Abstract
Objective:
The aim of the study was to analyze diverse patients' experiences throughout the medication use process to inform the development of overarching interventions that support safe medication use in community settings.
Methods:
Using a qualitative observational approach, we conducted approximately 18 hours of direct observation of the medication use process across multiple settings for a sample of vulnerable, high-risk patients. Observers recorded detailed field notes during the observations. To enrich the observational findings, we also conducted six semistructured interviews with medication safety experts representing a diversity of perspectives. Barriers and facilitators to safe medication use were identified based on inductive coding of the data.
Results:
Avariety of safety vulnerabilities plague all stages of the medication use process and many of the well-established evidence-based interventions aimed at improving the safety of medication use at key stages of the process have not been widely implemented in community settings observed in this study. Key safety vulnerabilities identified include: limited English proficiency, low health literacy, lack of clinician continuity, incomplete medication reconciliation and counseling, unsafe medication storage and disposal habits, and conflicting healthcare agendas with caregivers.
Conclusions:
Our findings underscore a need for overarching, comprehensive interventions that span the entire process of medication use, including integrated communication systems between clinicians, pharmacies, and patients, and a “patient navigator” program that assists patients in navigating the entire medication-taking process. Collective ownership of the medication management system and mutual motivation for devising collaborative solutions is needed among key sectors.
Keywords: outpatient medication use, medication safety, qualitative research, direct observation
The use of prescription drugs in the United States is on the rise—increasing from an estimated 51% of adults reporting use of prescription drugs in 1999 to 2000 to an estimated 59% of adults reporting use in 2011 to 2012.1 Medication errors, or failures in the medication use process that lead to, or have the potential to lead to, patient harm,2 are a leading cause of patient morbidity and mortality.3 As such, medication use is a critical patient safety issue in the United States. Medication use in community or outpatient settings, in particular, is associated with specific safety concerns, because patients interact with a variety of medical professionals across multiple care sites. In addition,patients and caregivers mostly self-administer and self-manage their medications in the outpatient setting, often with little support from health professionals.3 This specific quandary in outpatient care lends itself to unique patient safety issues related to medication use. Approximately 4.5 million ambulatory visits related to adverse drug events (ADEs), injuries due to medication, occur each year—the majority of those in outpatient practices.4
Vulnerable patient populations, including those with limited health literacy, low English proficiency, the elderly, and those taking multiple or high-risk medications are especially susceptible to unsafe medication use in the outpatient setting. The elderly, for example, use primary care more frequently and are prescribed more medications,3 as compared with younger populations, making them at higher risk for preventable ADEs.5 Patients with limited health literacy and limited English proficiency are at especially high risk for misunderstanding medication instructions6-8 and are at higher risk of adverse events with greater harm.9 Patients taking multiple and high-risk medications, such as an anticoagulant, opioid, or hypoglycemic, also face unique challenges and higher risk of ADEs.10,11
Research has found that medication errors in primary care occur across all stages of the medication management system, which includes prescribing, transcribing, dispensing, administration, and monitoring stages.3 Previous medication error studies have typically focused on assessing single stages within the medication management system12 and have found that the prescribing and administration stages are the most susceptible stages to medication error.13 Research is limited, however, that holistically evaluates medication use in the context of system assessment and identification of overarching improvement needs from the perspective of patients.3 To this end, we aimed to (1) develop a comprehensive portrayal of outpatient medication use across multiple settings from the perspective of diverse patients, (2) contextualize this description of outpatient medication use with input from multistakeholder medication experts, and (3) put forward recommendations for overarching interventions to support safer medication use.
