Abstract
Objective
Programmed death-1 (PD-1) and its ligand PD-L1 are now used as predictive biomarkers to guide clinical decisions. Precise characterization of PD-L1-positive cells may contribute to our knowledge of which patients derive benefit from the PD-L1 blockade therapy.
Results
To address this issue, we performed immunophenotyping of PD-L1-positive cells in Hodgkin lymphoma and in angioimmunoblastic T cell lymphoma (AITL) employing multiple immunofluorescent immunolabeling. We found that PD-L1-positive cells and PD-1-positive cells both in Hodgkin lymphoma and in AITL belong to two completely different cell lineages. In both lymphomas, PD-1 was found exclusively in T-lymphocytes, whereas PD-L1 was revealed in the tumor microenvironment cells including macrophages. PD-L1 was also detected in CD30-positive cells in Hodgkin lymphoma but not in AITL. The marker of B-cell lineage, CD20, was not detectable in PD-L1-positive cells both in AITL and in Hodgkin. Our study highlights the importance of comprehensive assessment of PD-1/PD-L1 regulatory pathways for employing PD-L1 as a predictive biomarker in clinical practice. PD-L1-antibody therapy is proven in Hodgkin lymphoma. Comparative immunophenotyping of the PD-1/PD-L1 axis provides a support for attempts to prove this principle also for AITL.
Keywords: Angioimmunoblastic T-cell lymphoma, Hodgkin lymphoma, Receptor PD-1, Ligand PD-L1
Introduction
In 1992 the team of Tasuku Honjo in a screen for genes, involved in apoptosis, discovered a protein expressed on the surface of a subset of immune cells known as T cells and named this protein PD-1 (short for Programmed death-1) [1]. PD-1 is expressed predominantly on activated T cells [2]. In 1999, a ubiquitous antiapoptotic receptor on cancer cells was reported from the Mayo Clinic [3]. Originally it was named B7-H1 but later renamed PD-L1, because it was identified as a ligand of PD-1. The binding of PD-1 to its ligand PD-L1 induces apoptosis or exhaustion in activated T cells thus preventing the immune system from killing cancer cells [4, 5]. PD-L1 is not present in large quantity in normal tissue, but it is upregulated in a variety of tumors [6, 7]. Upregulation of PD-L1 allows cancers to evade the host immune system [8, 9]. Development of therapeutic anti-PD-1/PD-L1 monoclonal antibodies leading to the reactivation of specific antitumor immune response has emerged as a promising strategy for hematological malignancy therapy including various lymphoma arts [10–16]. PD-1/PD-L1 immune-checkpoint blockade therapies reactivate the specific antitumor immune response [17–22]. However, to predict patients who are likely to respond to treatment with PD-1/PD-L1 blockers still remains a challenge [23].
Precise characterization of PD-L1-positive cells may contribute to our knowledge of which patients derive benefit from the PD-L1 blockade therapy [24, 25]. This study was aimed at the immunophenotyping of the PD-1/PD-L1 axis in Hodgkin lymphoma and in AITL. For immunofluorescent multiple immunolabeling we used antibodies to PD-L1, PD-1 and a panel of CD antibodies raised against diverse cell types.
Main text
Methods
Patients
15 AITL and 8 Hodgkin patients were included in this study. Informed consent was obtained from all subjects. The samples were retrieved from the files of the Institute for Hematopathology, Hamburg, Germany. Histological diagnoses were established according to the WHO classification [26, 27]. This study was conducted in accordance with the “Ethical Principles for Medical Research Involving Human Subjects” and approved by the Institutional Review Board of the Institute for Hematopathology, Hamburg, Germany.
Tissue probe stainings
Tissue probes were fixed in buffered 4% formaldehyde and routinely embedded in paraffin. Deparaffinized and rehydrated sections (1 µm thick) were subjected to antigen retrieval by heating in a steamer with sodium citrate buffer, pH 6.0, at 95 °C × 30 min. Blocking the endogenous Fc receptors prior to incubation with primary antibodies was omitted [28]. After antigen retrieval, sections were immunoreacted with primary antibodies (Additional file 1: Table S1). Bound primary antibodies were visualized using secondary antibodies listed in the Additional file 2: Table S2. Principally, immunohistochemical staining was performed according to the standard protocols described earlier [29–31].
Controls
Control incubations were: omission of primary antibodies or substitution of primary antibodies by the same IgG species (Dianova, Hamburg, Germany) at the same final concentration as the primary antibodies. The exclusion of either the primary or the secondary antibody from the immunohistochemical reaction, substitution of primary antibodies with the corresponding IgG at the same final concentration resulted in lack of immunostaining.
Results
Employing multiple immunofluorescent labeling of cellular components in tissue sections of the human AITL and Hodgkin lymphoma, we found that PD-1 and PD-L1 are localized in different cells (Fig. 1a; Additional file 3: Fig. S1). CD3, marker of T-cell lineage, was co-localized with PD-1 (Fig. 1b) and never with PD-L1. Triple immunofluorescent labelling for PD-1, PD-L1 and CD68 in tissues both of Hodgkin lymphoma and AITL (Fig. 2) revealed that CD68, marker for macrophage lineage, including monocytes and histiocytes, was solely and exclusively expressed in PD-L1+ cells and never in PD-1+ cells. This indicates that PD-1+ and PD-L1+ cells belong to completely different cell lineages.
Fig. 1.
