Abstract
Background: Telemedicine holds great promise for changing healthcare delivery. While telemedicine has been used significantly in the direct-to-consumer setting, the use of telemedicine in a preventive primary care setting is not well studied.
Introduction: ClickWell Care (CWC) is the first known implementation of a technology-enabled primary care model. We wanted to quantify healthcare utilization of primary care by patient characteristics and modality of care delivery.
Materials and Methods: Our study population included those who completed a visit to a CWC clinic between January 1, 2015 and September 30, 2015. We compared patients based on utilization of CWCs in-person and virtual visits across the following domains: patient demographics, distance from clinic, responses to a Health Risk Assessment, and top 10 conditions treated.
Results: Thousand two hundred seven patients completed a visit with a CWC physician in 2015. Nearly three-quarters of our patients were ≤40 years and sex was significantly different (p = 0.015) between visit cohorts. The greatest representation of men (47%) was seen in the virtual-only cohort. Patients' proximity to the clinic was also significantly different across visit cohorts (p = 0.018) with 44% of in-person-only and 34% of virtual-only patients living within 5 miles of Stanford Hospital.
Discussion: We found men were more likely to engage in virtual-only care. Young patients are willing to accept virtual care although many prefer to complete an in-person visit first.
Conclusions: Our findings suggest that a “bricks-and-clicks” care model where telemedicine is supported by a brick-and-mortar location may be an effective way to leverage telemedicine to deliver primary care.
Keywords: telehealth, telemedicine, e-health, m-health
Introduction
Primary care has gained increasing attention across the United States as healthcare spending continues to climb.1–3 Public and private payors are looking for innovative new models to deliver comprehensive, easily accessible primary care, often through patient-centered medical home (PCMH) models.1,3–5 Evidence about the quality and cost of care of PCMHs is mixed, with some studies showing positive clinical results in high-risk or elderly populations but not in healthy young adult populations.6–8 As health systems move toward shared-risk population health-based models, it is increasingly important to find a way to engage young adults early in their healthcare journey to ensure long-term health of the population.
Telemedicine holds great promise for changing the way we care for both chronically ill and healthy patients.9 Direct-to-consumer (DTC) telemedicine has emerged as a convenient way for patients to access care. DTC telemedicine may be well suited to engaging younger populations as studies have demonstrated a higher use of such services by 18–45 year olds.10,11 It is still unclear, however, how to incorporate such technologies into routine primary care practice.
There are currently three models of primary care delivery, all aimed at providing outpatient clinical care.
(1) Traditional in-office primary care
Delivered during normal business hours, traditional primary care models or “brick-and-mortar practices” limit patients to in-person visits for all of their care.12 In these practices, care coordination/follow-up often occurs through unscheduled phone calls.
(2) Traditional primary care with limited technology integration
Some primary care clinics now integrate technologies such as email and phone visits but often limit them to return patients only. Virtual visits may be conducted within the patient's own primary care practice or through the use of a third party clinical service (often within the same health system) but in urgent situations patients are often unable to see their own provider.13–15
(3) Technology-centered care
Often delivered during both normal business hours and after hours, these telemedicine services allow patients to connect to a physician through email, phone, or video visits completed with a mobile device or web browser.16,17 These services are often episodic and address only urgent issues, not preventive primary care services.
Our group recently implemented a fourth model: technology-enabled, patient-centered care.
Stanford Medicine designed ClickWell Care (CWC) for its accountable care organization (ACO), which is limited to employees of Stanford University. This virtual primary care clinic, which has been described in detail previously18 is a “bricks-and-clicks” model that integrates primary preventive, chronic, and urgent care services with wellness coaching, all supported through technology. Each time a patient wishes to interact with CWC, they may choose how they would like to receive their care, whether in-person or through virtual means.
In this article, we describe healthcare service utilization by the CWC patient population to understand the integration of telemedicine into routine primary care. We do this by examining differences during the first year of the clinic's existence between CWC patients who completed in-person visits alone, both in-person and virtual visits, and virtual visits alone.
Materials and Methods
Patients
Inclusion criteria for patients enrolled in CWC included age ≥18 years; ability to speak, read, and write in English; and willingness to do phone and video visits. Exclusion criteria included hospitalization in the past year for any serious chronic medical condition such as uncontrolled diabetes or hypertension, coronary artery disease, stroke, or another serious medical issue as measured by a health risk assessment (HRA) administered to all new ACO members.
The HRA (Supplementary Data S1) was a tool created within the organization to segment patients into appropriate risk categories. These categories allowed us to recommend a primary care clinic based on health risk and preference. Those with a score of 0–4 were offered CWC; a score from 5 to 11 were offered traditional primary care; and scores >12 were offered Stanford Coordinated Care, a clinic for patients requiring a higher level of care coordination.
Our study cohort consisted of all patients who enrolled in CWC between January 1, 2015 and September 30, 2015, with follow-up extending from their time of enrollment through December 31, 2015. Patients who made no visits during the year were excluded from our analyses. E-mail exchanges were excluded from consideration as most were not templated email visits. Stanford Healthcare uses Epic systems for its electronic health record. This study was approved by the Institutional Review Board of Stanford University.
Providers
CWC has a team of physicians and wellness coaches who work together to provide patients with comprehensive primary care, delivered either in-person or virtually through e-mail, phone, or video visits. Wellness coaches are certified trainers with additional training in nutrition and mindfulness-based stress reduction. They work with patients to create physical activity plans, review dietary habits, and teach mindfulness and sleep hygiene. Visits with wellness coaches are conducted only through phone or video.
