Abstract
Background: We designed two telemonitoring text and voice messaging interventions, EpxDecolonization (EpxDecol) and EpxWound, to improve management of orthopedic joint replacement patients at Washington University. We reviewed the use of these tools for a period of 88 weeks.
Methods: Cohorts of 1,392 and 1,753 participants completed EpxDecol and EpxWound, respectively. All patients who completed EpxDecol also completed EpxWound. We assessed patient use of and satisfaction with these interventions. A return on investment (ROI) analysis was conducted to determine the cost savings generated by EpxWound and EpxDecol.
Results: The proportions of patients who responded daily to EpxDecol and EpxWound were 91.9% and 77.7%, respectively, over the lengths of each intervention. The percent of daily responders declined <5% during each intervention. Ultimately, 88.4% of EpxDecol patients and 67.8% of EpxWound patients responded to ≥80% of all messages. Median patient survey responses (n = 1,246) were 9/9 (best possible) for care, 8/9 for improved communication, and 5/9 (perfect number) for number of messages received. ROI analysis for this 88-week period showed that using EpxDecol and EpxWound to engage patients (instead of nurses calling patients) saved the equivalent of 2.275 full-time nursing equivalents per week. We calculated net savings of $260,348 with an ROI of 14.85x for 1,753 patients over 88 weeks. One-year cost savings from these interventions were $153,800 with an ROI of 14.79x.
Conclusions: EpxDecol and EpxWound may serve important roles in the perioperative process for orthopedic joint reconstruction surgery given high patient usage of and satisfaction with these interventions. Implementing EpxDecol and EpxWound for a large patient population could yield substantial cost savings and ROI.
Keywords: e-health, telesurgery, telemedicine, telecommunications, telenursing
Introduction
Surgical site infections (SSIs) are the most frequent and costly hospital-acquired infection and may yield additional annual healthcare costs of $3.5–10 billion.1,2 SSIs prove especially problematic in orthopedic patients.3 By 2020, there will be a predicted 70,000 total hip and knee arthroplasty SSIs requiring additional treatment, with an associated annual cost of $1.62 billion.4
To supplement postoperative measures designed to reduce SSIs, many healthcare providers now use a preoperative decolonization protocol for patients undergoing elective surgery. Most protocols attempt to decolonize Staphylococcus aureus with a combination of daily chlorohexidine gluconate skin cleanser and intranasal mupirocin, which has been shown to diminish SSIs due to S. aureus in patients undergoing total joint replacement.3,5 Unfortunately, complete adherence to these protocols may be infrequent, potentially as low as 31.1%.6 Short message service (SMS) text message reminders have proven useful for increasing medication adherence for diabetic patients7 and dialysis adherence for chronic hemodialysis patients.8 Meta-analysis has found that mobile interventions may increase medication adherence by 22%.9 These data suggest that a preoperative automated messaging platform with daily reminders could address patient adherence challenges and improve decolonization rates.
Moreover, automated messaging interventions could address postoperative complications, particularly for SSIs. Surveys of surgery patients at time of discharge reveal concerns about wound care, monitoring of postoperative complications, and patients' ability to contact healthcare providers should problems occur.10,11 Patients also believe that mobile interventions could address postdischarge challenges by allowing for more frequent, thorough, and convenient follow-up.11 Using automated telemedicine interventions to solicit patient-reported information has been shown to improve management of hemoglobin A1c in diabetic patients.12 However, SMS or phone call platforms have not been used as often for SSI reduction.13
To address these inadequacies, we developed two automated messaging systems named “EpxDecolonization” (EpxDecol) and “EpxWound” for the Orthopedic Adult Joint Reconstruction Service at Barnes-Jewish Hospital in St. Louis, MO. EpxDecol was developed in concordance with the decolonization protocol already in place at Barnes-Jewish, and EpxWound was developed to improve postoperative monitoring of pain and symptoms suggestive of a potential SSI. The infrastructure for EpxDecol and EpxWound was provided by Epharmix, a startup company located in St. Louis. This study was an expansion of a prior pilot trial for EpxDecol and EpxWound.14 We investigated the usability of and patient satisfaction with EpxDecol and EpxWound for an 88-week period. Furthermore, we determined the return on investment (ROI) generated on using these automated systems in place of manual nurse follow-up with patients by phone call.
