Abstract
Background
Endotracheal intubation is a common procedure in newborn intensive care units. The choice of the oral or nasal route for intubation is usually determined by an institution's customary practice. The procedure of intubation for both the oral and nasal routes can be associated with complications. This systematic review was undertaken to compare the complications of both methods.
Objectives
The purpose of the review was to compare the complications associated with intubation by the nasal route with those associated with intubation by the oral route for mechanical ventilation in newborn infants.
Search methods
The standard search strategy of the Cochrane Neonatal Review Group as outlined in The Cochrane Library was used. This included searches of the Oxford Database of Perinatal Trials, Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 3, 2006), MEDLINE (from January 1996 to July, 2006, all languages), EMBASE (1988 to July 2006) and CINAHL (from 1982 to July 2006), previous reviews including cross references and abstracts. A call was placed on the list servers, NICU‐NET and Neonatal Talk for unpublished trials, conference presentations and current trials.
Selection criteria
All trials using random or quasi‐random allocation of patients to either the nasal or oral route of intubation were included. Study quality and eligibility were assessed independently by each author.
Data collection and analysis
The standard method of the Cochrane Collaboration and the Neonatal Review Group was used to assess the methodological quality of the included studies. The methodological quality of each study was reviewed by the second review author blinded to study authors and institutions.
Each review author extracted data separately before comparison and resolution of differences. The standard method of the Neonatal Review Group was used to measure the effect of the different routes of intubation, using Relative Risk (RR) and 95% Confidence Intervals (CI).
Main results
Only two eligible randomized trials were found. Data from these two trials did not demonstrate significant differences between the oral and nasal route of intubation for mechanically ventilated neonates. The rate of failure to intubate using the nasal route was higher in one study. One study found post extubation atelectasis occurred more frequently in nasally intubated infants who weighed less than 1500 grams.
The rates of malposition of the tube at the initial intubation, accidental extubation, tube blockage, re‐intubation after extubation, septicaemia, clinical infection and local trauma (nasal erosion or palatal groove) were not significantly different for the two groups.
Authors' conclusions
Post extubation atelectasis may be more frequent after nasal intubation, particularly in very low birth weight infants. One route of intubation does not seem to be preferable to the other. There is a need for further randomized controlled trials containing larger numbers of infants.
Plain language summary
Nasal versus oral intubation for mechanical ventilation of newborn infants
There is not enough evidence to demonstrate any differences in the effect of nasal versus oral intubation for mechanical ventilation of newborn babies in neonatal intensive care. Babies in neonatal intensive care often need help to breathe, sometimes via a ventilator (machine). Air is mechanically pumped into their lungs through a tube that is either inserted into their mouth or nose (endotracheal intubation). Insertion can fail and problems can include a blockage in the tube or the baby's airway, the wrong size tube or injury as a result of the presence of the tube. Complications caused by endotracheal intubation can also have serious adverse effects for the baby such as heart and breathing problems. The review did not find enough evidence from trials to demonstrate any differences in the effect of nasal versus oral intubation. More research is needed.
Background
Endotracheal intubation is a common procedure in newborn intensive care units (Bancalari 1992). The choice of the oral or nasal route for intubation is usually determined by an institution's customary practice, based on clinical experience regarding the perceived short and long term benefits and complications of one route compared with the other (Roberton 1992).
The procedure of intubation may be technically difficult (Dankle 1987) for both the oral and nasal routes. This is particularly true for infants who weigh less than 1000 gram or greater than 3000 gram (Noblett 1995). Approximately 30% of infants require repeated intubations (Dankle 1987; Noblett 1995) for accidental extubation, failure of extubation, tube blockage, inappropriate tube size and upper airway obstruction.
Endotracheal intubation may be attended by such complications as cardiorespiratory compromise during the procedure, tube malposition, tube blockage, traumatic injury to the nares or palate, glottis or trachea, lung or airway collapse, and infection (Spitzer 1982; McMillan 1986).
Specific complications may be associated with either the oral or nasal route of intubation. Palatal grooving and alveolar grooving (Angelos 1989) are associated with oral intubations. Nasal deformities were more likely to occur as a complication of nasotracheal intubation in infants weighing less than 1000 grams (Gowdar 1980).
