Abstract
Objective
The impact of early enteral nutrition (EN) on clinical outcomes in critically ill children has not been adequately described. We hypothesized that early EN is associated with improved clinical outcomes in critically ill children.
Design
Secondary analysis of the Heart And Lung Failure Pediatric INsulin Titration randomized controlled trial.
Setting
35 pediatric intensive care units (ICUs).
Patients
Critically ill children with hyperglycemia requiring inotropic support and/or invasive mechanical ventilation who were enrolled for at least 48 hours with complete nutrition data.
Exposures
Subjects received nutrition via guidelines that emphasized EN, and were classified into early EN (EN within 48 hours of study randomization) and no early EN (EN after 48 hours of study randomization, or no EN at any time).
Measurements and Main Results
Of 608 eligible subjects, 331 (54%) received early EN. Both early EN and no early EN groups had similar daily caloric intake over the first 8 study days (median 36 vs. 36 kcal/kg/day, p=0.93). After controlling for age, body mass index z-scores, primary reason for ICU admission, severity of illness, and mean vasopressor-inotrope score at the time of randomization, and adjusting for site, early EN was associated with lower 90-day hospital mortality (8% vs. 17%, p=0.007), more ICU-free days (median 20 vs. 17 days, p=0.02), more hospital-free days (median 8 vs. 0 days, p=0.003), more ventilator-free days (median 21 vs. 19 days, p=0.003), and less organ dysfunction (median maximum PELOD: 11 vs. 12, p<0.001).
Conclusions
In critically ill children with hyperglycemia requiring inotropic support and/or mechanical ventilation, early EN was independently associated with better clinical outcomes.
Keywords: timing, enteral nutrition, children, critical illness, outcomes
Introduction
Adult and pediatric guidelines for nutrition support in critical illness recommend early enteral nutrition (EN) to improve clinical outcomes (1,2). Early EN promotes and maintains gastrointestinal mucosal integrity and function (3). The benefits of early EN include fewer infections and better healing during ICU dependency with overall improved short-term and long-term clinical outcomes (3–6). While large randomized controlled trials and meta-analyses in critically ill adults have demonstrated the benefits of early EN in improving clinical outcomes and reducing costs (7–10), similar data are lacking in critically ill children (11–14). Nutrition support in critically ill children also needs to account for differences in growth, development, and metabolism that vary as a function of age and illness state (2). Though studies in critically ill children have demonstrated beneficial changes in nutritional biomarkers, nitrogen balance, inflammatory cytokines, and immune mechanisms from early EN (15–18), it is unclear if these benefits from early EN provided within 48 hours of onset of critical illness in children translate to improved clinical outcomes.
The Heart And Lung Failure Pediatric INsulin Titration (HALF-PINT) study was a randomized controlled trial that studied tight glycemic control in critically ill children who required inotropic support and/or invasive mechanical ventilation and developed hyperglycemia (19). After 50% of planned subject accrual, the study was halted following an interim analysis that examined the totality of the data and concluded a low likelihood of benefit and evidence of the possibility of harm from the intervention. Using data from this cohort of critically ill children enrolled in the HALF-PINT study across 35 centers, we performed a secondary analysis to study the association of timing of EN and clinical outcomes. We hypothesized that early EN within 48 hours from randomization into the study was associated with lower 90-day hospital mortality. Secondary outcome measures included 28-day hospital mortality, ICU-free days, hospital-free days, ventilator-free days, organ dysfunction, and healthcare associated infections (HAI).
Materials and Methods
Study Design
The HALF-PINT trial methods have been previously described (20). In this secondary analysis of subjects who received the HALF-PINT protocol, we included critically ill children who required inotropic support and/or invasive mechanical ventilation, and developed hyperglycemia [confirmed blood glucose (BG) ≥ 150 mg/dL (≥ 8.3 mmol/L)]. We excluded children with the following criteria: pre-existing diabetes mellitus, chronic ventilator dependence, limitations of care or redirection of care, inadequate vascular access, and recent cardiac surgery within the preceding 2 months. We also excluded subjects if 1) they did not provide study data for at least 48 hours, or 2) provided 48 hours or more of study data, but did not report any enteral or parenteral nutrition while on study.
All eligible subjects received either EN and/or parenteral nutrition (PN) to provide adequate energy and protein delivery via a nutrition guideline with an emphasis on use of EN. The nutrition guideline was a pragmatic algorithm designed for wide acceptance across sites, and did not curtail feeding goals. All participating sites were encouraged, but not mandated, to follow this guideline (20,21). The nutrition guideline recommended nutrition screening with anthropometry measurements to assess nutrition status, and consultation with a registered dietitian for appropriate prescription for daily energy and protein needs, volume goal, and formula type (or fluid composition) based on site specific practice. The guideline emphasized the early initiation of EN whenever feasible, with consideration for parenteral nutrition if EN was contraindicated or not tolerated. Once EN was initiated, the guideline recommended advancing feeds in step-wise fashion every 4 hours to goal volume. The guideline included recommendations to intervene in instances of feeding intolerance as well as increased gastric residual volumes, as applicable (eFigure 1, Supplemental Digital Content 1, HALF-PINT nutrition guideline). All enrolled subjects were stipulated to receive age-specific minimum glucose infusion rates (GIR) to minimize the risk of hypoglycemia. Subjects younger than 6 years of age were recommended to receive minimum GIR of 5 mg/kg/minute, while subjects older than 6 years of age were recommended to receive minimum GIR of 2.5 mg/kg/minute (22). This minimum GIR was calculated daily using both parenteral and enteral carbohydrates. All sites collected detailed nutrition data for each subject from the time of randomization until study-defined discharge criteria. No nutrition data was collected on subjects from time of ICU admission to time of study randomization, or following study-defined discharge criteria.
