Abstract
Studies indicate that Black patients report higher medical mistrust compared to their White counterparts. However, little is known about factors associated with higher medical mistrust among Black breast cancer patients. We examined predictors of medical mistrust and relationships between medical mistrust, subscales of mistrust, and process of care factors to identify opportunities to promote positive healthcare interactions between the trustees (e.g., providers) and Black breast cancer patients, or the trustors. A secondary analysis was conducted of survey data from 210 Black women with confirmed diagnosis of invasive breast cancer. Participants completed telephone surveys consisting of questions pertaining to sociodemographics, attitudes, and beliefs about medical care and breast cancer treatments. Multiple linear regression determined factors associated with medical mistrust and mistrust subscales. Most participants (61%) were over the age of 50 and currently single (64.8%). Women with greater medical mistrust reported less satisfaction with the trustee’s technical ability (p < 0.0001) and greater satisfaction with their own propensity to access care (p < 0.05). Additionally, women with public insurance demonstrated greater mistrust (p < 0.01) and suspicion (p < 0.05) than women with private insurance, and women with less education reported greater perceived discrimination than women who have at least a bachelor’s degree. Findings from this study may inform future endeavors to educate providers on ways to effectively interact with and treat Black breast cancer patients. Opportunities to develop interventions that address and tackle issues of mistrust as reported by Black patients may contribute to ongoing efforts to reduce health disparities.
Keywords: Medical mistrust, Breast cancer, African American women
Introduction
Mistrust of the medical system continues to emerge as a significant concern voiced by research participants and patients [1–4]. Specifically, Blacks report higher mistrust towards the medical establishment than their White counterparts [5–7]. Feelings of medical mistrust are more prevalent in Black breast cancer patients than White breast cancer patients and may contribute to existing disparities in treatment utilization [6, 8]. Studies have shown that individuals who report greater medical mistrust also tend to have poorer physical and emotional well-being and quality of life [9–14]. Black breast cancer patients not only report greater mistrust but also suffer from higher rates of cancer recurrence and mortality [6, 8, 15]. Some healthcare factors that may influence medical mistrust include provider communication and patient satisfaction [16, 17].
While complex in nature, feelings of medical mistrust likely range from historical events (e.g., Tuskegee Syphilis Study) to personal interactions that occur in healthcare settings [18–20]. Contemporary reports of perceived discrimination and racism, underrepresentation of Blacks in clinical trials, and the lack of participation by Black individuals in the blood and organ donor pools further exacerbate the problem of mistrust [1, 18, 21–24]. Regardless of the reasons behind feelings of mistrust, the effects continue to contribute to less uptake of healthcare services, dissatisfaction with care, and disparate outcomes. Such findings warrant the need to examine factors that contribute to and correlate with medical mistrust, particularly regarding to individuals with chronic diseases.
The conceptual framework that guides this investigation was adopted from Mayer and colleagues’ Integrative Model of Organizational Trust (Fig. 1) [25]. This multilevel model posits the roles of the trustor (e.g., breast cancer patient) and the trustee (e.g., breast cancer provider) with regard to one’s trust/mistrust in an organization (e.g., healthcare setting). Demographics and propensity, or ability and capability, affect the trustor’s capacity to trust. Further, three constructs related to the trustee—ability, benevolence, and integrity—also contribute to the trustor’s ability to trust in an organization. In our study, women provided demographic information and rated their satisfaction with their propensity to afford and access care. When assessing the trustor’s perspectives, it is important to consider the potential impact of unrelated or related prior experiences that may affect her assessment of the trustee and/or the organization [25]. Additionally, women assessed their providers’ ability, benevolence, and integrity by rating factors including communication, technical and professional quality, and interpersonal behavior. It is important to understand factors (e.g., provider ability, sociodemographics) that may contribute to greater medical mistrust felt by Black women because such factors may serve as potential intervention targets (e.g., provider education) and are known to contribute to the overall healthcare experience, therefore affecting patient outcomes.
Fig. 1.