Outcomes
We characterized and compared patients based on how they utilized CWCs services. Visits were defined as scheduled in-person office or virtual (video or phone) appointments between a patient and physician. We classified patients who had at least one CWC visit into one of four mutually exclusive cohorts based on their visit history with a CWC physician: clinic only, virtual only, and for patients with mixed visit types, clinic first and virtual first.
Analysis
We summarized the number of completed visits of each type in a Venn diagram and the total number of visits across visit types using quartiles. We defined visit completion as any visit scheduled and completed with a physician that was documented in Epic. To compare patients across cohorts, we considered patient demographics (enrollment age, sex, race, and ethnicity), distance from the clinic (as geodesic distance in miles between patients' zip code geo-coordinates and our clinic), patient responses to the HRA, and top 10 conditions diagnosed or managed during CWC visits.
To identify the top 10 conditions, a list of all unique primary diagnosis codes for CWC patients was produced for each billed visit from January 1 through December 31, 2015. These codes were grouped and ranked based on their frequency. Diagnosis groups were defined from two resources: ICD-9 codes from the National Ambulatory Medical Care Survey (NAMCS) 2012 and the Medicare Chronic Conditions Warehouse definitions for chronic conditions and potentially disabling conditions.19–21 NAMCS includes diagnosis code groups for acute diagnoses and some chronic conditions, and Medicare defines diagnosis code groups for chronic conditions and potentially disabling conditions only. Using both resources encompasses a combination of acute and chronic conditions, encountered in the primary care setting.
Continuous variables (enrollment age, distance from the clinic, and HRA score) were categorized, and all factors were then tabulated and compared across the four visit categories via chi-square or Fisher's exact tests at the 0.05 alpha level. To ensure sufficient cell counts, we combined the highest two age categories (51–65 and 65+), and combined the three longest distances from the clinic into one category before applying the statistical tests. For HRA responses, we collapsed the five original levels into three by combining the two levels above the middle category into one and the two below the middle category into another. All statistical tests were performed at the 0.05 level of significance, and analyses were performed using R version 3.2.22,23
Results
A total of 1,207 enrolled CWC patients (60% female) completed an in-person, video, or phone visit with a CWC physician in 2015. Nearly three-quarters were ≤age 40 at time of enrollment; 1% were over age 65. The majority of patients (57%) lived within 10 miles of Stanford Hospital, with median 6.8 miles and interquartile range (IQR) (2.5–15.4) miles (Table 1).
Table 1.
Demographics of Patients Who Made a ClickWell Care Visit in 2015
| OVERALL | CLICKWELL CARE MD VISITS (N = 1,207a) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| IN-PERSON ONLY | SOME VIRTUAL | VIRTUAL ONLYb | |||||||||
| IN-PERSON FIRST | VIRTUAL FIRST | ||||||||||
| N | % | N | % | N | % | N | % | N | % | pc | |
| Total patients | 1,207 | 100. | 559 | 46.3 | 310 | 25.7 | 124 | 10.3 | 214 | 17.7 | |
| Number of visits (median, IQR) | 2 | 1–3 | 1 | 1–1 | 3 | 2–4 | 3 | 2–4 | 1 | 1–2 | |
| Enrollment age group (years) | |||||||||||
| 17–30 | 418 | 34.6 | 191 | 34.2 | 123 | 39.7 | 41 | 33.1 | 63 | 29.4 | 0.092 |
| 31–40 | 471 | 39.0 | 232 | 41.5 | 115 | 37.1 | 41 | 33.1 | 83 | 38.8 | |
| 41–50 | 182 | 15.1 | 81 | 14.5 | 42 | 13.5 | 21 | 16.9 | 38 | 17.8 | |
| 51–65 | 124 | 10.3 | 52 | 9.3 | 29 | 9.4 | 18 | 14.5 | 25 | 11.7 | |
