Abstract
Cognitive engineering is focused on how humans can cope and master the complexity of processes and technological environments. In cardiothoracic surgery, the goal is to support safe and effective human performance by preventing medical errors. Strategies derived from cognitive engineering research could be introduced in cardiothoracic surgery practice in the near future to enhance patient safety and outcomes.
Keywords: Cognitive engineering, Mental workload, Patient safety, Surgical data science, Neuroergonomics, Human factors, Medical errors
Cognitive engineering (CE) is the analysis, modeling, design, and evaluation of complex sociotechnical systems (eg, nuclear plants, aviation, surgery) and is largely driven by the increased cognitive demands found in these technology-rich environments. CE studies the functional capabilities and limitations of humans and methods to integrate these findings into the design and optimization of systems, processes, and technology.1 The CE field acquired its current identity after the Three-Mile Island nuclear power plant accident in Pennsylvania in 1979 and the term “cognitive engineering” was first used by Norman in 1980.2 CE is focused on how humans can cope and master the complexity of processes and technological environments. For example, rather than using technology to automate an action in an effort to eliminate human error, a more beneficial approach would be to augment, rather than automate, human capabilities. In the case of driving, technology makes it possible for a vehicle to monitor both the roadway and the driver. Thus, it could enhance the driver’s awareness of the roadway conditions and improve the driver’s capacity to respond to those demands. Augmented cognition technology might improve safety by measuring the degree to which the driver is distracted and then directing a distracted driver’s attention by alerting the driver to roadway demands.3
CE IN HEALTHCARE
CE research in healthcare, with the goal of supporting safe and effective performance, focuses on characterizing complexities in the environment and demands on providers, with emphasis on preventing medical errors and on the design and impacts of new technologies. Understanding demands on providers, the strategies they use to meet those demands, and the role of information from different sources and technologies in work practice is essential to designing new information systems that can improve patient care.4
COGNITIVE WORK AND TASK ANALYSIS
Cognitive work analysis (CWA) is one of several analytic approaches to CE. CWA emerged from the work of Rasmussen at Risø National Laboratory in Denmark5 while advising how to design human-machine systems, such as nuclear power plant control rooms, so that they would be safer and more reliable. The Risø group found ways to ensure high technical reliability for such systems. However, accidents and incidents still occurred, usually when human operators were required to handle situations and abnormalities that system designers had not anticipated. In such situations, operators effectively had to “finish the design” of the system—that is, through their activities and the information available to them, the operators had to compensate for the information or resources that were missing to preserve the purpose of the system. Finding ways to support operators performing such “adaptive compensation” became very important.
Another technique related to CWA, and commonly used in the human factors field, is cognitive task analysis (CTA).6 CTA involves a structured mixed-methods approach to capture the cognitive processes used by experts to perform certain tasks. While hierarchical task analysis is focused on the determination of the correct sequence of tasks/subtasks and the relationships between them, CTA can further capture the cognitive processes underlying task execution, as well as variations from routine course of action and occurrence of unexpected events. In healthcare (eg, surgery), CTA has the potential to reveal the cognitive factors underpinning medical errors and inform prevention and mitigation strategies.
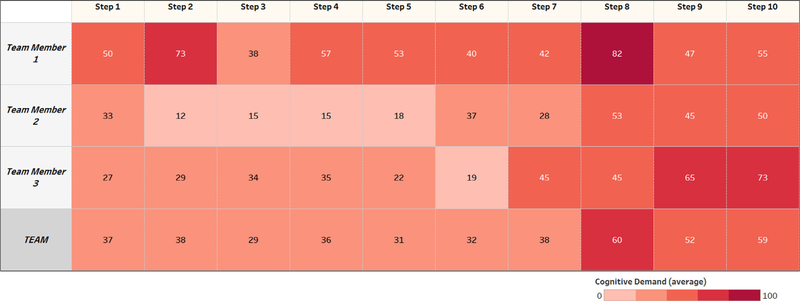
In cardiothoracic surgery, our research group at Harvard University has developed a video-based recall protocol to elucidate team cognitive processes in the operating room. We used CTA methods to interview subject matter experts from multiple domains (surgery, anesthesia, perfusion) and, built upon a previous cardiac surgery process model,7 we identified 137 unique intraoperative cognitive processes, including 33 decision points, 23 critical communication, 43 potential pitfalls, and 38 problem prevention/solving strategies during coronary artery bypass grafting (CABG) procedures.8 By quantifying the anticipated effort on a scale from 1 to 100, we were able to create a matrix that anticipates surgical phases during CABG that are associated with higher workload, thus supporting targeted efforts to improve performance both at the individual and at the team level (Fig. 1).
