle and easily missed even with the slightest probe pressure which may reduce the hernia. Without dynamic assessment or heavy transducer pressure, a muscle hernia could be missed particularly if the muscle is at rest and the hernia is spontaneously reducible. Sonographically normal appearing muscle fibres protrude through the weakened fascia with elevated muscle contraction and pressure from straining. These muscle fibres have the same echogenicity and fibrillar pattern as the normal muscle tissue. Ultrasound is considered fundamental in imaging the nerves and any possible nerve compression associated with a muscle hernia [4].
Sonography is advantageous as it is real time, muscle herniation is detected during dynamic examination, and nature of the lesion can be shown to the patient which helps in reassurance [5,6].
Though expensive, MRI can confirm muscle herniation in equivocal US findings. It better visualizes musculofascial demarcation and allows quantification of fascial splitting and muscle herniation. Dynamic ultrasonography and MRI incorporate fast imaging with forced muscular movements (dorsiflexion and plantar flexion at the ankle) and enable better visualization and pinpointing of the hernia and fascial defect. The defect is in the deep layer of the deep fascia. It may thin or elevate the superficial layer of deep fascia which is overlying the muscle [7,8].
Treatment & Prognosis
Most symptomatic muscle hernias are successfully treated with conservative therapy, including rest, activity restrictions and compression stockings. Because asymptomatic hernias do not necessitate treatment, a general guideline may suggest conservative therapy only for mildly symptomatic muscle hernias. Surgical referral is warranted for patients with moderate to severe symptoms that are not amenable to a conservative therapy. Optimal surgical treatment is controversial. A variety of surgical techniques have been described, ranging from fasciotomy to anatomical repair of the fascial defect, with no consensus. Described treatments include decompressive fasciotomy, direct primary fascial repair, tibial periosteal flap, fascial patch grafting or stripping (woven strips of fascia) using autologous fascia lata and the use of synthetic mesh. Every operation has disadvantages and potential complications that must be weighed. The safest surgical option for the treatment of symptomatic muscular hernias of the leg is a longitudinal fasciotomy. This belief is the opinion of the authors and one shared by others. Almost all techniques involve surgical exploration, which allows for dissection and release of the involved nerve. Fasciotomy treats the muscle hernia by enlarging the defect and eliminating risks of muscle ischemia or strangulation, which are potential causes of pain. Most importantly, it eliminates any future risks of acute or chronic compartment syndrome, which can still occur with anatomical repair of the fascia. Potential complications with fasciotomies are universal to any surgery in the lower extremity that crosses a musculofascial plane and includes exposed tendon or bone, neuromuscular damage with dysesthesias or weakness, muscle herniation and venous disease from disruption of the calf muscle pump. Incomplete pain resolution may occur with fasciotomies [2]. Achieving a successful outcome is predicated on performing the correct surgery and setting expectations accordingly. The generally accepted incidence of success after decompression of a SPN trunk is approximately 85%. Failure of any decompression should be looked at closely and the surgeon needs to evaluate carefully why the surgery may have failed. The longer a patient has had the condition then the less likely the chance of a positive outcome. It is also important to determine if there are any other peripheral nerve contributions to a patient’s pain that may have been missed, including more proximal pathology, such as lumbosacral pathology. Any central nervous system issues also must be ruled out, especially a patient who may have centralized nerve pain [9,10].
Differential Diagnosis
A variety of differential diagnoses for which muscular hernias have been mistaken require exclusion, including hematomas, varicosities, angiomas, arteriovenous malformations, epidermoid cysts, lipomas, schwannomas, tumours and ruptured muscle (pseudohernia). Although a clinical diagnosis, variable symptoms and a lengthy differential list may present a diagnostic challenge [2,4,5,8]. Both ultrasonography and MRI can demonstrate interruption of the deep fascia with the herniation of a peripheral muscle component in continuity with the rest of the muscle fibers, showing the same echogenicity and signal intensity of the muscle itself. These features can help differentiate muscle hernias from the following lesions.
Hematomas
They are usually subcutaneous, localized in the site of a just known anamnestic trauma with features depending on the timing; subacute and chronic hematomas are usually well defined with a variable echogenicity depending on liquefaction and degree of blood clot organization. They are usually avascular with mild peripheral hyperemia and often show fluid areas. Therefore also MRI findings will be variable. In T1w-T2w-PDw fat-sat sequences hematomas show heterogeneous intensity related to hemoglobin degradation and timing, subcutaneous edema, irregular indistinct margins in the acute phase and more regular margins when organized in the subacute and chronic phase. Typical, even if not always present, the blooming artifact due to hemosiderin deposition in T2*wGRE sequences and hyperintense foci when subacute in T1w fat-sat sequences. Finally they usually do not show significative intensification after contrast administration.