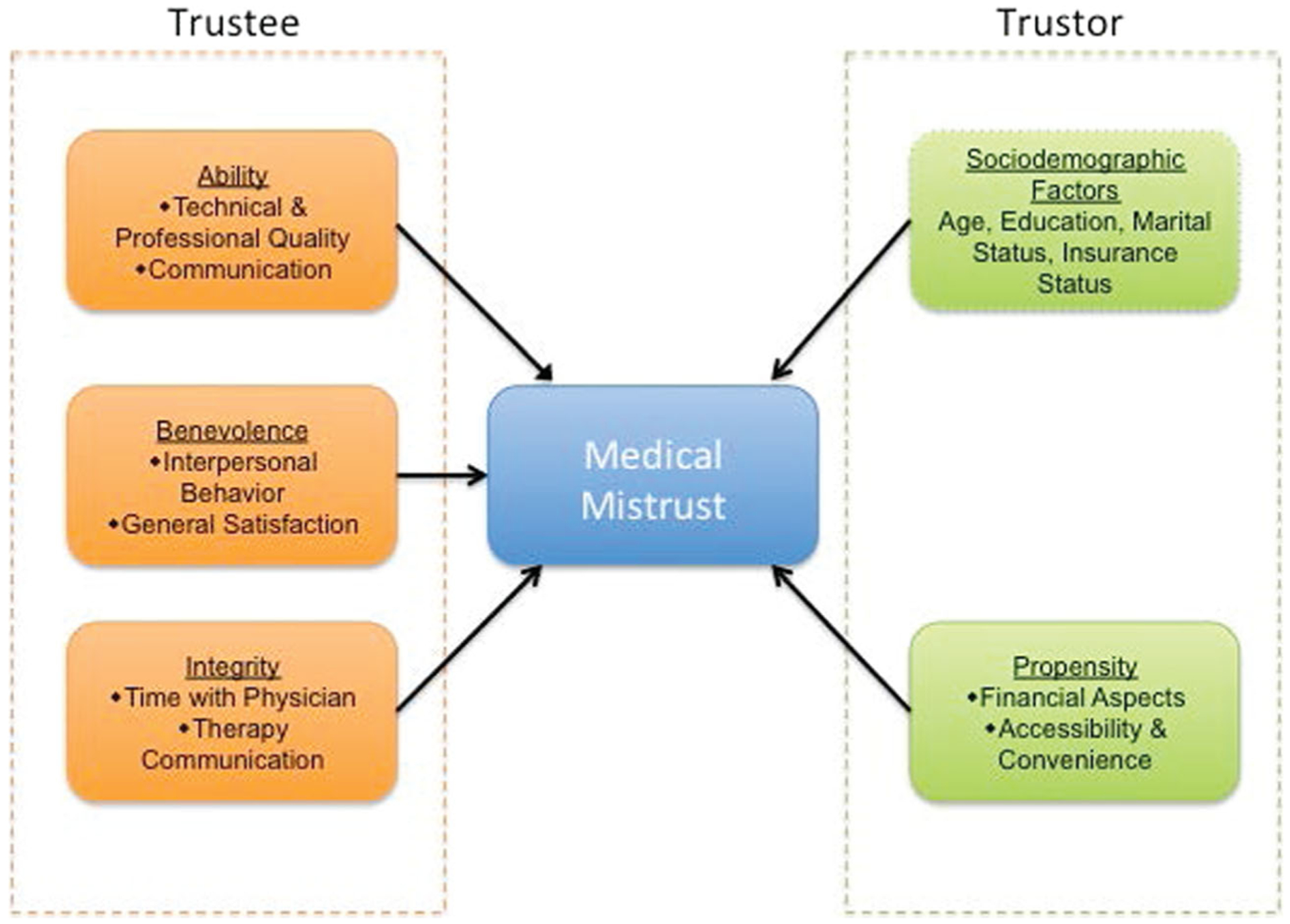
Conceptual model of medical mistrust in black breast cancer patients
While studies have examined factors associated with medical mistrust between races, few studies have identified attributing factors and predictors of mistrust within the Black cancer population [26, 27]. As medical mistrust has been shown to contribute to disparities experienced by Black breast cancer patients, focused inquiry is necessary to elucidate the roles of the trustor and the trustee. The goals of this investigation were to identify sociodemographic factors that contribute to group-based mistrust as reported by Black breast cancer patients and to assess the relationships between patient satisfaction, patient-provider communication, and group-based medical mistrust.
Methods
Settings and Population
This secondary analysis is of data from the “Narrowing the Gaps in Adjuvant Therapy” study, where investigators sought to reveal patient-reported factors and experiences related to various cancer treatment modalities (e.g., hormonal therapy, chemotherapy) [10]. Participants were recruited from two medical centers in Washington, DC, one in Detroit, MI, and via community outreach efforts. The Institutional Review Boards of all participating institutions approved the procedures and related materials for this study. Eligible participants were identified via pathology records at participating institutions. Eligibility criteria included self-identifying as Black/African-American or White/Caucasian, diagnosis of invasive, non-metastatic breast cancer and in the early stages of a treatment course (within 6 weeks post-surgery), indications for systemic adjuvant treatment, and ability to read and write in English. Participation required completion of one telephone survey. Additional details pertaining to methods outside the scope of this study are noted elsewhere [10]. Of the final sample of 359 women, Black women comprised 58.4% (n = 210) of the study sample. Notably, black women reported significantly greater medical mistrust than White women (p < 0.001) [10]. Therefore, the present analysis is restricted to the Black patients in the study.