For this secondary analysis, energy goals for each subject were calculated post-hoc from age- and sex-specific Schofield energy equations using weight and stature data for each subject (23). Protein goals for each subject were calculated post-hoc using subsequently published guidelines jointly released by the Society of Critical Care Medicine and the American Society of Parenteral and Enteral Nutrition (2). Body mass index (BMI) z-scores were calculated using World Health Organization (WHO) Child Growth Standards to standardize the current nutrition status [underweight (z < −2), normal (−2 ≤ z ≤ 1), overweight (z > 1] of the patient [WHO Anthro software (version 3.2.2, 2011) for patients younger than 5 years and WHO AnthroPlus software (version 1.0.4, 2007) for patients 5 years of age or older]. Inotropic support at randomization was expressed as mean vasopressor-inotrope score on study day 0/1, severity of illness was expressed as Pediatric Risk of Mortality score within 12 hours of ICU admission (PRISM III-12), and organ dysfunction was expressed as Pediatric Logistic Organ Dysfunction (PELOD) scores (24–26).
Definitions and Outcomes
Exposure to EN was dichotomously classified as early EN or no early EN. Early EN was defined as provision of EN within 48 hours of randomization into the study. No early EN was defined as initiation of EN after 48 hours of randomization into the study (late EN) or no exposure to EN at any time during study enrollment (no EN). The primary outcome measure of 90-day hospital mortality was chosen based on prior studies of nutrition support interventions in critically ill children and adults (27–29). Secondary outcome measures included 28-day hospital mortality, ICU-free days to day 28, hospital-free days to day 28, ventilator-free days to day 28, organ dysfunction [expressed as maximum PELOD from Day 2 to Day 28], and HAI reported in the parent HALF-PINT study (19).
Statistical Analyses
Baseline patient characteristics, nutrition, and glycemia summary variables were compared between patients in the early EN and no early EN groups using Wilcoxon rank sum and Fisher’s exact tests, as appropriate. Differences in the primary outcome between early EN and no early EN were determined using logistic regression. Secondary outcomes were evaluated using proportional hazards regression for time-to-event outcomes, linear regression for continuous outcomes, and logistic regression for binary outcomes. All regression models were adjusted a priori for variables that may have influenced the decision to provide EN: age category, inotropic support at the time of randomization (mean vasopressor-inotrope score on study day 0/1), BMI z-score category, primary reason for ICU admission, and severity of illness (PRISM-III 12 score), and accounted for PICU site as a cluster variable to control for site-specific practice using generalized estimating equations.
We repeated these analyses adjusting for BG target range and to evaluate the potential interaction between BG target range and early EN. Subsequent analyses compared differences in clinical outcomes in two separate subgroups to address the potential limitations of the primary analysis group. First, we excluded no EN patients to compare differences between early and late EN patients. Second, we excluded patients randomized more than 48 hours after ICU admission and compared differences between early and no early EN groups. All reported p values are two-sided and were considered to be statistically significant if less than 0.05.
Results
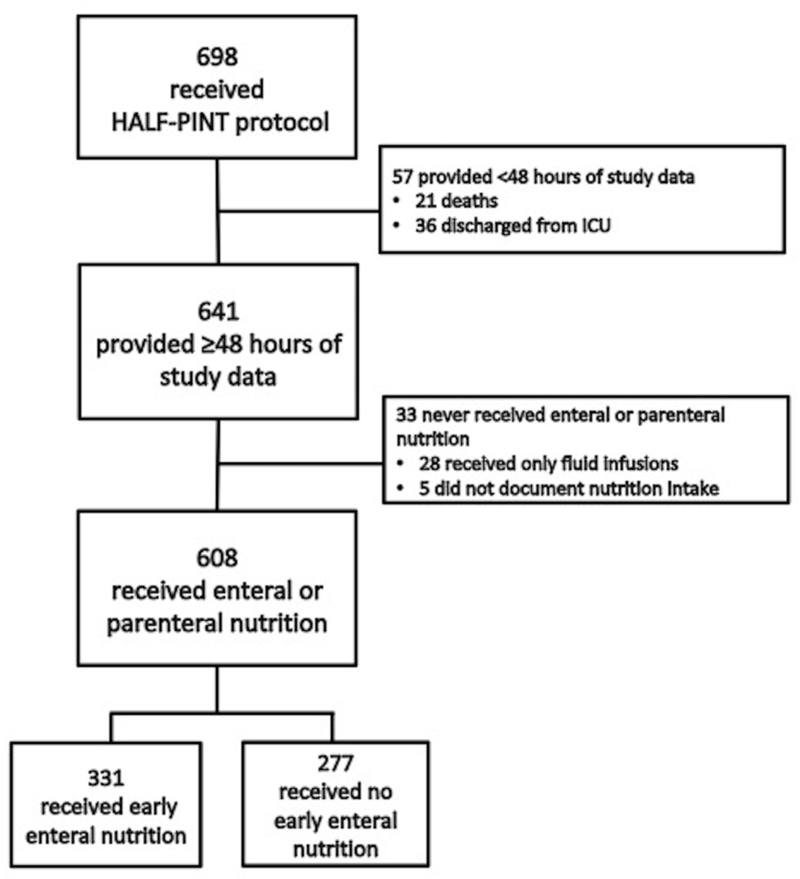
Of 698 subjects enrolled in the HALF-PINT trial, 608 subjects (87%) from 31 sites were eligible for this secondary analysis and 331 (54%) received early EN (Figure 1). The median time from ICU admission to study randomization was 37 hours [interquartile range (IQR), 22–61 hours] with 399 subjects (66%) being randomized within 48 hours of ICU admission. The early EN group had fewer subjects with immunodeficiency (2% vs. 6%, p=0.03) or immunocompromised from bone marrow transplant/cancer chemotherapy (3% vs. 12%, p<0.001) compared to the no early EN group (Table 1). Subjects in the early EN group received less inotropic support at the time of study randomization (39% vs. 65%, p<0.001) and had lower illness severity [median PRISM III-12 score (IQR), 10 (5–16) vs. 14 (8–21), p<0.001] with less baseline organ dysfunction [median PELOD score on Day 0 through Day 1 (IQR), 11 (2–12) vs. 12 (11–21), p<0.001] compared to the no early EN group. More subjects in the early EN group had respiratory dysfunction as the primary reason for ICU admission compared to the no early EN group (60% vs. 44%). Both groups were comparably well balanced for other characteristics.