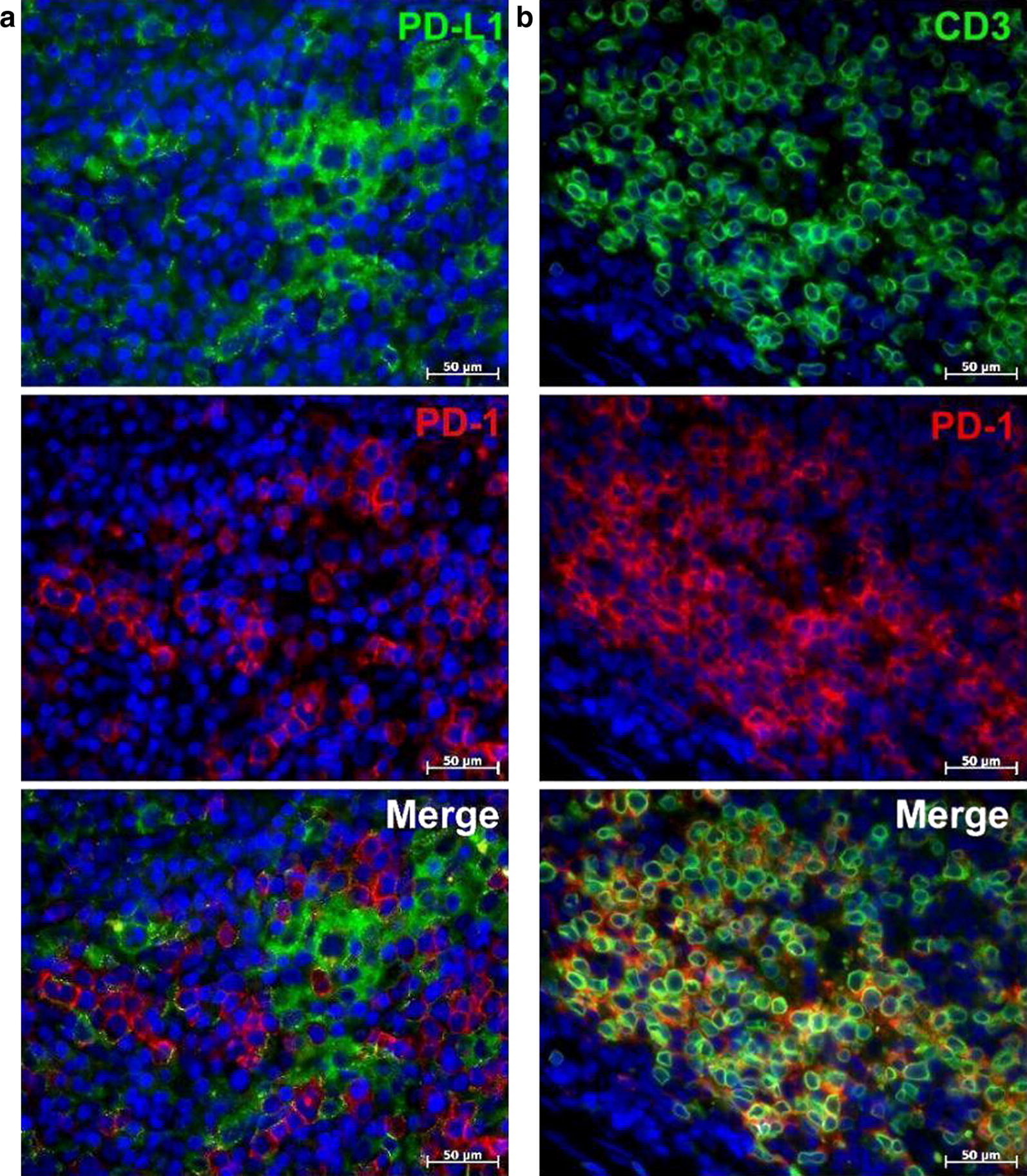
Immunofluorescent staining of PD-1, PD-L1 and CD3 in AITL. a Immunofluorescent double staining of PD-1 (Cy3, red) and PD-L1 (Alexa Fluor-488, green). PD-1 and PD-L1 are expressed poles apart from each other. b Immunofluorescent double staining of PD-1 (Cy3, red) and CD3 (Alexa Fluor-488, green). The majority of CD3-positive cells bear the PD-1 marker. Nuclei counterstained with DAPI (blue channel)
Fig. 2.