METHODS
Direct Observation
Direct observation of patient care has been used as a reliable qualitative research method to measure errors and adverse events in healthcare,14 observe team behavior and group processes in operating rooms during procedures,15 investigate the nature and causes of human errors in the intensive care unit,16 assess how health care professionals identify adverse events in the course of their regular tasks in surgical wards,17 and detect errors during medication administration.18,19 Although this methodology is time-intensive and requires training and experience to ensure the reliability of the data collected, previous research has found that direct observation produces results that are significantly more valid, accurate, and reliable than other methods.14
We recruited six patients for three rounds of direct observation (n = 18 observations) using purposive sampling to capture the medication use experience for a diversity of patients. Study investigators (A.E.S. and H.C.L.) recruited and observed patients from subspecialty clinics at a safety-net hospital that primarily serves medically uninsured, low-income, minority patients in an urban San Francisco Bay Area location, and study investigator (E.S.P.) recruited and observed patients from an outpatient clinic affiliated with a large academic medical center in Ohio during the fall of 2017. We reviewed clinic rosters and met with clinicians before identifying patients who met eligibility criteria; patients were eligible to participate if they (1) were older than 18 years; (2) had adequate cognitive ability to consent to participate; and (3) were receiving care and medication prescriptions from either of our two study sites. We approached patients in the clinic waiting room or exam room before their scheduled medical appointments to explain the study and obtain their consent to participate in the study. The first three patients from each study site who met all eligibility criteria and were amenable to having study investigators observe them for up to 3 hours on the day they were approached were enrolled in the study. Study investigator (A.E.S.) is proficient in English and Spanish and consented low English proficient Spanish-speaking patients into the study. Otherwise, all consent and observation procedures were conducted in English.
We targeted observations of the following three key stages of the medication management system: the prescribing stage (clinician's office), the dispensing stage (the pharmacy), and the administration stage (the home). Each observation sequence lasted approximately 3 hours. Study investigators recorded detailed field notes20 of the medication use experience from the patients' perspectives with a particular focus on issues of communication between the patient and the clinician and the patient and the pharmacist; patient comprehension of medication instructions and warnings; caregiver involvement; patient medication storage; patient medication adherence; and possible unintentional medication misuse. Occasionally, observers asked patients for clarification regarding their experiences, but otherwise, they were quiet observers.
Expert Interviews
Multistakeholder medication experts (n = 6) were recruited via e-mail during February 2018 using a purposive sampling approach in an effort to capture a diverse range of stakeholder perspectives. Individuals were eligible to participate if they were professionals in the field of medication use and patient safety. Initial prospective interviewees were identified based on study authors' professional contacts in the field of medication safety. We then used snowball sampling to ask initial interviewees to suggest other medication safety experts that we should contact. In total, we contacted eight experts and six agreed to participate. Study authors (K.M.M. and H.C.L.) conducted in-depth, semistructured interviews with the experts during February and March 2018 as a quality assurance check on data saturation and to contextualize the findings from the direct observation phase of the study. As such, our sample size was based on previous qualitative research that has found that samples as small as four individuals can be sufficient in providing complete and accurate information, as long as the participants possess a certain degree of expertise about the domain of inquiry,21 and that data saturation and thematic exhaustion can be reached after six interviews.22
Each interview lasted approximately 1 hour. Interviews were audio recorded and later transcribed for analysis. Study investigators recorded detailed notes during the interviews. Interview questions were open-ended and focused on participants' sense of the scope of the problem regarding patient safety and outpatient medication use, including how well medication safety events are being detected in community settings and what the biggest safety concerns are with outpatient medication use, as well as their general impressions of our direct observation findings, including their perspectives on our identified safety vulnerabilities.
All study procedures were approved by the University of California San Francisco's institutional review board.
Data Analysis
Field notes and interview transcripts were analyzed using an inductive content analysis approach23 to identify recurrent and overarching themes. Barriers and facilitators to safe medication use were identified from the field notes and key safety vulnerabilities experienced by the patients were grouped by setting, including the clinician's office, the pharmacy, and the home. Interview transcripts, meanwhile, were inductively coded for key themes and coding differences among study investigators were resolved via discussion until consensus was reached on salient, overarching themes.
RESULTS
Table 1 summarizes key characteristics and medical histories of the recruited patients. The patients range in age from 30 to 70 years and are primarily from low-income minority groups. Two are male and four are female, and four of the six patients have some form of caregiver support. Although we did not conduct formal assessments of English proficiency or health literacy, we classified half of the patients as having low English proficiency and four as having low to moderate health literacy, based on our observations of the patients.
TABLE 1.