Data Collection
Data were collected via trained interviewers via a telephone survey that lasted approximately 50 min. Participants received $25 for participating in the study. Clinical data were abstracted from medical records.
Measures
Group-Based Mistrust
Mistrust was measured using the Group-Based Medical Mistrust Scale, which consists of three subscales—suspicion (α = 0.78), perceived discrimination and group-based disparities in healthcare settings (α = 0.74), and lack of support (α = 0.013) [26]. Participants were to “Think about the relationship between various racial/ethnic groups and the American medical system and to rate how strongly they agreed or disagreed” with 12 5-point Likert-scale items (α = 0.55). Higher scores indicate more mistrust.
Sociodemographics
Sociodemographic factors included age, marital status, and education. Participants were also asked if they had health insurance; if they answered yes, they were asked to disclose the type of insurance (e.g., public, private, Medicare and private, other).
Communication
The Makoul [27] scale was adapted to assess patient’s ratings of overall communication and communication regarding chemotherapy (α = 0.83), hormonal therapy (α = 0.84), and radiation therapy (α = 0.87); higher scores represented higher levels of patient-provider communication.
Patient Satisfaction
Patient satisfaction was measured using the Patient Satisfaction Questionnaire Short Form (PSQ-18) [28]. Participants answered 18 Likert-scale items pertaining to their satisfaction with the medical care they received for the breast cancer across seven domains: (1) general satisfaction, (2) interpersonal behavior, (3) financial aspects, (4) technical and professional quality, (5) communication, (6) time with physicians, and (7) accessibility/convenience.
Data Analyses
Descriptive statistics, including the mean and frequencies, were analyzed for all variables. All two-tailed tests were assessed at a significance level of 0.05. F test for univariate analyses was used to assess the association between each independent variable and the continuous outcome variable, medical mistrust. Pearson correlation was reported between outcome variables and predictor variables. Stepwise analyses were applied in multiple linear regression models to select variables based on medical mistrust, suspicion, and perceived discrimination and group-based disparities in health care. The lack of support subscale was excluded from analysis due to its low reliability in this group of women. The statistical power for linear regression model was conducted through G*power (version 3.1). The power analyses showed that the powers for linear regression model with outcomes medical mistrust, suspicion, and perceived discrimination and disparities in healthcare were over 85%. All statistical analyses were performed using SAS version 9.4.
Results
Sample Characteristics
The sociodemographic characteristics for these women are presented in Table 1. The mean age for this group was54.1 years (SD = 12). Sixty-one percent of (n = 128) women were over the age of 50 and 64.8% who were single. With regard to education, there is an equal distribution of women with at least a high school education, some college, and a Bachelor’s degree or higher. While most women were not employed full time, a majority had private insurance. Overall feelings of medical mistrust for this group of women were relatively low (mean = 29.48). Bivariate analyses indicate significant relationships between medical mistrust and education (p = 0.029), employment status (p = 0.015), and insurance category (p = 0.005). Analysis also indicates significance with two process of healthcare factors—radiation therapy communication (p = 0.0047) and chemotherapy communication (p = 0.02). The total PSQ-18 score (p = 0.005) and one subscale, technical/professional quality (p = 0.0007), were also significantly related to women’s rating of mistrust. Significant associations were not found for overall communication, marital status, or age.
Table 1.
Study participant characteristics and predictors of medical mistrust (n = 210)
| Demographic characteristics | N (%) | Mean ± SD | p value | |
|---|---|---|---|---|
| Age (categorical) | ||||
| ≤ 50 | 210 | 82 (39.0) | 29.6 ± 4.2 | 0.74 |
| > 50 | 128 (61.0) | 29.4 ± 4.4 | ||
| Age (continuous) | 210 (100) | 54.1 ± 12.0 | 0.97 | |
| Marital status | ||||
| Married/living with partner | 210 | 74 (35.2) | 29.1 ± 3.6 | 0.3 |
| Currently single | 136 (64.8) | 29.7 ± 4.6 | ||
| Education level | ||||
| Bachelor’s and above | 210 | 71 (33.8) | 28.4 ± 4.3 | 0.029* |
| Some college | 74 (35.2) | 29.8 ± 3.7 | ||
| ≤ HS | 65 (31.0) | 30.3 ± 4.7 | ||
| Employment status | ||||
| Full-time employed | 190 | 64 (33.7) | 28.4 ± 4.3 | 0.015* |
| Not full-time employed | 126 (66.3) | 30.0 ± 4.2 | ||
| Insurance category | ||||
| Private only | 208 | 123 (59.1) | 28.9 ± 4.2 | 0.005** |
