Abstract
BACKGROUND:
The over projected nose, commonly referred to as the “Pinocchio” nose is a significant challenge to the rhinoplasty surgeon. Firstly, we speak about a very large nose, and secondly, we speak about the correction of nasal cartilages (alar and triangular). Surgical correction of the over projected nose is the most difficult and least predictable component of rhinoplasty surgery.
AIM:
By performing rhinoseptoplasty we aimed to achieve an ideal landmarks position according to concepts of nasal projection as well as by making preoperative analyses to determine the ideal position for the nasal tip after having understood and defined the ideal position for the nasion.
METHODS:
We performed a retrospective study of patients who were admitted to ENT University Clinic, University Campus “St. Mother Theresa” Skopje, the Republic of Macedonia in the period 2011-2019. A total of 70 patients were enrolled in the study; 46 women (33%) and 24 men (33%). Operative technique rhinoseptoplasty was realised in 70 patients. All of the 70 (100%) patients underwent preoperative and postoperative evaluation during this period regularly to record the effects of various approaches on nasal projection, rotation, need for revision, and patient satisfaction.
RESULTS:
All patients used one or more of the preferred methods to treat over projection. Patients who had undergone 2 previous rhino/septoplasty procedures were excluded from the study, and hence, a total of 70 patients were evaluated. Full-transfixion incisions were made in all patients. From 2011 to 2019, in 72 cases, 1 or more of the preferred methods were used to treat over projection.
CONCLUSION:
The crural anatomy of the nasal tip relates to the size and shape of the lower lateral cartilages (LLC) and their relationship with the caudal septum and upper lateral cartilages (ULC). Modification of nasal tip rotation and projection should attempt to preserve or reconstruct major tip mechanisms.
Keywords: Nasal tip over projection, Important nasal tip structures, Surgical techniques, Nasal tip deformities, Rhino/septoplasty
Introduction
All wisdom starts with the solid foundation of knowledge, maturity, experience, happiness and health. If for a few minutes we stop and look at some great architectural structures, for example, cathedrals, we will notice that they are laid on perfectly designed grounds, covered with concrete blocks to support the building. We can see a variety of shapes, forms, designs, but the strong pillars are crucial supporting architecture.
The same functions have the pillars of the nose; we can reshape and change the foundation and size of the nose; we can play with different forms; we can model the nasal pyramid. But the “pillars” of the nose are very important nasal structures. Thus, in this study, we wanted to discuss the importance of these “pillars of the nose” and to present different surgical methods in resolving over the projected nose. Every rhinoplasty surgeon has to take care of the nasal pillars. The aim of each rhinoplasty surgeon is to establish a balance between facial esthetic harmony and nasal function since they are in perfect unity. If they are separated, then breathing or esthetics is being sacrificed, which is of no interest to both the rhinoplasty surgeon and the nose as a physiological and esthetic unity [1], [2], [3], [4].
The over the projected nose, commonly referred to as the “Pinocchio” nose is a significant challenge to the rhinoplasty surgeon. Firstly, we speak about a very large nose, and secondly, we speak about the correction of nasal cartilages (alar and triangular), which have to be shortened and remodelled, but it can cause disturbance both to the nasal esthetic appearance and to the nasal function. Therefore, the rhinoplasty surgeon has to plan the surgical intervention thoroughly and to determine the ideal postoperative position of the nose to achieve an ideal esthetic and functional harmony. Surgical correction of the over projected nose is the most difficult and least predictable component of rhinoplasty surgery. To draw a parallel with the fashion industry: “Less is more” [5], [6].
The over the projected nose is important for aesthetic and functional reasons. The rhinoplasty surgeon must understand the concepts of nasal projection and with preoperative analyses to determine the ideal position for the nasal tip after having understood and defined the ideal position for the nasion.
The anatomy of the nasal tip is in close relation with its “pillars”: lower lateral cartilages (LLC), upper lateral cartilages (ULC) and their connection with the caudal septum. Any surgical intervention that might cause their distinct reshaping and resise can lead to disturbance of these supporting pillars, nasal mechanisms that can have an impact on the nasal function or irregularities in the esthetics. Many authors have discussed ways to deproject the tip and shorten the nose [7], [8].