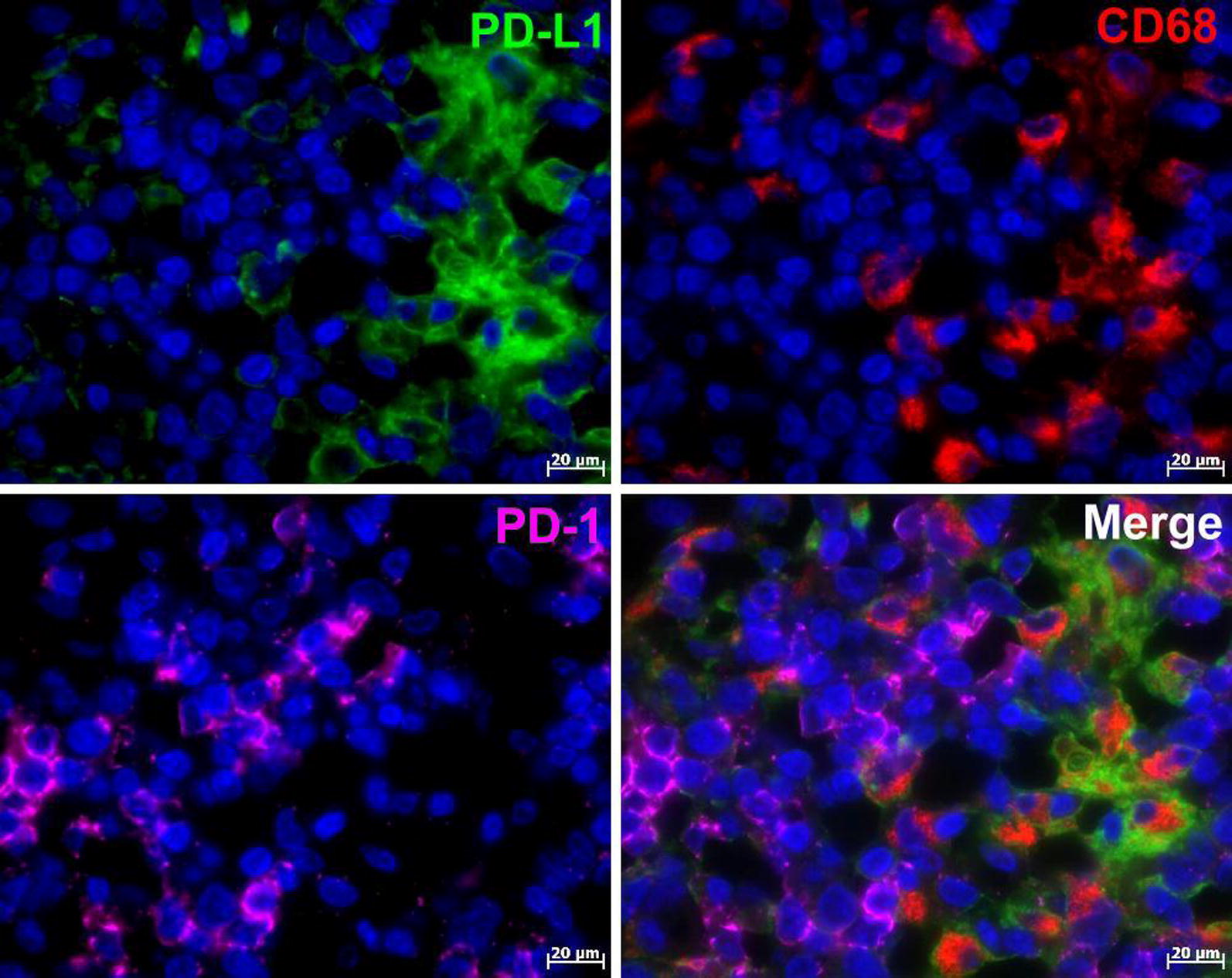
Immunofluorescent triple staining of PD-1, PD-L1 and CD68 in AITL: PD-L1 (Alexa Fluor-488, green), PD-1 (Alexa Fluor-647, magenta) and CD68 (Cy3, red). Nuclei counterstained with DAPI (blue channel). PD-1 and PD-L1 are expressed poles apart from each other, and only PD-L1- positive cells co-express CD68, the marker for macrophage lineage
For simultaneously detecting antigens from the same host species as presented in Fig. 2 and in Additional file 4: Fig. S2, we performed tyramide signal amplification (TSA) with the subsequent heat elution treatment after each immunostaining step [32, 33].
CD30 expression in AITL and Hodgkin lymphoma is currently of great interest, because therapy targeting CD30 is of clinical benefit [34]. CD30, belonging to the tumor necrosis factor receptor superfamily, is highly expressed on Reed/Sternberg cells (RSC) and believed to be involved in tumorigenesis and tumor progression [35]. In this study, we found CD30-positive cells both in Hodgkin lymphoma and in most cases in the AITL. However, histotopographic relations of CD30 antigen with PD-1 and PD-L1 revealed some differences. As seen in Fig. 3, CD30-positive cells in AITL do not express PD-L1, whereas PD-L1 antigen in Hodgkin lymphoma was detected in CD30-positive cells including Reed–Sternberg cells (RSC), preferably at the periphery, possibly at the cell membrane. In contrast to PD-L1, PD-1 was not found in RSC (Additional file 5: Fig. S3). Our results confirm and extend prior studies of PD-L1 expression in RSC in Hodgkin lymphoma [6, 36].
Fig. 3.
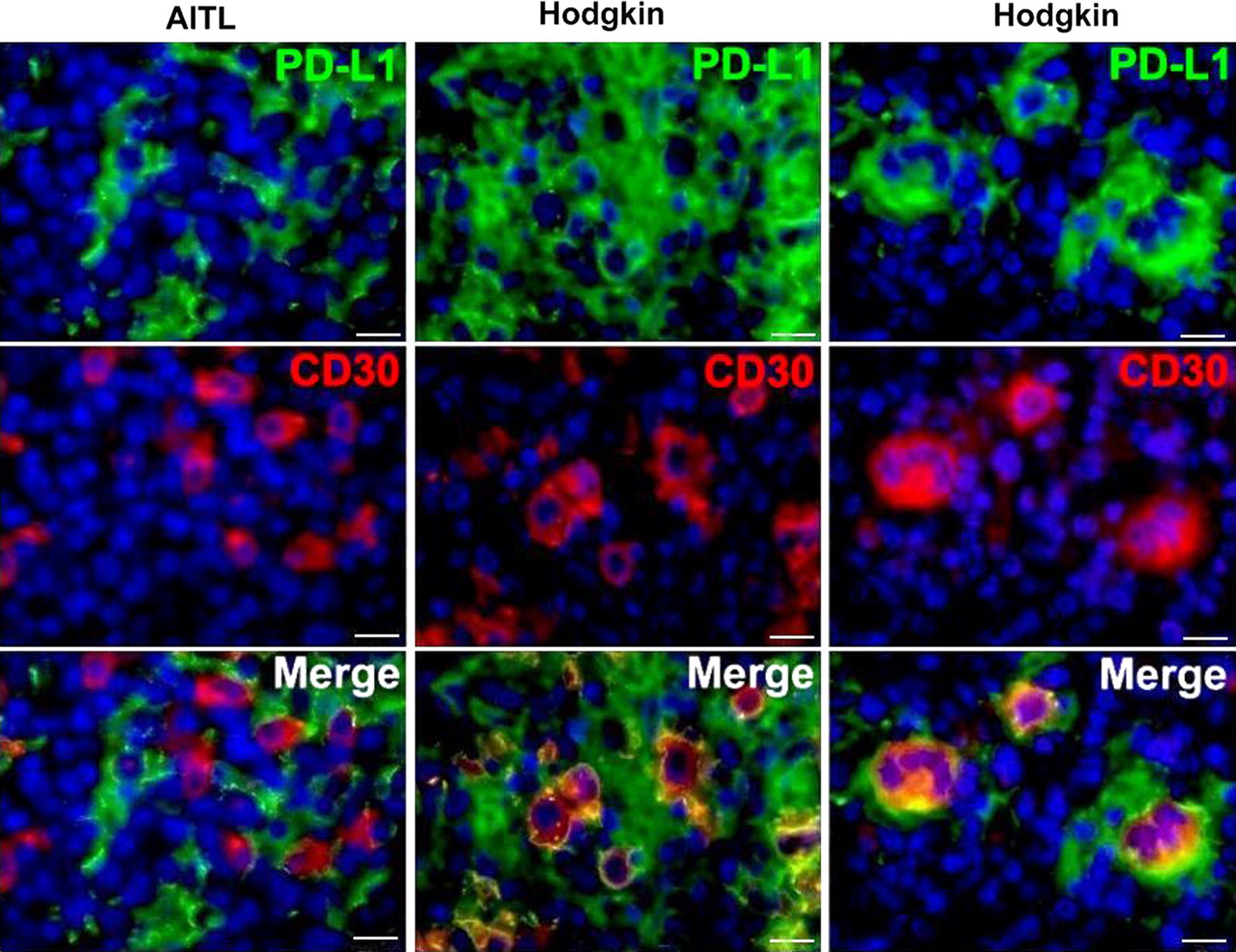
Immunofluorescent double staining of PD-L1 and CD30 in AITL and Hodgkin lymphoma: PD-L1 (Alexa Fluor-488, green), CD30 (Cy3, red). Nuclei counterstained with DAPI (blue channel). Unlike AITL, where CD30-positive cells no not co-express PD-L1, CD30+ cells in Hodgkin lymphoma bear PD-L1 antigen on the cell membrane. Scale bar 20 μm
It was earlier reported that CD30-positive cells exhibit a B-cell or a T-cell phenotype [37] and that RSC can derive from B lymphocytes [38, 39]. However in our study, we found that PD-L1-positive cells including rare malignant Hodgkin and RSC cells do not express CD20 (the marker of B-cell lineage) neither in Hodgkin lymphoma (Additional file 4: Fig. S2) nor in AITL (Additional file 6: Fig. S4). To prove a possible co-expression of CD20 in PD-L1+ cells in other tumors differing from AITL and Hodgkin lymphoma, we analyzed the probes of mediastinal lymphoma [4] taken as a control and in this case observed a definite co-localization of PD-L1 and CD20 (Additional file 7: Fig. S5).
