To the Editor:
Although the incidence of end-stage kidney disease is 34% higher in US Hispanics than non-Hispanics, the latter have a lower mortality rate following initiation of dialysis (107 vs 206 per 1,000 patient-years).1,2 Outcomes have not been examined in Puerto Rico, a US territory where 4 million Hispanic Americans reside. Puerto Rico outperforms the US states and the District of Columbia (“states” hereafter) on some measures of coverage and access,3 but substantial problems with quality of care have been documented.4 Compared with Hispanics in the states, Hispanics in Puerto Rico receive lower quality care for chronic conditions; have worse control of diabetes, hyperlipidemia, and hypertension; and use effective medications for rheumatoid arthritis and chronic obstructive pulmonary disease less frequently.5 In this study, we compared 1-year mortality rates and predialysis nephrology care among Hispanics in Puerto Rico and Hispanics and whites in the states who initiated maintenance hemodialysis or peritoneal dialysis between 2006 and 2015.
We identified 791,443 patients meeting these criteria using the Centers for Medicare & Medicaid Services (CMS) Renal Management Information System (REMIS), one of the primary sources of data for the US Renal Data System (USRDS).6 We included socioeconomic information from 2010 US Census data at the zip code level. Table S1 details data and variables.
The primary outcome was age-adjusted 1-year mortality from day 91 after dialysis initiation for all incident dialysis patients during the specified year, with censoring at the time of kidney transplantation (2% of whites and Hispanics in the states, 0.5% of Hispanics in Puerto Rico). Secondary outcomes were insurance status at dialysis initiation, the presence of AV fistula or graft at initiation (limited to hemodialysis patients), and receipt of predialysis nephrology care.1,7 Covariates included age, sex, primary cause of kidney failure (diabetes, hypertension, and other), comorbid conditions, current smoking, alcohol dependence, hemoglobin level, serum albumin level, body mass index, and year. We used multiple imputation for missing data; <12% of values were missing for covariates except for albumin level (29%). We fit probit models with robust standard errors and corresponding average marginal effects. The 1-year mortality models also included secondary outcomes as covariates.
The study included 13,131 Puerto Rican Hispanics (mean age, 62.6 years; 39.8% female; mean chronic conditions, 2.9; diabetes as primary cause, 66.2%) and in the states, 155,200 Hispanics (mean age, 58.2 years; 42.1% female; mean chronic conditions, 2.2; diabetes as primary cause, 58.6%), and 623,112 whites (mean age, 66.0 years; 40.6% female; mean chronic conditions, 2.3; diabetes as primary cause, 40.9%). Table S2 lists additional characteristics.
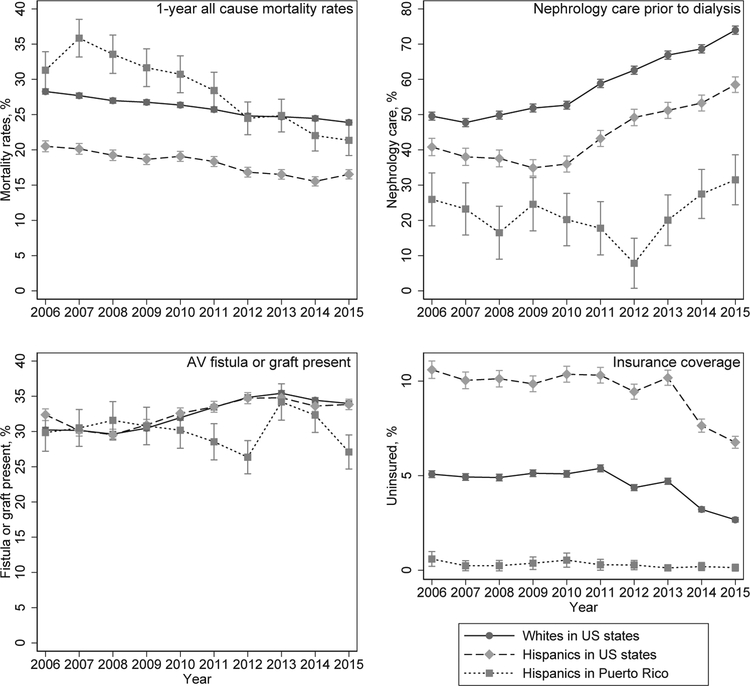