Figure 1.
Self-reported cognitive workload during different steps of CABG.
COGNITIVE BASIS OF MEDICAL ERRORS
Medical errors causing preventable adverse events are the third leading cause of death in the United States; the negative economic impact of preventable medical errors was estimated at $1 trillion per year in a US Senate hearing in 2014.9 The global burden of postoperative deaths is estimated at 4.2 million patients, making it the third greatest contributor after ischemic heart disease and stroke. For the last 20 years since the publication of the seminal report by the Institute of Medicine entitled “To Err is Human,”10 insufficient progress has been realized to make surgery safer. Procedural care (eg, cardiothoracic surgery) is particularly vulnerable and error-prone due to its complexity and need for multispecialty teams to cooperate.11,12
The traditional perspective of patient safety implicates that the desired patient outcome results from the interaction among patient risk factors and technical skills of the involved providers. These factors are meaningful and established contributors to medical errors but are not necessarily comprehensive. The field of surgery has more recently recognized the significant influence of nontechnical skill (ie, situation awareness, teamwork, decision-making, communication) on outcomes as well.13
Studies in high-hazard industries demonstrate that humans, irrespective of expertise, do not optimally retrieve or deploy key knowledge under high levels of mental workload (MWL).14 The reduction of high MWL not only may reduce the frequency of errors but also may increase the likelihood that errors will be detected and recovered.
COGNITIVE CHALLENGES IN SURGERY
In surgery, demands on attention and working memory processing have greatly increased, as providers engage with more data, perform more complex tasks, and exchange more information. Attention, working memory, and decision-making are 3 key areas of cognitive functioning that are negatively affected among healthcare providers experiencing excessive levels of MWL.15,16 In surgery, the frequency of flow disruptions (a surrogate of errors) experienced by providers is alarming (~100 per surgical case). During simulated surgeries, intraoperative workload was shown to be significantly higher when flow disruptions were intentionally introduced. Increasingly, safe levels of cognitive workload during complex surgical procedures are exceeded due to multitasking and interruptions. Human performance deficiencies (HPD—defined as errors associated with cognitive, technical, and team dynamic functions) have been identified in more than 50% of adverse events in surgery; the most common HPD was cognitive error in the execution of care.17
MWL
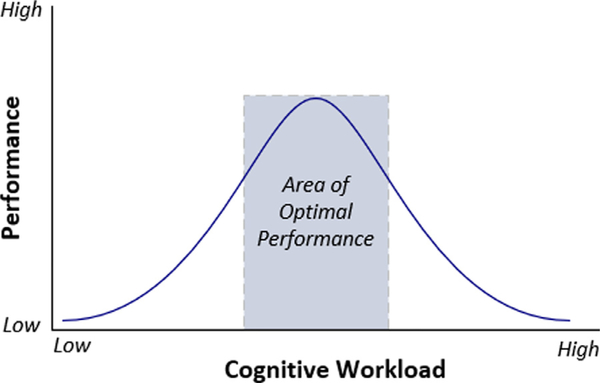
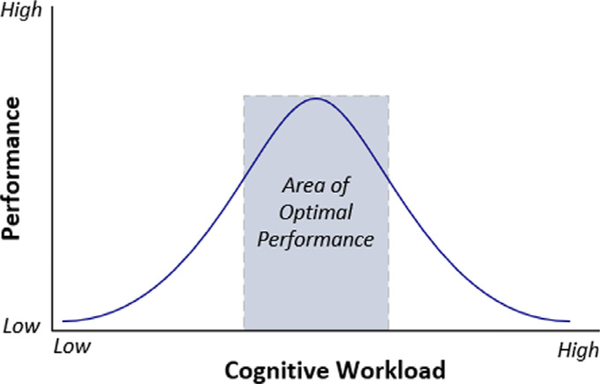
Cognitive or MWL is defined as a multidimensional construct representing the load that a task imposes on the performer.18 This also refers to the level of perceived effort for learning, thinking, and reasoning as an indicator of pressure on working memory during task execution. This measure of MWL represents the interaction between task processing demands and human capabilities or resources. MWL is usually considered to be a property of an individual rather than a task. Working memory is limited in capacity, processing, and duration. In situations in which the