Figure 1.
Flow diagram showing inclusion and exclusion of HALF-PINT subjects.
HALF-PINT= Heart And Lung Failure-Pediatric INsulin Titration, ICU= intensive care unit
Table 1.
Baseline Characteristics By Enteral Nutrition Group
| Baseline Characteristics | Early EN (n = 331) | No Early EN (n = 277) | pa |
|---|---|---|---|
| Lower glucose target group, n (%) | 159 (48) | 139 (50) | 0.63 |
| Age group, n (%) | 0.27 | ||
| 0 to 2 yr | 106 (32) | 79 (29) | |
| 2 to <7 yr | 89 (27) | 66 (24) | |
| 7 to <18 yr | 136 (41) | 132 (48) | |
| Female sex, n (%) | 156 (47) | 129 (47) | 0.94 |
| BMI z-score, n (%) | 0.14 | ||
| Underweight (z < −2) | 30 (9) | 14 (5) | |
| Normal (−2 ≤ z ≤ 1) | 170 (51) | 154 (56) | |
| Overweight (z > 1) | 131 (40) | 109 (39) | |
| Functional impairment (POPC>1), n (%) | 116 (35) | 118 (43) | 0.07 |
| Past medical history, n (%) | |||
| Premature | 61 (18) | 43 (16) | 0.39 |
| Immunodeficiency | 7 (2) | 16 (6) | 0.03 |
| Bone marrow transplant or cancer chemotherapy | 11 (3) | 33 (12) | <0.001 |
| Dialysis dependent kidney failure | 2 (<1) | 1 (<1) | 1.0 |
| Primary reason for ICU admission, n (%)b | <0.001 | ||
| Respiratory (including infections) | 200 (60) | 123 (44) | |
| Cardiovascular (including shock) | 31 (9) | 61 (22) | |
| Neurologic | 32 (10) | 22 (8) | |
| Trauma | 36 (11) | 17 (6) | |
| Following procedure | 22 (7) | 22 (8) | |
| Gastrointestinal or Liver | 1 (<1) | 22 (8) | |
| Other | 9 (3) | 10 (4) | |
| Glucocorticoid therapy at randomization, n (%) | 162 (49) | 146 (53) | 0.37 |
| Inotropic support for hypotension at randomization, n (%) | 128 (39) | 179 (65) | <0.001 |
| Mean VIS on Day 0 through Day 1, median (IQR) | 0 (0–6) | 5 (0–13) | <0.001 |
| Invasive mechanical ventilation at randomization, n (%) | 330 (>99) | 273 (99) | 0.18 |
| ECMO at randomization, n (%) | 16 (5) | 15 (5) | 0.85 |
| PRISM III-12 score, median (IQR) | 10 (5–16) | 14 (8–21) | <0.001 |
| Risk of death in the ICU, according to PRISM III-12 score, median (IQR) | 6.2 (2.1–22.8) | 16.6 (3.8–46.4) | <0.001 |
| Maximum PELOD score on Day 0 through Day 1, median (IQR) | 11 (2–12) | 12 (11–21) | <0.001 |
ECMO= extracorporeal membrane oxygenation, EN= enteral nutrition, ICU= intensive care unit, IQR= interquartile range, PRISM III-12= pediatric risk of mortality III 12 hour model, PELOD= pediatric logistic organ dysfunction, POPC= pediatric overall performance category, VIS = vasopressor-inotrope score
P values determined using Fisher’s exact tests and Wilcoxon rank-sum tests for categorical and continuous variables, respectively.
P Value determined using Pearson’s Chi-square test due to inability to perform exact computations.
Nutrition Support and Glycemia Measures
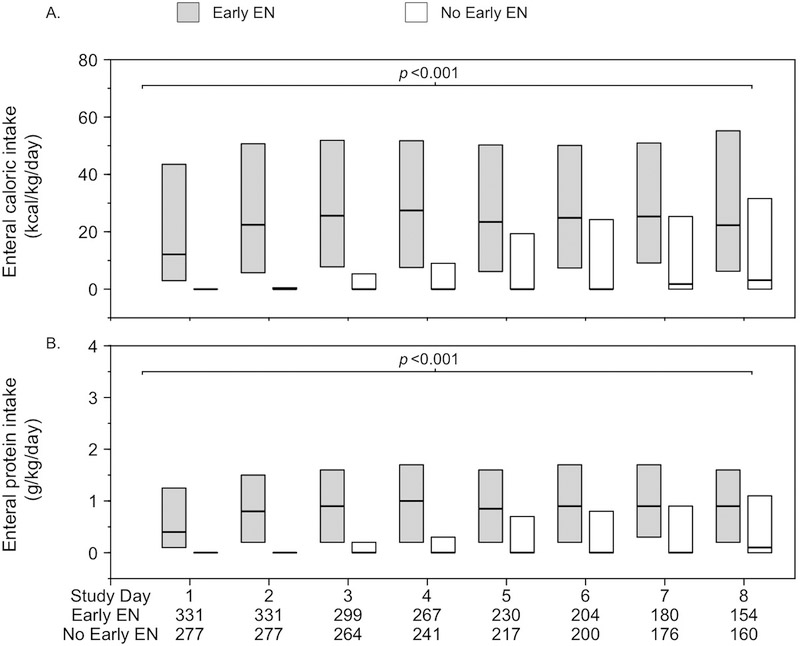
While the average daily total caloric intake over the first 8 study days was comparable across the two groups, the average total daily protein intake was lower in the early EN group compared to the no early EN group (eFigure 2, Supplemental Digital Content 2). During this same time period, the early EN group consistently received more enteral calorie and enteral protein intake compared to the no early EN group (Figure 2). Fewer subjects in the early EN group received PN compared to the no early EN group (29% vs. 79%, p<0.001) (Table 2). There were no differences across the groups when stratified for average total daily caloric intakes as percentages of their respective predicted energy goals. However, early EN patients received a higher percentage of their cumulative total caloric intake enterally compared to no early EN (84% vs 22%, p<0.001). Over three-quarters of subjects in each group received a total caloric intake that was greater than 60% of predicted energy goal during the first 8 study days (78% in early EN and 76% in no early EN). Similarly, 59% of subjects in early EN and 69% of subjects in no early EN received greater than 60% of predicted protein goal during the first 8 study days. Target feeds were achieved earlier in the early EN group compared to the no early EN group [median (IQR), 2 days (1–3) vs. 3 days (1–4), p=0.002].