Since it was assumed that CD10 antibody might be useful in the diagnosis of AITL [40], we decided to perform immunofluorescent double staining of PD-L1 and PD-1 vs CD10 in this lymphoma. We found that PD-L1 and CD10 are never co-localized in the same cells (Additional file 8: Fig. S6 a–c), whereas the majority of PD-1-positive cells revealed a co-expression of CD10 (Additional file 8: Fig. S6 d–f).
Discussion
PD-L1 was originally characterized as a ubiquitous antiapoptotic receptor on cancer cells [3] and it has been proposed as potential target in cancer immunotherapy in human clinic [24, 25]. However, we found that cancer cells (CD10+ and CD30+ cells) in AITL lacked the expression of PD-L1 (Additional file 5: Fig. S3 and Additional file 8: Fig. S6), whereas CD30+ cells including RSC in Hodgkin lymphoma revealed a co-expression of PD-L1 on the surface of these cells (Fig. 3). This is consistent with reports that PD-L1 expression in malignant cells of various cancers varies from 0 to 50% [7]. Therefore PD-L1 expression by tumor cells cannot serve as an absolute biomarker of clinical response to checkpoint blockade in immunotherapy, while patients, by which malignant cell in the tumor lack PD-L1 expression, also responded positively to PD-L1 checkpoint blockade therapies [7, 21, 41].
Patients with overexpressed PD-L1 in the tumor microenvironment, have improved clinical outcomes with anti-PD-L1-directed therapy [24]. Therefore PD-L1 expression in the tumor microenvironment can be regarded as a more valuable biomarker to guide clinical decisions. In our study, PD-L1 was found in the tumor microenvironment richly expressed in cells of macrophage lineage (Fig. 2). Apparently antigen-presenting cells such as macrophages may serve as a main target in PD-L1 checkpoint blockade therapies in AITL and Hodgkin lymphoma.
Our findings that CD10 in AITL is co-localized with PD-1-positive T-cells but not with PD-L1-positive cells in the tumor microenvironment support the recent studies describing CD10 as a phenotypic marker that specifically identifies the tumor cells in 90% of AITL, including the early cases [42]. The presence of CD10-positive T-cells distinguishes AITL from other unspecified peripheral T-cell lymphomas, where no CD10-positive T cells are present. Some authors reported the utility of CD10 antibody as a diagnostic marker of AITL [40]. However, further studies correlating with the clinical course will be of interest in determining the biological significance of CD10 in the AITL.