Nasal tip projection has to be in relation not only to the nasal dorsum but also to overall facial proportions. Rhino/septoplasty manoeuvres can increase, preserve, or decrease nasal tip projection. Therefore, they have to be chosen properly (Figure 1).
Figure 1.
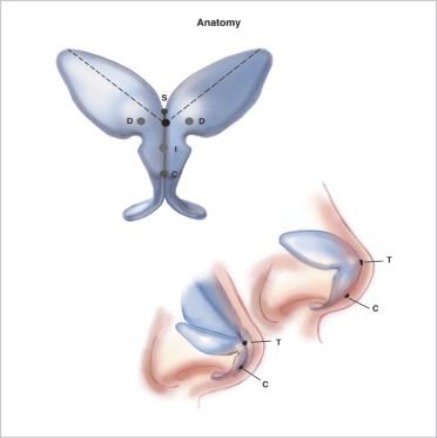
Anatomy of the nasal tip: lower lateral cartilages (LLC), caudal septum and upper lateral cartilages (ULC) [9]
Nasal tip projection is defined as the length of the perpendicular drawn from the vertical facial place to the tip-defining point [10], [11].
Nasal tip support has typically been classified as major and minor. Major tip support mechanisms were first described by Janke and Wright and have been further studied.
The “Tripod concept” is an oversimplification of nasal tip dynamics and emphasises the intimate relationship between projection and rotation. It also determines the position of the nasal tip. Each lateral crus represents the lateral legs of the tripoid, while the medial crus constitutes the central leg. The “Tripod concept” also highlights the effect of the operative procedure on one limb may have on the spatial position of the entire nasal tip [12], [13], [14], [15] (Figure 2).
Figure 2.
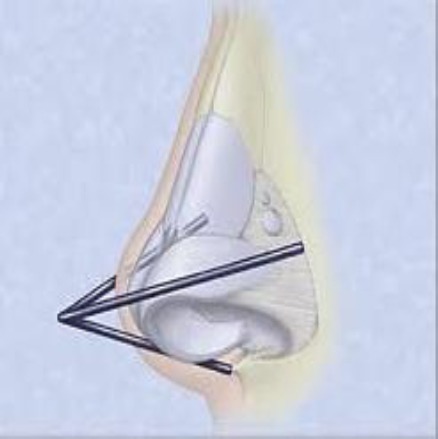
The “Tripod concept” [16]
Preoperative evaluation is necessary to prepare patients for surgical treatment. First of all, patients’ preoperative photographs were obtained to give the surgeon a clear picture of the correct amount of necessary surgical reduction. The nasal projection was measured from the alar facial groove to the tip-defining point. The amphas (horizontal plane) and profile view are important to show the irregularities of the nasal dorsum (dorsal hump), nasal length, nasofrontal angle, naso-facial angle, nasolabial angle [17], [18] (Figure 3).
Figure 3.
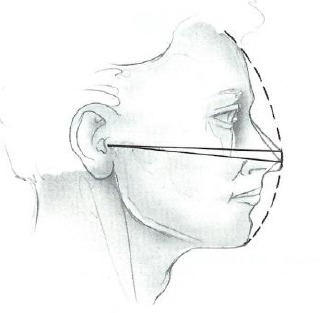
Profile view measurements [19]
The nasal skin is very important because the thick skin can cause more postoperative oedema and scarring, and less refinement is noticeable. Thin skin is more predictable healing, but less forgiving of minor asymmetries. Palpation of the nose helps in determining tip support, identifying septal character and better visualisation of the cartilages.
Considering the surgical anatomy, “the pillars of the nose” are lower lateral cartilages (LLC), upper lateral cartilage (ULC), medial crus, nasal dome, lateral crus, which are important in defining the nasal tip and projection. The term crural arch refers to the alar cartilage, which components arches are the lateral crura and the medial crura. They are joined by a transitional segment of cartilage in the domal region, which is termed the intermediate crura. The tip-defining point refers to the highest point of the tip cartilages [20], [21], [22] (Figure 4).