Methods
Patient Enrollment
Patient enrollment in EpxDecol and EpxWound was classified as a clinical pilot, not a quality improvement research study, by the Washington University School of Medicine Institutional Review Board. The pilot trial spanned from November 29, 2015 to September 3, 2016 (40 weeks) and included about 650 patients.14 The pilot trial was subsequently expanded, and the data for this article were collected between November 29, 2015 and August 7, 2017. Patients undergoing a hip or knee replacement at Barnes-Jewish Hospital were offered the choice to enroll in Epharmix and consented to the use of these interventions alongside usual standard of care. Patients were excluded if they did not speak English or did not have access to a phone (any phone, including a landline or nonsmartphone). Participants elected to receive messages from EpxDecol, EpxWound, or both. They chose a preferred mode of contact (either phone call or SMS text messaging) and the time of day at which they received messages. Patients could drop out of each intervention by replying “stop” to the system at any point.
Intervention Design
Figure 1 depicts the message algorithm for EpxDecol. Starting 6 days before surgery, EpxDecol asked patients if they had picked up their prescribed decolonization supplies (mupirocin nasal ointment and chlorhexidine gluconate cleanser) from the pharmacy (day 0). If the patient had not received their supplies 5 days before surgery, an alert was sent to the nurse in charge of their care. Beginning 5 days before surgery, those patients who had picked up their supplies were asked daily if they had used their decolonization supplies as specified by their physician (days 1–5). Two separate messages were sent—one asking about the nasal ointment and another about the chlorhexidine cleanser. All responses could be monitored by a member of the medical team. An alert was not generated if a patient did not use their decolonization supplies.
Fig. 1.
Message algorithms for EpxDecol and EpxWound (courtesy of Epharmix). For EpxDecol, two separate messages were sent for the 5 days before surgery: one asking about use of the nasal ointment and another about the chlorhexidine cleanser. EpxDecol, EpxDecolonization.
Figure 1 also depicts the message algorithm for EpxWound. EpxWound was designed to identify SSIs in the time frame between the patient's discharge and their 2-week follow-up appointment by tracking pain and wound symptoms. This intervention sent daily automated messages consecutively from postoperative day (POD) 5 to POD 19. Patients were asked daily about their postoperative pain, wound status (increased redness, drainage, or odor), and body temperature. An alert was sent to the nurse in charge of a patient's care if that patient reported increased redness, drainage, or odor; a fever ≥101°F; or significant pain. If a patient generated an alert while using either EpxDecol or EpxWound, their nurse received an e-mail notifying the nurse to follow-up with that patient. An alert notification was also created in the Epharmix portal. After an alert, the medical team contacted the patient through phone call within 2 h (if during business hours) or the following morning (if after hours).
Two weeks after using both interventions, an automated electronic survey using a 1–9 response scale was delivered to collect patients' opinions on their care (1 = terrible, 5 = average, and 9 = excellent), the number of messages they received (1 = too few, 5 = perfect amount, and 9 = too many), and whether they felt that our interventions improved communication with their doctors (1 = significantly worsened, 5 = no change, and 9 = significantly improved). Only fully completed survey responses were analyzed.
Data and Statistical Analysis
The primary outcome was daily response rates for each automated system. Secondary outcomes were patient satisfaction with the interventions, the number of alerts generated by each intervention, and an ROI calculation. A daily response rate was calculated for each patient during the months of November 2015 to August 2017 and was defined as a response to at least one message during that day. For the automated survey results, the medians, means, and standard deviations (SDs) for participants' assessed scores were calculated in Microsoft Excel (Redmond, WA).