| Medicare and private | 30 (14.4) | 28.7 ± 5.0 | ||
| Public | 55 (26.5) | 31.1 ± 3.9 | ||
| Process of healthcare factors | ||||
| Communication subscales (total score) | ||||
| General communication | 208 | 11.8 ± 1.9 | 0.23 | |
| Hormonal therapy communication | 194 | 18.5 ± 2.8 | 0.051 | |
| Chemotherapy communication | 206 | 20.3 ± 2.7 | 0.02* | |
| Radiation therapy communication | 182 | 19.5 ± 2.8 | 0.0047** | |
| PSQ-18 Subscales (average score) | ||||
| General satisfaction | 210 | 2.8 ± 0.5 | 0.59 | |
| Communication | 210 | 2.8 ± 0.5 | 0.078 | |
| Technical/professional quality | 210 | 2.7 ± 0.4 | 0.0007** | |
| Interpersonal behavior | 209 | 2.9 ± 0.5 | 0.12 | |
| Financial aspects | 210 | 2.9 ± 0.5 | 0.49 | |
| Time spent with physician | 208 | 2.9 ± 0.5 | 0.18 | |
| Accessibility/convenience | 210 | 2.8 ± 0.4 | 0.58 | |
| Total PSQ-18 Satisfaction score | 210 | 50.6 ± 4.4 | 0.02* |
p < 0.05;
p < 0.01
Correlational analysis offers insight to the relationships between our outcome and independent variables (Table 2). As evident through the table, all communication factors and most PSQ-18 subscale items are inversely related to medical mistrust overall and to suspicion. While no communication factors were significantly correlated with perceived discrimination and group-based disparities in healthcare, interpersonal behavior (p < 0.01) was positively correlated, and financial aspects (p < 0.05) and time spent with physician (p < 0.05) were negatively correlated with that outcome.
Table 2.
Pearson correlation between outcome variables and predictors
| Variables | Medical mistrust | Suspicion | Lack of support | Group disparities in healthcare |
|---|---|---|---|---|
| Communication subscales | ||||
| General communication | −0.083 | −0.15* | −0.045 | 0.1 |
| Hormonal therapy communication | −0.14 | −0.22** | −0.091 | 0.13 |
| Chemotherapy communication | −0.16* | −0.22** | −0.15* | 0.13 |
| Radiation therapy communication | −0.21** | −0.24** | −0.12 | 0.06 |
| PSQ-18 Subscales (average score) | ||||
| General satisfaction | −0.038 | −0.019 | −0.11 | 0.039 |
| Communication | −0.122** | −0.12 | −0.13 | 0.048 |
| Technical/professional quality | −0.23*** | −0.19** | −0.13 | −0.049 |
| Interpersonal behavior | −0.11 | −0.24*** | −0.099 | 0.22** |
| Financial aspects | −0.048 | 0.031 | 0.051 | −0.17* |
| Time spent with physician | −0.094 | −0.05 | −0.1 | −0.023 |
| Accessibility/convenience | 0.039 | −0.011 | −0.0069 | 0.089 |
| Total PSQ-18 Satisfaction score | −0.16* | −0.17* | −0.13 | 0.04 |
p < 0.05;
p < 0.01;
p < 0.001
Multiple Linear Regression Analyses
Medical mistrust
Multiple regression analysis was employed to determine which variables (e.g., education, satisfaction) were significantly related to medical mistrust (Table 3). Medical mistrust was negatively related to possessing a private form of health insurance. When compared to women with “public insurance” women “private insurance only” reported less mistrust (p < 0.01). Regarding communication factors, greater mistrust was associated with lower ratings of radiation communication (p < 0.01). There was no significant relationship between total satisfaction and medical mistrust; however, results of the model indicated a significant and inverse relationship between satisfaction with technical and professional quality and medical mistrust (p < 0.001). Also, women who reported more satisfaction with accessibility/convenience reported greater medical mistrust (p < 0.05).
Table 3.
Multiple regression models (variable selection with estimates and 95% confidence interval)
| Variables | Model 1 Medical mistrust |
Model 2 Suspicion |
Model 3 Group disparities in healthcare |
|---|---|---|---|
| Insurance (Medicare and private vs. public) | −1.87 (−3.77, 0.031) | −1.55 (−2.96, −0.14)* | - |
| Insurance (private vs. public) | −1.90 (−3.25, −0.55)** | −1.44 (−2.44, −0.44)** | - |
| Radiation communication | −0.30 (−0.52, −0.084)** | - | - |
| Chemotherapy communication | - | −0.27 (−0.43, −0.11)** | - |
| Technical and professional quality | −2.54 (−3.95, −1.13)*** | −1.02 (−2.02, −0.02)* | - |
| Accessibility/convenience | 1.79 (0.065, 3.51)* | - | - |
| Interpersonal behavior | - | −1.52 (−2.48, −0.56)** | 1.1 (0.43, 1.77)** |
| Education (≤ HS vs. ≥ bachelors) | - | - | 1.50 (0.74, 2.26)*** |
| Education (any college vs. ≥ bachelors) | - | - | 1.26 (0.53, 1.99)** |
p < 0.05;
p < 0.01;
p < 0.001
Suspicion
Women with private insurance only (p < 0.05) and Medicare and private insurance (p < 0.01) were less suspicious than women with public insurance. Women with less satisfaction with the technical and professional quality of their medical professional (p < 0.05) and interpersonal behavior with providers (p < 0.01) were more suspicious of the medical establishment. Additionally, women who reported lower ratings of communication about their chemotherapy also reported greater suspicion (p < 0.01).