Figure 2.
Average daily enteral caloric (A) and protein intake (B) by enteral nutrition group through Study Day 8.
Data are for the first eight study days (median duration of ICU stay). Panel A shows daily enteral caloric intake. Panel B shows daily enteral protein intake. In each panel, the boxes represent the interquartile range and the horizontal lines the median. P values for the comparison between groups were calculated with the use of Wilcoxon rank-sum tests (not adjusting for multiple comparisons).
EN= Enteral nutrition
Table 2.
Nutrition and Glycemia Summary By Enteral Nutrition Group
| Early EN (n = 331) | No Early EN (n = 277) | pa | |
|---|---|---|---|
| Nutrition Summary | |||
| Average daily total caloric intake over first 8 study days (kcal/kg/day), median (IQR) | 36 (22–56) | 36 (21–58) | 0.93 |
| Received <60% of their predicted energy goal, n (%)c | 74 (22) | 67 (24) | 0.08 |
| Received 60–100% of their predicted energy goal | 126 (38) | 82 (30) | |
| Received >100% of their predicted energy goal | 131 (40) | 128 (46) | |
| Average daily enteral caloric intake over first 8 study days | 25 (11–44) | 1.4 (0–11) | <0.001 |
| Percent of total caloric intake received enterally, median (IQR) | 84 (56–93) | 22 (3–57) | <0.001 |
| Average daily protein intake over first 8 study days (g/kg/day), median (IQR)c | 1.0 (0.6–1.6) | 1.4 (0.7–2.1) | <0.001 |
| Received <20% of their predicted protein goal, n (%) | 28 (8) | 39 (14) | <0.001 |
| Received 20–60% of their predicted protein goal | 109 (33) | 48 (17) | |
| Received >60% of their predicted protein goal | 194 (59) | 190 (69) | |
| Average daily enteral protein intake over first 8 study days (g/kg/day), median (IQR) | 0.84 (0.41–1.28) | 0.04 (0–0.40) | <0.001 |
| Any parenteral nutrition exposure, n (%) | 97 (29) | 219 (79) | <0.001 |
| Glycemia Summary | |||
| Time-weighted glucose average (mg/dL), median (IQR) | 112 (103–125) | 115 (105–132) | 0.02 |
| Treated with insulin therapy, n (%) | 255 (77) | 234 (84) | 0.02 |
| Average daily insulin dose (units/kg/day), median (IQR) | 0.16 (0.003–0.74) | 0.37 (0.02–0.96) | 0.001 |
| Average daily GIR (mg/kg/min), median (IQR)b | |||
| For subjects < 6 years old | 5.4 (4.2–6.5) | 6.4 (4.6–7.7) | <0.001 |
| For subjects ≥ 6 years old | 2.5 (1.9–3.3) | 3.1 (2.3–4.5) | <0.001 |
| Hypoglycemia, n (%) | |||
| Severe (<40 mg/dL) | 9 (3) | 14 (5) | 0.14 |
| Any (<60 mg/dL) | 52 (16) | 55 (20) | 0.20 |
EN= enteral nutrition, GIR= glucose infusion rate, IQR= interquartile range
P values determined using Fisher’s exact and Wilcoxon rank-sum test for categorical and continuous variables, respectively.
178 subjects less than 6 years old and 153 subjects 6 years and older received early enteral nutrition.
Based on the average daily caloric and daily protein intake over the course of the first eight days.
The early EN group had lower median time-weighted BG averages compared to the no early EN group [112 mg/dL (6.2 mmol/L) vs. 115 mg/dL (6.4 mmol/L), p=0.02] (Table 2). Fewer subjects in the early EN group were treated with insulin therapy and received less average daily insulin dosing compared to the no early EN group. Subjects in both groups received age specified average daily GIR. There were no differences in hypoglycemia rates across the two groups.
Clinical Outcomes
The 90-day mortality of the cohort was 12% (71/608). After controlling for age, BMI z-score, mean vasopressor-inotrope score at the time of randomization, primary reason for ICU admission, and severity of illness (PRISM-III 12 score) and adjusting for effect of site as cluster variable, early EN, compared to no early EN, was associated with lower 90-day hospital mortality (8% vs. 17%, p=0.007), more ICU free days [median (IQR), 20 (9–24) vs. 17 (0–22), p=0.02], more hospital-free days [median (IQR), 8 (0–17) vs. 0 (0–12), p=0.003], more ventilator-free days [median (IQR), 21 (13–25) vs. 19 (3–23), p=0.003], and less organ dysfunction [median (IQR), maximum PELOD, 11 (11–20) vs. 12 (11–22), p<0.001] (Table 3). There were no differences in 28-day hospital mortality, or HAI across groups. BG target range did not affect the relationship between early EN and observed clinical outcomes.