There are few reported studies that compare the benefits and complications of the two routes of intubation. The complications associated with endotracheal intubation may cause or aggravate cardiorespiratory and/or neurological disorder and, perhaps, result in long term respiratory, cosmetic or neurological disability. Therefore, determining the complications associated with the different routes of intubation is deemed important for clinical practice and good patient outcomes.
Objectives
The purpose of the review was to assess the effect of the route of intubation (nasal or oral) on the incidence of complications in newborn infants who were intubated for mechanical ventilation.
Subgroup analysis was planned to examine variation in results for infants of different birth weights or gestational age.
Methods
Criteria for considering studies for this review
Types of studies
All trials using random or quasi‐random selection of patients for either the oral or nasal route of intubation were included.
Types of participants
Newborn infants who required endotracheal intubation for mechanical ventilation.
Types of interventions
Tracheal intubation by either the nasal or the oral route.
Types of outcome measures
Primary outcomes
Procedure failure
Accidental malposition of the tube
Tube occlusion
Post extubation atelectasis
Post extubation stridor
Infection
Subglottic stenosis or deformity of the nares or palate
Secondary outcomes
Survival
Intracranial haemorrhage
Periventricular leukomalacia
Bronchopulmonary dysplasia
Abnormal phonation or speech
Mental and/or psychomotor disability
Search methods for identification of studies
The standard search strategy of the Neonatal Review Group as outlined in The Cochrane Library was used. This included searches of the Oxford Database of Perinatal Trials, Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Issue 3, 2006), MEDLINE (from January 1996 to July, 2006, all languages) and CINAHL (from 1982 to July, 2006), EMBASE (1988 to July 2006) previous reviews including cross references and abstracts. A call was placed on the list servers, NICU‐NET and Neonatal Talk for unpublished trials, conference presentations and current trials. The strategy used was MeSH headings and/or keywords: endotracheal, intubation, oral, nasal, neonatal.
Data collection and analysis
The standard method of the Cochrane Collaboration and the Neonatal Review Group was used to assess the methodological quality of the included studies. The methodological quality of each study was reviewed by the second review author blinded to study authors and institutions.
Each review author extracted data separately before comparison and resolution of differences.
The standard method of the Cochrane Neonatal Review Group was used to measure the effect of the different routes of intubation, using Relative Risk (RR) and 95% Confidence Intervals (CI).
McMillan 1986 was contacted for information regarding concealment of allocation but details regarding patients and data for this study were no longer available.
Heterogeneity will be examined using the I‐squared statistic. Where significant heterogeneity is noted, secondary subgroup analyses will evaluate possible sources of heterogeneity, including study population and study design.
Results
Description of studies
1. Included Studies
1.1.Spitzer 1982 A randomized controlled trial of 86 infants who were ventilated for more than 48 hours. Infants were randomly assigned to either the oral or nasal route of intubation. The infants were stratified into weight groups greater than 3000 gram or 3000 gram or less; the latter were further divided into 500 gram groups. A primary outcome of the study was post‐extubation atelectasis. Other outcome measures included tube blockage, need for reintubation after extubation, septicaemia and tube trauma to the nares or palate.
1.2. McMillan 1986 A randomized controlled trial of 91 neonates who received either the nasal or oral route of intubation for ventilation. The infants were of varying birth weight and their mean gestational age was 32 weeks. No results were reported for the infants according to their birth weight.
The failure of the initial procedure and malposition of the tube at the initial intubation were recorded. The six infants who failed nasal intubation were then intubated orally and all subsequent outcomes were analysed with the oral group.
Outcomes included post‐extubation atelectasis and tube blockage. Tube blockage was recorded as the number per 100 days of intubation. It is not clear whether the number of tube blockages referred to one infant or multiple infants. The other outcome measures included accidental extubation, need for reintubation after extubation and clinical infection.
2. Excluded studies
There were no other studies that compared the differences between the oral and the nasal route of intubation in neonates. There were several studies that looked at outcomes of intubation for either the oral or nasal route. These studies are listed as Excluded studies.