| 65+ | 12 | 1.0 | 3 | 0.5 | 1 | 0.3 | 3 | 2.4 | 5 | 2.3 | |
| Sex | |||||||||||
| Female | 724 | 60.0 | 330 | 59.0 | 195 | 62.9 | 86 | 69.4 | 113 | 52.8 | 0.015 |
| Male | 483 | 40.0 | 229 | 41.0 | 115 | 37.1 | 38 | 30.6 | 101 | 47.2 | |
| Race | |||||||||||
| American Indian or Alaskan Native | 4 | 0.3 | 1 | 0.2 | 0 | 0 | 1 | 0.8 | 2 | 0.9 | 0.089 |
| Asian | 251 | 20.8 | 133 | 23.8 | 65 | 21.0 | 19 | 15.3 | 34 | 15.9 | |
| Black or African American | 30 | 2.5 | 12 | 2.1 | 11 | 3.5 | 5 | 4.0 | 2 | 0.9 | |
| Native Hawaiian or other Pacific Islander | 13 | 1.1 | 7 | 1.3 | 2 | 0.6 | 2 | 1.6 | 2 | 0.9 | |
| Whited | 578 | 47.9 | 259 | 46.3 | 152 | 49.0 | 56 | 45.2 | 111 | 51.9 | |
| Hispanic White | 29 | 2.4 | 14 | 2.5 | 6 | 1.9 | 5 | 4.0 | 4 | 1.9 | |
| Non-Hispanic White | 541 | 44.8 | 243 | 43.5 | 144 | 46.5 | 50 | 40.3 | 104 | 48.6 | |
| White, unspecified | 8 | 0.7 | 2 | 0.4 | 2 | 0.6 | 1 | 0.8 | 3 | 1.4 | |
| Other | 205 | 17.0 | 95 | 17.0 | 47 | 15.2 | 24 | 19.4 | 39 | 18.2 | |
| Patient refused/unknown | 126 | 10.4 | 52 | 9.3 | 33 | 10.6 | 17 | 13.7 | 24 | 11.2 | |
| Ethnicity | |||||||||||
| Hispanic/Latino | 117 | 9.7 | 58 | 10.4 | 27 | 8.7 | 15 | 12.1 | 17 | 7.9 | 0.503 |
| Non-Hispanic/Latino | 972 | 80.5 | 453 | 81.0 | 250 | 80.6 | 93 | 75.0 | 176 | 82.2 | |
| Patient refused/unknown | 118 | 9.8 | 48 | 8.6 | 33 | 10.6 | 16 | 12.9 | 21 | 9.8 | |
| Distance from clinicc | |||||||||||
| 0.7–5 miles | 479 | 39.7 | 243 | 43.5 | 116 | 37.4 | 47 | 37.9 | 73 | 34.1 | 0.018 |
| >5–10 miles | 214 | 17.7 | 109 | 19.5 | 55 | 17.7 | 12 | 9.7 | 38 | 17.8 | |
| >10–20 miles | 306 | 25.4 | 124 | 22.2 | 83 | 26.8 | 35 | 28.2 | 64 | 29.9 | |
| >20–40 miles | 173 | 14.3 | 70 | 12.5 | 48 | 15.5 | 24 | 19.4 | 31 | 14.5 | |
| >40–100 miles | 22 | 1.8 | 4 | 0.7 | 6 | 1.9 | 6 | 4.8 | 6 | 2.8 | |
| >100 miles | 13 | 1.1 | 9 | 1.6 | 2 | 0.6 | 0 | 0 | 2 | 0.9 | |
| Median | Q1, Q3 | Median | Q1, Q3 | Median | Q1, Q3 | Median | Q1, Q3 | Median | Q1, Q3 | ||
| Age at enrollment (years) | 33 | 29, 41 | 33 | 29, 40 | 33 | 28, 39 | 35 | 29, 44 | 40 | 32, 51 | |
| Distance from clinicc (miles) | 6.8 | 2.5, 15.4 | 6.1 | 2.5, 13.7 | 9.1 | 2.5, 16 | 10.6 | 2.9, 18.3 | 9.2 | 2.9, 16.9 | |
Fifty-four patients had a ClickWell Care record besides in-person, phone, or video encounters and are not represented in this table.
Virtual refers to phone or video encounters.
Obtained from chi-square tests for categorical covariates.
White race categorized using ethnicity data. Other races include too few Hispanics to be further categorized.
IQR, interquartile range.
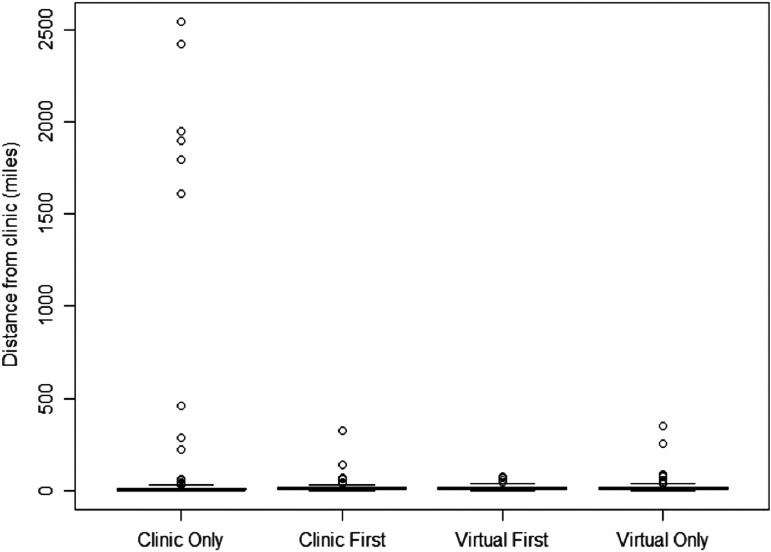
Categorical age was similarly distributed across visit cohorts with a median age of 33 for the in-person and some-virtual cohorts and median age of 40 for the virtual-only cohort. Patient sex, was significantly different (p = 0.015) across visit cohorts. The greatest representation of men (47%) was seen in the virtual-only cohort; men comprised 31%, 37%, and 41% of the virtual-first, clinic-first, and in-person-only cohorts, respectively. Patients' proximity to the clinic was also significantly different across visit cohorts (p = 0.018). The most striking difference was between the in-person-only and virtual-only patients, with 44% of the former group and 34% of the latter group living within 5 miles of Stanford Hospital. Box plots of distance from the clinic by visit group showed a lower median for in-person-only patients than for any other group (Fig. 1).
Fig. 1.
Distribution of distance from patient's home to the clinic. Distribution of geodesic distance from coordinates associated with residence zip codes to those associated with 94,304 for patients across four visit groups; inset figures are truncated at 100 miles for clearer view of boxplots.
