Abstract
Objective
Between 17% and 40% of patients undergoing elective arthroplasty are preoperative opioid users. This US study analyzed patients in this population to illustrate the relationship between preoperative opioid use and adverse surgical outcomes.
Design
Retrospective study of administrative medical and pharmaceutical claims data.
Subjects
Adults (aged 18+) who received elective total knee, hip, or shoulder replacement in 2014–2015.
Methods
A patient was a preoperative opioid user if opioid prescription fills occurred in two periods: 1–30 and 31–90 days presurgery. Zero-truncated Poisson (incidence rate ratio [IRR]), logistic (odds ratio [OR]), Cox (hazard ratio [HR]), and quantile regressions modeled the effects of preoperative opioid use and opioid dose, adjusted for demographics, comorbidities, and utilization.
Results
Among 34,792 patients (38% hip, 58% knee, 4% shoulder), 6,043 (17.4%) were preoperative opioid users with a median morphine equivalent daily dose of 32 mg. Preoperative opioid users had increased length of stay (IRR = 1.03, 95% CI = 1.02 to 1.05), nonhome discharge (OR = 1.10, 95% CI = 1.00 to 1.21), and 30-day unplanned readmission (OR = 1.43, 95% CI = 1.17 to 1.74); experienced 35% higher surgical site infection (HR = 1.35, 95% CI = 1.14 to 1.59) and 44% higher surgical revision (HR = 1.44, 95% CI = 1.21 to 1.71); had a median $1,084 (95% CI = $833 to $1334) increase in medical spend during the 365 days after discharge; and had a 64% lower rate of opioid cessation (HR = 0.34, 95% CI = 0.33 to 0.35) compared with patients not filling two or more prescriptions across periods.
Conclusions
Preoperative opioid users had longer length of stay, increased revision rates, higher spend, and persistent opioid use, which worsened with dose. Adverse outcomes after elective joint replacement may be reduced if preoperative opioid risk is managed through increased monitoring or opioid cessation.
Keywords: Arthroplasty, Surgery, Opioid, Length of Stay, Costs, Health Outcomes, Readmission, Surgical Revision, Surgical Site Infection
Introduction
Opioid use in the United States remains a major source of morbidity and mortality. Although the exact number of Americans who are prescribed opioids annually remains poorly defined, recent national pharmacy samples estimate that at least 289 million prescriptions for opioids are filled each year [1]. The public health threats related to opioids have been well documented, including an estimated prevalence of 1.9 million Americans who have developed opioid use disorder [2–3], nearly 530 individuals who die each week due to opioid overdose [4], and additional complications resulting in an annual estimated cost of $78.5 billion related to these medications [3].
Despite the many risks of opioid use, these medications are commonly prescribed for patients who are preoperative candidates for elective procedures for degenerative musculoskeletal conditions. Among patients with knee osteoarthritis, the proportion of patients receiving opioids preoperatively has been reported to be 40% and to be steadily increasing each year [5]. Among the general population of patients with osteoarthritis, at least 41% are receiving at least one opioid prescription, creating a sizeable number of individuals at risk from opioids [6]. Although the number of patients who continue use of opioids in the postoperative period is not precisely known, one large study using claims data estimated that among patients undergoing hip or knee arthroplasty, the incidence of persistent use postoperatively may be as high as 7.6% [7].
In addition to general risks inherent to their longstanding use, past research suggests that opioid use among patients who ultimately undergo orthopedic operations is associated with an elevated risk profile during the perioperative period. When compared with patients not using opioids preoperatively, preoperative patients using opioids have been shown to have a lower likelihood of opioid cessation postoperatively, worse functional outcomes, higher likelihood of needing surgical revision, and higher perioperative opioid requirements across multiple types of orthopedic procedures, including knee, hip, and shoulder arthroplasty [8–11]. However, the samples used in these studies have typically been limited to the experience of only a few institutions, and it is therefore difficult to assess the generalizability of the findings and reconcile differing estimates of risk magnitude.
The present study sought to describe the risks of preoperative opioid use among patients undergoing hip, knee, and shoulder joint replacement surgery using a large, multistate commercial insurance database with electronically linked pharmacy billing data. Prior literature examining perioperative outcomes has primarily used matched or cohort data from a single or a few institutions. This study’s goal was to draw from a large geographic catchment area, as medical practice patterns are known to vary across regions, producing markedly different prescribing patterns and medical outcomes. Thus, the present study presents a national sample of the effects of opioid use in the perioperative period for privately insured patients undergoing hip, knee, and shoulder orthopedic operations.
Methods
This work was given a nonhuman subject research determination by the Chesapeake Institutional Review Board (chesapeakeirb.com; Columbia, MD, USA). The study cohort, variable definitions, and statistical methods were specified a priori in a statistical analysis plan.
Study Cohort
This is a retrospective observational cohort study of administrative claims from Blue Health Intelligence in the United States. Adults (aged >18 years) who received elective total joint replacement surgery between January 1, 2014, and September 30, 2015, were eligible for analysis. Specifically, we considered total hip, knee, or shoulder arthroplasty (Current Procedural Terminology codes 27130, 27447, and 23472, respectively). We required continuous enrollment for pharmacy and medical coverage for approximately 24 months (six months before and 18 months after surgery). To avoid duplication of patients with multiple procedures, only the first total joint replacement surgery occurring within the study period was included for analysis. If a patient had evidence of other total joint replacement surgeries occurring in the previous six months (i.e., before the study period), the patient was excluded. Additionally, patients undergoing surgery due to urgent, trauma, or emergency surgical indications were removed.
Exposure
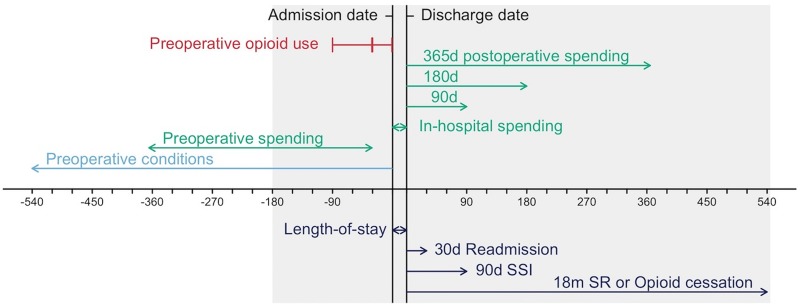
To capture patients with recent and extended opioid use continuing through the perioperative period, preoperative opioid use was given by at least one opioid prescription fill occurring within each of 1–30 days and 31–90 days before the date of admission (Figure 1). For example, opioid use during the week before surgery with no accompanying prescription fill in 31–90 days before surgery did not meet the definition of preoperative opioid use. An opioid prescription fill in 1–30 days before surgery captured recent opioid use and, when coupled with 31–90 days before surgery, additionally captured extended opioid use.