Figure 4.
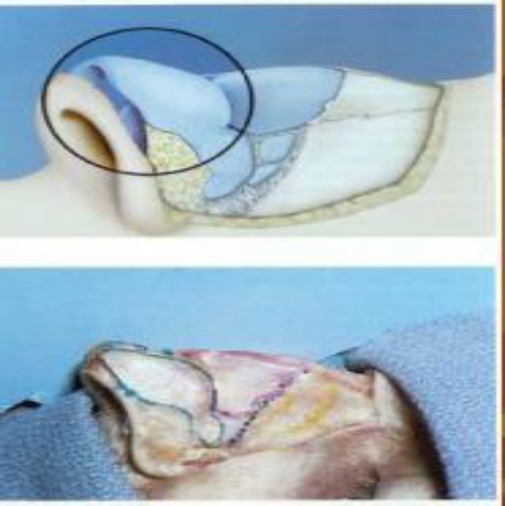
The “Pillars of the nose” [23]
Several techniques of deprojecting nose have been described, and most involve weakling, dividing or excising segments of the alar area. The most commonly used techniques are delivery approach, non-delivery approach and “Open Nose” approach. The delivery approach allows better visualisation of cartilaginous structures but requires more extensive dissection, more tissue trauma and greater risk of tip oedema but slightly increased risk of postoperative scarring. Non-delivery approach is less traumatic with less tip oedema, but allows poor visualisation of the cartilage and sacrificing of the scroll area. The “Open nose” technique allows the best visualisation of the cartilaginous skeleton, but the risk is that columellar incision has potential for scarring. Tip oedema is significant, and it makes intraoperative assessment more difficult.
The last step in correcting the over projected tip is decreasing the ala and sill of the nostril. Upon completion of the deprojection, a widened nasal base is left. If necessary, osteotomies are performed at this point. The incisions are closed and a routine dressing is applied [24], [25], [26], [27], [28].
In this study, we wanted to present that the application of contemporary rhinoplasty techniques has increased the surgeon’s ability to control tip projection, without disruption of the domes and medial crura. With the loss of tip support, scar contracture has led to an increased incidence of postoperative tip ptosis, alar insufficiencies, nasal asymmetries and other tip deformities.
Material and Methods
We performed a retrospective study of patients who were admitted to ENT University Clinic, University Campus “St. Mother Theresa” Skopje, the Republic of Macedonia in the period 2011-2019.
A total of 70 patients were enrolled in the study; 46 women (33%) and 24 men (33%). The age of the patients ranged from 16 to 50 years (mean age ± SD 33 ± 5.6 min = 16 max = 50). Operative technique rhinoseptoplasty was realised in 70 patients.
Inclusion criteria for septo/rhinoplasty were: patients older than 16 years, patients with nasal septal deviation, nasal obstruction as a result of nasal septal deviation, rhinokyphosis, rhinoscoliosis, rhinolordosis, functional tension nose, saddle nose, moderate to severe degree of nasal obstruction detected with functional tests. All of those patients had nasal tip asymmetries and over the projected nose.
The exclusion criteria for septo/rhinoplasty were: severe nasal deformities that were to be managed with an open approach, septo/rhinoplasty after verified malignant processes of the nose and nasal septum, severe degree of nasal obstruction caused by chronic rhinosinusitis without changes in the nasal septum or nasal pyramid, cardiovascular and other chronic diseases, coagulopathies and diseases of the hematopoietic system, autoimmune diseases. All of the 70 patients gave oral consent that their images can be used for research-medical purposes.
All of the 70 (100%) patients underwent preoperative and postoperative evaluation during this period regularly to record the effects of various approaches on nasal projection, rotation, need for revision, and patient satisfaction. All patients used one or more of the preferred methods to treat over projection. Patients who had undergone 2 previous rhino/septoplasty procedures were excluded from the study, and hence, a total of 70 patients were evaluated. Full-transfixion incisions were made in all patients.