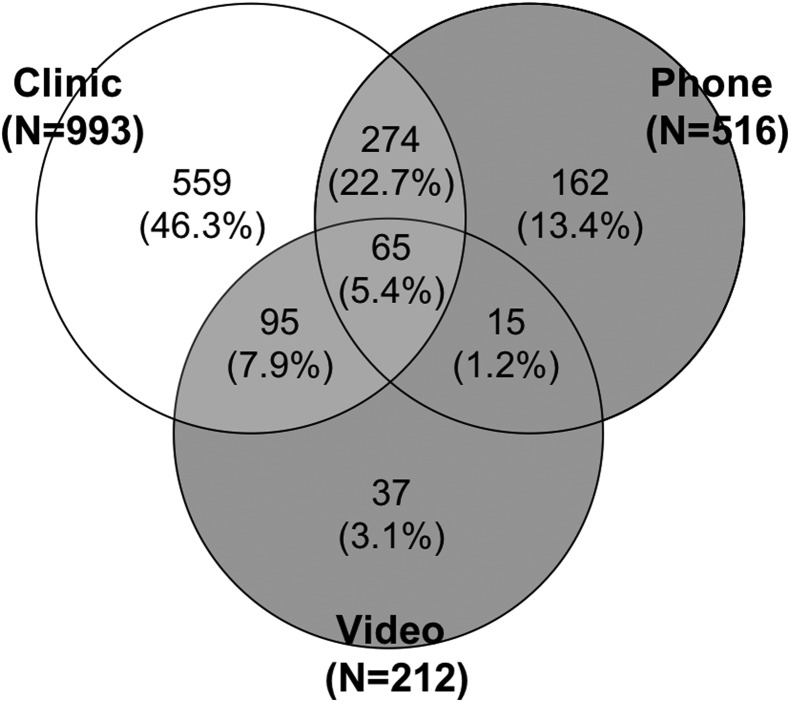
The 1,207 patients completed a total of 2,573 in-person, video, and phone visits with physicians in 2015. The median (IQR) number of completed visits per patient was 2 (1–3); the greatest number of visits was 17. The vast majority of patients (82.2%) who utilized CWC services had at least one in-person visit, followed by 42.7% with at least one phone visit and 17.5% with at least one video visit (Fig. 2). Five hundred fifty-nine (46.3%) patients received all of their care in-person compared with 449 (37.2%) who completed a mixture of virtual and in-person visits, and 199 (16.5%) who received all care virtually, 13.4% having only phone visits, and 3.1% having only video visits. Just over 5% of patients engaged in all three types of visits.
Fig. 2.
Segmentation of ClickWell Care Utilization by Visit Modality. Venn diagram depicting ClickWell Care utilization of 1,207 patients who completed at least one visit with a physician. Five hundred fifty-nine in-person-only patients are represented in the white region, 214 exclusively virtual (phone or video) patients are represented in the dark grey region, and 434 patients with both in-person and virtual visits are represented in the light grey region. VPC, virtual primary care.
Eighty percent of in-person-only patients and 66% of virtual-only patients completed just a single visit. The median (IQR) number of visits completed by those who had a mixture of virtual and in-person visits was 3 (2–4). Most patients (71%) who had a combination of in-person and virtual visits had an initial in-person visit.
According to the HRAs, patients perceived their health similarly across the visit cohorts (Table 2). The most prevalent response was “Very Good,” while <3% in each group rated their health as “Fair” or “Poor.” We observed no differences in categorized health risk scores. Among self-reported preferences for primary care delivery, the groups differed in preference patterns for in-person contact (p < 0.001) and video chat (p = 0.007). A greater percentage of in-person-only patients preferred in-person contact “Always” or “Very Frequently” than did virtual-only patients (33% vs. 22%), and a greater percentage of virtual-only patients preferred video chat “Always” or “Very Frequently” than did in-person-only patients (21% vs. 14%). Kappa statistics for consistency between self-reported preference of “Always” or “Frequently” for in-person or virtual visits and ever making a visit of the preferred type indicated slight agreement, according to Landis and Koch's23 interpretation.
Table 2.