Patient Characteristics
| Patient | Sex | Age | Race/Ethnicity | Socioeconomic Status |
Caregiver Support |
English Proficiency |
Health Literacy |
Medical History | Medications |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Female | 30s | White | Low income | NA | High | Moderate | Anxiety, asthma, back pain, overweight, PTSD | Levalbuterol, acetaminophen, ibuprofen, fluoxetine |
| 2 | Male | 60s | Black | Low income | Girlfriend | High | Low | Cirrhosis of the liver, HTN, high cholesterol, carpal tunnel syndrome, depression, COPD | Lisinopril, chlorthalidone, atorvastatin, oxycodone, acetaminophen, ibuprofen |
| 3 | Male | 50s | White | Middle income | Wife | High | High | Type II insulin-dependent diabetes, degenerative arthritis, HTN, overweight, melanoma | Insulin, alfuzosin, trazodone, omeprazole, triamterene, losartan, bupropion, sumatriptan, vitamin D, cetirizine, loperamide |
| 4 | Female | 70s | Filipino | Low income | Niece | Low | Low | Diabetes, valvular disease of the heart, HTN, CKD, celiac disease, Hypothyroidism, essential tremor | Amlodipine, metformin, losartan, propranolol, atorvastatin, levothyroxine, insulin, vitamin B, iron, multivitamin, aspirin |
| 5 | Male | 50s | Hispanic | Low income | NA | Low | Low/moderate | HTN, chronic back pain | Oxycodone, lisinopril |
| 6 | Male | 60s | Hispanic | Low income | Health worker | Low | Low | HIV, HTN, CKD, DVT, prostate issues | Warfarin, atorvastatin, fish oil, coenzyme Q10, docusate sodium, losartan, abacavir/lamivudine, nevirapine, raltegravir, fiber supplement, terbinafine, clotrimazole, finasteride, tamsulosin, oxybutynin, triamcinolone acetonide, vitamin D3 |
COPD, chronic obstructive pulmonary disease; DVT, deep vein thrombosis; PTSD, posttraumatic stress disorder.
The patients' medical histories vary in complexity from a history of back pain and hypertension (HTN) (Patient 5) to a history of multiple and high-risk conditions including HIV, HTN, chronic kidney disease (CKD), deep vein thrombosis (DVT), and prostate issues (Patient 6). Because of the varying nature of each patient's medical background, their medication regimes also differ substantially from regularly taking more than eight prescribed medications (Patients 3, 4, and 6) to taking only two prescribed medications daily (Patient 5). What is more, several of the patients are prescribed high-risk medications, including opioid (Patients 2 and 5), anticoagulant (Patient 6), and hypoglycemic (Patient 4).
Safety Vulnerabilities
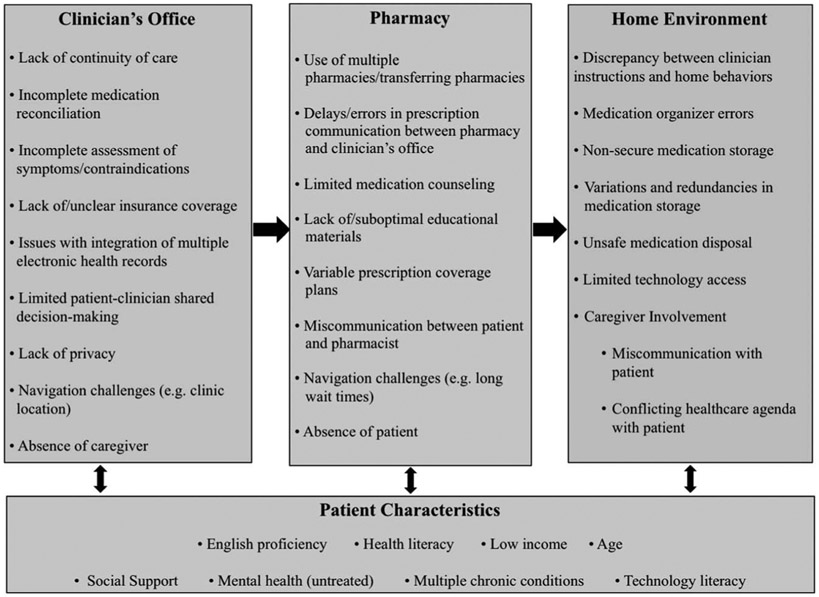
We observed numerous safety vulnerabilities experienced by the patients as they traversed different stages of medication management (Fig. 1). At the prescribing stage, we observed clinician discontinuity as a key safety vulnerability. For example, during Patient 6's appointment with a nurse practitioner for anticoagulation management, he brought up several concerning symptoms and adverse effects during his medication reconciliation, including bruising, lower extremity swelling, and chest pressure. The nurse practitioner deferred his concerns to be addressed by the patient's primary care physician at a later time. Limited patient-clinician shared decision-making was another safety vulnerability we identified at the prescribing stage. Patient 4, a Tagalog-speaking Filipina female, for example, complained of tendon pain during her medical appointment but did not participate in shared decision-making with her clinician because of her limited English proficiency and health literacy. The clinician made the decision alone to prescribe the patient a calcium supplement to treat her tendon pain.