Results
A total of 70 patients were enrolled in the study; 46 women (33%) and 24 men (33%). The age of the patients ranged from 16 to 50 years (mean age ± SD 33±5.6 min=16 max=50). Operative technique rhinoseptoplasty was realised in 70 patients (Table 1).
Table 1.
Demographic characteristics of the patients
| Variable | ||
|---|---|---|
| Gender n (%) | Men | 24 (34.3%) |
| Women | 46 (65.7%) | |
| Age (year) | Mean ± sd 33 ± 5.6 min = 16 max = 50 | |
The preoperative data showed the following results: 47 (67.14%) patients had rhinoseptoplasty for the first time, 9 (12.9%) patients had had the previous rhinoplasty performed by another physician, 13 patients (18.6%) were classified as having tension nose and only 1 (1.4%) patient had congenital tip deformity. There were no cases of postoperative functional complaints (Figure 5).
Figure 5.
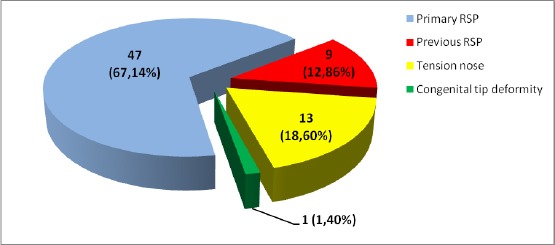
Preoperative data in patients who had rhino/septoplasty
The operative procedures included full-transfixion incision, release of tension septum, lateral crural overlay (LCO) in 12 (17%) of patients, dome truncation in 12 (17%) of patients, medial crural overlay (MCO) in 12 (20%) of patients and combinations of both techniques were performed in 32 (46%) of patients (Figure 6).
Figure 6.
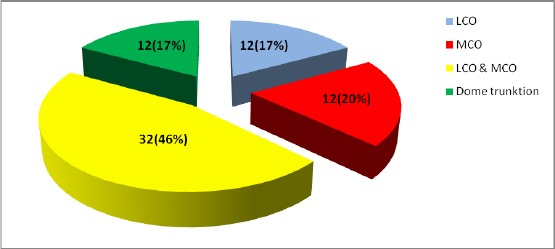
Operative procedures
In further medical attention in the postoperative period, we made major and minor secondary revision procedures, monitored for postoperative complications, and any functional complaints. We followed-up the patients immediately after the mask/splint removal (one week after the surgical intervention), then two weeks after the intervention when stitches were to be removed, one month after the surgery and six months later when the final results from the surgical intervention rhinoseptoplasty were to be expected. The results obtained are herein presented.
In the postoperative period, we made major and minor secondary revision procedures, monitored for postoperative complications, and any functional complaints. Sixty-three (90%) patients were satisfied without qualification, 3 (4.3%) were not satisfied and went for revision surgery, 2 (2.9%) patients underwent radix graft after the first rhinoseptoplasty, and 2 (2.9%) of the patients wanted to have minor revision of the dorsal irregularities (Figure 7).
Figure 7.
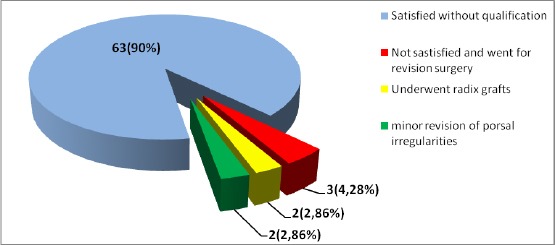
Further medical attention in the postoperative period
Case study
Case 1: Rhinokyphosis (nasal septal deviation) DSN. Closed approach, reducing of the nasal hump, rasping of the dorsum, medial and lateral osteotomy, septal medioposition, resection of lateral alar cartilages for alar rim grafts, tip reconstruction with dome suturing (Fig. 8).
Figure 8.

Rhinokyphosis, (nasal septal deviation) DSN
Case 2: “Pinocchio” nose, Rhinokyphosis, DSN, closed approach, reducing of the nasal hump, rasping of the dorsum, medial and lateral osteotomy, septal medioposition, resection of lateral alar cartilages for alar rim grafts, tip reconstruction with dome suturing (Fig. 9).