Medical History of Patients Who Enrolled in ClickWell Care from January 1, 2015 to September 30, 2015
| OVERALL | IN-PERSON ONLY | SOME VIRTUALa | VIRTUAL ONLYa | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| IN-PERSON FIRST | VIRTUAL FIRST | ||||||||||
| N | %b | N | % | N | % | N | % | N | % | pc | |
| Total patients | 1,207 | 100. | 559 | 100. | 310 | 100. | 124 | 100. | 214 | 100. | |
| SHCA Health Risk Assessment survey items (n missing) | |||||||||||
| Self-perception of health (n = 130) | |||||||||||
| Excellent | 312 | 25.8 | 141 | 25.2 | 65 | 21 | 36 | 29 | 70 | 32.7 | 0.647 |
| Very good | 452 | 37.4 | 210 | 37.6 | 130 | 41.9 | 40 | 32.3 | 72 | 33.6 | |
| Good | 288 | 23.8 | 130 | 23.3 | 81 | 26.1 | 35 | 28.2 | 42 | 19.6 | |
| Fair | 23 | 1.9 | 12 | 2.1 | 5 | 1.6 | 3 | 2.4 | 3 | 1.4 | |
| Poor | 2 | 0.2 | 1 | 0.2 | 0 | 0 | 0 | 0 | 1 | 0.5 | |
| Preference for in-persond (n = 230) | |||||||||||
| Always | 134 | 11.1 | 69 | 12.3 | 41 | 13.2 | 8 | 6.5 | 16 | 7.5 | <0.001 |
| Very frequently | 241 | 20 | 118 | 21.1 | 69 | 22.3 | 23 | 18.5 | 31 | 14.5 | |
| Occasionally | 494 | 40.9 | 223 | 39.9 | 124 | 40.0 | 54 | 43.5 | 93 | 43.5 | |
| Rarely | 106 | 8.8 | 39 | 7.0 | 22 | 7.1 | 12 | 9.7 | 33 | 15.4 | |
| Never | 2 | 0.2 | 1 | 0.2 | 0 | 0 | 0 | 0 | 1 | 0.5 | |
| Preference for phone contacte (n = 225) | |||||||||||
| Always | 139 | 11.5 | 67 | 12 | 38 | 12.3 | 9 | 7.3 | 25 | 11.7 | 0.434 |
| Very frequently | 274 | 22.7 | 114 | 20.4 | 77 | 24.8 | 38 | 30.6 | 45 | 21 | |
| Occasionally | 455 | 37.7 | 216 | 38.6 | 113 | 36.5 | 45 | 36.3 | 81 | 37.9 | |
| Rarely | 97 | 8 | 50 | 8.9 | 21 | 6.8 | 5 | 4 | 21 | 9.8 | |
| Never | 17 | 1.4 | 6 | 1.1 | 7 | 2.3 | 1 | 0.8 | 3 | 1.4 | |
| Preference for video chate (n = 227) | |||||||||||
| Always | 59 | 4.9 | 23 | 4.1 | 18 | 5.8 | 5 | 4 | 13 | 6.1 | 0.007 |
| Very frequently | 145 | 12 | 55 | 9.8 | 37 | 11.9 | 22 | 17.7 | 31 | 14.5 | |
| Occasionally | 458 | 37.9 | 202 | 36.1 | 122 | 39.4 | 43 | 34.7 | 91 | 42.5 | |
| Rarely | 173 | 14.3 | 100 | 17.9 | 38 | 12.3 | 17 | 13.7 | 18 | 8.4 | |
| Never | 145 | 12 | 71 | 12.7 | 41 | 13.2 | 11 | 8.9 | 22 | 10.3 | |
| Preference for email contact (n = 226) | |||||||||||
| Always | 234 | 19.4 | 106 | 19 | 53 | 17.1 | 21 | 16.9 | 54 | 25.2 | 0.422 |
| Very frequently | 297 | 24.6 | 123 | 22 | 87 | 28.1 | 35 | 28.2 | 52 | 24.3 | |
| Occasionally | 385 | 31.9 | 190 | 34 | 100 | 32.3 | 38 | 30.6 | 57 | 26.6 | |
| Rarely | 46 | 3.8 | 27 | 4.8 | 7 | 2.3 | 4 | 3.2 | 8 | 3.7 | |
| Never | 19 | 1.6 | 6 | 1.1 | 9 | 2.9 | 1 | 0.8 | 3 | 1.4 | |
| Health Risk Score (n = 132) | |||||||||||
| 0 | 208 | 17.2 | 108 | 19.3 | 40 | 12.9 | 22 | 17.7 | 38 | 17.8 | 0.368 |
| 1–2 | 602 | 49.8 | 278 | 49.7 | 163 | 52.6 | 62 | 50.0 | 99 | 46.3 | |
| 3–4 | 214 | 17.7 | 85 | 15.2 | 64 | 20.6 | 24 | 19.4 | 41 | 19.2 | |
| 5+ | 51 | 4.2 | 22 | 3.9 | 14 | 4.5 | 5 | 4.0 | 10 | 4.7 | |
| Wellness coaching sessionsa | |||||||||||
| None | 967 | 80.1 | 475 | 85.0 | 226 | 72.9 | 97 | 78.2 | 169 | 79.0 | 0.003 |
| 1–2 sessions | 122 | 10.1 | 41 | 7.3 | 42 | 13.5 | 16 | 12.9 | 23 | 10.7 | |
| 3+ sessions | 118 | 9.8 | 43 | 7.7 | 42 | 13.5 | 11 | 8.9 | 22 | 10.3 | |
| Conditions ever diagnosed within VPC | |||||||||||
| General medical examination | 263 | 21.8 | 127 | 22.7 | 66 | 21.3 | 28 | 22.6 | 42 | 19.6 | 0.810 |
| Spinal disorders | 74 | 6.1 | 35 | 6.3 | 23 | 7.4 | 9 | 7.3 | 7 | 3.3 | 0.238 |
| Arthropathies and related disorders | 79 | 6.5 | 26 | 4.7 | 19 | 6.1 | 7 | 5.6 | 27 | 12.6 | 0.001 |
| Acute upper respiratory infections excluding pharyngitis | 80 | 6.6 | 39 | 7.0 | 21 | 6.8 | 7 | 5.6 | 13 | 6.1 | 0.936 |
| Rheumatism excluding back | 67 | 5.6 | 32 | 5.7 | 21 | 6.8 | 5 | 4.0 | 9 | 4.2 | 0.532 |
| Essential hypertension | 30 | 2.5 | 15 | 2.7 | 5 | 1.6 | 2 | 1.6 | 8 | 3.7 | 0.455 |
| Disorders of lipoid metabolism | 40 | 3.3 | 20 | 3.6 | 12 | 3.9 | 4 | 3.2 | 4 | 1.9 | 0.607 |
| Acquired hypothyroidism | 25 | 2.1 | 16 | 2.9 | 4 | 1.3 | 1 | 0.8 | 4 | 1.9 | 0.393 |
| Acute pharyngitis | 41 | 3.4 | 23 | 4.1 | 11 | 3.5 | 1 | 0.8 | 6 | 2.8 | 0.307 |
| Specific procedures and aftercare | 31 | 2.6 | 17 | 3.0 | 3 | 1.0 | 4 | 3.2 | 7 | 3.3 | 0.167 |
“Virtual” and “Wellness Coaching” are limited to phone and video encounters.