Table 3.
Clinical Outcomes By Enteral Nutrition Group
| Clinical Outcomes | Early EN (n = 331) | No Early EN (n = 277) | Estimate (95% CI)a | pb |
|---|---|---|---|---|
| 90-day hospital mortality, n (%) | 25 (8) | 46 (17) | OR = 0.43 (0.24–0.80) | 0.007 |
| 28-day hospital mortality, n (%) | 23 (7) | 35 (13) | OR = 0.56 (0.31–1.03) | 0.06 |
| ICU-free days (through Day 28), median (IQR) | 20.2 (9.1–23.7) | 17.2 (0–22.3) | HR = 1.26 (1.03–1.55) | 0.02 |
| Hospital-free days (through Day 28), median (IQR) | 8 (0–17) | 0 (0–12) | HR = 1.62 (1.18–2.23) | 0.003 |
| Ventilator-free days (through Day 28), median (IQR) | 21.4 (13.2–24.8) | 19.0 (3.0–23.2) | HR = 1.29 (1.07–1.57) | 0.009 |
| Maximum PELOD score (Day 2 through Day 28), median (IQR) | 11 (11–20) | 12 (11–22) | MD = −3.1 (−4.8 to −1.4) | <0.001 |
| Healthcare-associated infections, n (%) | 6 (2) | 10 (4) | OR = 0.47c (0.15–1.48) | 0.20c |
CI = confidence interval, EN = enteral nutrition, HR = hazard ratio, ICU = intensive care unit, IQR = interquartile range, MD = mean difference, OR = odds ratio, PELOD = pediatric logistic organ dysfunction.
OR < 1 indicates fewer events; HR > 1 indicates more ICU-free, hospital-free, and ventilator-free days; and MD < 0 indicates lower maximum PELOD scores for the early EN group compared to the no early EN group.
Effect estimates and p values comparing early EN and no early EN groups were calculated with the use of logistic, proportional hazards, or linear regression, as appropriate, adjusting for age category, BMI z-score category, mean vasopressor-inotrope score at randomization, primary reason for ICU admission, and PRISM-III score at 12 hours from ICU admission accounting for site as a cluster variable.
Unadjusted odds ratio and p value comparing early EN and no early EN groups were calculated with the use of univariate logistic regression accounting for site as a cluster variable due to low counts.
After excluding no EN subjects (n=78), early EN was significantly associated with more ICU-free days [median (IQR), 20 (9–24) vs. 16 (0–22), p=0.005], more ventilator-free days [21 (13–25) vs. 18 (5–23), p=0.002], more hospital-free days [8 (0–17) vs. 0 (0–12), p=0.01], less organ dysfunction [maximum PELOD, 11 (11–20) vs. 12 (11–22), p<0.001], and fewer HAIs (2% vs. 5%, p=0.02) as compared to late EN (eTable 1, Supplemental Digital Content 3). In addition, after excluding subjects randomized more than 48 hours after ICU admission (n=209), early EN was associated with more hospital-free days [11 (0–19) vs. 3.5 (0–14), p=0.02], fewer HAIs (<1% vs. 3%, p=0.03), and improved trends towards other outcomes compared to no early EN (eTable 2, Supplemental Digital Content 4).
Discussion
Our study reflects contemporary nutrition support practice for a large cohort of critically ill children across multiple centers in North America and provides compelling evidence that a nutrition support strategy of early EN is beneficial and likely to improve both short-term and long-term clinical outcomes in critically ill children with hyperglycemia. In this secondary analysis, we observed that early EN initiation within 48 hours following randomization into the HALF-PINT study was associated with lower 90-day hospital mortality in critically ill children with hyperglycemia. Early EN was also associated with more hospital-free days, more ventilator-free days, and less organ dysfunction compared to no early EN.
The better clinical outcomes in the early EN group might be directly due to the benefits of early EN. The early EN group received a greater median percentage of total caloric intake via the enteral route during study enrollment in comparison to the no early EN group (84% vs 22%). These observations in the early EN group demonstrate the feasibility of providing sustained EN to this population of critically ill children (30). The early EN group also reached target feeds faster than the no early EN group. Additionally, the average daily total caloric intake over the first 8 study days in the early EN group was comparable to the no early EN group with three-quarters of subjects in both groups receiving greater than 60% of predicted energy goal. The comparable total energy intake across both groups raises the intriguing possibility that the early provision of EN maybe an even more important factor than the absolute amount of energy provided in improving clinical outcomes, though it is possible that this may be of consequence only above a critical energy threshold. Additionally, the higher average enteral daily protein intake in the early EN group compared to the no early EN group may have also influenced clinical outcomes favorably in the early EN group and could reflect the importance of the enteral route for protein intake (31,32).
Alternatively, the combination of more PN exposure, higher GIR, and/or greater insulin exposure may have adversely impacted clinical outcomes in the no early EN group. The no early EN group experienced earlier and higher PN exposure with higher average daily GIR compared to the early EN group. Subjects in the no early EN group had more exposure to insulin with higher time-weighted BG average measurements compared to the early EN group. The impact of timing of PN was explored in a recent randomized controlled trial (The Early versus Late Parenteral Nutrition in the Pediatric Intensive Care Unit – PEPaNIC) that compared early versus late PN in critically ill children and observed that early PN was associated with worse clinical outcomes compared to the late PN group (33). Notably, in the present study, subjects in the no early EN group had higher average total daily protein intake compared to those in the early EN group, likely due to greater PN use in the no early EN group. Interestingly, a secondary analysis of the PEPaNIC study recently raised the possibility that harm from the use of early PN may be associated with higher doses of parenterally delivered amino acids, but not glucose or lipids (15,34).