ROI Calculations
An ROI calculation (Table 1) was conducted to determine the cost savings and ROI produced by EpxDecol and EpxWound for our 88-week period and for 1 year. ROI was based on the estimated average time required to manually call each patient for EpxDecol and EpxWound in lieu of automated messages. We conservatively estimated that each EpxDecol phone call would take 10 min and each EpxWound phone call would take 15 min. These estimates were based on nurses' evaluations of how long a call would have to be to obtain patient answers to every question posed by EpxDecol and EpxWound. We calculated how many full-time nursing equivalents (FTEs) were saved using Epharmix by determining how much time would be spent on making calls for each intervention in 1 week. One FTE was defined as one nurse working a 40-h week. Weekly time spent on EpxDecol and EpxWound equaled 60 and 225 min per patient, respectively, multiplied by the average number of patients enrolled per week for each intervention. The weekly times for EpxDecol and EpxWound were summed and divided by 40 h to yield the FTE saved. The Price Per FTE was the cost of hiring a nurse to work for a certain number of weeks. For this calculation we used $1,388 for a nurse's weekly wage, based on the average annual American nursing salary of $72,180.15 There is a $10 per month cost to enroll a patient in any number of Epharmix interventions (i.e., in EpxDecol, EpxWound, or both). To calculate Total Cost Savings, we multiplied the Price per FTE by the number of FTE saved and then subtracted the cost of enrolling every patient in Epharmix for a given time period. ROI equaled Total Cost Savings divided by the cost of enrolling all patients in Epharmix over that time period.
Table 1.
Equations for Return on Investment Analysis
| EpxDecol = (6 calls/patient) × (10 min/call) = 60 min/patient |
| EpxWound = (15 calls/patient) × (15 min/call) = 225 min/patient |
| Weekly time per intervention |
| EpxDecol = (60 min/patient) × (average No. of patients enrolled/week) |
| EpxWound = (225 min/patient) × (average No. of patients enrolled/week) |
| FTE saved = (EpxDecol weekly time + EpxWound weekly time)/(40 h/week) |
| Price per FTE = (nurse weekly wage) × (time period in weeks) |
| Total cost savings = (price per FTE × FTE saved) − $10(total No. of patients enrolled in a given time period) |
| ROI = total cost savings/$10(total patients enrolled in a given time period) |
EpxDecol, EpxDecolonization; FTE, full time nursing equivalent; ROI, return on investment.
Results
Patient Overview
In total over the 88-week period, 1,392 patients were enrolled in EpxDecol, and 1,753 patients were enrolled in EpxWound. On average, 16 patients were enrolled per week in EpxDecol and 20 per week in EpxWound. For EpxDecol, 1,070 patients (77%, 1,070/1,392) elected to receive text messages, while 322 (23%, 322/1,392) chose phone calls. For EpxWound, 1,302 patients (74%, 1,302/1,753) received text messages, and 451 (26%, 451/1,753) chose phone calls. Ultimately, 28 patients (2%, 28/1,392) and 68 patients (3.9%, 68/1,753) dropped out of EpxDecol and EpxWound, respectively, over the course of each intervention. EpxDecol saw the highest dropout rate (eight patients, 0.58%, 8/1,382) on day 2; EpxWound had the highest dropout rate (16 patients, 0.91%, 16/1,753) on day 0 (POD 5).
The average SSI rates for the Washington University Orthopedic Surgery Department over this period were 0.31% and 0.47% for primary hip and knee surgeries, respectively. The department averaged 25 hip or knee replacements per week. Given constraints as a clinical pilot, both the enrollment percentage for EpxDecol and EpxWound during this study and the number of patients who underwent knee replacement versus hip replacement were unobtainable. About 99% of patients elected to receive their messages at 6 PM.