Figure 1.
Diagram of study exposures and end points. Preoperative opioid use was identified among patients with at least one opioid prescription fill occurring within each of 1–30 days and 31–90 days before the date of admission. For example, opioid use during the week before surgery with no accompanying prescription fill in the 31–90 days before surgery does not meet the definition of preoperative opioid use. Preoperative spending and preoperative conditions were captured in 31–365 days and 18 months before admission, respectively. Length of stay and in-hospital spending occur between admission and discharge dates. After discharge, postoperative spending is measured up to 90, 180, and 365 days. Other outcomes include 30-day readmission, 90-day surgical site infection (SSI), 18-month surgical revision (SR), 18-month opioid cessation, and nonhome discharge (not pictured). The gray rectangle gives the minimum continuous eligibility requirement (six months before admission and 18 months after discharge); nearly the entire cohort (99.6%) also had continuous eligibility 18 months before admission, although this was not an inclusion criterion.
Preoperative dose was calculated as the morphine equivalent daily dose for all opioid prescriptions, which is the sum of the morphine equivalence divided by the number of prescription days during the 90 days before surgery. Preoperative dose is only calculated for patients meeting the definition for preoperative opioid use; patients with an opioid prescription but not meeting the definition were assigned a morphine equivalent daily dose value equal to 0.
Outcomes
To characterize the broad impact of preoperative opioid use, a number of utilization and postsurgical outcomes were ascertained for the study cohort, including length of stay, medical spending, discharge location (nonhome discharge), readmission, surgical site infection, surgical revision, and opioid cessation (Figure 1). The exact time of admission and discharge were not available in the administrative claims data; therefore, length of stay was calculated to the nearest whole day as the date of discharge minus the date of admission plus 1. Medical spending was calculated using the total amount paid for medical claims by the commercial insurance plan and the patient during four windows: in-hospital (inclusive of admission and discharge dates) and 90, 180, and 365 days following discharge. Discharge location was dichotomized to home vs facility (including skilled nursing, rehabilitation facility, or inpatient transfer). All-cause unplanned readmission within 30 days of discharge was measured using an established methodology, which excludes planned readmission such as transplant, cancer treatment, or elective procedures [12]. Surgical revision within 18 months was identified using Current Procedural Terminology (CPT) codes corresponding to the replaced joint, including hip (27134/7/8), knee (27486/7), and shoulder (23473/4). Similarly, surgical site infection within 90 days was identified using CPT codes based on an established methodology [13]. Time to opioid cessation within 18 months postoperatively was assessed for those patients who filled retail pharmacy opioid prescriptions with days’ supply extending into or initiated during the 45 days immediately after surgery. The date of opioid cessation was the last day of an opioid prescription immediately preceding a period of 45 days or longer with no opioid prescription coverage.
Covariates
Patient characteristics and conditions associated with pain, medication use, and health care utilization were measured as potential confounders. Demographic characteristics included age, sex, US region, and type of insurance plan. Preoperative spending was calculated using the amount paid for medical claims by the commercial insurance provider and the patient during 365 until 31 days before the date of admission (Figure 1). Severity of comorbid conditions recorded in the prior 18 months was captured using the Charlson comorbidity index [14,15]. Behavioral health diagnoses received in the past 18 months were separated into three indicators: mood or anxiety disorders, substance use disorder, and personality or trauma and stressor disorders. Current or past tobacco use was assessed using International Classification of Diseases (ICD) or CPT codes for smoking or smoking cessation. Date of surgery and surgical location (hip, knee, or shoulder) were also recorded as covariates. Surgical location and not diagnosis type was included as a covariate, because this is how patients are being grouped from a health systems standpoint, and we are trying to inform those management decisions.
Statistical Analysis
Descriptive statistics were used to describe patient attributes and outcomes, stratified by preoperative opioid use and surgical location. Median and interquartile range (IQR) were calculated for continuous variables, whereas frequency and percentage are given for categorical variables.
Multivariable regression models were fit to estimate the covariate-adjusted association between binary preoperative opioid use and patient outcomes. For length of stay, zero-truncated Poisson regression was used to model the number of days and then summarized using expected values and incidence rate ratios [16]. Medical spending was highly skewed; thus, we used quantile regression to estimate the 50th (or median) and 90th percentiles of spend and the differences across exposure groups [17]. The median and 90th percentile were selected to best represent the expected cost of the average patient and the cost of a relatively high-cost patient. Nonhome discharge and 30-day readmission were modeled using logistic regression. Time to surgical site infection, surgical revision, and opioid cessation were modeled using Cox regression [18]. All models adjusted for the same set of covariates (see Covariates), including age, sex, geographic region, insurance, comorbidity index, date of surgery (number of days since January 1, 2014), surgical location, tobacco use, preoperative medical spend, and behavioral health diagnoses. Age, comorbidity index, preoperative spending, and date of surgery were included as continuous covariates with restricted cubic spline transformation to allow for nonlinear relationships with outcome variables [19].
A second set of models included preoperative morphine equivalent daily dose as a continuous exposure of interest in order to estimate the association of increased preoperative opioid dose; if there was evidence of nonlinearity with the outcome variable (P < 0.05), then dose was modeled using a restricted cubic spline with four knots. Interaction terms were planned for behavioral health conditions and preoperative opioid exposure but were not included in the final analysis to reduce comparisons. R software (version 3.4; http://www.r-project.org/) was used for analysis.
Sensitivity Analysis
Because the comorbidity index may not capture all confounding for disease severity and other unmeasured confounding may exist, we conducted a sensitivity to unmeasured confounding tipping point analysis [20]. Unmeasured confounding tipping point analysis results are given for binary outcomes (those models summarized by odds ratios or hazard ratios). The results are presented from least robust (small effect size needed to tip analysis) to most robust.
Results
Cohort Preoperative Characteristics
From January 1, 2014, through September 30, 2015, we identified 34,792 adults who received elective total joint arthroplasty (38% hip, 58% knee, and 4% shoulder) (Table 1). The study population had a median age (IQR) of 59 (55–62) years, and about half were female (52%). More than half of the study population had a comorbidity index equal to 0, whereas 2% had a severe comorbidity index (Charlson index ≥ 5). Among 8,139 (23.3%) patients who filled any opioid prescription in the 90 days leading to surgery, 6,043 (17.4%) patients met the definition of preoperative opioid use. Among these patients, the median morphine equivalent daily dose in the 90 days leading to arthroplasty (IQR) was 32 (21–50) mg morphine equivalence. History of behavioral health disorders was higher in the preoperative opioid user group for mood or anxiety disorder (34% vs 21%), substance use disorder (8% vs 2%), and personality or trauma and stressor disorder (4% vs 2%). History of tobacco use was also higher for preoperative opioid users (20% vs 11%). Medical utilization, as measured by preoperative spend, was higher by about $2,000 for preoperative opioid users (median = $5651 vs $3497) in the 31–365-day period before surgery. Patients who received shoulder arthroplasty had higher preoperative opioid use compared with hip and knee (23% vs 20% and 15%, respectively) (Table 2). Patients with hip replacement had the highest rate of nonhome discharge (8%).