Some patients did not complete all parts of the HRA survey, so column percents may not sum to 100. The first nonmissing response for each item was tabulated for patients with multiple HRA entries.
P-values were obtained via chi-square tests or Fisher's exact tests (“self-perception of health” and the five bottom diagnoses). Five-level ordinal covariates were first collapsed into three levels by combining the two levels above and below the middle category.
Kappa of 0.052 for agreement between self-reported preference of “Always” or “Very Frequently” for in-person contact and ever making in-person visit.
Kappa of 0.054 for agreement between self-reported preference of “Always” or “Very Frequently” for phone contact or video chat and ever making virtual visit.
HRA, health risk assessment; VPC, virtual primary care.
We observed 722 unique ICD-9 primary diagnosis codes among patients with any encounter, and these were categorized into 38 diagnosis groups. The top 10 CWC conditions were general medical examination, spinal disorders, arthropathies and related disorders, acute upper respiratory infections (URIs) (excluding pharyngitis), rheumatism (excluding back), essential hypertension, disorders of lipid metabolism, acquired hypothyroidism, acute pharyngitis, and specific procedures and aftercare. Arthropathies and related disorders, which included arthritis, synovitis, joint derangement, and collagen disorders, was the only diagnosis group among the top 10 that was distributed differently across the four groups (p = 0.001): nearly 13% of virtual-only patients had received this diagnosis since their enrollment, more than double that of other groups.
Discussion
To our knowledge, this is the first study to examine the similarities and differences in a population that is offered both in-person and virtual primary care from a dedicated group of physicians. Previous studies have described only patients who participate in in-person or virtual care,11,17,24 and none has looked at a population that was allowed to choose whether they would receive care virtually or in-person, both for new and return visits, from the same group of physicians.
Our results suggest that CWC effectively engaged a younger subset of patients in primary care, as evidenced by the median age of 33–40 years in patients seeking care in the clinic. This is consistent with other studies demonstrating higher utilization of telemedicine by younger patients.11,17 This compares with an average age of 47.6 years among patients in traditional primary care clinics in our institution's local service area.25 Adding telemedicine to primary care may create a care model that better engages younger populations, which is important as shared risk models emerge since young patients often tend to use emergency and urgent care centers for their nonemergent needs.26–29 These avenues of acute care are often costly and do not engage patients in preventive care, leaving them vulnerable to developing chronic disease while increasing costs across the health system.29
We found statistically significant differences between cohorts in gender, distance between home and the clinic, preferences for types of visits, and diagnoses categorized as arthropathies compared with other diagnoses. Men were more likely than women to receive all of their care virtually. Numerous studies have documented a lower engagement in healthcare, especially preventive medicine, in men compared with women,30,31 despite the fact that life expectancy for men in the United States is 5 years shorter than women.32 Young men, aged 20–44 years, are more likely to avoid healthcare, not just visits to a doctor but also lower rates of visits to the pharmacy and dentist.33 Our findings suggest that virtual care may be a more effective method to engage and deliver care to young men.
As patients in our ACO are Stanford employees, it was not surprising that the majority of patients live within 5 miles of the clinic. We found patients who conducted most of their care in-person lived closer to the brick-and-mortar clinic. Patients who were more inclined toward virtual visits lived farther from the clinic. Despite this, a large proportion of patients who participated in virtual visits lived within 5 miles of the clinic, demonstrating that telemedicine is popular with patients who live close to healthcare and those who live farther from it.
Surveys have suggested a high acceptance of virtual visits among consumers, indicating that up to 72% of consumers would choose to see a doctor virtually34; one survey found that 50% of Gen Y respondents (18–36 years old) would switch doctors for one with better online access.35 However, many of these surveys asked participants to hypothetically choose based on a set of symptoms or specific illnesses and did not measure actual patient practice. Our findings suggest patients' preferences for how they would like to receive care correlate with how they actively get care. Patients with a higher preference for video visits were more likely to be part of the virtual-only cohort and those with a higher preference for in-person visits were more likely to be part of the in-person-only cohort.
Nevertheless, even those who indicated a high preference for virtual care often presented to the clinic in-person first. We suspect this preference for an initial visit in-person is due to a greater comfort level in building a primary care patient–physician relationship in-person compared with virtual care. It has been suggested that technology, which may reduce interpersonal risk during a patient–provider encounter, may consequently undermine the creation of a trusting and compassionate relationship36; it is possible that this notion is implicit, manifesting in our study as a large proportion of patients seeking in-person visits initially before proceeding with care virtually. Patients may see an initial in-person encounter as a supportive way to build a stronger patient–provider relationship.