Perceived Discrimination and Group-Based Disparities in Healthcare
Women with a high school diploma or less (p < 0.001) and women with some college (p < 0.01) reported stronger feelings regarding perceived discrimination and group-based disparities in healthcare settings than women with at least a bachelor’s degree. Lastly, greater satisfaction with interpersonal behavior with providers was associated with greater perceived discrimination (p < 0.01).
Discussion
This is the first study, to our knowledge, that assessed the contributing roles of the trustor and the trustee towards medical mistrust in Black breast cancer patients. Findings from this study revealed three key points: (1) Modifiable factors related to mistrust predominantly occur within the context of the trustee, (2) assessing domains of medical mistrust provide targeted insight into Black women’s feelings of mistrust, and (3) inequities persist within social determinants of health (propensity, sociodemographics) and contribute to feelings of mistrust.
Feelings of mistrust towards the medical establishment continue to resonate throughout the Black community. These feelings were evident in our sample as ratings of mistrust ranged from low to high (14–47) although overall feelings of mistrust were relatively low (mean = 29.48). However, Black women diagnosed with breast cancer report feelings of mistrust that may be attributed to factors within the clinical setting. As many studies focus on racial differences with regard to medical mistrust, our study highlights contributing sociodemographic and process of healthcare factors related to Black women’s feelings of mistrust. Observing differences within this patient population reveals potential areas of further investigation into why these differences exist, how they may impact patient outcomes, and mechanisms for developing efficacious provider education curricula pertaining to medical mistrust.
Our work contributes to an existing body of literature that emphasizes the role of patient-provider communication within the context of clinical outcomes and perceptions of medical personnel [6, 20]. In this study, greater medical mistrust was found in women who reported lower ratings of provider communication. Specifically, communication regarding radiation and chemotherapy was significantly related to overall mistrust and suspicion, respectively. Other studies have reported similar findings [29, 30]. This finding suggests the need to develop effective communication strategies for providers who interact and treat Black breast cancer survivors. Notably, a study by White and colleagues suggests the need to examine health literacy in the context of mistrust and communication, as they found that among mistrustful individuals, those with high health literacy reported better ratings of provider communication than those with low health literacy [31]. Additional work in this area is warranted.
Interestingly, there was a significant relationship between accessibility to care and feelings of mistrust; women with greater satisfaction with accessibility to care also were more likely to be more mistrusting. This finding may suggest that access to care does not mitigate feelings of mistrust; additionally, mistrust may evolve from numerous health-related encounters and interactions. Further, qualitative research with black breast cancer patients may address the cause and effect relationship between satisfaction and medical mistrust.
There were other unexpected findings. Women in our study who reported greater satisfaction with their providers’ interpersonal behavior also had higher ratings of perceived discrimination and group-based disparities in healthcare settings. To our knowledge, no other studies have reported similar findings. However, Hagiwara et al. and Penner and colleagues found that Black cancer patients who reported greater perceived discrimination tended to interact or engage more with their physicians [32, 33]. A better understanding of the relationship between providers’ interpersonal manner and cancer patients’ reporting of perceived discrimination is needed in order to assess how the presence or absence of past discrimination may affect or dictate how individuals interact with their providers.
In our study, education was a significant contributor to women’s reporting of perceived discrimination and group-based disparities in the healthcare setting. Women with less education reported more feelings of perceived discrimination than women with more education. Similarly, a multi-center trial of post-surgical breast cancer patients found that women with less than a high school education were more likely to report feeling discriminated against than women who had at least a high school diploma [6]. Results from our study and findings from others suggest a need to investigate factors within individuals with less education that may be predictors of or cause feelings of perceived discrimination, specifically within the healthcare setting. Leveraging the knowledge and insight of patient navigators and/or community health workers may improve provider-patient relationships and interactions [34, 35]. This notion needs to be explored in the context of the patient’s level of education. Moreover, future studies that examine provider interactions with Black cancer patients with less education may inform methods to combat issues of discrimination.