demand imposed by tasks exceeds our working memory capacity, a state of cognitive overload occurs. The result of competition for limited cognitive resources is often a decrease in task performance. The relationship between workload and performance is described by an inverted U-shape curve according to the Hebb-Yerkes-Dodson Law, suggesting that both very high workload (overload) and very low workload (underload) are associated with lower performance, and that higher performance is achieved in a medium workload condition (Fig. 2). Thus, depending on where the individual is on the curve, increasing cognitive workload could increase or decrease performance. If cognitive workload rises too high, performance suffers (because the individual no longer can manage the cognitive demands of the task).
Figure 2.
Relationship between cognitive workload and performance.
Ineffective mental states (eg, high emotions, peak workload, lack of situation awareness, fatigue) play a significant role in the sequence of events leading to errors and preventable adverse events.19,20 Regardless of how competent and expert surgical team members may be, they are still subject to the common cognitive limitations, frailties, and fallibilities that characterize the human brain. In certain situations, high demands imposed by surgical tasks and other factors may exceed the cognitive capacity, leading to a potentially risky cognitive overload. A recent report from our group identified for the first time high emotional state (anger/frustration) as a precursor to a near-miss error in cardiac surgery, leading to potential for system redesign.21
MEASUREMENT OF COGNITIVE WORKLOAD
We performed a systematic review of the literature on available tools to measure cognitive workload in surgery.22 Among the available psychophysiological tools for the measurement of cognitive workload that can be used in real-time, heart rate variability (HRV) is the most studied. HRV is established as a sensitive and reliable physiological index of work stress and mental effort.23 Tools using HRV can be applied in an unobtrusive manner with inexpensive, wearable, and wireless devices. HRV metrics are based on the analysis of interbeat intervals (R-R intervals) allowing the quantification of sinoatrial rhythm variability. These HRV measures are most commonly divided in 2 broad categories: HRV frequency-domain and HRV time-domain parameters. Two frequency-domain parameters, low-frequency (LF) band and high-frequency (HF) band, have been shown to reflect the balance between the sympathetic and parasympathetic autonomic nervous system. In situations imposing a high cognitive demand, there is a sympathetic predominance, increasing the LF/HF ratio. Other well-established HRV parameters, such as the root mean square of the successive differences (RMSSD), the standard deviation of normalto-normal (SDNN) interbeat interval duration, and the percentage of consecutive inter-beat intervals varying by at least 50 milliseconds (pNN50) are reflective of parasympathetic control, such that higher cognitive demands decrease these time-domain values. LF/HF ratio, RMSSD, SDNN, and pNN50 have all been used as objective and real-time measures of cognitive workload in the literature.24 A third category of HRV analysis includes nonlinear measures such as measures of entropy, which are also gaining attention as valuable workload indicators.