Patients who engaged in virtual-only visits were significantly more likely to have visits for arthropathies and related disorders than patients who had clinic-only or some virtual visits. Traditionally, telemedicine services have been utilized most commonly for treating URIs including acute pharyngitis. In our clinical setting, however, URIs were seen in both in-person and virtual settings.
Of note, there was no statistically significant difference between patients who used in-person, virtual, or both visit types, when seeing a physician for a general medical or annual physical exam. This category includes both adult physicals and preventive care. This finding suggests some patients are willing to receive preventive health services though virtual care, rather than solely traditional in-person means.
Telemedicine has often been used to deliver urgent care,11,17 but our findings suggest its use should not be limited to urgent care alone. Some preventive care can be delivered virtually, including assessing a patient's risk factors and need for additional diagnostic screening and immunizations, without requiring an in-person physical examination. As Choosing Wisely guidelines37 do not recommend annual physical exams in healthy patients, telemedicine may offer patients a convenient opportunity to engage in preventive care and address health concerns.
Limitations
Our study has several limitations. First, there were a limited number of repeat visits. With the majority of patients completing only one visit in the clinic, it is difficult to assess whether the modality they chose for the one visit is truly how they will engage in healthcare in CWC longer term. This limitation will be addressed with further study within the CWC population. Second, these results may not be easily generalizable given our focused ACO population and our use of the HRA to limit the disease severity of our patients. The HRA also made it less likely for older patients to receive care through the clinic. Third, some diagnoses occur with higher prevalence in the CWC patient population compared to available NAMCS data and diagnosis groups. For example, urinary tract infection (UTI) as a single diagnosis code was not prevalent enough in CWC to make the top 10 diagnosis groups analyzed here; however, if grouped with other urinary symptoms, then UTI would be among the top 10 diagnosis groups. Finally, we were not able to compare this model to an external/existing model or to a traditional in-person primary care or urgent care-based telemedicine service.
Conclusions
Our study provides the first evaluation, to our knowledge, of the differences between patients who choose virtual versus in-person care. We found men were more likely to engage in virtual-only care and young patients are willing to accept virtual care, although many would prefer to complete an in-person visit first. Our findings suggest that a “bricks-and-clicks” model of care where telemedicine is supported by a brick-and-mortar location may be an effective way to leverage telemedicine to deliver primary care. Given the learnings achieved from this virtual care pilot, the decision was made to integrate the clinic into the rest of primary care to scale both the learnings and aspects of the model.
Supplementary Material
Acknowledgments
We are grateful to Stanford Translational Research Integrated Database Environment (STRIDE) for producing the data for this article. STRIDE is a research and development project38 at Stanford University to create a standards-based informatics platform supporting clinical and translational research. STRIDE was supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through grant UL1 RR025744. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. This study was supported by a Stanford Spectrum Learning Healthcare Innovation Challenge Grant.
Disclosure Statement
No competing financial interests exist.
Supplementary Material
References
- 1. Bodenheimer T, Pham HH. Primary Care: Current problems and proposed solutions. Health Aff (Millwood) 2010;29:799–805 [DOI] [PubMed] [Google Scholar]
- 2. Beaulieu D. How the ACA will transform primary care practices. Med Econ 2013;90:41–43 [PubMed] [Google Scholar]
- 3. Meyers D, Clancy CM. Primary Care: Too important to fail. Ann Intern Med 2009;150:272–273 [DOI] [PubMed] [Google Scholar]
- 4. Berenson RA, Rich EC. US approaches to physician payment: The deconstruction of primary care. J Gen Intern Med 2010;25:613–618 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. Joint Principles of the Patient-Centered Medical Home. 2007. Available at www.aafp.org/dam/AAFP/documents/practice_managementpcmh/initiatives/PCMHJoint.pdf (last accessed September27, 2016).