Risk of bias in included studies
The overall quality of the two studies was poor and there were methodological problems in each study that could lead to bias. Randomization of route of intubation was by blind allocation in one study (McMillan 1986). In the other study (Spitzer 1982), the route of intubation was randomized within blocks for each eligible infant to create similar groups by weight.
In both studies, the randomized infants were included in the analysis. However, McMillan 1986 analysed six infants from the nasal group with those in the oral group after failure of nasal intubation. Spitzer did not state to which group the 14 excluded infants had been randomized, or if they were excluded from the data analysis. The data are not available to allow an intention to treat analysis.
One study (Spitzer 1982) did not state whether there was blinded assessment of all outcome measures. Blinded assessment was deemed not possible by the reviewer in the other study (McMillan 1986).
Effects of interventions
Procedure Failure (Outcome 01‐01)
In one study (McMillan 1986), intubation via the nasal route was unsuccessful in six (13.3%) of 45 infants compared with 0 (0%) of 46 for intubation by the oral route (RR 13.28, 95% CI 0.77, 229.08). The failure rate was not stated in the other study (Spitzer 1982).
Post‐extubation atelectasis (Outcome 01‐05)
In one study (Spitzer 1982), post extubation atelectasis occurred in 15 (34.9%) of 43 nasally intubated infants compared with five (11.6%) of 43 orally intubated infants (RR 3.00, 95% CI 1.20, 7.53). In the other study (McMillan 1986), the rate of post extubation right upper lobe atelectasis was not significantly different for the two groups (RR 1.28, 95% CI 0.65, 2.53).
Overall, the meta‐analysis of these two studies suggests an increased risk of post‐extubation atelectasis associated with nasal intubation (typical RR 1.85, 95% CI 1.08, 3.18).
Subgroup analysis (Comparison 02)
In one study (Spitzer 1982), the rate of post extubation atelectasis was stratified by weight. Post extubation atelectasis did not occur in infants > 2500 gram birth weight. In infants < 1500 gram birth weight, post extubation atelectasis occurred in 10 (58.8%) of 17 nasally intubated compared with two (11.8%) of 17 orally intubated infants (RR 5.00, 95% CI 1.28, 19.50).
Other complications
The rates of malposition of the tube at the initial intubation (McMillan 1986), accidental extubation (McMillan 1986), tube blockage (McMillan 1986; Spitzer 1982), re‐intubation after extubation (McMillan 1986; Spitzer 1982), septicaemia (Spitzer 1982), clinical infection (McMillan 1986) and local trauma (nasal erosion or palatal groove) (Spitzer 1982) were not significantly different for the two groups.
Many of the prespecified primary and secondary outcomes listed in 'Types of outcome measures' were not reported in the studies.
Discussion
The results of this review should be interpreted with caution. The included studies contained small numbers, measured different outcomes and did not assess long‐term outcomes associated with either the oral or nasal route of tracheal intubation.
The failure rate for intubation was greater by the nasal route compared with the oral route, indicating the former procedure may be more difficult.
Post extubation atelectasis may be more common in nasally intubated infants, particularly if they are of very low birth weight.
Both studies have a potential for bias. In McMillan's study the analysis of the six infants who failed nasal intubation in the oral group is a concern. In Spitzer's study, it is unknown in what group the 14 infants who died early or who received ventilation for less than 48 hours were randomized.
Authors' conclusions
Implications for practice.
In view of the small numbers and methodological difficulties, no firm recommendations for practice can be made. However, the nasal route of intubation may be more difficult, and therefore oral intubation might be preferred for inexperienced operators. Post extubation atelectasis may be more frequent after nasal intubation, particularly in very low birth weight infants. One route does not seem to be preferable to the other in relation to the rate of tube malposition, accidental extubation, tube blockage, re‐intubation after extubation, infection and local trauma.
Implications for research.
There is a need for further randomized controlled trials containing larger numbers of infants. The short‐term outcome measures should assess the relative difficulty of the two procedures, including their effect on cardiorespiratory function and cerebral blood flow, the patency of the tube and its stability within the trachea, systemic infection, nasal or palatal injury, and subglottic stenosis. The long‐term outcome measures should assess the relative rates of intracranial haemorrhage, periventricular leukomalacia, hearing and speech deficits, and mental and psychomotor disability.