FIGURE 1.
Observed safety vulnerabilities.
At the pharmacy stage, insufficient medication counseling was a key safety vulnerability identified. Patient 1, for example, received limited patient education for her newly prescribed antidepressant prescription. The pharmacist did not provide a full counseling session, failed to obtain teach-back to ensure the patient understood information about the drug, and shared only very brief answers to her questions regarding the new medication. The use of multiple pharmacies was another key observed safety vulnerability. Patient 6, in particular, uses two pharmacies to fill his prescriptions—a retail pharmacy located in his neighborhood and another pharmacy that mails his prescriptions to him. His use of more than one pharmacy leads to prescription redundancy and significant confusion surrounding his refills, because some of the refills are sent to only one pharmacy, and some are sent to both. Lastly, because the pharmacy systems do not communicate with each other, any serious and critical drug-drug interactions risk are not being identified or addressed.
We also identified key safety vulnerabilities that occurred in the home environment. First, incorrect use of medication dosing aids (e.g., weekly pill organizers) emerged as an important safety vulnerability. Patient 4, for example, who takes nearly a dozen prescribed medications daily, diligently sorts out her dailymedications into a weekly pill organizer on a regular basis. Her weekly pill organizer has compartments for morning and evening medications; however, she uses one compartment for an entire day’s worth of medications and relies on memorizing the shapes and colors of the pills to know which to take in the morning and which to leave for the evening. What is more, one of the pill compartments on the organizer is broken, so she skips that compartment when refilling the organizer.
We also observed variations in medication storage across all six patients. Patient 5, for instance, keeps his medications in multiple locations throughout his house—his opioid pain medication is in the top drawer of his dresser in his bedroom, and his HTN medicine inside a woven bag that he keeps on the floor of his bedroom closet. He also has sorted medications in a pill organizer on his kitchen table, and he has a small metal canister that he keeps on his key chain with a twist-off top that he uses to carry his medications with him when he leaves the house. In addition, we observed unsafe medication disposal in the patients' home environments. Patient 1 flushes unused medications down the toilet, whereas Patient 6 mentioned that he has a place where he takes his expired medications. During our home visit, however, we observed numerous bottles of expired medications that had not been properly disposed.
Our analysis also revealed several patient-specific characteristics that represented barriers to safe medication use. Limited English proficiency, for example, was a key safety vulnerability. Patient 6, for example, is Spanish-speaking and had difficulty communicating in English to the technician at the pharmacy regarding his need for medicated eye drops and whether his blood thinner prescription refill was ready to be picked up. Ultimately, the patient left the pharmacy without eye drops or his prescription refill. Miscommunication and misunderstanding between the patient and the technician about the patient's medications occurred in part because of language discordance, despite the patient's repeated requests for Spanish interpretation. Mental health was another patient-specific characteristic we observed. Patient 1, for example, experiences uncontrolled anxiety and has a history of not taking prescribed medications. During her medical appointment, the patient was prescribed an antidepressant, but the patient communicated that she is afraid to take the medication and feels anxious about the adverse effects, underscoring her untreated mental health as a key barrier to medication adherence and safe medication use.
Finally, we identified safety vulnerabilities associated with caregiver involvement in the medication use process. Patient 4's niece brings the patient to appointments but waits in the lobby during the appointments. She also regularly picks up the patient's prescriptions for her from the pharmacy and drops them off at her home without the patient present. The absence of the caregiver during the medical appointments and the patient during the pharmacy stage of the medication use process is a barrier to safe medication use when shared knowledge across contexts is important. The patient never interacts with the pharmacist, whereas the caregiver misses important medication instructions during the medical appointment.
Expert Interviews
Table 2 describes the sample of multistakeholder medication experts interviewed. Three experts are practicing primary care physicians, one is a patient safety advocate, one is a pharmacist, and one is a clinical product manager at a pharmacy benefit manager company. The experts represent varied perspectives on outpatient medication use, including prescriber, health system (clinic and network level), pharmacy, patient, and payer viewpoints.
TABLE 2.