Table 1.
Descriptive summary of cohort characteristics and outcomes by preoperative opioid use
| Not Preoperative Opioid User (N = 28,749) | Preoperative Opioid User (N = 6,043) | Total (N = 34,792) | |
|---|---|---|---|
| Age, median (IQR), y | 59 (55 to 62) | 58 (53 to 61) | 59 (55 to 62) |
| Female, No. (%) | 14,877 (52) | 3,298 (55) | 18,175 (52) |
| Region, No. (%) | |||
| Missing | 31 (<1) | 4 (<1) | 35 (<1) |
| Midwest | 9,418 (33) | 1,811 (30) | 11,229 (32) |
| Northeast | 6,878 (24) | 1,159 (19) | 8,037 (23) |
| South | 9,985 (35) | 2,633 (44) | 12,618 (36) |
| West | 2,437 (8) | 436 (7) | 2,873 (8) |
| Insurance plan type, No. (%) | |||
| HMO | 2,362 (8) | 422 (7) | 2,784 (8) |
| PPO | 24,356 (85) | 5,300 (88) | 29,656 (85) |
| Other (EPO, PEP, POS, TRD) | 2,031 (7) | 321 (5) | 2,352 (7) |
| Charlson comorbidity index, median (IQR) | 0 (0 to 1) | 0 (0 to 1) | 0 (0 to 1) |
| Severe comorbidity (CCI 5+), No. (%) | 442 (2) | 182 (3) | 624 (2) |
| History of mood or anxiety disorder, No. (%) | 6,028 (21) | 2,074 (34) | 8,102 (23) |
| History of substance use disorder, No. (%) | 693 (2) | 488 (8) | 1,181 (3) |
| History of personality or trauma and stressor disorder, No. (%) | 496 (2) | 237 (4) | 733 (2) |
| Surgical location, No. (%) | |||
| Hip | 10,496 (37) | 2,658 (44) | 13,154 (38) |
| Knee | 17,184 (60) | 3,067 (51) | 20,251 (58) |
| Shoulder | 1,069 (4) | 318 (5) | 1,387 (4) |
| History of tobacco use, No. (%) | 3,199 (11) | 1,221 (20) | 4,420 (13) |
| Preoperative spend, median (IQR), $ | 3,497 (1,595 to 7,782) | 5,651 (2,609 to 12,957) | 3,796 (1,714 to 8,557) |
| Preoperative MEDD, median (IQR), mg | — | 32 (21 to 50) | — |
| Length of stay, median (IQR), d | 3 (3 to 4) | 3 (3 to 4) | 3 (3 to 4) |
| Nonhome discharge, No. (%) | 3,212 (11) | 702 (12) | 3,914 (11) |
| 30-d hospital readmission, No. (%) | 438 (2) | 152 (3) | 590 (2) |
| 90-d surgical site infection, No. (%) | 613 (2) | 211 (3) | 824 (2) |
| 18-mo surgical revision, No. (%) | 544 (2) | 191 (3) | 735 (2) |
| Opioid prescription filled w/in 45 d postsurgery, No. (%) | 26,153 (91) | 5,984 (99) | 32,137 (92) |
| Opioid cessation within 18 mo, No. (%*) | 25,301 (97) | 4,240 (71) | 29,541 (92) |
CCI = Charlson comorbidity index; EPO = exclusive provider organization; HMO = health maintenance organization; IQR = interquartile range; MEDD = morphine equivalent daily dose; PEP = plan exclusive product; POS = point of service; PPO = preferred provider organization; TRD = indemnity/traditional.
The denominator is the number of patients with an opioid prescription filled within 45 days postsurgery.
Table 2.
Descriptive summary of cohort characteristics and outcomes by surgical location
| Hip (N = 13,154) | Knee (N = 20,251) | Shoulder (N = 1,387) | Total (N = 34,792) | |
|---|---|---|---|---|
| Age, median (IQR), y | 58 (53 to 62) | 59 (55 to 62) | 61 (57 to 64) | 59 (55 to 62) |
| Female, No. (%) | 6,059 (46) | 11,566 (57) | 550 (40) | 18,175 (52) |
| Region, No. (%) | ||||
| Missing | 17 (<1) | 18 (<1) | 0 (0) | 35 (<1) |
| Midwest | 4,177 (32) | 6,621 (33) | 431 (31) | 11,229 (32) |
| Northeast | 3,321 (25) | 4,453 (22) | 263 (19) | 8,037 (23) |
| South | 4,542 (35) | 7,500 (37) | 576 (42) | 12,618 (36) |
| West | 1,097 (8) | 1,659 (8) | 117 (8) | 2,873 (8) |
| Insurance plan type, No. (%) | ||||
| HMO | 1,133 (9) | 1,541 (8) | 110 (8) | 2,784 (8) |
| PPO | 11,102 (84) | 17,388 (86) | 1,166 (84) | 29,656 (85) |
| Other (EPO, PEP, POS, TRD) | 919 (7) | 1,322 (7) | 111 (8) | 2,352 (7) |
| Charlson comorbidity index, median (IQR) | 0 (0 to 1) | 0 (0 to 1) | 0 (0 to 1) | 0 (0 to 1) |
| Severe comorbidity (CCI 5+), No. (%) | 245 (2) | 332 (2) | 47 (3) | 624 (2) |
| History of mood or anxiety disorder, No. (%) | 2,817 (21) | 4,887 (24) | 398 (29) | 8,102 (23) |
| History of substance use disorder, No. (%) | 510 (4) | 589 (3) | 82 (6) | 1,181 (3) |
| History of personality or trauma and stressor disorder, No. (%) | 273 (2) | 422 (2) | 38 (3) | 733 (2) |
| History of tobacco use, No. (%) | 1,881 (14) | 2,307 (11) | 232 (17) | 4,420 (13) |
| Preoperative spend, median (IQR), $ | 3,390 (1,477 to 7,679) | 3,977 (1,858 to 8,881) | 4,882 (2,230 to 12,197) | 3,796 (1,714 to 8,557) |
| Preoperative opioid use, No. (%) | 2,658 (20) | 3,067 (15) | 318 (23) | 6,043 (17) |
| Length of stay, median (IQR), d | 3 (3 to 4) | 4 (3 to 4) | 2 (2 to 3) | 3 (3 to 4) |
| Nonhome discharge, No. (%) | 1,057 (8) | 2,812 (14) | 45 (3) | 3,914 (11) |
| 30-d hospital readmission, No. (%) | 235 (2) | 330 (2) | 25 (2) | 290 (2) |
| 90-d surgical site infection, No. (%) | 311 (2) | 484 (2) | 29 (2) | 824 (2) |
| 18-mo surgical revision, No. (%) | 257 (2) | 432 (2) | 46 (3) | 735 (2) |
| Opioid prescription filled w/in 45 d postsurgery, No. (%) | 11,861 (90) | 19,033 (94) | 1,243 (90) | 32,137 (92) |
| Opioid cessation within 18 mo, No. (%*) | 10,931 (92) | 17,545 (92) | 1,065 (86) | 29,541 (92) |
CCI = Charlson comorbidity index; EPO = exclusive provider organization; HMO = health maintenance organization; IQR = interquartile range; MEDD = morphine equivalent daily dose; PEP = plan exclusive product; POS = point of service; PPO = preferred provider organization; TRD = indemnity/traditional.