In addition to HRV, eye movements and changes in pupil dilation also provide important information about how users interact with complex visual displays (eg, during endoscopy). Data can be obtained by using eye-tracking apparatus that captures eye data in a nearly continuous signal, providing precise information about what the user looks at, how long he looks at it, and how much his pupils dilate as he looks. Gaze duration, derived from eye-gaze metrics, has been shown to differentiate expertise level as well as the presence of unexpected adverse events while viewing surgical video clips. Marshall introduced the Index of Cognitive Activity that allows reliable and rapid estimation of cognitive workload from changes in pupil dilation. This approach has been useful in military simulations associated with screen-based tasks under the augmented cognition program funded by the US Department of Defense through DARPA.25 Research done with eye-tracking technology in the healthcare setting is being conducted for intraoperative use in surgery, aiming to reduce its invasiveness and need for continuous screen monitoring and tracking.
The temporal sensitivity and high accuracy of noninvasive brain imaging techniques such as electroencephalography and functional near infrared spectroscopy afford insight into cognitive workload as well. Both technologies have been used in medical simulation and have demonstrated their utility in this domain but cannot currently be utilized during live surgeries due to their obtrusiveness and physical constraints.
AUGMENTED COGNITION IN SURGERY
Augmented cognition refers to the design and implementation of closed-loop systems based upon real-time psychophysiological assessment. This approach relies on sensing a user’s cognitive state via psychophysiological measures, and utilizing this knowledge to adapt the human-computer interaction and tailor the user’s environment to their current state in real time.26 The goal of implementing augmented cognition systems is to enhance operational capability, minimize redundancies in task completion, and improve human performance in high-consequence, high-demand environments.27
Workload-adaptive systems have been pioneered in the military for time-critical and high workload situations associated with risk of excessive operator mental workload and loss of situation awareness. For example, the index of cognitive activity utilizes real-time measurement of pupillary diameter and has been validated to allow rapid and reliable estimation of cognitive workload during unmanned aerial vehicle operations in the US Air Force.
Advanced applications of augmented cognition for healthcare providers are lacking. To address this gap, we have designed a team cognitive guidance system for the operating room using process and patient real-time data dynamically and proactively to provide guidance forward from the current surgical state. This workload-adaptive system will identify plausible upcoming situations in which cognitive load can be expected to approach safety-concerning levels. Process analysis will then be used to warn of such possibilities, advise of immediate actions (eg, task shedding), and/or to explore such approaches as resource reallocation or alternative paths, all aimed at avoiding or reducing high-risk cognitive load levels on an individual and team-wide basis.
TEAM PERFORMANCE IN SURGERY
Teamwork characterizes virtually all work performed in the healthcare system. Ideally, the entire healthcare team and medical devices work together flawlessly in real time; this amounts to a complex cyber-physical-human system, posing a medical information and workflow management challenge. The cardiac surgical OR is a technically complex, fast-paced environment where multiple disciplines are expected to collaborate in an efficient and effective manner. Individual roles further require the acquisition of specialized skills, interdependent work, decision-making, and a high cognitive demand.
Team performance measurement systems in healthcare have benefited from sensor-based approaches. Sensor-based measures refer to automated data collection tools (eg, infrared sensors, radio frequency identification tags) used to dynamically capture socio-metrical data (ie, behavior, team member composition, speech content). Activity traces can complement sensor-based measures to understand patterns of behavior between team members because they capture the byproduct of information system use (eg, paging system, e-mail activity, electronic health record entries).