In our study, we found that PD-L1-positive cells including RSC in Hodgkin lymphoma (Additional file 4: Fig. S2) and in AITL (Additional file 6: Fig. S4) do not express CD20 (the marker of B-cell lineage). It is in accord with reports that HRS cells are CD20 negative due to downregulation of the B-cell program and it is not surprising that they CD20 and PD-L1 do not co-localize together [4, 43]. Also, these cells universally express PD-L1 in most instances with amplifications of the PD-L1 locus. This issue must further be assessed in view of the reports on elevated PD-L1 expression on B cells in other tumors [44].
Hodgkin lymphoma and AITL are malignancies in which rare malignant cells are surrounded by an extensive but ineffective inflammatory/immune cell infiltrate including PD-1-positive T-cells and PD-L1-positive antigen presenting cells. This striking feature suggests that malignant cells in these lymphomas escape immunosurveillance and interact with immune cells in the cancer microenvironment for survival and growth. Enhanced PD-1/PD-L1 signaling in Hodgkin lymphoma [4] and likewise in AITL can make these both tumors uniquely sensitive to PD-1/PD-L1 blockade.
Some authors reported on the co-expression of PD-1/PD-L1 in tumors, but virtually they presented only a simultaneous expression of PD-1 and PD-L1 in a tumor tissue taken en bloc and not in the same cells [45]. We employed multiple immunofluorescent labeling of cellular components in tissue sections of the human AITL and Hodgkin lymphoma and found that PD-1 and PD-L1 are localized in different cells, which implies that PD-1+ and PD-L1+ cells both in AITL and in Hodgkin lymphoma belong to two different cell lineages.
To summarize, our data allowed us to draw several conclusions. PD-1+ and PD-L1+ cells in the AITL and Hodgkin lymphoma are never co-localized in the same cells and therefore belong to two different cell lineages. Generally, the immunophenotype of PD-1+ and PD-L1+ cells in AITL and Hodgkin is similar, with an only exception relating to CD30 and CD10. In both lymphomas, PD-1 was found exclusively in T-lymphocytes, whereas PD-L1 was revealed in antigen-presenting cells—macrophages. PD-L1 was also detected in CD30-positive cells in Hodgkin lymphoma but not in AITL. The marker of B-cell lineage, CD20, was not detectable in PD-L1-positive cells both in AITL and in Hodgkin. HRS cells are CD20 negative due to downregulation of the B-cell program and it is not surprising that they CD20 and PD-L1 do not co-localize together. Characterization of PD-L1+ cells in these lymphomas may contribute to the development of effective approaches to the delivery anti-PD-L1 antibodies to tumors in PD-L1 blockade therapy for patients suffering from PD-L1-expressing tumors. PD-L1-antibody therapy is already proven in Hodgkin lymphoma, but there is no information about PD-L1-antibody effect in AITL. Our findings may provide further insight into an opportunity of at least an experimental attempt or clinical study as proof of the similar approach to improve the results of treatment in AITL.
Limitations
It would be interesting to what proportion of CD30+ cells in AITL are CD3+ . This question was beyond the scope of our study but it must further be assessed since that has therapeutic implications in this disease.
Supplementary information
Additional file 1: Table S1. Primary antibodies used in this study.
Additional file 2: Table S2. Secondary antibodies and other reagents.
Additional file 3: Figure S1. Immunofluorescent double staining of PD-1 and PD-L1 in Hodgkin lymphoma: PD-L1 (Alexa Fluor-488, green), PD-1 (Cy3, red). Nuclei counterstained with DAPI (blue channel). PD-1 and PD-L1 are expressed poles apart from each other.
Additional file 4: Figure S2. Immunofluorescent triple staining of PD-1, PD-L1 and CD20 in Hodgkin lymphoma: PD-1 (Alexa Fluor-488, green), PD-L1 (Alexa Fluor-647, magenta) and CD20 (Cy3, red). Nuclei counterstained with DAPI (blue channel). CD20 was not found in Reed/Sternberg cells (RSC).
Additional file 5: Figure S3. Double immunostaining of PD-1 and CD30 in Hodgkin lymphoma: (a, b) Immunofluorescent double staining of PD-1 (Alexa Fluor-488, green) and CD30 (Cy3, red). RSC intensely express CD30 in the cytoplasm and do not bear PD-1 antigen. (c) Double immunoenzyme staining for CD30 (red) and PD-1 (brown). Nuclei counterstained with hematoxylin. RSC do not bear PD-1 antigen.
Additional file 6: Figure S4. Immunofluorescent double staining of PD-L1 and CD20 in AITL: PD-L1 (Alexa Fluor-488, green), CD20 (Cy3, red). Nuclei counterstained with DAPI (blue channel). PD-L1+ cells do not co-express CD20.
Additional file 7: Figure S5. Immunofluorescent double staining of PD-L1 and CD20 in mediastinal lymphoma: PD-L1 (Alexa Fluor-488, green), CD20 (Cy3, red). Nuclei counterstained with DAPI (blue channel). Co-expression of PD-L1 and CD20 in the same cells in mediastinal lymphoma is manifested by a hybrid orange colour.
Additional file 8: Figure S6. Immunofluorescent double staining of PD-L1 (FITC, green) and PD-1 (Alexa Fluor-488, green) vs CD10 (Cy3, red) in AITL. Nuclei counterstained with DAPI (blue channel). Whereas PD-L1 and CD10 were never found in the same cells (a–c), the majority of PD-1-positive cells revealed a co-expression of CD10 manifested by a hybrid orange coulour (d–f).
Acknowledgements
This research received no specific grants from any funding agency in the public, commercial or not-for-profit sectors. We thank Denis Morozov and Alexander Glomb for perfect technical assistance and other colleagues from the immunohistology laboratory for sharing probes and reagents.
Abbreviations
- PD-1
Programmed death-1 and its ligand PD-L1
- AITL
Angioimmunoblastic T-cell lymphoma
- RSC
Reed–Sternberg cells
Authors’ contributions
MT and IB designed the study, performed the analysis and draft the manuscript. VS, and DA collected the clinical data and did immunohistochemistry. All authors read and approved the final manuscript.