The denominator is the number of patients with an opioid prescription filled within 45 days postsurgery.
Length of Stay
We found evidence that length of stay was longer for patients who were preoperative users of opioids (incidence rate ratio [IRR] = 1.03, 95% confidence interval [CI] = 1.02 to 1.05, P < 0.001) (Table 3) compared with those who were not after covariate adjustment (Table 3). The expected length of stay for an average individual with preoperative opioid use was 3.98 days, compared with 3.87 days among those without preoperative opioid use. When opioid dose was considered, the expected length of stay consistently increased as dose increased. Although the magnitude of increase in length of stay was not particularly large with increasing amount of preoperative opioid dose, there was a statistically significant dose–response trend with increasing preoperative opioid use (P < 0.001) (Table 4).
Table 3.
Covariate-adjusted results for all end points by preoperative opioid use (binary): Estimate (95% CI)
| Not Preoperative Opioid User* (N = 28749) | Preoperative Opioid User* (N = 6043) | Comparison | P Value | |
|---|---|---|---|---|
| Length of stay, d | 3.87 (3.82 to 3.91) | 3.98 (3.92 to 4.06) | IRR = 1.03 (1.02 to 1.05) | <0.001 |
| In-hospital spend, median, $ | 20,511 (20,022 to 20,999) | 19,848 (19,247 to 20,450) | Diff = –662 (–1,067 to –257) | 0.001 |
| In-hospital spend, 90th percentile, $ | 42,866 (41,958 to 43,773) | 42,478 (41,301 to 43,654) | Diff = –388 (–1,253 to 476) | 0.379 |
| 90-d postoperative spend, median, $ | 3,271 (3,199 to 3,342) | 3,344 (3,245 to 3,442) | Diff = 73 (–6 to 151) | 0.068 |
| 90-d postoperative spend, 90th percentile, $ | 7,841 (7,394 to 8,288) | 8,817 (8,126 to 9,509) | Diff = 976 (384 to 1,568) | 0.001 |
| 180-d postoperative spend, median, $ | 4,218 (4,105 to 4,332) | 4,521 (4,364 to 4,677) | Diff = 302 (178 to 427) | <0.001 |
| 180-d postoperative spend, 90th percentile, $ | 13,049 (11,551 to 14,548) | 17,697 (15,243 to 20,150) | Diff = 4,647 (2,541 to 6,753) | <0.001 |
| 365-d postoperative spend, median, $ | 6,245 (6,051 to 6,439) | 7,209 (6,911 to 7,507) | Diff = 964 (715 to 1,214) | <0.001 |
| 365-d postoperative spend, 90th percentile, $ | 27,195 (25,349 to 29,041) | 32,243 (29,790 to 34,696) | Diff = 5,048 (3,170 to 6,925) | <0.001 |
| Nonhome discharge, % | 10.1 (9.3 to 11.1) | 11.0 (9.9 to 12.3) | OR = 1.10 (1.00 to 1.21) | 0.048 |
| 30-d readmission, % | 1.0 (0.8 to 1.2) | 1.4 (1.0 to 1.8) | OR = 1.43 (1.17 to 1.74) | <0.001 |
| 90-d surgical site infection, % | 1.3 (1.0 to 1.6) | 1.8 (1.3 to 2.2) | HR = 1.35 (1.14 to 1.59) | <0.001 |
| 18-mo surgical revision, % | 1.6 (1.3 to 2.0) | 2.2 (1.7 to 2.8) | HR = 1.36 (1.15 to 1.62) | <0.001 |
| 18-mo opioid cessation, % | 95.1 (94.6 to 95.6) | 64.2 (62.6 to 65.7) | HR = 0.34 (0.33 to 0.35) | <0.001 |
Estimates are presented along with 95% confidence intervals in parenthesis. HR = hazard ratio; IRR = incidence rate ratio; OR = odds ratio.
Expected values were adjusted to the median or most prevalent values of covariates, including age 59 years, female, Southern region, PPO insurance, Charlson comorbidity index = 0, November 2014, knee, no tobacco use, $3,796 preoperative spend, and no behavioral health condition.
Table 4.