In the present study, significantly fewer children on inotropic support at the time of randomization received early EN compared to no early EN. Though studies in critically ill children have demonstrated the safety of EN in children supported with vasoactive infusions (35,36), our analysis highlights that clinicians tend to avoid early EN initiation in the setting of hemodynamic instability requiring inotropic support. On the other hand, invasive mechanical ventilation support did not appear to influence timing of EN initiation, in contrast to findings from a retrospective cross-sectional study of critically ill children that identified invasive mechanical ventilation as a risk factor for delay in EN initiation (37,38). Not surprisingly, very few children with gastrointestinal reasons for ICU admission received early EN. Children with traumatic injury as the primary indication for ICU admission were more likely to receive early EN compared to no early EN (11% vs 6%).
While smaller studies in critically ill children have demonstrated beneficial changes in nutritional biomarkers, nitrogen balance, inflammatory cytokines and immune mechanisms from early EN (15–18), large randomized controlled trials to study the impact of early EN to improve clinical outcomes in critically ill children are lacking. A prospective study that randomized critically ill children to early EN (within 6–24 hours of ICU admission) or late EN (after 24 hours of ICU admission) did not observe any differences in mortality, measures of ICU dependency or infections, but was notably underpowered to detect these differences (39). A recent secondary analysis of nutrition support in children who experienced severe traumatic brain injury and were managed with therapeutic hypothermia observed that early EN when provided within 72 hours of initial brain injury was associated with improved clinical outcomes (40).
We defined the no early EN group as a pragmatic comparison group to include both late EN and no EN to reflect contemporary real world practice. When we restricted our comparison to early EN and late EN by excluding no EN, we continued to observe similar trends in association of early EN with improved clinical outcomes. Though baseline characteristics of late EN and no EN groups were comparable (data not shown), the no EN group had higher 90-day mortality compared to both early EN and late EN groups.
The present study has several strengths. First, the HALF-PINT study enrolled critically ill children receiving inotropic support and/or invasive mechanical ventilation, with a high severity of illness and mortality that enabled us to test our hypothesis that early EN initiation is associated with clinical improvements in this population. Second, nutrition support data was rigorously and prospectively collected for the HALF-PINT study with trained data abstractors (19). Third, the sample size represents 31 pediatric ICUs and thus reflects current practice across multiple sites, lending external validity to the results and generalizability to current care models in North America. Fourth, our study design involved the use of a standardized approach to nutrition support across sites with the use of guidelines that emphasized provision of EN with a stepwise algorithmic approach to reaching goal energy needs (20,21).
Our study was limited by lack of nutrition support data from the time of ICU admission to the time of study randomization. This limits comparability to other studies that have traditionally followed nutrition support from the time of ICU admission (26,38,41,42). To address this limitation in our design, we performed a subgroup analysis to compare outcomes in subjects randomized within 48 hours of ICU admission and observed similar outcomes favoring early EN. Additionally, the cohort of critically ill children with cardiovascular and/or respiratory failure in this study arguably represents a more accurate and enriched target population that is most likely to benefit from early EN in contrast to typical pediatric ICU populations that often also consist of less severely ill children including those frequently admitted for observation. The early EN group had fewer subjects with immunodeficient states compared to the no early EN group, although both groups had very few subjects with immunodeficient states. We also did not collect information on feeding interruptions and site of feeding (gastric vs. postpyloric), both of which are known to influence the feasibility of early EN in critically ill children (43,44). Though the HALF-PINT study included a pre-specified nutrition guideline with emphasis on EN that was distributed to all sites, compliance with this guideline cannot be guaranteed for all subjects. Challenges included inability to accurately define energy needs in critically ill children to avoid overfeeding or underfeeding (45). Predictive equations such as Schofield equations are inferior to indirect calorimetry methods to estimate energy requirements in critically ill children (46). We attempted to overcome variations in site-specific nutrition practice by accounting for PICU site as a cluster variable. To account for the possibility that sicker children may have been less likely to receive early EN, we adjusted for severity of illness using PRISM-III 12 score as a marker that may have influenced EN delivery, and noted that early EN continued to be associated with improved clinical outcomes in this population. As this was a secondary analysis of the HALF-PINT study, our study was not primarily powered to study the impact of timing of EN on clinical outcomes. Finally, the results of this secondary analysis may not be generalizable to other populations of critically ill children as the parent HALF-PINT cohort enrolled critically ill children with hyperglycemia.
Conclusions
In this secondary analysis of the HALF-PINT study of critically ill children with hyperglycemia, early EN within 48 hours of randomization into the study was independently associated with lower 90-day mortality, more ventilator-free days, more hospital-free days, and less organ dysfunction after adjusting for age, BMI z-score, inotropic support at the time of study randomization, primary reason for ICU admission, and severity of illness. Prospective studies to investigate the quantity of EN (both energy and protein) delivered would be helpful to better characterize the impact of early EN in influencing clinical outcomes in critically ill children.
Supplementary Material
Acknowledgements
We thank the children who participated in the HALF-PINT study and their parents and guardians, as well as the study coordinators at all the participating sites.
Funding Support: Supported by grants (U01HL107681-MA/VN and U01HL108028-DW) from the National Heart, Lung, and Blood Institute, National Institutes of Health and by endowed chairs (to Drs. Agus and Nadkarni); HALF-PINT ClinicalTrials.gov number, NCT01565941
Copyright form disclosure: Drs. Srinivasan, Hasbani, Allen, Typpo, Faustino, Wypij, and Agus received support for article research from the National Institutes of Health (NIH). Dr. Irving received funding for partial meeting registration fee for presentation faculty from ASPEN and Society of Critical Care Medicine. Dr. Allen’s institution received funding from NIH (through Boston Children’s Hospital and also through Oklahoma Medical Research Foundation) and the American Nurses Foundation (through Akron Children’s Hospital). Dr. Typpo’s institution received funding from NIH NIDDK and Baxter. Dr. Cvijanovich’s institution received funding from Cincinnati Children’s Hospital Medical Center, Boston Children’s Hospital Medical Center, Children’s Hospital of Philadelphia, UCLA, and Seattle Children’s Hospital. Dr. Wypij’s institution received funding from the National Heart, Lung, and Blood Institute/NIH. The remaining authors have disclosed that they do not have any potential conflicts of interest.