Funding
No funding was acquired for this study.
Availability of data and materials
All data and materials are available on reasonable request. Address to I.B. (email: buchwalow@pathologie-hh.de) or M.T. (email: mtiemann@hp-hamburg.de) Institute for Hematopathology, Hamburg, Germany.
Ethics approval and consent to participate
This study was conducted in accordance with the principles of World Medical Association Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects” and approved by the Institutional Review Board of the Institute for Hematopathology, Hamburg, Germany (approval No. 383). All patients were informed of the investigational nature of this study and provided their written informed consent. The samples were qualified as redundant clinical specimens that had been de-identified and unlinked from patient information.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Markus Tiemann, Email: mtiemann@hp-hamburg.de.
Igor Buchwalow, Email: buchwalow@pathologie-hh.de.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13104-020-04975-w.
References
- 1.Ishida Y, Agata Y, Shibahara K, Honjo T. Induced expression of PD-1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death. EMBO J. 1992;11(11):3887–3895. doi: 10.1002/j.1460-2075.1992.tb05481.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Simon S, Labarriere N. PD-1 expression on tumor-specific T cells: friend or foe for immunotherapy? Oncoimmunology. 2017;7(1):e1364828. doi: 10.1080/2162402X.2017.1364828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dong H, Zhu G, Tamada K, Chen L. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med. 1999;5(12):1365–1369. doi: 10.1038/70932. [DOI] [PubMed] [Google Scholar]
- 4.Liu WR, Shipp MA. Signaling pathways and immune evasion mechanisms in classical Hodgkin lymphoma. Blood. 2017;130(21):2265–2270. doi: 10.1182/blood-2017-06-781989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Goodman A, Patel SP, Kurzrock R. PD-1-PD-L1 immune-checkpoint blockade in B-cell lymphomas. Nat Rev Clin Oncol. 2017;14(4):203–220. doi: 10.1038/nrclinonc.2016.168. [DOI] [PubMed] [Google Scholar]
- 6.Panjwani PK, Charu V, DeLisser M, Molina-Kirsch H, Natkunam Y, Zhao S. Programmed death-1 ligands PD-L1 and PD-L2 show distinctive and restricted patterns of expression in lymphoma subtypes. Hum Pathol. 2018;71:91–99. doi: 10.1016/j.humpath.2017.10.029. [DOI] [PubMed] [Google Scholar]
- 7.Kim HR, Ha SJ, Hong MH, Heo SJ, Koh YW, Choi EC, Kim EK, Pyo KH, Jung I, Seo D, et al. PD-L1 expression on immune cells, but not on tumor cells, is a favorable prognostic factor for head and neck cancer patients. Sci Rep. 2016;6:36956. doi: 10.1038/srep36956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thompson RH, Gillett MD, Cheville JC, Lohse CM, Dong H, Webster WS, Krejci KG, Lobo JR, Sengupta S, Chen L, et al. Costimulatory B7-H1 in renal cell carcinoma patients: indicator of tumor aggressiveness and potential therapeutic target. Proc Natl Acad Sci USA. 2004;101(49):17174–17179. doi: 10.1073/pnas.0406351101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maekawa N, Konnai S, Okagawa T, Nishimori A, Ikebuchi R, Izumi Y, Takagi S, Kagawa Y, Nakajima C, Suzuki Y, et al. Immunohistochemical analysis of PD-L1 expression in canine malignant cancers and PD-1 expression on lymphocytes in canine oral melanoma. PLoS ONE. 2016;11(6):e0157176. doi: 10.1371/journal.pone.0157176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Armand P. Immune checkpoint blockade in hematologic malignancies. Blood. 2015;125(22):3393–3400. doi: 10.1182/blood-2015-02-567453. [DOI] [PubMed] [Google Scholar]
- 11.Kekre N, Kim HT, Thanarajasingam G, Armand P, Antin JH, Cutler C, Nikiforow S, Ho VT, Koreth J, Alyea EP, et al. Efficacy of immune suppression tapering in treating relapse after reduced intensity allogeneic stem cell transplantation. Haematologica. 2015;100(9):1222–1227. doi: 10.3324/haematol.2015.129650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Goodman A, Patel SP, Kurzrock R. PD-1–PD-L1 immune-checkpoint blockade in B-cell lymphomas. Nat Rev Clin Oncol. 2016;14:203. doi: 10.1038/nrclinonc.2016.168. [DOI] [PubMed] [Google Scholar]
- 13.Gatalica Z, Bilalovic N, Vranic S, Arguello D, Reddy S, Ghosh N. PD-L1 and PD1 expression in lymphomas. Blood. 2015;126(23):3899. doi: 10.1182/blood.V126.23.3899.3899. [DOI] [Google Scholar]
- 14.He J, Hu Y, Hu M, Li B. Development of PD-1/PD-L1 pathway in tumor immune microenvironment and treatment for non-small cell lung cancer. Sci Rep. 2015;5:13110. doi: 10.1038/srep13110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zak KM, Grudnik P, Magiera K, Dömling A, Dubin G, Holak TA. Structural biology of the immune checkpoint receptor PD-1 and its ligands PD-L1/PD-L2. Structure. 2017;25(8):1163–1174. doi: 10.1016/j.str.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 16.Xu-Monette ZY, Zhou J, Young KH. PD-1 expression and clinical PD-1 blockade in B-cell lymphomas. Blood. 2018;131(1):68–83. doi: 10.1182/blood-2017-07-740993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aguiar PN, Jr, De Mello RA, Hall P, Tadokoro H, Lima Lopes GD. PD-L1 expression as a predictive biomarker in advanced non-small-cell lung cancer: updated survival data. Immunotherapy. 2017;9(6):499–506. doi: 10.2217/imt-2016-0150. [DOI] [PubMed] [Google Scholar]