The type of insurance one possessed emerged as a significant predictor of medical mistrust. In our study, women with public insurance coverage (e.g., Medicaid) reported greater mistrust and suspicion than women with private insurance and women with both private insurance and Medicare. Mistrust may prevent individuals of certain socioeconomic groups from seeking and receiving care, ultimately resulting in a contributing factor of health outcome disparities within these groups. There is a dearth of studies with similar findings. A qualitative study that examined perceptions of health among Black individuals in an urban setting noted that participants with public insurance felt that providers possessed negative preconceived notions about them because of their lack of private insurance, thus perpetuating feelings of mistrust [36]. Furthermore, it is common for individuals to possess a mistrust in the government and in physicians [37, 38]. This may explain why individuals with government-provided insurance reported greater feelings of mistrust. This finding presents a multi-faceted and complex concern regarding the perception of public insurance; however, given the potential impact of such feelings, we must consider multilevel approaches including educating patients and providers on interactions that may contribute to such perceptions. Moreover, policies that ensure equitable access to quality care (e.g., specialists) for those possessing public insurance may attenuate feelings of mistrust. Further investigation is warranted to examine and compare provider and patient views regarding insurance status and care.
Findings in this study further demonstrate the prevalence of mistrust in Black breast cancer patients and identify key contributing sociodemographic and healthcare factors. Strengths of this study include the intentional recruitment and oversampling of black women, allowing for between and within race comparisons rather than Black versus White comparisons that have already been cited in the literature. The sample size also allowed us to observe variations in demographic, clinical, and healthcare factors.
Despite the valuable findings and strengths, we must consider limitations of this study. Participants were recruited via convenience sampling; therefore, information is lacking for women who decided not to participate. Differences may exist between the women who chose to participate and those who did not. Next, since provider communication was one focus of this study, input from physicians may have provided additional insight into patient-provider interactions. Additionally, ratings of the trustee did not occur via self-report but were assessed by the trustor. This is also noted as a limitation of the theory [25]. Future studies should include the provider, or the trustee, to assess self-reported measures of provider domains. All women recruited to this study possessed health insurance; therefore, these findings are not generalizable to uninsured women. Although our Cronbach’s alpha for the total mistrust scale is acceptable, we recognize that the lack of support may have affected the overall reliability. There is limited evidence that suggests loading group-based mistrust items into two subscales instead of three [39]. Using this approach may have improved our reliability; however, validation studies are needed to verify this assumption, specifically within the context of Black breast cancer patients. Lastly, prior experiences unrelated to treatment and care for cancer (e.g., prior surgeries) may have influenced our participants’ responses. Therefore, the cross-sectional design of this study limited our ability to assess domains of at multiple points during and after the women’s treatment and care.
Conclusion
Contributing factors of the health disparities experienced by Black breast cancer patients are multifaceted. Medical mistrust may play a pivotal role within the spectrum of causal factors related to disparities (e.g., poorer outcomes, lack access to care) affecting Black women. This study provides an impetus to initiate dialog with trustors and trustees on the topic of medical mistrust. Strategies to improve interactions between providers and black cancer patients, specifically women of lower socioeconomic status, are needed. Further, additional efforts are necessary to gain a better understanding of (1) why Black women report higher mistrust than other races, (2) what modifiable factors contribute to mistrust, and (3) approaches and interventions that engage and educate providers on Black women’s feelings of medical mistrust methods to address mutable provider-level factors that may ease or diminish such feelings.
Acknowledgements
We would like to thank the women who agreed to participate in this study. Funding for this work was supported in part by the American Cancer Society (MRSGT-06-132-01 CPPB) and Virginia Commonwealth University Massey Cancer Center Shared Resource, supported, in part, with funding from NIH-NCI Cancer Center Support Grant P30 CA016059.
Footnotes
Conflict of Interest The authors have no conflicts of interest.
Ethical Approval All procedures performed involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable standards.
Informed Consent Informed consent was obtained from all individual participants included in the study.