Footnotes
Financial Disclosure/Conflicts of Interest: None
References
- 1.Taylor BE, McClave SA, Martindale RG, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). Crit Care Med 2016; 44:390–438. [DOI] [PubMed] [Google Scholar]
- 2.Mehta NM, Skillman HE, Irving SY, et al. Guidelines for the provision and assessment of nutrition support therapy in the pediatric critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition. Pediatr Crit Care Med 2017; 18:675–715. [DOI] [PubMed] [Google Scholar]
- 3.Nguyen NQ, Besanko LK, Burgstad C, et al. Delayed enteral feeding impairs intestinal carbohydrate absorption in critically ill patients. Crit Care Med 2012; 40:50–4. [DOI] [PubMed] [Google Scholar]
- 4.Xi F, Li N, Geng Y, et al. Effects of delayed enteral nutrition on inflammatory responses and immune function competence in critically ill patients with prolonged fasting. Hepatogastroenterology 2014; 61:606–12. [PubMed] [Google Scholar]
- 5.McClave SA, Heyland DK. The physiologic response and associated clinical benefits from provision of early enteral nutrition. Nutr Clin Pract 2009; 24:305–15. [DOI] [PubMed] [Google Scholar]
- 6.Briassoulis G, Zavras N, Hatzis T. Malnutrition, nutritional indices, and early enteral feeding in critically ill children. Nutrition 2001; 17:548–57. [DOI] [PubMed] [Google Scholar]
- 7.Doig GS, Heighes PT, Simpson F, et al. Early enteral nutrition, provided within 24 h of injury or intensive care unit admission, significantly reduces mortality in critically ill patients: a meta-analysis of randomised controlled trials. Intensive Care Med 2009; 35:2018–27. [DOI] [PubMed] [Google Scholar]
- 8.Elke G, van Zanten AR, Lemieux M, et al. Enteral versus parenteral nutrition in critically ill patients: an updated systematic review and meta-analysis of randomized controlled trials. Crit Care 2016; 20:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doig GS, Chevrou-Séverac H, Simpson F. Early enteral nutrition in critical illness: a full economic analysis using US costs. Clinicoecon Outcomes Res 2013; 5:429–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tian F, Heighes PT, Allingstrup MJ, et al. Early enteral nutrition provided within 24 hours of ICU admission: a meta-analysis of randomized controlled trials. Crit Care Med 2018; 46:1049–56. [DOI] [PubMed] [Google Scholar]
- 11.Silva FM, Bermudes AC, Maneschy IR, et al. Impact of early enteral nutrition therapy on morbimortality reduction in a pediatric intensive care unit: a systematic review. Rev Assoc Med Bras (1992) 2013; 59:563–70. [DOI] [PubMed] [Google Scholar]
- 12.Joffe A, Anton N, Lequier L, et al. Nutritional support for critically ill children. Cochrane Database Syst Rev 2016; (5):CD005144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kerklaan D, Fivez T, Mehta NM, et al. Worldwide survey of nutritional practices in PICUs. Pediatr Crit Care Med 2016; 17:10–8. [DOI] [PubMed] [Google Scholar]
- 14.Greathouse KC, Sakellaris KT, Tumin D, et al. Impact of early initiation of enteral nutrition on survival during pediatric extracorporeal membrane oxygenation. JPEN J Parenter Enteral Nutr 2018; 42:205–211. [DOI] [PubMed] [Google Scholar]
- 15.Briassoulis G, Venkataraman S, Thompson A. Cytokines and metabolic patterns in pediatric patients with critical illness. Clin Dev Immunol 2010; 2010:354047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Briassoulis G, Filippou O, Kanariou M, et al. Comparative effects of early randomized immune or non-immune-enhancing enteral nutrition on cytokine production in children with septic shock. Intensive Care Med 2005; 31:851–8. [DOI] [PubMed] [Google Scholar]
- 17.Briassoulis G, Tsorva A, Zavras N, et al. Influence of an aggressive early enteral nutrition protocol on nitrogen balance in critically ill children. J Nutr Biochem 2002; 13:560. [DOI] [PubMed] [Google Scholar]
- 18.Briassoulis G, Filippou O, Kanariou M, et al. Temporal nutritional and inflammatory changes in children with severe head injury fed a regular or an immune-enhancing diet: A randomized, controlled trial. Pediatr Crit Care Med 2006; 7:56–62. [DOI] [PubMed] [Google Scholar]
- 19.Agus MS, Wypij D, Hirshberg EL, et al. Tight glycemic control in critically ill children. N Engl J Med 2017; 376:729–741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agus MS, Hirshberg E, Srinivasan V, et al. Design and rationale of Heart and Lung Failure - Pediatric INsulin Titration Trial (HALF-PINT): A randomized clinical trial of tight glycemic control in hyperglycemic critically ill children. Contemp Clin Trials 2017; 53:178–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hamilton S, McAleer DM, Ariagno K, et al. A stepwise enteral nutrition algorithm for critically ill children helps achieve nutrient delivery goals. Pediatr Crit Care Med 2014; 15:583–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bier DM, Leake RD, Haymond MW, et al. Measurement of “true” glucose production rates in infancy and childhood with 6,6-dideuteroglucose. Diabetes 1977; 26:1016–1023. [DOI] [PubMed] [Google Scholar]
- 23.Schofield WN. Predicting basal metabolic rate, new standards and review of previous work. Hum Nutr Clin Nutr 1985; 39 Suppl 1:5–41. [PubMed] [Google Scholar]