Response Proportions
The proportion of EpxDecol messages to which patients responded at least once per day was 91.9% (7,600 responses/8,266 total messages). The proportion of daily responders declined less than 5% over the course of the intervention, with a high of 94.2% on day 0 (1,312/1,392) and a low of 90.3% (1,232/1,364) on day 5 (Fig. 2). Ultimately, 1,230 patients (88.4%, 1,230/1,392) responded to at least 80% of all EpxDecol sessions, while 1,097 (78.8%, 1,097/1,392) responded to 90–100% of all sessions (Fig. 3). The proportion of patients responding to questions about using the nasal ointment was 91.9% (7,600 responses/8,266 total messages) compared to 87.5% (7,230 responses/8,266 total messages) for the questions regarding use of the chlorhexidine cleanser. Concerning self-reported decolonization protocol adherence, 89.5% (1,115/1,246) of patients applied their nasal ointment as instructed on day 1, and 76% (947/1,246) used their nasal ointment every day for days 1–5. For the chlorhexidine cleanser, 67% (820/1,222) used their cleanser as instructed on day 1 and 50.8% (621/1,222) used it every day for days 1–5. These EpxDecol adherence values were calculated using only patients who reported that they had picked up their decolonization supplies from the pharmacy.
Fig. 2.
Average proportion of patients who responded on each day of the intervention over the 88-week period.
Fig. 3.
Distribution of percentage of sessions answered by patients.
For EpxWound, the proportion of messages to which patients responded was 77.7% (19,914 responses/25,642 total messages). Daily responses to EpxWound declined <7% at any point during the intervention. The highest daily response proportion was 80.7% (1,414/1,753) on day 0 (POD 5) and the lowest was 74.4% (1,257/1,689) on day 13 (POD 18) (Fig. 2). The response proportion on day 14 (POD 19) was 76.8% (1,295/1,685). When broken down by week, the average proportions of responses for EpxWound were 79% (9,542/12,074) for week 1 and 76.4% (10,372/13,568) for week 2. Overall, 1,189 patients (67.8%, 1,189/1,753) responded to at least 80% of all EpxWound sessions and 908 patients (51.8%, 908/1,753) responded to 90–100% of all sessions (Fig. 3).
Alerts
There were 8,266 total EpxDecol messages sent during the 88-week period. Seventy-five alerts were generated among all EpxDecol patients, resulting in an alert rate of 5.4% (75/1,392). Of these, 53 alerts (70.7%, 53/75) were generated on day 0. All alerts corresponded to patients replying “No” to the questions regarding the acquisition of their medications from the pharmacy.
A total of 25,642 messages were sent for EpxWound. In all, 128 alerts were generated among all EpxWound patients, resulting in an alert rate of 7.3% (128/1,753). Twenty-eight alerts were generated by patients calling their physician's office and were not included in our analysis, leaving a patient-generated alert rate of 5.7% (100/1,753) (Fig. 4). The majority of alerts (n = 51, 51%) came from days 0 to 4 (POD 5–9). The highest number of alerts was generated on day 2 (POD 7, n = 14, 14%, 14/100) and day 5 (POD 10, n = 11, 11%, 11/100). Ninety-one of the 100 alerts (91%) were generated by patients who reported increased pain, and 9 alerts (9%) were generated by patients who claimed signs of wound degeneration (increased drainage, redness, or odor with or without an accompanying fever).
Fig. 4.
The percentage of EpxWound alerts generated per day.