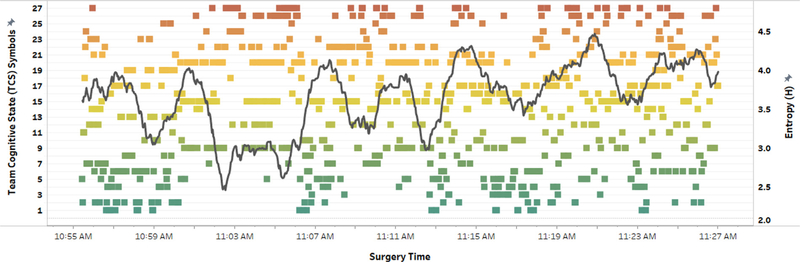
In the OR environment, task demands are not equally distributed across different team members and over the course of surgery. In fact, we have demonstrated that both perceived and objective measured (via HRV) cognitive load varies depending on team role and surgical step.28,29 A useful conceptual model that can be applied in cardiothoracic surgery is the “distributed cognition” framework. It considers the activity system as the unit of cognitive analysis rather that the individual team member, allowing the study of how cognitive resources and demands are handled and distributed throughout the surgical team.30 To investigate how cognitive load is distributed during CABG procedures, we developed a novel method that uses a psychophysiological biomarker (interbeat interval—IBI in milliseconds) captured from surgeons, anesthesiologists, and perfusionists via wearable sensors, and derives a combined team measure of physiological synchronization, as a proxy for team cognitive load. We were able to demonstrate, for the first time, how a cardiac surgery team responds to an intraoperative adverse event (medication error) based on physiological synchronization metrics (Fig. 3).31 Concurrent/mirrored peaks across multiple team members may reflect problem-solving mentalities, focused attention, task coordination, and/or shared mental models converging during times of ambiguity or crisis.32
Figure 3.
Team physiological synchronization during a CABG procedure.
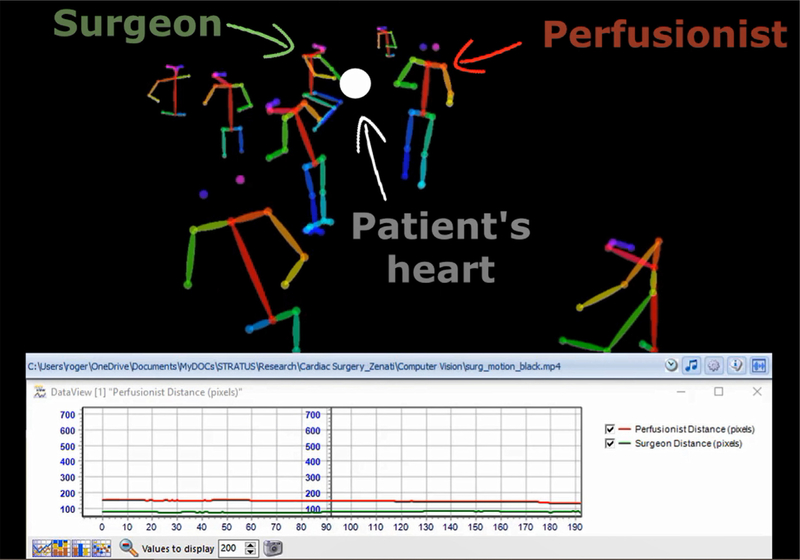
COMPUTER VISION FOR TEAM MONITORING IN SURGERY
Modern operating rooms are high-tech environments, where surgical activities are increasingly captured with cameras. The automatic understanding of this visual data by extracting rich and meaningful information is a promising way of developing machine intelligence and context-aware systems in the clinical environment. It will help to improve the workflow in hospitals by developing better decision support systems for the clinicians. We demonstrated the feasibility of using multiperson pose estimation from video recordings in conjunction with psychophysiological data reflecting team cognitive load.28 Our work illustrates the utility in computer vision approaches to monitor spatial relationships between providers, the patient, and medical devices in the operating room, and the added potential to incorporate temporal cognitive workload data simultaneously (Fig. 4).
Figure 4.
Deep learning-enabled software tracking team members’ position and motion.
SURGICAL DATA SCIENCE
Future advances in surgery will be motivated by safety, effectiveness, and efficiency of care. Cognition-guided surgery will promote a culture of continuous measurement, assessment, and improvement using evidence from data as a core component; in addition, it will facilitate the transition from subjective to objective decision-making and from qualitative to quantitative assessment in surgery. Although large amount of data is available during interventional care, it is not routinely captured and annotated using standardized protocols.