Covariate-adjusted results for all end points by preoperative opioid use (continuous): Estimate (95% CI)
| MEDD = 0* | MEDD = 20* | MEDD = 50* | MEDD = 100* | Comparison (50 vs 0) | P Value† | |
|---|---|---|---|---|---|---|
| Length of stay, d | 3.88 (3.83 to 3.92) | 3.90 (3.86 to 3.95) | 3.94 (3.89 to 3.99) | 4.00 (3.93 to 4.07) | IRR = 1.02 (1.01 to 1.03) | <0.001 |
| In-hospital spend, median, $ | 20,503 (20,014 to 20,991) | 19,735 (18,995 to 20,475) | 19,702 (19,007 to 20,397) | 19,822 (18,877 to 20,767) | Diff = –801 (–1,333 to –269) | 0.005 |
| In-hospital spend, 90th percentile, $ | 42,915 (42,064 to 43,767) | 41,957 (40,783 to 43,131) | 42,540 (41,215 to 43,865) | 43,069 (41,186 to 44,952) | Diff = –375 (–1,458 to 707) | 0.104 |
| 90-d postoperative spend, median, $ | 3,268 (3,197 to 3,339) | 3,297 (3,222 to 3,371) | 3,340 (3,243 to 3,437) | 3,413 (3,257 to 3,568) | Diff = 72 (0 to 145) | 0.050 |
| 90-d postoperative spend, 90th percentile, $ | 7,866 (7,402 to 8,330) | 8,086 (7,570 to 8,602) | 8,415 (7,613 to 9,218) | 8,964 (7,525 to 10,404) | Diff = 549 (–158 to 1,257) | 0.128 |
| 180-d postoperative spend, median, $ | 4,231 (4,116 to 4,345) | 4,361 (4,165 to 4,556) | 4,586 (4,359 to 4,812) | 4,879 (4,521 to 5,236) | Diff = 355 (151 to 559) | <0.001 |
| 180-d postoperative spend, 90th percentile, $ | 12,918 (11,412 to 14,423) | 16,269 (13,368 to 19,171) | 18,442 (15,286 to 21,598) | 20,862 (16,118 to 25,605) | Diff = 5,525 (2,653 to 8,396) | <0.001 |
| 365-d postoperative spend, median, $ | 6,251 (6,054 to 6,448) | 6,666 (6,312 to 7,020) | 7,632 (7,163 to 8,100) | 8,529 (7,776 to 9,282) | Diff = 1,381 (945 to 1,816) | <0.001 |
| 365-d postoperative spend, 90th percentile, $ | 27,380 (25,519 to 29,240) | 29,607 (26,487 to 32,727) | 33,312 (30,231 to 36,393) | 37,404 (32,882 to 41,927) | Diff = 5,932 (3,314 to 8,550) | <0.001 |
| Nonhome discharge, % | 10.2 (9.4 to 11.1) | 10.5 (9.6 to 11.4) | 10.9 (9.9 to 11.9) | 11.6 (10.4 to 12.9) | OR = 1.07 (1.03 to 1.12) | 0.001 |
| 30-d readmission, % | 1.0 (0.8 to 1.2) | 1.2 (0.9 to 1.5) | 1.4 (1.0 to 1.9) | 1.6 (1.2 to 2.2) | OR = 1.45 (1.14 to 1.85) | <0.001 |
| 90-d surgical site infection, % | 1.3 (1.1 to 1.6) | 1.4 (1.0 to 1.8) | 1.9 (1.4 to 2.4) | 2.5 (1.7 to 3.3) | HR = 1.46 (1.21 to 1.76) | <0.001 |
| 18-mo surgical revision, % | 1.6 (1.3 to 2.0) | 1.9 (1.4 to 2.5) | 2.4 (1.8 to 3.0) | 2.8 (1.8 to 3.8) | HR = 1.46 (1.20 to 1.78) | <0.001 |
| 18-mo opioid cessation, % | 95.4 (94.9 to 95.9) | 74.7 (72.8 to 76.4) | 59.0 (56.9 to 61.0) | 45.9 (43.1 to 48.5) | HR = 0.29 (0.28 to 0.30) | <0.001 |
Estimates are presented along with 95% confidence intervals in parenthesis. HR = hazard ratio; IRR = incidence rate ratio; MEDD = morphine equivalent daily dose; OR = odds ratio.
Expected values were adjusted to the median or most prevalent values of covariates, including age 59 years, female, Southern region, PPO insurance, Charlson comorbidity index = 0, November 2014, knee, no tobacco use, $3,796 preoperative spend, and no behavioral health condition.
Wald test for overall association of preoperative opioid dose with outcome (including nonlinear terms when applicable).
Medical Spending
We also found evidence that the median in-hospital spending was about $600 lower for patients who were not preoperative opioid users (95% CI = –$1,067 to –$257) (Table 3). Although there was evidence of an association, opioid dose did not appear to have a strictly increasing or decreasing association with median in-hospital spend. There was little evidence that preoperative opioid use or dose was associated with the costliest patients in the 90th percentile (P = 0.068 and P = 0.104, respectively). With the exception of 90-day median postoperative spend, there were significantly higher costs associated with preoperative opioid use, with differences ranging from $302 to $5,048 (Table 3). There was a dose–response effect between opioid dose and postoperative spend, with expected differences as high as $6,000 (Table 4).
Postsurgical Outcomes
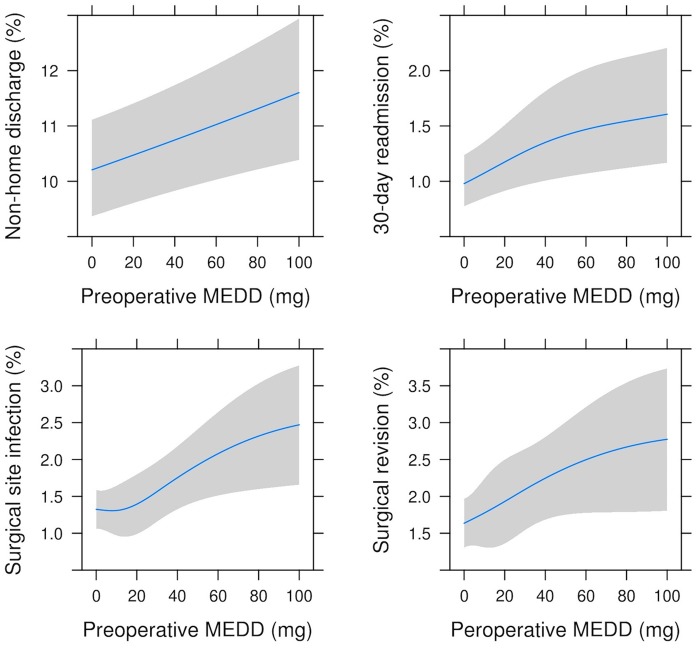
Preoperative opioid users had 10% higher odds of nonhome discharge (odds ratio [OR] = 1.10, 95% CI = 1.00 to 1.21, P = 0.048) (Table 3). The average individual on high-dose opioids (100 mg) had a nonhome discharge rate of 11.6% compared with 10.2% among those without opioid use (P = 0.001) (Table 4, Figure 2). This difference in rates is equivalent to an increase of 14 per 1,000 individuals who are discharged to extended care facilities.
Figure 2.
Covariate-adjusted association of preoperative opioid dose with postsurgical outcomes. Increasing preoperative morphine equivalent daily dose (MEDD) has a dose–response effect with costly or adverse patient outcomes. Although 7.6% of preoperative opioid users had a MEDD in excess of 100 mg (1.3% overall), graphics are limited in range to 0–100 mg.
Preoperative opioid users had 43% higher odds of readmission within 30 days (OR = 1.43, 95% CI = 1.17 to 1.74, P < 0.001) (Table 3). The average individual on high-dose opioids (100 mg) had a 30-day readmission rate of 1.6%, compared with 1.0% among those without opioid use (P < 0.001) (Table 4, Figure 2). This difference in rates is equivalent to an increase of six per 1,000 individuals with an unplanned readmission to the hospital within 30 days after arthroplasty.
Surgical site infection rates were 35% higher for preoperative opioid users (hazard ratio [HR] = 1.35, 95% CI = 1.14 to 1.59) (Table 3) in the 90 days after surgery. Risk of surgical revision in the 18 months after surgery was 36% higher among preoperative opioid users (HR = 1.36, 95% CI = 1.15 to 1.62) (Table 3). Surgical site infection risk and surgical revision risk both increased as opioid doses increased (HR = 1.46, 95% CI = 1.21 to 1.76, and HR = 1.46, 95% CI = 1.20 to 1.78, respectively) (Table 4, Figure 2).