- 18.Topalian SL, Drake CG, Pardoll DM. Targeting the PD-1/B7-H1(PD-L1) pathway to activate anti-tumor immunity. Curr Opin Immunol. 2012;24(2):207–212. doi: 10.1016/j.coi.2011.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Topalian SL, Hodi FS, Brahmer JR, Gettinger SN, Smith DC, McDermott DF, Powderly JD, Carvajal RD, Sosman JA, Atkins MB, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–2454. doi: 10.1056/NEJMoa1200690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Klyuchagina Y, Sokolova Z, Baryshnikova M. Role of PD-1 receptor and its ligands PD-L1 and PD-L2 in cancer immunotherapy. Onkopediatria. 2017;4(1):49–55. doi: 10.15690/onco.v4i1.1684. [DOI] [Google Scholar]
- 21.Patel SP, Kurzrock R. PD-L1 expression as a predictive biomarker in cancer immunotherapy. Mol Cancer Ther. 2015;14(4):847–856. doi: 10.1158/1535-7163.MCT-14-0983. [DOI] [PubMed] [Google Scholar]
- 22.Alsaab HO, Sau S, Alzhrani R, Tatiparti K, Bhise K, Kashaw SK, Iyer AK. PD-1 and PD-L1 checkpoint signaling inhibition for cancer immunotherapy: mechanism, combinations, and clinical outcome. Front Pharmacol. 2017;8:561. doi: 10.3389/fphar.2017.00561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fujii T, Naing A, Rolfo C, Hajjar J. Biomarkers of response to immune checkpoint blockade in cancer treatment. Crit Rev Oncol Hematol. 2018;130:108–120. doi: 10.1016/j.critrevonc.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 24.Liu D, Wang S, Bindeman W. Clinical applications of PD-L1 bioassays for cancer immunotherapy. J Hematol Oncol. 2017;10(1):110. doi: 10.1186/s13045-017-0479-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schildhaus HU. Predictive value of PD-L1 diagnostics. Pathologe. 2018;39(6):498–519. doi: 10.1007/s00292-018-0507-x. [DOI] [PubMed] [Google Scholar]
- 26.Harris NL, Jaffe ES, Diebold J, Flandrin G, Muller-Hermelink HK, Vardiman J. Lymphoma classification–from controversy to consensus: the R.E.A.L. and WHO Classification of lymphoid neoplasms. Ann Oncol. 2000;11(Suppl 1):3–10. doi: 10.1023/A:1008383406103. [DOI] [PubMed] [Google Scholar]
- 27.Stein H. The new WHO classification of malignant lymphoma. After “REAL” a further step on the road to a worldwide consensus. Pathologe. 2000;21(2):101–105. doi: 10.1007/s002920050377. [DOI] [PubMed] [Google Scholar]
- 28.Buchwalow I, Samoilova V, Boecker W, Tiemann M. Non-specific binding of antibodies in immunohistochemistry: fallacies and facts. Sci Rep. 2011;1:28. doi: 10.1038/srep00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Buchwalow IB, Boecker W. Immunohistochemistry: basics and methods. 1. Heidelberg: Springer; 2010. [Google Scholar]
- 30.Buchwalow I, Atiakshin D, Samoilova V, Boecker W, Tiemann M. Identification of autofluorescent cells in human angioimmunoblastic T-cell lymphoma. Histochem Cell Biol. 2018;149(2):169–177. doi: 10.1007/s00418-017-1624-y. [DOI] [PubMed] [Google Scholar]
- 31.Boecker W, Stenman G, Loening T, Andersson MK, Bankfalvi A, von Holstein S, Heegaard S, Lange A, Berg T, Samoilova V, et al. K5/K14-positive cells contribute to salivary gland-like breast tumors with myoepithelial differentiation. Mod Pathol. 2013;26(8):1086–1100. doi: 10.1038/modpathol.2013.45. [DOI] [PubMed] [Google Scholar]
- 32.Buchwalow I, Samoilova V, Boecker W, Tiemann M. Multiple immunolabeling with antibodies from the same host species in combination with tyramide signal amplification. Acta Histochem. 2018;120(5):405–411. doi: 10.1016/j.acthis.2018.05.002. [DOI] [PubMed] [Google Scholar]
- 33.Zhang W, Hubbard A, Jones T, Racolta A, Bhaumik S, Cummins N, Zhang L, Garsha K, Ventura F, Lefever MR, et al. Fully automated 5-plex fluorescent immunohistochemistry with tyramide signal amplification and same species antibodies. Lab Invest. 2017;97(7):873–885. doi: 10.1038/labinvest.2017.37. [DOI] [PubMed] [Google Scholar]
- 34.Bhatt G, Maddocks K, Christian B. CD30 and CD30-targeted therapies in hodgkin lymphoma and other B cell lymphomas. Curr Hematol Malig Rep. 2016;11(6):480–491. doi: 10.1007/s11899-016-0345-y. [DOI] [PubMed] [Google Scholar]
- 35.Molin D, Fischer M, Xiang Z, Larsson U, Harvima I, Venge P, Nilsson K, Sundstrom C, Enblad G, Nilsson G. Mast cells express functional CD30 ligand and are the predominant CD30L-positive cells in Hodgkin’s disease. Br J Haematol. 2001;114(3):616–623. doi: 10.1046/j.1365-2141.2001.02977.x. [DOI] [PubMed] [Google Scholar]