Varicosities, Angiomas, Arteriovenous malformations
They are usually tubular vascular structures or solid masses with tubular vascular structures associated to connective tissue, with polilobulated margins and vascular signs at Echo-Color-Doppler exam. They typically show phleboliths. MRI findings include T1w isointensity to hypointensity relative to skeletal muscle with foci of adipose tissue or slow flow blood, T2w hyperintense vascular regions in slow flow lesions or signal voids in high flow lesions. Vascular regions intensely enhance while little or no early enhancement can be present in large cavitary lesions due to slow flow.
Epidermoid cysts
Ultrasonographic findings depend on maturation of cyst, compactness and amount of keratin. Most are subcutaneous, ovoid, unilocular, heterogeneous mildly hyperechoic, with increased acoustic transmission and thin capsule. Usually they do not present subfascial extension and show a hypoechoic punctum between cyst and dermis. In T1w images they appear isointense to slightly hyperintense, in T2w-PDw fat-sat images hyperintense with high or low signal content depending on the amount of debris and usually show only thin capsule enhancement after contrast administration.
Lipomas
They can be classified in subcutanous, subfascial or intramuscular and are often oval, well marginated nodules mildly hypoechoic and discernible from the muscle. They are typically hyperintense in T1w-T2w sequences with homogeneous hypointensity in every sequence with fat signal suppression. They usually don’t show signal intensification after contrast administration.
Schwannomas
They appear as a well-defined homogeneous, hypoechoic, fusiform mass oriented along nerve long axis. Nerve entering and exiting from the tumor is a typical finding and posterior acoustic enhancement is common. MRI can show typical findings like split-fat sign associated muscle atrophy better seen in T1w sequences, target sing and fascicular sign better seen in T2w-PDw fat-sat sequences. Schwannomas tend to show similar to slightly increased signal relative to muscle on T1w sequences and hyperintensity in fluid sensitive sequences. After contrast administration there are variable patterns of enhancement, even if the diffuse one is more typical.
Ruptured muscle
Ultrasound can show discontinuity and retraction of muscle fibers either within muscle or at myofascial junction, the tear filled with hematoma or fluid, associated to muscle and subcutaneous edema. MRI findings include low to intermediate signal intensity hemorrhage associated to hyperintense subacute hemorrhagic foci and loss of normal muscle striations and continuity in T1w sequences. T2w and PDw fat-sat sequences show hyperintense edema, inhomogeneous signal intensity mass due to hemorrhage and perimuscular hyperintense fluid [11,12,13,14].
TEACHING POINT
Muscle herniation is defined as a portion of muscle through acquired or congenital fascial layer defect, that can cause potentially neuropathic symptoms due to nerve compression and MRI exams can demonstrate this correlation. Most symptomatic muscle hernias are successfully treated with conservative therapy. Surgical referral is warranted for patients with moderate to severe symptoms that are not amenable to a conservative therapy. Fasciotomy appears to be the preferred method by most surgeons, having the least complications and the most successful outcomes postoperatively.
Table 1.
Summary table for nerve neuropathy due to leg muscle hernia.
| Etiology | Congenital fascial weakness or acquired fascial defects (post-traumatic or post-surgical) |
| Incidence | Rare: more common tibialis anterior, less common peroneals, lateral head of gastrocnemius and flexor or extensor digitorum longus. |
| Gender Ratio | More frequent in men |
| Age predilection | Adolescents or young adults |
| Risk Factors | Occupational (military soldiers) and sporting activities (athletes, mountain climbers, skiers), trauma, chronic compartment syndrome and weakness in the overlying fascia due to perforating vessels. |
| Treatment | The first option is conservative treatment and it includes the limitation of physical activity, the use of compressive stockings, partial weight-bearing. The second option is surgical treatment; optimal surgical treatment is controversial with no consensus, including fasciotomy, primary repair of defect fascia, patch repair, synthetic mesh. |
| Prognosis | Most symptomatic muscle hernias are successfully treated with conservative therapy. The safest surgical option is longitudinal fasciotomy. |
| Findings on imaging |
|
Table 2.
Differential diagnosis table for muscle hernias.