Sensitivity analysis for these outcomes conservatively considered a situation where an unmeasured confounder was prevalent in 15% of the exposed population and 0% of the unexposed to determine the minimum effect size required to lose statistical significance (Table 5). The results for nonhome discharge were least robust in situations where such unmeasured confounding may have occurred. For the association between binary preoperative opioid use and 90-day surgical site infection, a binary unmeasured confounder had to have an association with the outcome equal to an odds ratio of 1.95 or greater in order to render the observed association nonsignificant.
Table 5.
Unmeasured confounding tipping point analysis: p0 = 0, p1 = 0.15
| Outcome | Preoperative Opioid Use | Observed 95% CI | Tipping Point Effect Size |
|---|---|---|---|
| Nonhome discharge | Binary | (1.00 to 1.21) | 1.01 |
| Nonhome discharge | Continuous* | (1.03 to 1.12) | 1.20 |
| 90-d surgical site infection | Binary | (1.14 to 1.59) | 1.95 |
| 30-d hospital readmission | Continuous | (1.14 to 1.85) | 1.96 |
| 18-mo surgical revision | Binary | (1.15 to 1.62) | 1.97 |
| 30-d hospital readmission | Binary | (1.17 to 1.74) | 2.16 |
| 90-d surgical site infection | Continuous | (1.20 to 1.78) | 2.31 |
| 18-mo surgical revision | Continuous | (1.21 to 1.76) | 2.41 |
| 18-mo opioid cessation | Binary | (0.33 to 0.35) | Unlimited |
| 18-mo opioid cessation | Continuous | (0.28 to 0.30) | Unlimited |
CI = confidence interval.
The observed confidence interval for continuous preoperative opioid use exposure corresponds to 50 morphine equivalent daily dose vs none (Table 4, column 4).
Opioid Cessation
Among all patients with surgery, 92% filled an opioid prescription in the 45 days postsurgery, including 99% among preoperative opioid users and 91% among those without preoperative opioid use (Table 1). An average patient with preoperative opioid use had an 18-month opioid cessation rate of 64%, compared with 95% for a patient without preoperative opioid use. There was a 66% lower rate of quitting opioids in the 18 months after surgery among preoperative opioid users (HR = 0.34, 95% CI = 0.33 to 0.35) (Table 3). For opioid doses of 0, 20, 50, and 100 mg, the rates of opioid cessation were 95%, 75%, 59%, and 46%, respectively (P < 0.001) (Table 4). These results were robust to consideration for unmeasured confounding (Table 5).
Discussion
In this analysis of nearly 35,000 patients undergoing orthopedic surgeries, including total hip, knee, and shoulder arthroplasty, we found several statistically significant risks for worsened perioperative outcomes and higher costs between patients using opioids preoperatively as compared with those who were not using opioids before surgery. The association for most of the outcomes demonstrated a dose–response relationship with higher doses of preoperative opioids leading to higher costs and worse outcomes.
At preoperative baseline, patients using opioids before elective arthroplasty were more likely to have comorbid psychiatric disorders and to have incurred high costs in the year before surgery. Irrespective of surgery type, patients using opioids preoperatively were more likely to incur greater postoperative costs persisting through one year postoperatively. Although in-hospital spending between preoperative opioid users and nonusers did not differ, we are led to suspect that the effects of preoperative opioid use on surgical outcomes are more likely to manifest in the postoperative period, because these patients were more frequently discharged to a location other than their preoperative home of record. During the postoperative period, preoperative opioid users were more likely to be readmitted within 30 days postoperatively, experience a surgical site infection at 90 days postoperatively, and undergo surgical revision within 18 months of their operation. They were also substantially less likely to discontinue opioid use at 18 months after their procedure when compared with those patients who were not using opioids preoperatively.
Many prior studies in this area have been limited by the use of study designs that cannot determine population prevalence [8,9,11]. In smaller cohort studies of preoperative opioid use among patients undergoing elective knee, hip, and shoulder arthroplasty, the prevalence of preoperative opioid use has been reported variably as 34%, 39%, and 52% [10,21,22]. Kim et al. reported the preoperative prevalence of opioid use among patients in a large commercially insured population undergoing knee or hip arthroplasty as 17.6% when considering patients using opioids for at least four months before surgery [7]. By contrast, a cohort study conducted by Ben-Ari et al. in the Veterans Administration reported that the preoperative prevalence of opioid use was 39.1% in a similar arthroplasty population [22]. One explanation for this difference may be related to their source cohorts, and this is further strengthened by the similarity of our preoperative prevalence to that of Kim et al., who also examined a commercially insured cohort. Those authors defined persistent preoperative opioid use as a prescription filled within each of the four months before surgery, whereas we defined preoperative opioid use as at least one opioid prescription fill occurring within each of 1–30 days and 31–90 days before the date of admission. We note the very similar preoperative opioid use in these independent cohorts (17.4% vs 17.6%), using similar case definitions.
In-hospital and postoperative outcomes among patients using opioids preoperatively appeared to be almost uniformly worse in our study cohort, as compared with patients who were not preoperative users of opioids. These findings were largely consistent with previous reports in the literature. In a study of 32,636 patients in the Veterans Administration (VA) system examining long-term outcomes for total knee arthroplasty, patients were followed for one year postoperatively. Patients who used opioids for more than three months before surgery were found to have a higher rate of surgical revision at one year [22]. Smaller studies have similarly suggested that patients using opioids preoperatively experience delayed discharge, revision surgery for recalcitrant pain, lower mean Knee Society scores at the time of follow-up at three years, increased likelihood of discharge to a care facility, and lower success with physical therapy sessions following knee arthroplasty [8,23,24]. Among patients undergoing total hip arthroplasty, several series have concluded that daily opioid use is associated with longer hospital stay, lower likelihood of weaning off opioids postoperatively, and lower Harris hip scores at a mean follow-up of 58 months [9,21]. Patients undergoing shoulder arthroplasty (either anatomic or reverse) who use opioids preoperatively appear to have higher perioperative opioid consumption and pain scores and poorer long-term outcomes, though there does not appear to be a strong indication of higher rates of surgical revision or readmission rates [10,11]. The mechanisms for these differences in function remain somewhat speculative but may be related to weight-bearing joints—that is, hip and knee—undergoing earlier mobilization, which prevents major muscle group atrophy that would otherwise persist into the postoperative period [25,26].
Many biochemical and cellular mechanisms have been proposed for these observed effects, and based on these insights from primary research, there have been thorough reviews of the rationale for preoperative opioid weaning [27]. Some of the adverse outcomes observed in the present study—increased length of stay, nonhome discharge, in-hospital spending, increased readmission rates, and higher surgical revision rates—may be mediated by ineffective pain control [23]. This may be related to opioid-induced hyperalgesia, which involves development of tolerance to these agents and complex remodeling of endogenous pathways, including increased NMDA receptor activation, which may develop even with short courses of opioids preoperatively [28–30]. Other outcomes presented in our study, such as surgical infection and perhaps surgical revision rate and readmission, may be related to opioid-induced immunosuppression [31,32]. Furthermore, opioid-sparing anesthetic techniques have been associated with reduced immunosuppression in general surgery populations, and other mechanisms including opioid modification of neutrophil chemotaxis and T-cell expression have been reviewed elsewhere [31,33,34].