What's new
| Date | Event | Description |
|---|---|---|
| 22 August 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 2, 1998 Review first published: Issue 2, 1999
| Date | Event | Description |
|---|---|---|
| 31 August 2006 | New search has been performed | This is an update of the previously published version "Nasal versus oral intubation for mechanical ventilation of newborn infants" published in The Cochrane Library, Issue 1, 2002 (Spence 2002). No new eligible trials were found. Thus, there is no change to the conclusion that there is not enough evidence that one route of intubation is preferable to the other. |
| 18 February 1999 | New citation required and conclusions have changed | Substantive amendment |
Acknowledgements
Professor David Henderson‐Smart for his guidance in the undertaking of this review.
Data and analyses
Comparison 1. Nasal vs oral intubation (all infants).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Procedure failure | 1 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 13.28 [0.77, 229.07] |
| 2 Malposition on initial intubation | 1 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.64, 1.57] |
| 3 Accidental extubation | 1 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.67 [0.27, 1.62] |
| 4 Tube blockage | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.83 [0.75, 4.51] |
| 5 Post extubation atelectasis in babies extubated | 2 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.85 [1.08, 3.18] |
| 6 Re‐intubation in babies extubated | 2 | 160 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.64 [0.75, 3.59] |
| 7 Septicemia | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.0 [0.15, 6.78] |
| 8 Clinical infection | 1 | 91 | Risk Ratio (M‐H, Fixed, 95% CI) | 2.10 [0.89, 4.91] |
| 9 Nasal or palatal trauma | 1 | 86 | Risk Ratio (M‐H, Fixed, 95% CI) | 1.33 [0.32, 5.61] |
1.1. Analysis.
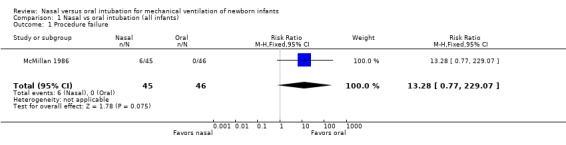
Comparison 1 Nasal vs oral intubation (all infants), Outcome 1 Procedure failure.
1.2. Analysis.
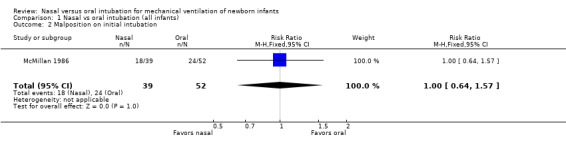
Comparison 1 Nasal vs oral intubation (all infants), Outcome 2 Malposition on initial intubation.
1.3. Analysis.
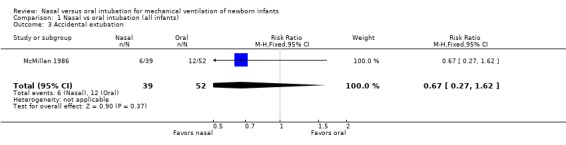
Comparison 1 Nasal vs oral intubation (all infants), Outcome 3 Accidental extubation.
1.4. Analysis.
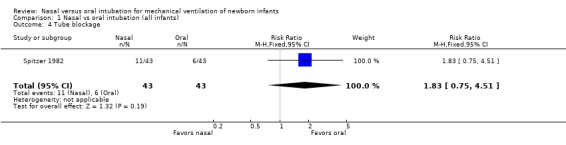
Comparison 1 Nasal vs oral intubation (all infants), Outcome 4 Tube blockage.
1.5. Analysis.
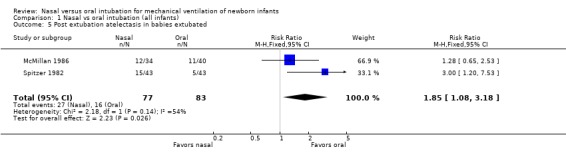
Comparison 1 Nasal vs oral intubation (all infants), Outcome 5 Post extubation atelectasis in babies extubated.