Multistakeholder Medication Expert Characteristics
| Expert | Job Description | Setting | Perspective |
|---|---|---|---|
| 1 | Primary care physician; medical director of a primary care clinic | Safety net | Prescriber, health system |
| 2 | Primary care physician | Community clinic | Prescriber |
| 3 | Retail pharmacist | Retail pharmacy | Pharmacy |
| 4 | Patient safety advocate | Nonprofit organization | Patient |
| 5 | Primary care physician; director of a network of primary care clinics | Safety net | Prescriber, health system |
| 6 | Clinical product manager | Pharmacy benefit manager company | Payer |
Analysis of our interviews validated the key safety vulnerabilities we identified across the patients' experiences and contextualized our findings. In particular, the experts emphasized time constraints, limited communication between clinicians, pharmacists, and prescription insurance companies, and challenges with the design of electronic health record (EHR) systems as key factors underlying many of the safety vulnerabilities we observed (Table 3).
TABLE 3.
Multistakeholder Medication Expert Interview Key Themes
| Theme | Quotes |
|---|---|
| Time constraints | “Even though we should do [medication reconciliation], I try to do it for every single patient, but it's not being done as thoroughly as we'd like because of the time crunch.” (Expert 2) “I think one of the barriers perhaps to medication safety is just the volume of prescriptions that are being processed at the pharmacy level. So, again, just not having that time to really talk to the patient.” (Expert 3) |
| Limited communication among clinicians, pharmacists, and insurance companies | “In some cases, the pharmacist can communicate to us [through the EHR] but we can't communicate directly back to the pharmacist. Even when I can communicate directly back to the pharmacist, I'm never assured that segment actually works. So, I don't feel like we have a two-way communication with the pharmacy.” (Expert 1) “I think the biggest one really that stands out is just the [communication] delays between the pharmacy and the doctor's office and even between the insurance company and us. For some of the medications that aren't covered, the patient will decide to pay out of pocket, but if that's not an option, then they'll just be without their medications for a couple of days while we wait to hear back from their insurance company.” (Expert 3) |
| Issues with EHR design | “You'll get a warning for basically any medicine you prescribe. There's definitely a warning for anything and then you just can't read them all. I think that's the problem any EHR-based thing.” (Expert 5) “The pull-down field in our EHR is so poorly designed that I think it probably actually leads to delays in treatment in some cases. It's not designed in a way to help the clinician get to the most generic and widely available type of that medication that's most likely to be covered by all insurance types. So, I think we're constantly putting in a weird form of medication that then goes to the pharmacy, it gets bounced back to us, it takes a while for us to figure out what happened, we don't know what's wrong with it. I think that there's probably a lot of delays in getting the patient the right medications, in part because of some of the flaws of our EHR.” (Expert 1) |
First, the interviewees couched many of the vulnerabilities we identified, including limited medication reconciliation, lack of patient-clinician shared decision-making, and insufficient medication counseling, in the context of time constraints that clinicians and pharmacists face on a regular basis. For example, Expert 3, a retail pharmacist, told us how the volume of prescriptions she handles creates a rushed environment in the pharmacy in which she lacks the time to speak with patients to conduct thorough medication counseling. Similarly, Expert 2, a physician, explained how he simply lacks the time to do in-depth medication reconciliation or education with all of his parents because he is “so damn busy.”
The experts also confirmed from their professional experience that fractured communication between clinicians, pharmacists, and insurance companies contributes to many of the observed safety vulnerabilities. For example, Experts 1 and 2 explained how it is difficult for clinicians to communicate with outside retail and community pharmacies because they are never assured that the messages they send through the EHR actually go through to the pharmacy. Expert 3, a retail pharmacist, also pointed out that fragmented communication creates safety vulnerabilities in which patients may have to go days without their medications while the pharmacy waits to hear back from the insurance company or the prescriber.
Challenges with the design of EHRs was a third key theme emerging from expert commentary on our observed safety vulnerabilities. Expert 2, for instance, described how many clinicians experience “alert fatigue” with the EHR systems, in which they get in the habit of ignoring the warnings regarding potential drug interactions because of design weaknesses.24 Expert 1, meanwhile, explained how suboptimal EHR design can lead to delays in care. For instance, she described how there are 57 different 81-mg aspirins in the EHR pull-down menu and the clinician might not find the right one, causing the prescription to bounce back from the pharmacy without being filled for the patient.
Finally, the experts generated several additional or more specific safety concerns related to medication use based on their individual experiences, including opioid medications, polypharmacy, and language discordant medication labels (Table 4).
TABLE 4.