| Ultrasound | Magnetic Resonance | |
|---|---|---|
| Muscle Hernia | Interruption of the deep fascia where the nerve becomes subcutaneous with herniation of a peripheral muscle component with same echogenicity of the muscle. |
|
| Hematomas | Subcutaneous, heterogeneous echogenicity depending on the timing, lack of fascial defect and muscle continuity. Subacute and chronic timing: well defined, variable echogenicity depending on liquefaction and degree of blot clot organization. Fluid areas. Avascular. |
|
| Varicosities, Angiomas, Arteriovenous aneurysms | Tubular structures or masses with tubular structures, polilobulated margins and vascular signs at Echo-Color –Doppler exam. Phleboliths. |
|
| Epidermoid cysts | Depend on maturation of cyst, compactness and amount of keratin. Most are ovoid, unilocular, heterogeneous mildly hyperechoic, with increased acoustic transmission and thin capsule. No subfascial extension. Hypoechoic punctum between cyst and dermis. |
|
| Lipomas | Subcutaneous, subfascial or intramuscular, oval well marginated nodule mildly hypoechoic and discernible from the muscle. |
|
| Schwannomas | Well defined homogeneous, hypoechoic mass, fusiform oriented along nerve long axis. Nerve entering and exiting from tumor. Posterior enhancement is common. |
|
| Ruptured muscle | Discontinuity +/− retraction of muscle fibers either within muscle or at myofascial junction. Tear filled with hematoma or fluid +/− muscle and subcutaneous edema. |
|
ABBREVIATIONS
- CECS
chronic exertional compartment syndrome
- MRI
Magnetic Resonance Imaging
- PDw fat sat
PD weighted sequence with fat saturation
- SPN
superficial peroneal nerve
- T1w
T1 weighted sequence
- T1w fat sat
T1 weighted sequence with fat saturation
- T2w
T2 weighted sequence
REFERENCES
- 1.Paolasso I, Cambise C, Coraci D, et al. Tibialis anterior muscle herniation with superficial peroneal nerve involvement: ultrasound role for diagnosis and treatment. Clin Neurol Neurosurg. 2016 Dec;151:6–8. doi: 10.1016/j.clineuro.2016.09.019. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen JT, Nguyen JL, Wheatley MJ, Nguyen TA. Muscle hernias of the leg: A case report and comprehensive review of the literature. Can J Plast Surg. 2013 Winter;21(4):243–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Oktay B, Tevfik Y, Murat G, Mehmet K. Muscle herniation of the extremities: two case report. Prog Orthop SCI. 2016;2(1):4–7. [Google Scholar]
- 4.Toms AF, Rushton LA, Kennedy NR. Muscle herniation of the peroneus longus muscle triggering superficial fibular nerve paresthesia. Sonography. 2017;5:36–40. [Google Scholar]
- 5.Artul S, Habib G. The importance of dynamic ultrasound in the diagnosis of tibialis anterior muscle herniation. Crit Ultrasound J. 2014 Sep 4;6(1):14. doi: 10.1186/s13089-014-0014-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma N, Kumar N, Verma R, Jhobta A. Tibialis Anterior Muscle Hernia: A case of Chronic, Dull Pain and Swelling in Leg Diagnosed by Dynamic Ultrasonography. Pol J Radiol. 2017 May 31;82:293–295. doi: 10.12659/PJR.900846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Khaladkar SM, Kondapavuluru SK, Kamal A, Kalra R, Kamal V. Detection of Myofascial Herniation on Dynamic Sonography and Magnetic Resonance Imaging. Case Rep Radiol. 2016;2016 doi: 10.1155/2016/4245189. 4245189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mellado JM, Perez del Palomar L. Muscle hernias of the lower leg: MRI findings. Skeletal Radiol. 1999 Aug;28(8):465–9. doi: 10.1007/s002560050548. [DOI] [PubMed] [Google Scholar]
- 9.Bregman PJ, Schuenke M. Current Diagnosis and Treatment of Superficial Fibular Nerve Injuries and Entrapment. Clin Podiatr Med Surg. 2016 Apr;33(2):243–54. doi: 10.1016/j.cpm.2015.12.007. [DOI] [PubMed] [Google Scholar]
- 10.Molavi S, Huettner F, Durand P, Djohan R. A Rare Finding of Symptomatic Bilateral Lower extremity Hernia. Orthopedic Muscul Syst. 2014;3(2):154. [Google Scholar]
- 11.Manaster BJ. Muscoloskeletal non-traumatic disease. 2nd ed. Salt Lake City, UT: Elsevier Inc; 2016. Section 3 Soft tissue tumors; pp. 474–687. [Google Scholar]
- 12.Griffith JF. Diagnostic Ultrasound Musculoskeletal. Philadelphia, PA: Elsevier; 2015. Section 3 Soft tissue, Bone and joint injury; II-3-14– II-3-31. Section 8 Soft tissue and Bone tumors II-8-8– II-8-49. [Google Scholar]
- 13.Costantinou M, Vincenzino B. Differential diagnosis of a soft tissue mass in the calf. J Orthop Sports Phys Ther. 2005 Feb;35(2):88–94. doi: 10.2519/jospt.2005.0814. [DOI] [PubMed] [Google Scholar]
- 14.Kotha KM, Tandra VS, Murthy GV, Vutukuri SR, Vyjayanthi Y. Tibialis anterior partial rupture mimicking muscle hernia: a rare case report. J Clin Diagn Res. Oct;8(10):L08–9. doi: 10.7860/JCDR/2014/10410.5056. 214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asp AR, Marsland D, Elliot RR. The superficial peroneal nerve: A review of its anatomy and surgical relevance. OA Anatomy. 2014 Mar 15;2(1):6. [Google Scholar]