References
- 1.Salma S-M, Smith Katherine C, Ann K, Hee-Soon J (2008) A healthy mistrust: how worldview relates to attitudes about breast cancer screening in a cross sectional survey of low-income women. Int J Equity Health 7(1):5 10.1186/1475-9276-7-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Glover L, Sims M, Winters K (2017) Perceived discrimination and reported trust and satisfaction in african americans: the Jackson heart study. Ethn Dis 27(3):209–216. 10.18865/ed.27.3.209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stevens EM, Patterson CA, Li YB, Smith-Whitley K, Barakat LP (2016) Mistrust of pediatric sickle cell disease clinical trials research. Am J Prev Med 51(1):S78–S86. 10.1016/j.amepre.2016.01.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheppard VB, Harper FWK, Davis K, Hirpa F, Makambi K (2014) The importance of contextual factors and age in association with anxiety and depression in black breast cancer patients. Psycho-Oncology 23(2):143–150. 10.1002/pon.3382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cuevas AG, O’Brien K, Saha S (2016) African American experiences in healthcare: “I always feel like I’m getting skipped over”. Health Psychol 35(9):987–995. 10.1037/hea0000368 [DOI] [PubMed] [Google Scholar]
- 6.Bickell NA, Weidmann J, Fei K, Lin JJ, Leventhal H (2009) Underuse of breast cancer adjuvant treatment: patient knowledge, beliefs, and medical mistrust. J Clin Oncol Off J Am Soc Clin Oncol 27(31):5160–5167. 10.1200/JCO.2009.22.9773 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sohler NL, Fitzpatrick LK, Lindsay RG, Anastos K, Cunningham CO (2007) Does patient-provider racial/ethnic concordance influence ratings of trust in people with HIV infection? AIDS Behav 11(6):884–896. 10.1007/s10461-007-9212-0 [DOI] [PubMed] [Google Scholar]
- 8.Sheppard V (2016) Reducing racial disparities in breast Cancer Survivors’ ratings of quality Cancer care: the enduring impact of trust. J Healthc Qual 38(3):143–163 [DOI] [PubMed] [Google Scholar]
- 9.Hershman D, Tsui J, Wright J, Coromilas E, Tsai W, Neugut A (2015) Household net worth, racial disparities, and hormonal therapy adherence among women with early stage breast cancer. J Clin Oncol Off J Am Soc Clin Oncol 33(1059):1053–1059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sheppard V, Isaacs B, Luta C, Willey G, Boisvert S, Harper C, …, Mandelblatt M (2013) Narrowing racial gaps in breast cancer chemotherapy initiation: the role of the patient–provider relationship. Breast Cancer Res Treat 139(1):207–216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dragun A, Huang B, Tucker T, Spanos W (2011) Disparities in the application of adjuvant radiotherapy after breast-conserving surgery for early stage breast cancer. Cancer 117(12):2590–2598 [DOI] [PubMed] [Google Scholar]
- 12.Royak-Schaler R, Pelser C, Langenberg P, Hayes J, Gardner L, Nesbitt K, …, Dwyer D (2012) Characteristics associated with the initiation of radiation therapy after breast-conserving surgery among African American and white women diagnosed with earlystage breast cancer in Maryland, 2000–2006. Ann Epidemiol 22(1): 28–36 [DOI] [PubMed] [Google Scholar]
- 13.Bustillo NE, Mcginty HL, Dahn JR, Yanez B, Antoni MH, Kava BR, Penedo FJ (2017) Fatalism, medical mistrust, and pretreatment health-related quality of life in ethnically diverse prostate cancer patients. Psycho-Oncology 26(3):323–329. 10.1002/pon.4030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kinlock BL, Parker LJ, Bowie JV, Howard DL, LaVeist TA, Thorpe RJ (2017) High levels of medical mistrust are associated with low quality of life among black and white men with prostate cancer. Cancer Control 24(1):72–77 [DOI] [PubMed] [Google Scholar]
- 15.O’Malley AS, Sheppard VB, Schwartz M, Mandelblatt J (2004) The role of trust in use of preventive services among low-income African-American women. San Diego, CA: 10.1016/j.ypmed.2004.01.018 [DOI] [PubMed] [Google Scholar]
- 16.White RO, Chakkalakal RJ, Presley CA, Bian A, Schildcrout JS, Wallston KA, …, Rothman R (2016) Perceptions of provider communication among vulnerable patients with diabetes: influences of medical mistrust and health literacy. J Health Commun 21:127–134. 10.1080/10810730.2016.1207116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Benkert R, Hollie B, Nordstrom CK, Wickson B, Bins-Emerick L (2009) Trust, mistrust, racial identity and patient satisfaction in urban African American primary care patients of nurse practitioners. J Nurs Scholarsh 41(2):211–219. 10.1111/j.15475069.2009.01273.x [DOI] [PubMed] [Google Scholar]
- 18.Smith SA, Blumenthal DS (2012) Community health workers support community based participatory research ethics: lessons learned along the research-to-practice-to community continuum. J Health Care Poor Underserved 23(4):77–87. 10.1353/hpu.2012.0156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gamble VN (1997) Under the shadow of Tuskegee: African Americans and healthcare. Am J Public Health 87(11):1773–1778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moore AD (2013) Increasing access to care and reducing mistrust: important considerations when implementing the patient- centered medical home in army health clinics. Mil Med 178(3):291–298. 10.7205/MILMED-D-12-00443 [DOI] [PubMed] [Google Scholar]