Multistakeholder Medication Expert Interview Safety Concerns
| Safety Vulnerability | Quotes |
|---|---|
| Opioid medications | “The narcotic or opioid utilization—that I think is probably one of the biggest and most well known at this point in time as far as medication safety issues.” (Expert 6) |
| Medication labels | “It's already hard to understand a medication label, and if it's not even in your language, it's even more hard to understand.” (Expert 1) |
| Polypharmacy | “To me, the big issue is polypharmacy. That people are taking a lot of drugs that they don't understand. The prescribers don't necessarily understand and no one will know about the interactions of a lot of these things. I think it's just such a critical issue, people taking too many drugs.” (Expert 4) |
| Confusing refill procedures | “One thing that is absolutely missing is this whole idea of the refill system. I'm finding that patients do not understand the refill system at all like on the label. So what ends up happening is we give them three months' worth of medication, they stop after one month and it's like “I don't know. I didn't know I was supposed to go and refill.” They come back and they're like, “Why is it time to change it? I'm done with the medication.” You need to actually teach the patient how to refill the medications, what to look for on the labels.” (Expert 2) |
| Generic versus brand name medication confusion | “I've found that for generics, they are made by different manufacturers so I've heard time and time again where patients complain and because they don't read the labels, especially my patients who are Chinese-speaking, they say “It's an oblong pill, now it's a diamond-shaped pill. I don't know what they are. Gosh, I'm afraid to take it because it's different from what I'm used to.” They switch manufacturers without telling the patients or warning them and I can imagine anybody who is used to taking one pill looking at a different type of pill, just totally not taking it anymore.” (Expert 2) |
| Clinician-specific characteristics | “There's a lot of prejudice against patients and assumptions that if you're low income, they've got to be dumb, if they have mental health issues, you shouldn't pay attention to what they say There's a lot of that. I think the physician characteristics, prescriber characteristics, they're in this too. I think it's really important that the physician characteristics are as important. You get people who are dismissive and rushed, maybe not adequately trained. I think how clinicians act—if they're not sensitive to how these patients are responding to them, mistakes are going to happen.” (Expert 4) |
| Unstable housing | “I would add unstable housing, homelessness, group housing, things like that. So many people say, “My medicines were stolen,” or whatever, if they're living in shelters.” (Expert 5) |
| Insufficient pharmacy staffing | “Oftentimes during the evening rush hour times there is just two people: the pharmacist and one tech. If the store is lucky, someone from out on the floor will come to the pharmacy to help ring up customers at the registers; but you can imagine that they are not familiar with the pharmacy system or how to process new prescriptions. Meanwhile the pharmacist and the tech are overwhelmed with a flood of phone calls, new prescriptions, flu and other vaccines, doing stock checks, and multiple priorities piling up at once. Bottom line, not enough man power to meet the demand.” (Expert 3) |
| Lack of consistent pharmacy policies | “Lack of consistency maybe between the different pharmacies on their policies. For example, for the high-risk medication, some pharmacies require a driver's license of a patient every time they pick up. Other pharmacies, they don't do that. For different locations that I've been to, there's different requirements. Well that kind of confuses the patient also and also gets them frustrated. A lot of times we'll say, “I apologize. It's the policy of the pharmacy.” I mean they might just take their medication and go somewhere else.” (Expert 3) |
| Coupons to transfer pharmacies | “I remember one of the biggest pain points when I was in retail pharmacy was the coupon to transfer to a different pharmacy…It was a nightmare from the retail side because we're constantly calling pharmacies to transfer. It's like 10 to 20 medications that you're transferring on the phone, person-to-person, so the room for error was definitely large, but then you just have this idea that there's no continuation of care. There's no rapport with the same pharmacist over and over again. You're just constantly jumping ship because of the coupon.” (Expert 6) |
DISCUSSION AND RECOMMENDATIONS
Our results highlight that medication use remains a complex, confusing, multistep process that spans fragmented and disconnected stages of the health care system. In this overwhelming environment, patients develop their own strategies for self-management with little support or oversight from healthcare professionals. In addition, our results reveal how no single organization is accountable for designing a system that oversees and supports the many different actors and locations involved in medication use and management. Numerous safety vulnerabilities arise as patients and their caregivers cross formal and informal organizational boundaries between the clinician's office, the pharmacy, and the home.