- 24.Gaies MG, Gurney JG, Yen AH, et al. Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med 2010; 11:234–8. [DOI] [PubMed] [Google Scholar]
- 25.Pollack MM, Patel KM, Ruttimann UE. PRISM III: an updated Pediatric Risk of Mortality score. Crit Care Med 1996; 24:743–52. [DOI] [PubMed] [Google Scholar]
- 26.Leteurtre S, Martinot A, Duhamel A, et al. Validation of the paediatric logistic organ dysfunction (PELOD) score: prospective, observational, multicentre study. Lancet 2003; 362:192–7. [DOI] [PubMed] [Google Scholar]
- 27.Mehta NM, Bechard LJ, Cahill N, et al. Nutritional practices and their relationship to clinical outcomes in critically ill children--an international multicenter cohort study. Crit Care Med 2012; 40:2204–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alberda C, Gramlich L, Jones N, et al. The relationship between nutritional intake and clinical outcomes in critically ill patients: results of an international multicenter observational study. Intensive Care Med 2009; 35:1728–37. [DOI] [PubMed] [Google Scholar]
- 29.Arabi YM, Aldawood AS, Haddad SH, et al. Permissive underfeeding or standard enteral feeding in critically ill adults. N Engl J Med 2015; 372:2398–408. [DOI] [PubMed] [Google Scholar]
- 30.Briassoulis GC, Zavras NJ, Hatzis TD. Effectiveness and safety of a protocol for promotion of early intragastric feeding in critically ill children. Pediatr Crit Care Med 2001; 2:113–21. [DOI] [PubMed] [Google Scholar]
- 31.Mehta NM, Bechard LJ, Zurakowski D, et al. Adequate enteral protein intake is inversely associated with 60-d mortality in critically ill children: a multicenter, prospective, cohort study. Am J Clin Nutr 2015; 102:199–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Briassoulis G, Filippou O, Hatzi E, et al. Early enteral administration of immunonutrition in critically ill children: results of a blinded randomized controlled clinical trial. Nutrition 2005; 21:799–807. [DOI] [PubMed] [Google Scholar]
- 33.Fivez T, Kerklaan D, Mesotten D, et al. Early versus Late Parenteral Nutrition in Critically Ill Children. N Engl J Med 2016; 374: 1111–22. [DOI] [PubMed] [Google Scholar]
- 34.Vanhorebeek I, Verbruggen S, Casaer MP, et al. Effect of early supplemental parenteral nutrition in the paediatric ICU: a preplanned observational study of post-randomisation treatments in the PEPaNIC trial. Lancet Respir Med 2017; 5: 475–483. [DOI] [PubMed] [Google Scholar]
- 35.King W, Petrillo T, Pettignano R. Enteral nutrition and cardiovascular medications in the pediatric intensive care unit. JPEN J Parenter Enteral Nutr 2004; 28:334–8. [DOI] [PubMed] [Google Scholar]; Panchal AK, Manzi J, Connolly S, et al. Safety of enteral feedings in critically ill children receiving vasoactive agents. JPEN J Parenter Enteral Nutr 2016; 40:236–41. [DOI] [PubMed] [Google Scholar]
- 36.Mehta NM, McAleer D, Hamilton S, et al. Challenges to optimal enteral nutrition in a multidisciplinary pediatric intensive care unit. JPEN J Parenter Enteral Nutr 2010; 34: 38–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Panchal AK, Manzi J, Connolly S, et al. Safety of enteral feedings in critically ill children receiving vasoactive agents. JPEN J Parenter Enteral Nutr 2016; 40:236–41. [DOI] [PubMed] [Google Scholar]
- 38.Canarie MF, Barry S, Carroll CL, et al. Risk factors for delayed enteral nutrition in critically ill children. Pediatr Crit Care Med 2015; 16:e283–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Prakash V, Parameswaran N, Biswal N. Early versus late enteral feeding in critically ill children: a randomized controlled trial. Intensive Care Med 2016; 42:481–2. [DOI] [PubMed] [Google Scholar]
- 40.Meinert E, Bell MJ, Buttram S, et al. Initiating nutritional support before 72 hours is associated with favorable outcome after severe traumatic brain injury in children: A secondary analysis of a randomized, controlled trial of therapeutic hypothermia. Pediatr Crit Care Med 2018; 19:345–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mikhailov TA, Kuhn EM, Manzi J, et al. Early enteral nutrition is associated with lower mortality in critically ill children. JPEN J Parenter Enteral Nutr 2014; 38:459–66. [DOI] [PubMed] [Google Scholar]
- 42.Haney A, Burritt E, Babbitt CJ. The impact of early enteral nutrition on pediatric acute respiratory failure. Clin Nutr ESPEN 2018; 26:42–6. [DOI] [PubMed] [Google Scholar]
- 43.Keehn A, O’Brien C, Mazurak V, et al. Epidemiology of interruptions to nutrition support in critically ill children in the pediatric intensive care unit. JPEN J Parenter Enteral Nutr 2015; 39:211–7. [DOI] [PubMed] [Google Scholar]
- 44.Moreno YM, Hauschild DB, Barbosa E, et al. Problems with optimal energy and protein delivery in the pediatric intensive care unit. Nutr Clin Pract 2016; 31:673–80. [DOI] [PubMed] [Google Scholar]
- 45.Briassoulis G, Briassouli E, Tavladaki T, et al. Unpredictable combination of metabolic and feeding patterns in malnourished critically ill children: the malnutrition-energy assessment question. Intensive Care Med 2014; 40:120–2. [DOI] [PubMed] [Google Scholar]
- 46.Meyer R, Kulinskaya E, Briassoulis G, et al. The challenge of developing a new predictive formula to estimate energy requirements in ventilated critically ill children. Nutr Clin Pract 2012; 27:669–76. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.