The emerging field of surgical data science strives toward a data-driven healthcare environment, leveraging data from medical records and devices, imaging, and/or sensors to improve interventional approaches.33 Such extensive data capture introduces the potential for predictive modeling, decision support, adaptive aiding, and further applications across clinical disciplines. Challenges facing the field of surgical data science include the availability and analytic power of acquired data, stakeholder buy-in, and the end-user patient experience. Harnessing advancing technology and emphasizing dissemination efforts will be critical to support the impact of the field.
FUTURE DIRECTIONS
It is anticipated that many strategies derived from CE studies could be introduced in cardiothoracic surgery in the near future to support human performance and enhance patient safety and outcomes (Table 1). In some cases, introduction of dedicated technology could be envisioned to leverage available surgical data for error modeling and prevention and recovery. Advanced workload-adaptive associate systems are already operational in the military (drones, submarine nav) and translation into the cardiovascular operating room is being tested in simulated environments.
Table 1.
Cognitive Engineering Strategies for Error Prevention and Management
| Cognitive engineering strategies for error management in cardiothoracic surgery |
| • Task shedding34 |
| • Intelligent interruption system35 |
| • Sterile cockpit36 |
| • Short breaks15 |
| • Team strengthening15 |
| • Preincision time-out37 |
| • Safety system for device interoperabilty38 |
| • Workload-adaptive associate systems |
| • Cognitive aids for high-risk/low-frequency situations39 |
Central Message.
Improved understanding of the cognitive basis of preventable medical errors offers the opportunity to develop new strategies to prevent and mitigate human errors in cardiothoracic surgery.
Yerkes-Dodson Law correlating mental workload and performance.
Acknowledgments
Funding: Supported by the National Institutes of Health and National Heart, Lung and Blood Institute under award no. 1R01 HL126896 (PI: Marco Zenati, MD).
REFERENCES
- 1.Hollnagel E, Woods DD: Joint Cognitive Systems: Foundations of Cognitive Systems Engineering. Boca Raton, FL, CRC Press; 2005. ISBN 0–84932821-7 [Google Scholar]
- 2.Norman DA: Cognitive engineering In: Norman DA, Draper SW, eds. User-Centered System Design, Mahwah, NJ: Erlbaum, 1986, pp 31–61 [Google Scholar]
- 3.Donmez B, Boyle LN, Lee JD, et al. : Safety implications of providing real-time feedback to distracted drivers. Accid Anal Prev 39:581–590, 2007 [DOI] [PubMed] [Google Scholar]
- 4.Bisantz AM, Burns CM, Fairbanks RJ: Cognitive Systems Engineering in Health Care. Boca Raton, FL, CRC Press; 2014. ISBN-10: 1466587962 [Google Scholar]
- 5.Rasmussen J, Vicente KJ: Coping with human errors through system design: Implications for ecological interface design. Int J Man Mach Stud 31:517–534, 1989 [Google Scholar]
- 6.Hoffman RR, Shadbolt NR, Burton A, et al. : Eliciting knowledge from experts: A methodological analysis. Organ Behav Hum Decis Process 62:129–158, 1995. 10.1006/obhd.1995.1039 [DOI] [Google Scholar]
- 7.Avrunin GS, Christov SC, Clarke LA, et al. : Process-driven guidance for complex surgical procedures. In: American Medical Informatics Association (AMIA) Annu Symp Proc 2018 Dec 5; 2018. p. 175–184 [PMC free article] [PubMed] [Google Scholar]
- 8.Dias RD, Zenati MA, Conboy HM, et al. : Dissecting cardiac surgery: A video-based recall protocol to elucidate team cognitive processes in the operating room. Ann Surg 2019. 10.1097/SLA.0000000000003489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Makary MA, Daniel M: Medical error—The third leading cause of death in the US. BMJ 353:1–5, 2016 [DOI] [PubMed] [Google Scholar]