Supporting previous research that has found that a broad culture of change, combined with well-designed technologies, is necessary to improve the quality and safety of the medication use process,25 our results highlight that a systems approach is needed to improve patient safety in relation to medication taking in community settings. Specifically, our findings emphasize an urgent need to foster collective ownership of the medicationmanagement system among key stakeholders across different settings to encourage mutual motivation for devising collaborative solutions. Moving beyond isolated interventions targeted at single stages of the medication management system requires a culture shift to develop and implement comprehensive, overarching structural interventions that span and support the entire process of medication use.
First, we suggest consideration of a comprehensive “medication navigator” program modeled after traditional patient navigator programs that have been successfully implemented at all stages of cancer care for underserved patients.26-28 In a medication navigator program, patients would be partnered with a skilled medication specialist at the time a medication is first prescribed who would (1) teach patients about their medication, including how to properly administer and store it and (2) help patients navigate the entire medications management system, including prescription coverage, identifying an appropriate pharmacy they are comfortable with, and how to manage refills and disposals. Through expert knowledge, flexible problem-solving, and individualized assistance, a medication-specific navigator program could help patients transcend barriers to safe medication use across all stages of the process.
Next, to address structural linkages, we suggest the development of robust, integrated communication systems to enhance awareness of potential adverse events between clinicians, pharmacies, and patients. In line with previous Institute of Medicine recommendations for reducing medication errors,25 we suggest that these comprehensive communication systems rely on drastically improving EHR linkages between clinics, pharmacies, and insurance companies to facilitate efficient sharing of accurate information and may include reporting systems that are accessible to nonclinicians as well as patients, or standardized expectations between clinics, pharmacies, patients, and caregivers.
Finally, building on the success of mHealth text message-based interventions to support patient-centered treatment and medication adherence,29 we recommend the development of technology-enabled medication self-management support tools that would help decrease patient-specific safety vulnerabilities with medication taking. Ideally, these would be interactive tools such as mobile applications and/or instructional videos, which would be available in multiple languages and at a basic reading level, and would serve to address common pitfalls of medication use. These tools should be co-developed and pilot tested with target end-user populations to ensure optimal usability.
Study Limitations
Our study has a few limitations. First, our relatively small sample size of patients and limited duration of observations limit the generalizability of our findings. Nevertheless, common vulnerabilities were found among our sample of diverse patients, and focusing on a smaller sample provides a richer, more granular look at medication taking from the patient and caregiver perspective. Future qualitative studies exploring a broader set of themes related to outpatient medication use, however, would benefit from more prolonged observational periods and a larger sample of patients. Second, although the specific recommendations emanate from the vulnerabilities identified, they have not been tested for effectiveness at addressing the identified issues. Future studies could focus on assessing the implementation and effectiveness of the suggested recommendations across multiple community settings.
CONCLUSIONS
Our study reveals that a variety of safety vulnerabilities plague all stages of the medication use process for a diversity of patients. There is a pressing need for improved and shared accountability for the outpatient medication use process. Overarching interventions focused on improving medication safety for vulnerable patient populations are needed that span the entire medication management system, including a patient navigator program, integrated communication systems, and technology-enabled support tools.
ACKNOWLEDGMENTS
The authors thank the patients, medical staff, and pharmacists who allowed us to observe them, the experts who participated in our stakeholder interviews, the Gordon and Betty Moore Foundation (Grant Number 6890), and the Agency for Healthcare Research and Quality (Grant Number P30HS023558) for funding this research.
This study was supported by Gordon and Betty Moore Foundation (Grant Number 6890) and the Agency for Healthcare Research and Quality (Grant Number P30HS023558).