Puerto Rican Hispanics had higher 1-year mortality rates than did Hispanics and whites in the states (Table 1). The adjusted absolute difference in 1-year mortality rates between Puerto Rican and states-based Hispanics was 10.2 (95% CI, 9.3–11.1) percentage points. Adjusted 1-year mortality rates declined for all 3 groups, with nonsignificant differences between Puerto Rican Hispanics and states-based whites by 2015 (Fig 1). However, in 2015, mortality remained 4.7 (95% CI, 2.5–7.0) percentage points higher for Puerto Rican versus states-based Hispanics. In addition, Puerto Rican Hispanics had lower adjusted rates of receiving predialysis nephrology care (12.8 [95% CI, 11.8–13.8] and 8.1 [95% CI, 7.2–9.1] percentage point differences vs whites and Hispanics in the states, respectively) and initiating dialysis with an AV graft or fistula (2.4 [95% CI, 1.4–3.3] and 2.5 [95% CI, 1.6–3.4] percentage point differences vs whites and Hispanics in the states, respectively). Puerto Rican Hispanics had significantly higher rates of insurance coverage compared with the states-based groups. Sensitivity analysis excluding data with missing values and restricting to the 5 states with the highest proportions of Hispanics from Puerto Rico showed similar findings (Tables S3 and S4).
Table 1.
One-Year Mortality Rates, Access to Predialysis Nephrology Care, and Presence of an AV Fistula or Graft Among Hispanic and White Patients Initiating Dialysis in US States and Puerto Rico, 2006 to 2015
| Puerto Rican Hispanics | Hispanics in the States | Whites in the States | |
|---|---|---|---|
| 1-y Age-Standardized All-Cause Mortality (n = 791,443) | |||
| Unadjusted | 28.1 (27.4–29.0)a,b | 17.9 (17.7–18.1)b | 25.6 (25.5–25.7) |
| Adjusted (n = 633,451) | 28.4 (27.5–29.3)a,b | 18.1 (17.9–18.4)b | 26.0 (25.8–26.1) |
| Predialysis Nephrology Care (n = 696,661) | |||
| Unadjusted | 57.8 (57.0–58.7)a,b | 61.8 (61.5–62.1)b | 72.0 (71.9–72.1) |
| Adjusted | 58.2 (57.2–59.2)a,b | 66.3 (66.1–66.6)b | 71.0 (70.9–71.1) |
| AV Fistula or Graft Present (n = 725,306) | |||
| Unadjusted | 30.3 (29.5–31.2)b | 30.9 (30.6–31.1)b | 33.0 (32.8–33.1) |
| Adjusted | 30.1 (29.2–31.0)a,b | 32.6 (32.4–32.9) | 32.5 (32.4–32.6) |
| Insurance Coverage (n = 791, 443) | |||
| Unadjusted | 99.7 (99.6–99.8)a,b | 86.6 (86.4–86.8)b | 96.1 (96.0–96.1) |
| Adjusted | 99.7 (99.6–99.8)a,b | 90.5 (90.4–90.7)b | 95.5 (95.5–95.6) |
Note: Age-standardized mortality rates were calculated using direct standardization with 5-year age bands. Adjusted rates were calculated using multiple imputation. For the adjusted model, covariates included age, sex, primary cause of dialysis initiation (diabetes, hypertension, or other), comorbid conditions (including congestive heart failure, atherosclerotic heart disease, other cardiac disease, hypertension, diabetes, diabetic retinopathy, cancer, current smoking, and alcohol dependence), hemoglobin level, serum albumin level, body mass index, type of insurance (except for the insurance coverage model), and zip code level information regarding poverty, unemployment, income, and education. In addition, mortality models adjusted for nephrology care, AV fistula or graft present before dialysis, and insurance coverage before dialysis. All 95% confidence intervals (values in parentheses) are derived from probit models with Huber-White robust standard errors. We calculated corresponding average marginal effects.