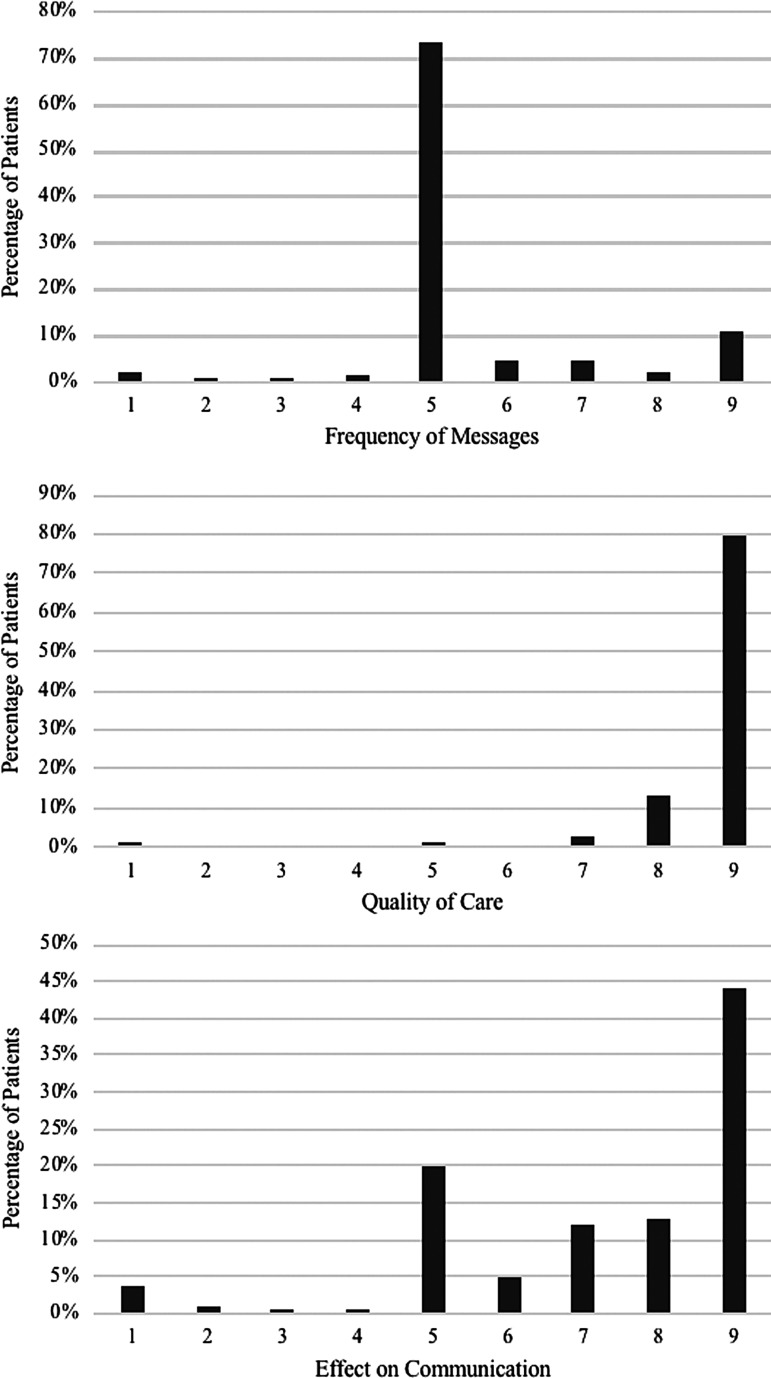
Satisfaction with the Interventions
A cohort of 1,246 patients completed postintervention surveys. The median response for how patients rated the care they received was 9/9 (the best possible score), and the mean response was 8.6 (SD = 1.2) (Fig. 5). There was a median score of 8/9 with respect to how Epharmix improved communication with physicians, with a mean response of 7.2 (SD = 2.1). The median score for the number of messages received during each intervention was 5/9 (the best possible score, with 0 = too few messages and 9 = too many messages) with a mean of 5.5 (SD = 1.5). Due to IRB constraints as a pilot study, it was not possible to formally survey nurses to quantify their satisfaction with our automated systems. Anecdotally, EpxDecol and EpxWound were appreciated by nurses as a way to improve and streamline patient care.
Fig. 5.
Patient satisfaction with EpxDecol and EpxWound. On a scale of 1–9, patients rated their care provided by their medical care team (1 = terrible, 5 = average, and 9 = excellent), whether EpxDecol and EpxWound improved communication with their doctor (1 = significantly worsened, 5 = no change, and 9 = significantly improved), and their satisfaction with the number of messages that they received (1 = too few, 5 = perfect amount, and 9 = too many).