- 10.Institute of Medicine: To Err Is Human: Building a Safer Health System In: Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building a Safer Health System, Washington, D.C.: National Academy Press; 1999 [Google Scholar]
- 11.Brown EKH, Harder KA, Apostolidou I, et al. : Identifying variability in mental models within and between disciplines caring for the cardiac surgical patient. Anesth Analg 125:29–37, 2017 [DOI] [PubMed] [Google Scholar]
- 12.Wahr JA, Prager RL, Abernathy JH, et al. : Patient safety in the cardiac operating room: Human factors and teamwork. Circulation 128:1139–1169, 2013 [DOI] [PubMed] [Google Scholar]
- 13.Patel VL, Kannampallil TG, Shortliffe EH: Role of cognition in generating and mitigating errors. BMJ Qual Saf 24:468–474, 2015. [DOI] [PubMed] [Google Scholar]
- 14.Leveson NG: Engineering a safer world Systems Thinking Applied to Safety. MIT Press; 2011 [Google Scholar]
- 15.Enhancing Surgical Performance In: Flin R, Youngson GG, Yule SJ, eds. Enhancing Surgical Performance, Boca Raton, FL: CRC Press; 2016 [Google Scholar]
- 16.Yurko YY, Scerbo MW, Prabhu AS, et al. : Higher mental workload is associated with poorer laparoscopic performance as measured by the NASA-TLX tool. Simul Healthc 5:267–271, 2010 [DOI] [PubMed] [Google Scholar]
- 17.Suliburk JW, Buck QM, Pirko CJ, et al. : Analysis of human performance deficiencies associated with surgical adverse events. JAMA Network Open 2:e198067, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Young MS, Brookhuis KA, Wickens CD, et al. : State of science: Mental workload in ergonomics. Ergonomics 58:1–17, 2015 [DOI] [PubMed] [Google Scholar]
- 19.Endsley MR: Toward a theory of situation awareness in dynamic systems. Hum Factors 37:32–64, 1995 [Google Scholar]
- 20.Albayram Y, Khan MMH, Jensen T, et al. : The effects of risk and role on users’ anticipated emotions in safety-critical systems. In Harris D (Ed.): Engineering Psychology and Cognitive Ergonomics (EPCE) 2018, LNAI 10906, pp. 369–388. [Google Scholar]
- 21.Zenati MA, Dias RD, Leissner K, et al. : First reported use of team cognitive workload for root cause analysis in cardiac surgery. Semin Thorac Cardiovasc Surg 2018. 10.1053/j.semtcvs.2018.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dias RD, Ngo-Howard C, Boskowski M, et al. : Systematic review of measurement tools to assess surgeon’s intraoperative cognitive workload. Br J Surg 105:491–501, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hughes AM, Hancock GM, Marlow SL, et al. : Cardiac measures of cognitive workload: a meta-analysis. Hum Factors 2019. 10.1177/0018720819830553 [DOI] [PubMed] [Google Scholar]
- 24.Kennedy-Metz LR, Dias RD, Conboy HM, et al. : Quantifying intraoperative cognitive workload in complex surgical environments. In: Proceedings, 2019 International Conference on Robotics and Automation (ICRA), Full- Day Workshop: Next Generation Surgery: Seamless Integration of Robotics, Machine Learning and Knowledge Representation Within the Operating Rooms, Montreal, Quebec, Canada; 2019 [Google Scholar]
- 25.Marshall SP: The index of cognitive activity: Measuring cognitive workload. In: Proceedings of the IEEE 7th Conference on Human Factors and Power Plants; 2002. p. 5–9. 10.1109/HFPP.2002.1042860 [DOI] [Google Scholar]
- 26.Raley C, Stripling R, Kruse A, et al. : Augmented cognition overview: Improving information intake under stress. Proc Hum Factor Ergon Soc Annu Meet 48:1150–1154, 2004. 10.1177/154193120404801001 [DOI] [Google Scholar]