REFERENCES
- 1.Kantor ED, Rehm CD, Haas JS, et al. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA. 2015;314:1818–1831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Aronson JK. Medication errors: what they are, how they happen, and how to avoid them. QJM. 2009;102:513–521. [DOI] [PubMed] [Google Scholar]
- 3.Olaniyan JO, Ghaleb M, Dhillon S, et al. Safety of medication use in primary care. Int J Pharm Pract. 2015;23:3–20. [DOI] [PubMed] [Google Scholar]
- 4.Sarkar U, Lopez A, Maselli JH, et al. Adverse drug events in U.S. Adult Ambulatory Medical Care. Health Serv Res. 2011;46:1517–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gurwitz JH, Field TS, Harrold LR, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289:1107–1116. [DOI] [PubMed] [Google Scholar]
- 6.Davis TC, Wolf MS, Bass PF 3rd, et al. Literacy and misunderstanding prescription drug labels. Ann Intern Med. 2006;145:887–894. [DOI] [PubMed] [Google Scholar]
- 7.Wolf MS, Davis TC, Tilson HH, et al. Misunderstanding of prescription drug warning labels among patients with low literacy. Am J Health Syst Pharm. 2006;63:1048–1055. [DOI] [PubMed] [Google Scholar]
- 8.Masland MC, Kang SH, Ma Y. Association between limited English proficiency and understanding prescription labels among five ethnic groups in California. Ethn Health. 2011;16:125–144. [DOI] [PubMed] [Google Scholar]
- 9.Divi C, Koss RG, Schmaltz SP, et al. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007; 19:60–67. [DOI] [PubMed] [Google Scholar]
- 10.Wolf MS, Curtis LM, Waite K, et al. Helping patients simplify and safely use complex prescription regimens. Arch Intern Med. 2011;171:300–305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.U.S. Department of Health and Human Services OoDPaHP. National Action Plan for Adverse Drug Event Prevention. Washington, DC; 2014. [Google Scholar]
- 12.Garfield S, Barber N, Walley P, et al. Quality of medication use in primary care—mapping the problem, working to a solution: a systematic review of the literature. BMC Med. 2009;7:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avery AJ, Sheikh A, Hurwitz B, et al. Safer medicines management in primary care. Br J Gen Pract. 2002;52:S17–S22. [PMC free article] [PubMed] [Google Scholar]
- 14.Thomas EJ, Petersen LA. Measuring errors and adverse events in health care. J Gen Intern Med. 2003;18:61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Helmreich RL, Schaefer H-G. Team Performance in the Operating Room. In: Bogner MS, ed. Human Error in Medicine. Hillsdale, NJ: Lawrence Erlbaum Associates, Inc; 1994:225–253. [Google Scholar]
- 16.Donchin Y, Gopher D, Olin M, et al. A look into the nature and causes of human errors in the intensive care unit. 1995. Qual Saf Health Care. 2003;12:143–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andrews LB, Stocking C, Krizek T, et al. An alternative strategy for studying adverse events in medical care. The Lancet. 1997;349:309–313. [DOI] [PubMed] [Google Scholar]
- 18.Barker KN, Flynn EA, Pepper GA. Observation method of detecting medication errors. Am J Health Syst Pharm. 2002;59:2314–2316. [DOI] [PubMed] [Google Scholar]
- 19.Flynn EA, Barker KN, Pepper GA, et al. Comparison of methods for detecting medication errors in 36 hospitals and skilled-nursing facilities. Am J Health Syst Pharm. 2002;59:436–446. [DOI] [PubMed] [Google Scholar]
- 20.Emerson RM, Fretz RI, Shaw LL. Writing Ethnographic Fieldnotes. 2nd ed. Chicago: University of Chicago Press; 2011. [Google Scholar]
- 21.Romney AK, Weller SC, Batchelder WH. Culture as consensus: a theory of culture and informant accuracy. Am Anthropol. 1986;88: 313–338. [Google Scholar]
- 22.Guest G, Bunce A, Johnson L. How many interviews are enough? An experiment with data saturation and variability. Field Methods. 2006;18:59–82. [Google Scholar]
- 23.Weber RP. Basic Content Analysis. Beverly Hills, CA: Sage; 1990. [Google Scholar]
- 24.Slight SP, Seger DL, Nanji KC, et al. Are we heeding the warning signs? Examining providers' overrides of computerized drug-drug interaction alerts in primary care. PLoS One. 2013;8:e85071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bates DW. Preventing medication errors: a summary. Am J Health Syst Pharm. 2007;64(suppl 9):S3–S9. [DOI] [PubMed] [Google Scholar]
- 26.Percac-Lima S, Grant RW, Green AR, et al. A culturally tailored navigator program for colorectal cancer screening in a community health center: a randomized, controlled trial. J Gen Intern Med. 2009;24:211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jandorf L, Gutierrez Y, Lopez J, et al. Use of a patient navigator to increase colorectal cancer screening in an urban neighborhood health clinic. J Urban Health. 2005;82:216–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Burhansstipanov L, Dignan MB, Schumacher A, et al. Breast screening navigator programs within three settings that assist underserved women. J Cancer Educ. 2010;25:247–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sarabi RE, Sadoughi F, Orak RJ, et al. The effectiveness of mobile phone text messaging in improving medication adherence for patients with chronic diseases: a systematic review. Iran Red Crescent Med J. 2016;18:e25183. [DOI] [PMC free article] [PubMed] [Google Scholar]