The finding of a dose response between preoperative opioid consumption and adverse outcomes following surgery has been suggested in previous studies. In a series of 583 patients undergoing spine surgery, Lee et al. found that preoperative opioid consumption was correlated with poor postoperative outcomes. In fact, each 10-mg increase in daily morphine equivalents was associated with linearly worse outcomes measured by several patient-reported health indices, including the Short Form Health Survey, EuroQol-5D, and Oswestry Disability Index, up to 12 months postoperatively [35]. These data support the findings of the present study, as we observed a statistically significant increase in postoperative spending up to one year, rate of nonhome discharge, 30-day readmission rate, 18-month surgical revision rate, and continued opioid use at 18 months tracking with increasing preoperative opioid dose.
Given the adverse effects associated with preoperative opioid use and our findings of frequent persistent postoperative use, there is an important role for reducing the use of these medications in the perioperative period. Nguyen et al. found that among patients undergoing either total knee or hip arthroplasty, successful opioid weaning was associated with several improved health outcomes, including patient-reported health outcome measures and activity scores [36]. This strategy has also been used extensively for patients on high doses of opioids undergoing implantation of intrathecal opioid pumps [37]. Given that the demand for primary hip and knee arthroplasties is projected to continue increasing, the matter of optimizing perioperative outcomes takes on growing economic importance [38]. Although our study found that patients using the highest doses of opioids generated up to $5,048 of increased costs at one year postoperation, other studies in general surgery populations have estimated up to $13,000 in increased postoperative spending at one year after surgery [39].
As health care payment models continue to shift toward accountable care organizations bearing the risk for patient outcomes and/or bundled payments for medical services, factors that directly affect costs will continue to grow in importance. Cost prediction is already highly relevant to health plans and the health systems that bear this risk, thus highlighting the need to proactively employ administrative data to describe the magnitude of costs created by patient-specific risk factors, such as preoperative opioid use.
Our study is subject to limitations imposed by its retrospective cohort design using administrative data. Although this is a commercially insured population, we were not able to obtain measures of socioeconomic status from the current database and therefore are unable to determine whether this covariate may have been relevant to our study end points. There is also the possibility that preoperative opioid use is a marker for worse preoperative joint condition or some other factor that would predispose these patients to worse outcomes, thus confounding our results. We attempted to overcome these limitations by use of sensitivity analysis methods and believe that our results are robust despite the lack of possible unmeasured covariates. For outcomes in which a single numerical increase was clinically significant (e.g., length of stay), we were limited by whole-day discharge changes. Also, opioid use was abstracted from prescription and pharmacy data, which assumes that patients are physically taking their prescribed daily morphine equivalent rather than filling these prescriptions as a “just in case” measure.
Other issues with data attribution errors may have occurred as well, for instance, coding elective procedures correctly, coding procedure types accurately, or coding other comorbidities (e.g., depression) accurately and in a way that is abstracted by the database. For example, some physicians may be reluctant to record in a medical record some comorbid conditions such as substance use disorder.
Conclusions
In this large, retrospective cohort study of nearly 35,000 patients covered by a multistate commercial health insurance plan, we describe the effects of preoperative opioid use on adverse outcomes, medical spending, and persistent opioid use following elective total joint arthroplasty in the United States. We present data that demonstrate a significant association between preoperative opioid use and both increased health care costs and adverse perioperative surgical outcomes. This study also presents a proof of concept for how continuously collected administrative data can be used to stratify patient risk and predict perioperative outcomes.
Funding sources: The study was funded by axialHealthcare, a health data analytics company.
Conflicts of interest: All authors work for or received paid compensation from axialHealthcare through this study: MBP and EAS (paid employment), HLW (paid internship), AJBP (paid consultancy), RJY (chair of the Scientific Advisory Board).
References
- 1. Levy B, Paulozzi L, Mack KA, Jones CM.. Trends in opioid analgesic-prescribing rates by specialty, U.S., 2007-2012. Am J Prev Med 2015;49(3):409–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Kirson NY, Shei A, Rice JB, et al. The burden of undiagnosed opioid abuse among commercially insured individuals. Pain Med 2015;16(7):1325–32. [DOI] [PubMed] [Google Scholar]
- 3. Florence CS, Zhou C, Luo F, Xu L.. The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Med Care 2016;54(10):901–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Jones CM, Mack KA, Paulozzi LJ.. Pharmaceutical overdose deaths, United States, 2010. JAMA 2013;309(7):657–659. [DOI] [PubMed] [Google Scholar]
- 5. Wright EA, Katz JN, Abrams S, Solomon DH, Losina E.. Trends in prescription of opioids from 2003-2009 in persons with knee osteoarthritis. Arthritis Care Res (Hoboken) 2014;66(10):1489–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Dominick KL, Bosworth HB, Dudley TK, et al. Patterns of opioid analgesic prescription among patients with osteoarthritis. J Pain Palliat Care Pharmacother 2004;18(1):31–46. [PubMed] [Google Scholar]
- 7. Kim SC, Choudhry N, Franklin JM, et al. Patterns and predictors of persistent opioid use following hip or knee arthroplasty. Osteoarthr Cartil 2017;25(9):1399–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zywiel MG, Stroh DA, Lee SY, Bonutti PM, Mont MA.. Chronic opioid use prior to total knee arthroplasty. J Bone Jt Surgery-American 2011;93(21):1988–93. [DOI] [PubMed] [Google Scholar]
- 9. Pivec R, Issa K, Naziri Q, et al. Opioid use prior to total hip arthroplasty leads to worse clinical outcomes. Int Orthop 2014;38(6):1159–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cheah JW, Sing DC, McLaughlin D, et al. The perioperative effects of chronic preoperative opioid use on shoulder arthroplasty outcomes. J Shoulder Elb Surg 2017;26(11):1908–14. [DOI] [PubMed] [Google Scholar]
- 11. Morris BJ, Laughlin MS, Elkousy HA, Gartsman GM, Edwards TB.. Preoperative opioid use and outcomes after reverse shoulder arthroplasty. J Shoulder Elb Surg 2015;24(1):11–6. [DOI] [PubMed] [Google Scholar]
- 12. Horwitz LI, Grady JN, Dorsey KB, et al. 2014. Measure Updates and Specifications Report Hospital-Wide All-Cause Unplanned Readmission. Version 3.0. New Haven, CT: Yale New Haven Health Services Corporation/Center for Outcomes Research & Evalutation; 2014. Available at: https://altarum.org/sites/default/files/uploaded-publication-files/Rdmsn_Msr_Updts_HWR_0714_0.pdf (accessed March 17, 2018).