1.6. Analysis.
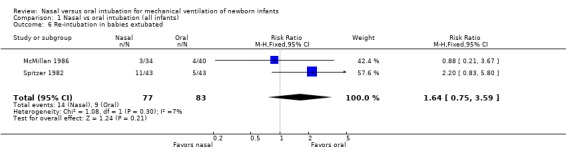
Comparison 1 Nasal vs oral intubation (all infants), Outcome 6 Re‐intubation in babies extubated.
1.7. Analysis.
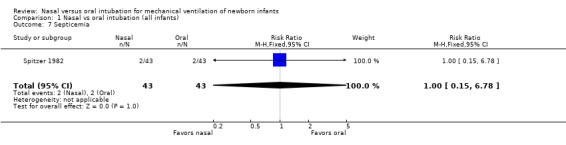
Comparison 1 Nasal vs oral intubation (all infants), Outcome 7 Septicemia.
1.8. Analysis.
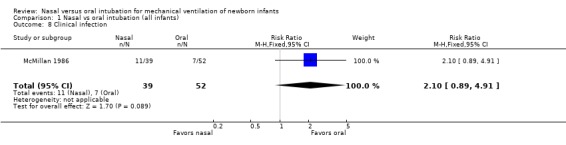
Comparison 1 Nasal vs oral intubation (all infants), Outcome 8 Clinical infection.
1.9. Analysis.
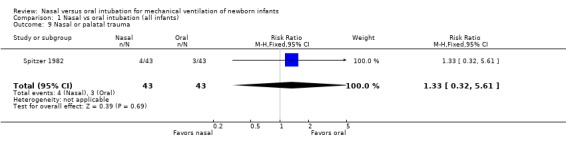
Comparison 1 Nasal vs oral intubation (all infants), Outcome 9 Nasal or palatal trauma.
Comparison 2. Nasal vs oral intubation (birth weight <1500 gram).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Post extubation atelectasis in babies extubated | 1 | 34 | Risk Ratio (M‐H, Fixed, 95% CI) | 5.0 [1.28, 19.50] |
2.1. Analysis.
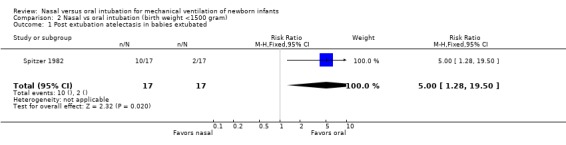
Comparison 2 Nasal vs oral intubation (birth weight <1500 gram), Outcome 1 Post extubation atelectasis in babies extubated.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
McMillan 1986.
| Methods | Concealment ‐ opaque envelopes. Blinding of randomization by card selection method. Blinding of intervention ‐ no. Completeness of follow up ‐ yes. Blinding of outcome assessment ‐ yes for xrays no for other outcomes. | |
| Participants | 91 ventilated newborn infants of varying birth weight, mean gestational age approximately 31 weeks in nasal and 32 weeks in oral group. Stratified by weight groups | |
| Interventions | Endotracheal intubation by either nasal or oral route | |
| Outcomes | Procedure failure reported by original groups as randomized. For other outcomes failed nasal intubation infants (6) included in oral group ‐ malposition, tube blockage, post extubation right upper lobe atelectasis, clinical infection. | |
| Notes | Results not stratified by weight. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
Spitzer 1982.
| Methods | Allocation concealment ‐ can't tell. Randomization into blocks of two in order to stratify according to birth weight. The intervention was randomized for the first infant entering into a birth weight category and the next infant received the other intervention. Blinding of intervention ‐ no. Completeness of follow‐up ‐ no, as 14 additional infants were excluded because of early death or because they required ventilation for <48 hours. Blinding of outcome ‐ no. | |
| Participants | Analysis resulted in 86 newborn infants requiring ventilation for >48 hours. Stratified into weight groups >3000 gram and 3000 gram and less divided into 500 grams groups | |
| Interventions | Endotracheal intubation by either nasal or oral route | |
| Outcomes | Tube blockage Pneumothorax Post extubation atelectasis reported by weight groups Re‐intubation Local trauma | |
| Notes | The focus of the study was on post‐extubation atelectasis | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Dankle 1987 | Retrospective analysis of infants intubated using predominantly orotracheal tubes. No comparison made between the two routes of intubation. |
| Erenberg 1984 | Infants requiring orotracheal or orogastric tubes were studied for palatal grooves using maxillary casts. It was not stated how the infants were recruited into the study. No comparison between two routes of intubation. |
| Gowdar 1980 | Cohort study of infants who required nasal CPAP and/or nasal intubation. No comparison with oral route of intubation. |
| Noblett 1995 | The study evaluated the performance of respiratory care practitioners through self evaluation following each oral intubation. No comparison with nasal route of intubation. |
| Stewart 1980 | Retrospective review of surviving infants who required nasotracheal intubation. No comparison with oral route of intubation. |
Contributions of authors
Both reviewers assessed the trials for eligibility, quality, and extracted data independently. The review was written by KS with the editorial assistance of PB.