- 27.Dias RD, Conboy HM, Gabany JM, et al. : Development of an interactive dashboard to analyze cognitive workload of surgical teams during complex procedural care. In: 2018 IEEE Conference on Cognitive and Computational Aspects of Situation Management (CogSIMA) Boston, MA; 2018. p. 77–82. 10.1109/COGSIMA.2018.8423995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dias RD, Yule SJ, Kennedy-Metz L, et al. : Psychophysiological data and computer vision to assess cognitive load and team dynamics in cardiac surgery. In: Proceedings, Information Processing in Computer Assisted Interventions (IPCAI), Rennes, France; 2019. June 18–19 [Google Scholar]
- 29.Suliburk JW, Buck QM, Pirko CJ, et al. : Analysis of human performance deficiencies associated with surgical adverse events. JAMA Network Open 2:e198067, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hazlehurst B, McMullen CK, Gorman PN: Distributed cognition in the heart room: How situation awareness arises from coordinated communications during cardiac surgery. J Biomed Inform 40:539–551, 2007 [DOI] [PubMed] [Google Scholar]
- 31.Dias RD, Zenati MA, Stevens R, et al. : Physiological synchronization and entropy as measures of team cognitive load. J Biomed Inform 96:103250, 2019. 10.1016/j.jbi.2019.103250. Epub 2019 Jul 8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kennedy-Metz LR, Dias RD, Stevens RH, et al. : Analysis of mirrored psychophysiological change of cardiac surgery team members during open surgery. Acad Surg Congr 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Meier-Hein L, Vedula SS, Speidel S, et al. : Surgical data science for next-generation interventions. Nat Biomed Eng 1:691–696, 2017 [DOI] [PubMed] [Google Scholar]
- 34.Zenati MA, Scarinci A: Cutting off the lizard’s tail in surgery. J Thorac Cardiovasc Surg 156:1220–1221, 2018. 10.1016/j.jtcvs.2018.02.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dias RD, Conboy HM, Gabany JM, et al. : Intelligent interruption management system to enhance safety and performance in complex surgical and robotic procedures In: Stoyanov D, Taylor Z, Sarikaya D, eds. OR 2.0 Context-Aware Operating Theaters, Computer Assisted Robotic Endoscopy, Clinical Image-Based Procedures, and Skin Image Analysis, ed 1, Springer Nature International, 2018, pp. 62–68. 10.1007/978-3-030-01201-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zenati MA, Dias RD, Gabany JM, et al. : A cognitive “Safe Zone Rule” to protect situation awareness and improve communication in surgery. In: Proceedings, AATS Surgical Patients Safety Course, Renaissance Boston Waterfront, Boston, MA; 2018. June 29–30 [Google Scholar]
- 37.Spanjersberg AJ, Ottervanger JP, Nierich AP, et al. : Implementation of a specific safety check is associated with lower postoperative mortality in cardiac surgery. J Thorac Cardiovasc Surg 2019. in press [DOI] [PubMed] [Google Scholar]
- 38.Arney D, Rance G, Srey R, et al. : A novel interoperable safety system for improved coordination and communication in cardiac surgery In: Stoyanov D, Taylor Z, Sarikaya D, eds. OR 2.0 Context-Aware Operating Theaters, Computer Assisted Robotic Endoscopy, Clinical Image-Based Procedures, and Skin Image Analysis, 1st ed., Springer Nature International, 2018, pp. 39–45. 10.1007/978-3-030-01201-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tarola CL, Hirji S, Yule SJ, et al. : Cognitive support to promote shared mental models during safety-critical situations in cardiac surgery. 2018 IEEE Conf Comput Asp Situat Manag CogSIMA (2018): 165–167, 2018. 10.1109/COGSIMA.2018.8423991. Epub 2018 Aug 2 [DOI] [PMC free article] [PubMed] [Google Scholar]