Abbreviation: AV, arteriovenous.
P < 0.05 vs Hispanics in US states;
P < 0.05 vs whites in US states.
Figure 1.
Trends in adjusted 1-year all-cause mortality rate, predialysis nephrology care, AV fistula or graft present, and insurance coverage among US whites and Hispanics in the states and Hispanics in Puerto Rico initiating dialysis.
Limitations include that the prevalence of nephrology care may be underestimated in our cohort due to our use of the CMS-2728 form.8 We lacked individual-level information regarding patients’ socioeconomic variables, disability, disease self-management practices, and regional variables that may mediate some of the differences that we found. We were unable to stratify our results by Hispanic subgroups in the states. However, results remained similar after comparing Hispanics in Puerto Rico with Hispanics in states with the highest fractions of Puerto Ricans.9
Despite higher rates of insurance coverage, we identified substantial disparities in mortality and access to recommended nephrology care between Puerto Rico and the states. This may relate to differences in quality of care for Puerto Ricans with serious chronic illness and complex care needs or lower funding for Medicare and Medicaid in Puerto Rico, although we are not able to identify the mechanisms for the observed differences.5 Overall, we found that lower mortality for Hispanic patients receiving dialysis10 may hold true only for those living in the states. Recently, overall mortality rates for Puerto Ricans have been declining, resulting in a narrowing of disparities compared with the states. Additional efforts are needed to improve specialty care access and quality of care for Puerto Ricans with kidney failure.
Supplementary Material
Support:
Research reported in this publication was supported by Institutional Development Award Number U54GM115677 from the NIGMS of the NIH, which funds Advance Clinical and Translational Research (Advance-CTR) and by the NIH/NIDDK (award R01DK113398-01). The funders had no role in study design; data collection, analysis, or reporting; or the decision to submit for publication.
Footnotes
Financial Disclosure: The authors declare that they have no other relevant financial interests.
Publisher's Disclaimer: Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- 1.Saran R, Robinson B, Abbott KC, et al. US Renal Data System 2017 Annual Data Report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2018;71(3)(suppl 1):S1–S676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Desai N, Lora CM, Lash JP, Ricardo AC. CKD and ESRD in US Hispanics. Am J Kidney Dis. 2019;73(1):102–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Portela M, Sommers BD. On the outskirts of national health reform: a comparative assessment of health insurance and access to care in Puerto Rico and the United States. Milbank Q. 2015;93(3):584–608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nunez-Smith M, Bradley EH, Herrin J, et al. Quality of care in the US territories. Arch Intern Med. 2011;171(17):1528–1540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rivera-Hernandez M, Leyva B, Keohane LM, Trivedi AN. Quality of care for white and Hispanic Medicare Advantage enrollees in the United States and Puerto Rico. JAMA Intern Med. 2016;176(6):787–794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.US Renal Data System. 2016 Researcher’s Guide to the USRDS Database. https://www.usrds.org/2016/rg/2016_USRDS_Researchers_Guide_16.pdf. 2016. Accessed July 23, 2019.
- 7.Swaminathan S, Sommers BD, Thorsness R, Mehrotra R, Lee Y, Trivedi AN. Association of Medicaid expansion with 1-year mortality among patients with end-stage renal disease. JAMA. 2018;320(21):2242–2250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim JP, Desai M, Chertow GM, Winkelmayer WC. Validation of reported predialysis nephrology care of older patients initiating dialysis. J Am Soc Nephrol. 2012;23(6):1078–1085. [DOI] [PubMed] [Google Scholar]
- 9.Wang Y, Rayer S. Growth of the Puerto Rican population in Florida and on the U.S. Mainland. Bureau of Economic and Business Research; Published 2018, https://www.bebr.ufl.edu/population/website-article/growth-puerto-rican-population-florida-and-us-mainland. Accessed June 18, 2019. [Google Scholar]
- 10.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis. 2001;11(3):496–518. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.