Return on Investment
ROI results can be seen in Table 2. Without the benefit of an automated messaging system, a nurse would be expected on average to spend 60 min for EpxDecol and 225 min for EpxWound per patient. Given mean enrollment of 16 patients per week for EpxDecol and 20 patients per week for EpxWound, this would result in 91 h of phone calls or 2.275 FTE. Assuming an annual nursing salary of $72,180 and subtracting the $17,530 that it would cost to enroll 1,753 patients in Epharmix, we found that use of EpxDecol and EpxWound to contact patients saved the Orthopedic Surgery Department $260,363 over the course of our 88-week time period. This corresponded to an ROI of 14.85x (1,485%). On an annual basis, based on 1,040 enrolled patients (20 patients/week for 52 weeks), cost savings were $153,800, and the ROI was 14.79x (1,479%).
Table 2.
Return on Investment Calculations for EpxWound and EpxDecol
| EpxDecol = (6 calls/patient) × (10 min/call) = 60 min/patient |
| EpxWound = (15 calls/patient) × (15 min/call) = 225 min/patient |
| Weekly time per intervention |
| EpxDecol = (60 min/patient) × (16 patients/week) = 960 min/week = 16 h/week |
| EpxWound = (225 min/patient) × (20 patients/week) = 4,500 min/week = 75 h/week |
| FTE saved = (16 h/week +75 h/week)/(40 h/week) = 2.275 FTE |
| Price per FTE |
| 88 Weeks = ($1,388/week) × (88 weeks) = $122,144 |
| 52 Weeks = ($1,388/week) × (52 weeks) = $72,176 |
| Total cost savings |
| 88 Weeks = ($122,144/FTE × 2.275 FTE) − $10(1,753 patients) = $260,348 |
| 52 Weeks = ($72,176/FTE × 2.275 FTE) − $10(1,040 patients) = $153,800 |
| ROI |
| 88 Weeks = $260,348/$17,530 = 1,485% (14.85x) |
| 52 Weeks = $153,800/$10,400 = 1,479% (14.79x) |
FTE, full time nursing equivalent.
Discussion
Currently, patients are responsible for following pre- and postoperative protocols based on instructions that they are given before surgery and after discharge. This system is inherently inefficient and prone to error and nonadherence. Interventions such as EpxDecol and EpxWound are needed to increase patient adherence and to more effectively interface with patients outside of the hospital. Multiple digital platforms exist that utilize email or portal sites to enhance patient–provider communication.16 Nevertheless, these arrangements may fall short because they require smartphone or computer access, which are unavailable to many patients, particularly those of lower socioeconomic status.16 Use of an SMS- or phone call-based intervention, on the other hand, allows providers to engage a larger portion of patients due to the near-ubiquitous capability of all phones to answer basic text messages or phone calls.17
These results suggest that EpxDecol and EpxWound effectively engage a broad range of patients in the perioperative process, as demonstrated through high response proportions that declined minimally over the length of each intervention. The overall proportions of patients who responded daily were nearly 92% and 78% for EpxDecol and EpxWound, respectively. These numbers are higher than those for similar interventions mentioned in the literature.18,19 Self-reported measures of adherence to our decolonization protocol were higher than adherence rates that have been previously reported for similar decolonization therapies,6,20 although the validity of patient-reported adherence rates could be questioned. We believe that adherence to the chlorhexidine cleanser aspect of EpxDecol may be an underestimate of true adherence. The disparity in patient-reported adherence regarding use of their nasal spray (76% used every day) versus their cleanser (50.8% used every day), despite similar average response proportions to both questions (nasal spray: 91.9%, cleanser: 87.5%), suggests that patients are either much less adherent to using their Scrub Care or that our message timing was suboptimal. Since about 99% of patients received EpxDecol messages at 6 PM, we hypothesize that a sizable proportion of these patients planned on using their scrub care later in the night, but had not yet taken a shower. Consequently, they responded that they had not completed their decolonization for that day.
The high levels of patient satisfaction reported with EpxDecol and EpxWound indicate that patients value these interventions despite the fact that patients received automated messages instead of personal phone calls. Indeed, automated messages made patients feel like they had improved communication with their physician. Patients, for the most part, did not experience notable message fatigue and reported that they received almost the perfect number of inquiries, suggesting Epharmix's role as a helpful supplement to discharge instructions.