- 36.Roemer MG, Advani RH, Ligon AH, Natkunam Y, Redd RA, Homer H, Connelly CF, Sun HH, Daadi SE, Freeman GJ, et al. PD-L1 and PD-L2 genetic alterations define classical Hodgkin lymphoma and predict outcome. J Clin Oncol. 2016;34(23):2690–2697. doi: 10.1200/JCO.2016.66.4482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Onaindia A, Martínez N, Montes-Moreno S, Almaraz C, Rodríguez-Pinilla SM, Cereceda L, Revert JB, Ortega C, Tardio A, González L, et al. CD30 expression by B and T cells: a frequent finding in angioimmunoblastic T-Cell lymphoma and peripheral T-cell lymphoma-not otherwise specified. Am J Surg Pathol. 2016;40(3):378–385. doi: 10.1097/PAS.0000000000000571. [DOI] [PubMed] [Google Scholar]
- 38.Smith LB. Nodular lymphocyte predominant Hodgkin lymphoma: diagnostic pearls and pitfalls. Arch Pathol Lab Med. 2010;134(10):1434–1439. doi: 10.5858/2010-0207-OA.1. [DOI] [PubMed] [Google Scholar]
- 39.Kuppers R, Roers A, Kanzler H. Molecular single cell studies of normal and transformed lymphocytes. Cancer Surv. 1997;30:45–58. [PubMed] [Google Scholar]
- 40.Mlika M, Helal I, Laabidi S, Braham E, El Mezni F. Is CD10 antibody useful in the diagnosis of angioimmunoblastic T-cell lymphoma? J Immunoassay Immunochem. 2015;36(5):510–516. doi: 10.1080/15321819.2014.1001031. [DOI] [PubMed] [Google Scholar]
- 41.Gibbons Johnson RM, Dong H. Functional expression of programmed death-ligand 1 (B7-H1) by immune cells and tumor cells. Front Immunol. 2017;8:961. doi: 10.3389/fimmu.2017.00961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Attygalle A, Al-Jehani R, Diss TC, Munson P, Liu H, Du MQ, Isaacson PG, Dogan A. Neoplastic T cells in angioimmunoblastic T-cell lymphoma express CD10. Blood. 2002;99(2):627–633. doi: 10.1182/blood.V99.2.627. [DOI] [PubMed] [Google Scholar]
- 43.Liu WR, Shipp MA. Signaling pathways and immune evasion mechanisms in classical Hodgkin lymphoma. Hematology Am Soc Hematol Educ Program. 2017;2017(1):310–316. doi: 10.1182/asheducation-2017.1.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Khan AR, Hams E, Floudas A, Sparwasser T, Weaver CT, Fallon PG. PD-L1hi B cells are critical regulators of humoral immunity. Nat Commun. 2015;6:5997. doi: 10.1038/ncomms6997. [DOI] [PubMed] [Google Scholar]
- 45.Gatalica Z, Snyder C, Maney T, Ghazalpour A, Holterman DA, Xiao N, Overberg P, Rose I, Basu GD, Vranic S, et al. Programmed cell death 1 (PD-1) and its ligand (PD-L1) in common cancers and their correlation with molecular cancer type. Cancer Epidemiol Biomarkers Prev. 2014;23(12):2965–2970. doi: 10.1158/1055-9965.EPI-14-0654. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Primary antibodies used in this study.
Additional file 2: Table S2. Secondary antibodies and other reagents.
Additional file 3: Figure S1. Immunofluorescent double staining of PD-1 and PD-L1 in Hodgkin lymphoma: PD-L1 (Alexa Fluor-488, green), PD-1 (Cy3, red). Nuclei counterstained with DAPI (blue channel). PD-1 and PD-L1 are expressed poles apart from each other.
Additional file 4: Figure S2. Immunofluorescent triple staining of PD-1, PD-L1 and CD20 in Hodgkin lymphoma: PD-1 (Alexa Fluor-488, green), PD-L1 (Alexa Fluor-647, magenta) and CD20 (Cy3, red). Nuclei counterstained with DAPI (blue channel). CD20 was not found in Reed/Sternberg cells (RSC).
Additional file 5: Figure S3. Double immunostaining of PD-1 and CD30 in Hodgkin lymphoma: (a, b) Immunofluorescent double staining of PD-1 (Alexa Fluor-488, green) and CD30 (Cy3, red). RSC intensely express CD30 in the cytoplasm and do not bear PD-1 antigen. (c) Double immunoenzyme staining for CD30 (red) and PD-1 (brown). Nuclei counterstained with hematoxylin. RSC do not bear PD-1 antigen.
Additional file 6: Figure S4. Immunofluorescent double staining of PD-L1 and CD20 in AITL: PD-L1 (Alexa Fluor-488, green), CD20 (Cy3, red). Nuclei counterstained with DAPI (blue channel). PD-L1+ cells do not co-express CD20.
Additional file 7: Figure S5. Immunofluorescent double staining of PD-L1 and CD20 in mediastinal lymphoma: PD-L1 (Alexa Fluor-488, green), CD20 (Cy3, red). Nuclei counterstained with DAPI (blue channel). Co-expression of PD-L1 and CD20 in the same cells in mediastinal lymphoma is manifested by a hybrid orange colour.
Additional file 8: Figure S6. Immunofluorescent double staining of PD-L1 (FITC, green) and PD-1 (Alexa Fluor-488, green) vs CD10 (Cy3, red) in AITL. Nuclei counterstained with DAPI (blue channel). Whereas PD-L1 and CD10 were never found in the same cells (a–c), the majority of PD-1-positive cells revealed a co-expression of CD10 manifested by a hybrid orange coulour (d–f).
Data Availability Statement
All data and materials are available on reasonable request. Address to I.B. (email: buchwalow@pathologie-hh.de) or M.T. (email: mtiemann@hp-hamburg.de) Institute for Hematopathology, Hamburg, Germany.