- 13. Simoes J, Grady JN, DeBuhr J, Silverberg A, Suter LG KJ.. 2017. Procedure-Specific Measure Updates and Specifications Report Hospital-Level Risk-Standardized Complication Measure: Elective Primary Total Hip Arthroplasty (THA) and/or Total Knee Arthroplasty (TKA). Version 6.0. 2017. New Haven, CT: Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation; 2017.
- 14. Charlson ME, Pompei P, Ales KL, MacKenzie CR.. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J Chronic Dis 1987;40(5):373–83. [DOI] [PubMed] [Google Scholar]
- 15. Charlson M, Szatrowski TP, Peterson J, Gold J.. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47(11):1245–51. [DOI] [PubMed] [Google Scholar]
- 16. Yee TW. Vector Generalized Linear and Additive Models: With an Implementation in R - Thomas W. New York: Yee - Google Books; 2015. Available at: https://books.google.com/books? hl=en&lr=&id=E5GKCgAAQBAJ&oi=fnd&pg=PR7&dq=Yee,+T.+W.+(2015)+Vector+Generalized+Linear+and+Additive+Models:+With+an+Implementation+in+R.+New+York,+USA:+Springer&ots=xINrR5WbaT&sig=UaMiYbtFsDy7PErBT_1vW63NZkA#v=onepage&q=Yee%25 (accessed March 17, 2018). [Google Scholar]
- 17. Koenker RW. Quantile Regression. Cambridge, UK: Cambridge University Press; 2005. [Google Scholar]
- 18. Therneau T, Grambusch P. Modeling Survival Data: Extending the Cox Model. New York: Springer-Verlag; 2000.
- 19. Harrell FE. Regression Modeling Strategies: With Applications to Linear Models, Logistic and Ordinal Regression, and Survival Analysis. New York: Springer; 2015.
- 20. Lin DY, Psaty BM, Kronmal RA.. Assessing the sensitivity of regression results to unmeasured confounders in observational studies. Biometrics 1998;54(3):948–963. [PubMed] [Google Scholar]
- 21. Rozell JC, Courtney PM, Dattilo JR, Wu CH, Lee G-C.. Preoperative opiate use independently predicts narcotic consumption and complications after total joint arthroplasty. J Arthroplasty 2017;32(9):2658–62. [DOI] [PubMed] [Google Scholar]
- 22. Ben-Ari A, Chansky H, Rozet I.. Preoperative opioid use is associated with early revision after total knee arthroplasty. J Bone Jt Surg 2017;99(1):1–9. [DOI] [PubMed] [Google Scholar]
- 23. Sing DC, Barry JJ, Cheah JW, Vail TP, Hansen EN.. Long-acting opioid use independently predicts perioperative complication in total joint arthroplasty. J Arthroplasty 2016;31(9):170–4.e1. [DOI] [PubMed] [Google Scholar]
- 24. Menendez ME, Ring D, Bateman BT.. Preoperative opioid misuse is associated with increased morbidity and mortality after elective orthopaedic surgery. Clin Orthop Relat Res 2015;473(7):2402–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bade MJ, Stevens-Lapsley JE.. Early high-intensity rehabilitation following total knee arthroplasty improves outcomes. J Orthop Sport Phys Ther 2011;41(12):932–41. [DOI] [PubMed] [Google Scholar]
- 26. Payne C, Jaggi A, Le Leu A, Garofalo R, Conti M.. Rehabilitation for shoulder arthroplasty. Orthop Trauma 2015;29(5):313–23. [Google Scholar]
- 27. McAnally H. Rationale for and approach to preoperative opioid weaning: A preoperative optimization protocol. Perioper Med 2017;6(1):19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chang G, Chen L, Mao J.. Opioid tolerance and hyperalgesia. Med Clin North Am 2007;91(2):199–211. [DOI] [PubMed] [Google Scholar]
- 29. Angst MS, Clark DJ.. Opioid-induced a qualitative systematic review. Anesthesiol J Am Soc Anesthesiol 2006;104(3):570–87. [DOI] [PubMed] [Google Scholar]
- 30. Hina N, Fletcher D, Poindessous-Jazat F, Martinez V.. Hyperalgesia induced by low-dose opioid treatment before orthopaedic surgery. Eur J Anaesthesiol 2015;32(4):255–61. [DOI] [PubMed] [Google Scholar]
- 31. Ramaswamy S, Langford R.. Antinociceptive and immunosuppressive effect of opioids in an acute postoperative setting: An evidence-based review. BJA Educ 2017;17(3):105–10. [Google Scholar]
- 32. Vallejo R, de Leon-Casasola O, Benyamin R.. Opioid therapy and immunosuppression. Am J Ther 2004;11(5):354–65. [DOI] [PubMed] [Google Scholar]
- 33. Long X, Li Y, Qiu S, et al. MiR-582-5p/miR-590-5p targeted CREB1/CREB5–NF-κB signaling and caused opioid-induced immunosuppression in human monocytes. Transl Psychiatry 2016;6(3):e757.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chen W-K, Ren L, Wei Y, et al. General anesthesia combined with epidural anesthesia ameliorates the effect of fast-track surgery by mitigating immunosuppression and facilitating intestinal functional recovery in colon cancer patients. Int J Colorectal Dis 2015;30(4):475–81. [DOI] [PubMed] [Google Scholar]
- 35. Lee D, Armaghani S, Archer KR, et al. Preoperative opioid use as a predictor of adverse postoperative self-reported outcomes in patients undergoing spine surgery. J Bone Jt Surg Am 2014;96(11):e89. [DOI] [PubMed] [Google Scholar]
- 36. Nguyen L-CL, Sing DC, Bozic KJ.. Preoperative reduction of opioid use before total joint arthroplasty. J Arthroplasty 2016;31(9):282–7. [DOI] [PubMed] [Google Scholar]
- 37. Grider JS, Harned ME, Etscheidt MA.. Patient selection and outcomes using a low-dose intrathecal opioid trialing method for chronic nonmalignant pain. Pain Physician 2011;14(4):343–51. Available at: http://www.painphysicianjournal.com/current/pdf? article=MTQ4Ng%3D%3D&journal=62 (accessed April 11, 2018). [PubMed] [Google Scholar]
- 38. Kurtz S. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Jt Surg 2007;89(4):780–5. [DOI] [PubMed] [Google Scholar]
- 39. Waljee JF, Cron DC, Steiger RM, et al. Effect of preoperative opioid exposure on healthcare utilization and expenditures following elective abdominal surgery. Ann Surg 2017;265(4):715–21. [DOI] [PMC free article] [PubMed] [Google Scholar]