- 21.Brown ER (2012) African american present perceptions of organ donation: a pilot study. ABNF J 23(2):29–33 [PubMed] [Google Scholar]
- 22.James AB, Demmons DG, Schreiber GB, Hillyer CD, Shaz BH (2011) Contribution of attitudinal factors to blood donation in African American church attendees. Transfusion 51(1):158–165. 10.1111/j.1537-2995.2010.02775.x [DOI] [PubMed] [Google Scholar]
- 23.Armstrong TD, Crum LD, Rieger RH, Bennett TA, Edwards LJ (1999) Attitudes of African Americans toward participation in medical research. J Appl Soc Psychol 29(3):552–574. 10.1111/j.1559-1816.1999.tb01401.x [DOI] [Google Scholar]
- 24.Roberson NL (1994) Clinical trial participation: viewpoints from racial/ethnic groups. Cancer 74:2687–2691. 10.1002/1097-0142 [DOI] [PubMed] [Google Scholar]
- 25.Mayer RC, Davis JH, Schoorman FD (1995) An integrative model of organizational trust. Acad Manag Rev 20(3):709–734. 10.2307/258792 [DOI] [Google Scholar]
- 26.Thompson HS, Valdimarsdottir HB, Winkel G, Jandorf L, Redd W (2004) The group based medical mistrust scale: psychometric properties and association with breast cancer screening. Prevent Med 38(2):209–218 [DOI] [PubMed] [Google Scholar]
- 27.Makoul G, Arntson P, Schofield T (1995) Health promotion in primary care: physician-patient communication and decision making about prescription medications. Soc Sci Med 41:1241–1254 [DOI] [PubMed] [Google Scholar]
- 28.Moore AD, Hamilton JB, Knafl GJ, Godley PA, Carpenter WR, Bensen JT, …, Mishel M (2013) The influence of mistrust, racism, religious participation, and access to care on patient satisfaction for African American men: the North Carolina-Louisiana prostate cancer project. J Natl Med Assoc 105(1):59 10.1016/S00279684(15)30086-9, 68 [DOI] [PubMed] [Google Scholar]
- 29.Gordon H, Street R, Sharf B, Kelly P, Souchek J (2006) Racial differences in trust and lung cancer patients’ perceptions of physician communication. J Clin Oncol Off J Am Soc Clin Oncol 24(6): 904–909. 10.1200/JCO.2005.03.1955 [DOI] [PubMed] [Google Scholar]
- 30.Halbert CH, Armston K, Gandy OH, Shaker L (2006) Racial differences in trust in health care providers. Arch Intern Med 166(8): 896–901. 10.1001/archinte.166.8.896 [DOI] [PubMed] [Google Scholar]
- 31.White R, Chakkalakal R, Presley C, Bian A, Schildcrout J, Wallston K, Rothman R (2016) Perceptions of provider communication among vulnerable patients with diabetes: influences of medical mistrust and health literacy. J Health Commun 21:127–134. 10.1080/10810730.2016.1207116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hagiwara N, Dovidio JF, Eggly S, Penner LA (2016) The effects of racial attitudes on affect and engagement in racially discordant medical interactions between non Black physicians and Black patients. Group Process Intergroup Relat 19(4):509–527. 10.1177/1368430216641306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Penner H, Dovidio A, Hamel S, Eggly (2017) The impact of Black cancer patients’ race-related beliefs and attitudes on racially-discordant oncology interactions: a field study. Soc Sci Med 191: 99–108. 10.1016/j.socscimed.2017.08.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Molina Y, Kim S, Berrios N, Calhoun EA (2015) Medical mistrust and patient satisfaction with mammography: the mediating effects of perceived self-efficacy among navigated african american women. Health Expect 18(6):2941–2950. 10.1111/hex.12278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Natale-pereira A, Enard KR, Nevarez L, Jones LA (2011) The role of patient navigators in eliminating health disparities. Cancer 117: 3541–3550. 10.1002/cncr.26264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sachs D, Peltzer JN & McGee JL (2017) Perceptions of health among black adults living in a diverse urban community. Malden, MA: 10.1111/phn.12323 [DOI] [PubMed] [Google Scholar]
- 37.Corbie-Smith G, Thomas S, Williams M, Moody-Ayers S (1999) Attitudes and beliefs of African Americans toward participation in medical research. J Gen Intern Med 14(9):537–546. 10.1046/j.1525-1497.1999.07048.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Masi C, Gehlert M (2009) Perceptions of breast cancer treatment among african-american women and men: implications for interventions. J Gen Intern Med 24(3):408–414. 10.1007/s11606-008-0868-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Valera P, Boyas J, Bernal C, Chiongbian V, Chang Y & Shelton R (2016) A validation of the group-based medical mistrust scale in formerly incarcerated Black and Latino Men. Am J Men’s Health, 04 May 2016 10.1177/1557988316645152 [DOI] [PMC free article] [PubMed] [Google Scholar]