The cost savings and ROI analysis indicated that using EpxDecol and EpxWound may have helped the Barnes-Jewish Orthopedic Department save $260,363 over an 88-week span, with a yearly savings of $146,679. These numbers may be conservative estimates. We assumed the average nursing salary across the United States, but did not attempt to factor in benefits or other supplementary costs that accompany hiring additional nurses. This potentially reduced the reported cost savings and ROI.
Limitations
We could not fully clarify the effects of EpxDecol and EpxWound beyond patient responses and patient satisfaction and, thus, could not conclude any direct benefits from these interventions. For EpxDecol, we were unable to verify if patients truly were using their decolonization materials as specified and had to rely solely on patient responses. Since this was chiefly a feasibility study, we could not compare decolonization adherence rates between a control group and an intervention group. Our status as a clinical pilot prohibited retrospective access to patient medical records; we therefore could not determine the sensitivity and specificity of EpxWound for identifying SSIs. Future studies of EpxDecol and EpxWound will prospectively compare adherence rates with control groups and examine the efficacy with which these interventions may help prevent or catch SSIs. Our clinical pilot status also blocked us from calculating the percentage of patients who declined enrollment and which patients underwent knee versus hip replacement. The volunteer structure of this study may impart some bias upon our results: patients who consented possibly were more likely to respond to inquiries from the interventions. Finally, the time at which patients received messages may have inadvertently affected their responses to questions. We will consider adjusting message timing in future studies.
Conclusion
EpxDecol and EpxWound may serve important roles in the perioperative process for orthopedic joint reconstruction surgery given high usage of and patient satisfaction with the interventions. Anecdotally, nurses appreciated and recommend these interventions. Meaningful cost savings and substantial ROI may be realized by implementing these interventions in place of manual calls to patients. Moving forward, in addition to more prospective studies of EpxDecol and EpxWound in orthopedic patient populations, we hope to expand these interventions to other surgical subspecialties such as neurosurgery, colorectal, trauma, and cardiothoracic. Adapting this technology to more surgical patients could have widespread impacts on overall patient care and enable cost savings across different departments.
Acknowledgments
The authors thank Avik Som for providing us with the resources to make this project possible, Tonya An for her ideas and feedback, Evan Huang for his data retrieval, Christine Stavridis for her design help, and everyone on the Epharmix surgery research team who have provided support and feedback. We recognize Thea Paar for her assistance in helping create the initial quality improvement initiative. We appreciate Drs. Barrack, Nunley, Nam, Adelani, McDonald, Cipriano, O'Keefe, and Wright for contributing patients and all the nurses on the Joint Reconstruction team (Joanna Waller, Madelyn Curry, Alyssa Hesser, Desiree Trotter, Kelly Osterman, Mendi Lawson, Stephanie Hanneken, Kim Burgess, and Emily Peters) for helping with enrollment of patients. The authors acknowledge the in-kind support the Epharmix development team gave to make this project possible.
Disclosure Statement
None of the authors of this article were compensated for their work on this project, and none have equity in Epharmix. The authors are solely research volunteers at the Epharmix-sponsored Epharmix Research Center. Epharmix paid for the costs of sending messages to enrolled patients and for the storage of data.