Sources of support
Internal sources
Department of Neonatology, The Children's Hospital at Westmead, Australia.
External sources
Centre for Perinatal Health Services Research, University of Sydney, Australia.
Declarations of interest
None
Edited (no change to conclusions)
References
References to studies included in this review
McMillan 1986 {published and unpublished data}
- McMillan DD, Rademaker AW, Buchan KA, Reid A, Machin G, Sauve RS. Benefits of orotracheal and nasotracheal intubation in neonates requiring ventilatory assistance. Pediatrics 1986;77:39‐44. [PubMed] [Google Scholar]
Spitzer 1982 {published data only}
- Spitzer AR, Fox WW. Postextubation atelectasis ‐ the role of oral versus nasal endotracheal tubes. Journal of Pediatrics 1982;100:806‐10. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Dankle 1987 {published data only}
- Dankle SK, Schuller DE, McClead RE. Prolonged intubation of neonates. Archives of Otolaryngology‐‐Head & Neck Surgery 1987;113:841‐3. [DOI] [PubMed] [Google Scholar]
Erenberg 1984 {published data only}
- Erenberg A, Nowak AJ. Palatal groove formation in neonates and infants with orotracheal tubes. American Journal of Diseases of Children 1984;138:974‐5. [DOI] [PubMed] [Google Scholar]
Gowdar 1980 {published data only}
- Gowdar K, Bull MJ, Schreiner RL, Lemons JA, Gresham EL. Nasal deformities in neonates. American Journal of Diseases of Children 1980;134:954‐7. [PubMed] [Google Scholar]
Noblett 1995 {published data only}
- Noblett KE, Meibalane R. Respiratory care practitioners as primary providers of neonatal intubation in a community hospital: an analysis. Respiratory Care 1995;40:1063‐7. [PubMed] [Google Scholar]
Stewart 1980 {published data only}
- Stewart AR, Finer NN, Moriartey RR, Ulan OA. Neonatal nasotracheal intubation: an evaluation. Laryngoscope 1980;90:826‐31. [PubMed] [Google Scholar]
Additional references
Angelos 1989
- Angelos GM, Smith DR, Jorgenson R, Sweeney EA. Oral complications associated with neonatal oral tracheal intubation: a critical review. Pediatric Dentistry 1989;11:133‐40. [PubMed] [Google Scholar]
Bancalari 1992
- Bancalari E, Sinclair JC. Mechanical ventilation. In: Sinclair JC, Bracken MB editor(s). Effective Care of the Newborn Infant. Oxford: Oxford University Press, 1992:210‐1. [Google Scholar]
Roberton 1992
- Roberton NRC. Pulmonary diseases of the newborn. In: Roberton, NRC editor(s). Textbook of Neonatology. Melbourne: Churchill Livingston, 1992:478‐9. [Google Scholar]
References to other published versions of this review
Spence 1999
- Spence K, Barr P. Nasal versus oral intubation for mechanical ventilation of newborn infants. The Cochrane Database of Systematic Reviews 1999, Issue 2. [DOI: 10.1002/14651858.CD000948] [DOI] [PMC free article] [PubMed] [Google Scholar]
Spence 2002
- K Spence, P Barr. Nasal versus oral intubation for mechanical ventilation of newborn infants. The Cochrane Database of Systematic Reviews 2002, Issue 1. [DOI: 10.1002/14651858.CD000948] [DOI] [PMC free article] [PubMed] [Google Scholar]