- 6. Fishman PA, Johnson EA, Coleman K, et al. . Impact on seniors of the patient-centered medical home: Evidence from a pilot study. Gerontologist 2012;52:703–711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Higgins S, Chawla R, Colombo C, Snyder R, Nigam S. Medical homes and cost and utilization among high-risk patients. Am J Manag Care 2014;20:e61–e71 [PubMed] [Google Scholar]
- 8. Paustian ML, Alexander JA, El Reda DK, Wise CG, Green LA, Fetters MD. Partial and incremental PCMH practice transformation: Implications for quality and costs. Health Serv Res 2014;49:52–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Daniel H, Sulmasy LS; for the Health and Public Policy Committee of the American College of Physicians. Policy recommendations to guide the use of telemedicine in primary care settings: An American College of Physicians position paper. Ann Intern Med 2015;163:787–789 [DOI] [PubMed] [Google Scholar]
- 10. Courneya PT, Palattao KJ, Gallagher JM. HealthPartners' online clinic for simple conditions delivers savings of $88 per episode and high patient approval. Health Aff (Millwood) 2013;32:385–392 [DOI] [PubMed] [Google Scholar]
- 11. Uscher-Pines L, Mulcahy A, Cowling D, Hunter G, Burns R, Mehrotra A. Access and quality of care in direct-to-consumer telemedicine. Telemed J E Health 2016 DOI: 10.1089/tmj.2015.0079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schoen C, Osborn R, Squires D, Doty MM. Access, affordability, and insurance complexity are often worse in the United States compared to ten other countries. Health Aff (Millwood) 2013;32:2205–2214 [DOI] [PubMed] [Google Scholar]
- 13. Pearl R. Kaiser Permanente Northern California: Current experiences with internet, mobile, and video technologies. Health Aff (Millwood) 2014;33:251–257 [DOI] [PubMed] [Google Scholar]
- 14. Shah MN, Morris D, Jones CMC, et al. . A qualitative evaluation of a telemedicine-enhanced emergency care program for older adults. J Am Geriatr Soc 2013;61:571–576 [DOI] [PubMed] [Google Scholar]
- 15. Rohrer JE, Angstman KB, Adamson SC, Bernard ME. Bachman JW, Morgan ME. Impact of online primary care visits on standard costs: A pilot study. Popul Health Manag 2010;13:59–63 [DOI] [PubMed] [Google Scholar]
- 16. DeJong C, Santa J, Dudley RA. Websites that offer care over the Internet: Is there an access quality tradeoff? JAMA 2014;311:1287–1288 [DOI] [PubMed] [Google Scholar]
- 17. Uscher-Pines L, Mehrotra A. Analysis of Teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Aff (Millwood) 2014;33:258–264 [DOI] [PubMed] [Google Scholar]
- 18. Cheung L, Norden J, Harrington RA, Desai SA. New delivery model for rising risk patients: The forgotten lot? Telemed J E Health 2017;23:649–653 [DOI] [PubMed] [Google Scholar]
- 19. NAMCS 2012 Survey Data on outpatient visits. Available at www.cdc.gov/nchs/data/ahcd/namcs_summary/2012_namcs_web_tables.pdf (Table 16) (last accessed January25, 2018)
- 20. Medicare Chronic Conditions Data Warehouse. Available at www.ccwdata.org/web/guest/condition-categories (last accessed January25, 2018)
- 21. CCW Chronic Conditions. Available at www.ccwdata.org/cs/groups/public/documents/document/ccw_chronic_cond_algos.pdf Other Chronic or Potentially Disabling Conditions. Available at www.ccwdata.org/cs/groups/public/documents/document/other_cond_algos_consolidated.pdf (last accessed January25, 2018)
- 22. R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2015. Available at www.R-project.org (last accessed January25, 2018). [Google Scholar]
- 23. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–174 [PubMed] [Google Scholar]
- 24. Schoenfeld AJ, Davies JM, Marafino B, et al. . Variation in quality of urgent health care provided during commercial virtual visits. JAMA Intern Med DOI: 10.1001/jamainternmed.2015.8248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chung S, Eaton LJ, Luft HS. Standardizing primary care physician panels: Is age and sex good enough? Am J Manag Care 2012;18:e262–e268 [PubMed] [Google Scholar]
- 26. Villani J, Mortensen K. Having a usual source of care reduces ED visits. J Am Board Fam Med 2013;26:680–691 [DOI] [PubMed] [Google Scholar]
- 27. Garcia TC, Bernstein AB, Bush MA. Emergency department visitors and visits: Who used the emergency room in 2007? NCHS Data Brief 2010;38:1–8 [PubMed] [Google Scholar]
- 28. Guttman N, Zimmerman DR, Nelson MS. The many faces of access: Reasons for medically nonurgent emergency department visits. J Health Polit Policy Law 2003;28:1089–1120 [DOI] [PubMed] [Google Scholar]
- 29. Maciosek MV, Coffield AB, Flottemesch TJ, Edwards NM, Solberg LI. Greater use of preventive services in U.S. health care could save lives at little or no cost. Health Aff (Millwood) 2010;29:1656–1660 [DOI] [PubMed] [Google Scholar]
- 30. Courtenay WH. Constructions of masculinity and their influence on men's well-being: A theory of gender and health. Soc Sci Med 2000;50:1385–1401 [DOI] [PubMed] [Google Scholar]
- 31. Williams D. The health of men; structure inequalities and opportunities. Am J Pub Health 2003;93:724–731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Arias E. United States Life Tables, 2011. Natl Vital Stat Rep 2015;64:1–63 [PubMed] [Google Scholar]
- 33. Hippisley-Cox J, Vinogradova Y. Trends in consultation rates in general practice 1995/1996-2008/2009: Analysis of the QResearch® database. NHS Health and Social Care Information Centre, 2009 [Google Scholar]
- 34. The Advisory Board Company. Prepare for the adoption of virtual visits for Primary Care. 2015 [Google Scholar]
- 35. Intuit Health Survey. Americans worried about costs; want greater access to physicians. 2011. Available at www.fiercehealthcare.com/press-releases/intuit-health-survey-americans-worried-about-costs-want-greater-access-phys-0 (last accessed January25, 2018).
- 36. Bauer K. Cybermedicine and the moral integrity of the physician-patient relationship. Ethics Inf Technol 2004;6:83–91 [Google Scholar]
- 37. Society of General Internal Medicine. Don't perform routine general health checks for asymptomatic adults. Choosing Wisely Campaign. 2013 [Google Scholar]
- 38. Lowe HJ, Ferris TA, Hernandez PM, Weber SC. STRIDE–An Integrated Standards-Based Translational Research Informatics Platform. AMIA Annu Symp Proc. 2009;39:1–5 [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.