References
- 1. Ban KA, Minei JP, Laronga C, et al. American College of Surgeons and Surgical Infection Society: Surgical site infection guidelines, 2016 update. J Am Coll Surg 2017;224:59–74 [DOI] [PubMed] [Google Scholar]
- 2. Scott RD., II The Direct medical costs of healthcare-associated infections in U.S. hospitals and the benefits of prevention. Division of Healthcare Quality Promotion National Center for Preparedness, Detection, and Control of Infectious Diseases, Atlanta, GA, 2009 [Google Scholar]
- 3. Rao N, Cannella B, Crossett LS, Yates AJ, McGough R. A preoperative decolonization protocol for Staphylococcus aureus prevents orthopaedic infections. Clin Orthop Relat Res 2008;466:1343–1348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kurtz SM, Lau E, Watson H, Schmier JK, Parvizi J. Economic burden of periprosthetic joint infection in the United States. J Arthroplasty 2012;27:61.e1–65.e1 [DOI] [PubMed] [Google Scholar]
- 5. Anderson DJ, Podgorny K, Berríos-Torres SI, et al. Strategies to prevent surgical site infections in acute care hospitals: 2014 Update. Infect Control Hosp Epidemiol 2014;35:605–627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Caffrey AR, Woodmansee SB, Crandall N, Tibert C, Fielding C, Mikolich DJ, Vezeridis MP, LaPlante KL. Low adherence to outpatient preoperative methicillin-resistant Staphylococcus aureus decolonization therapy. Infect Control Hosp Epidemiol 2011;32:930–932 [DOI] [PubMed] [Google Scholar]
- 7. Hugtenburg JG, Timmers L, Elders PJM, Vervloet M, van Dijk L. Definitions, variants, and causes of nonadherence with medication: A challenge for tailored interventions. Patient Prefer Adherence 2013;7:675–682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Som A, Groenendyk J, An T, et al. Improving dialysis adherence for high risk patients using automated messaging: Proof of concept. Sci Rep 2017;7:4177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kashgary A, Alsolaimani R, Mosli M, Faraj S. The role of mobile devices in doctor-patient communication: A systematic review and meta-analysis. J Telemed Telecare 2017;23:693–700 [DOI] [PubMed] [Google Scholar]
- 10. Pieper B, Sieggreen M, Freeland B, et al. Discharge information needs of patients after surgery. J Wound Ostomy Continence Nurs 2006;33:281–289 [DOI] [PubMed] [Google Scholar]
- 11. Sanger PC, Hartzler A, Han SM, et al. Patient perspectives on post-discharge surgical site infections: Towards a patient-centered mobile health solution. PLoS One 2017;9:e114016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Peters RM, Lui M, Patel K, et al. Improving glycemic control with a standardized text-message and phone-based intervention: A community implementation. JMIR Diabetes 2017;2:e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Horvath T, Azman H, Kennedy GE, Rutherford GW. Mobile phone text messaging for promoting adherence to antiretroviral therapy in patients with HIV infection. Cochrane Database Syst Rev 2012;3:CD009756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yu K, et al. Feasibility study on implementing accessible communication tools for SSI monitoring and prevention in joint reconstruction. JMIR Rehabil Assist Technol 2018;5:e929699967 [Google Scholar]
- 15. U.S. Bureau of Labor Statistics. 29–1141 Registered nurses. Occupational Employment Statistics, 2017. Available at www.bls.gov/oes/current/oes291141.htm (last accessed December12, 2017)
- 16. Lu K, Marino NE, Russell D, et al. Use of short message service and smartphone applications in the management of surgical patients: A systematic review. Telemed J E Health 2018;24:406–414 [DOI] [PubMed] [Google Scholar]
- 17. Rainie L, Zickuhr K. Americans' views on mobile etiquette. Pew Research Center, 2015. Available at www.pewinternet.org/2015/08/26/americans-views-on-mobile-etiquette (last accessed December12, 2017) [Google Scholar]
- 18. Anthony CA, Lawler EA, Ward CM, Lin IC, Shah AS. Use of an automated mobile phone messaging robot in postoperative patient monitoring. Telemed J E Health 2018;24:61–66 [DOI] [PubMed] [Google Scholar]
- 19. Price M, Ruggiero KJ, Ferguson PL, et al. A feasibility pilot study on the use of text messages to track PTSD symptoms after a traumatic injury. Gen Hosp Psychiatry 2014;36:249–254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kapadia BH, Cherian JJ, Issa K, et al. Patient compliance with preoperative disinfection protocols for lower extremity total joint arthroplasty. Surg Technol Int 2015;26:351–354 [PubMed] [Google Scholar]