Figure 9.

“Pinocchio” nose
Case 3: Overprojected nose. Rhinokyphosis, DSN. Closed approach, reducing of the nasal hump, rasping of the dorsum, medial and lateral osteotomy, septal medioposition, resection of lateral alar cartilages for alar rim grafts, tip refinement (Fig. 10).
Figure 10.

Overprojected nose
Case 4: Overprojection nose, DSN. Closed approach, the rasping of the dorsum, medial and lateral osteotomy, septal medioposition, resection of lateral alar cartilages for alar rim grafts, tip reconstruction with dome suturing (Fig. 11).
Figure 11.

Overprojection nose, DSN
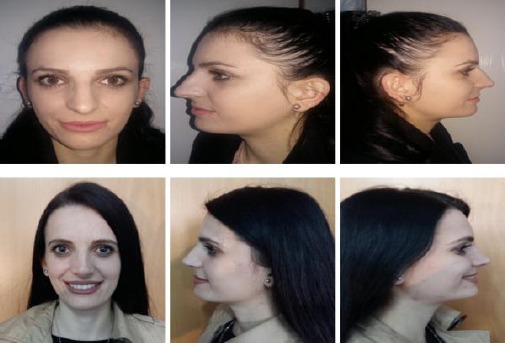
Case 5: Overprojected nose. Rhinokyphosis, DSN. Closed approach, reducing of the nasal hump, rasping of the dorsum, medial and lateral osteotomy, septal medioposition, resection of lateral alar cartilages for alar rim grafts, tip refinement (Fig. 12).
Figure 12.

Overprojected nose
Case 6: Overprojection nose, DSN. Closed approach, the rasping of the dorsum, medial and lateral osteotomy, septal medioposition, resection of lateral alar cartilages for alar rim grafts, refinement of the nasal tip (Fig. 13).
Figure 13.
Overprojection nose, DSN
Discussion
Surgery of over projecting nose has become significantly more complex since the introduction of tip grafting and the many suture designs that followed open rhinoplasty. Two nasal tip features require mandatory preoperative identification: whether the tip is adequately projecting and whether the alar cartilage lateral crura are orthotopic or cephalically rotated (malpositioned).
According to literature, only 33% of the patient population have adequate preoperative tip projection, and only 54% have inadequate lateral crura, whereas 46% of the patients have lateral crura cephalically rotated [29], [30], [31], [32].
Numerous authors have (pointed to the tripod theory and) suggested that when the medial crura are shortened about the lateral crura, there is a high tendency for alar flaring. However, this was not the case with our patients when we used MCO. When MCO was used alone, no cases needed alar base reduction. Even more surprising was our finding that in our entire experience with deprojection, only 7.5% of the patients needed alar base reduction, and many of these patients desired this reduction before deprojection [33], [34], [35], [36].
The surgeon can reduce excessive tip support mechanisms, reduce overdeveloped anatomic components, and normalise adjacent anatomic components.
As with any rhinoplasty, tip asymmetries can arise. Compared to literature reports, our revision rate of tip irregularity is low. Also, a larger number of patients have been satisfied with the operative procedure undertaken, and there has been no nasal obstruction. Being satisfied with the esthetic appearance, patients recovered their self-confidence and showed better social adaptation [37], [38], [39], [40].
In conclusion, from an aesthetic point of view, this type of operative procedure is superior in resolving over projected nose.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
References
- 1.Perkins SW. Anatomy and Physiology. In: Krause ChJ., editor. Aesthetic facial surgery. Philadelphia: Lippincott Company; 2003. [Google Scholar]
- 2.Pirsig W, Kern EB, Verse T. Reconstruction of anterior nasal septum:back-to-back autogenous ear cartilage graft. Laryngoscope. 2004;114:627–638. doi: 10.1097/00005537-200404000-00007. https://doi.org/10.1097/00005537-200404000-00007 PMid:15064615. [DOI] [PubMed] [Google Scholar]
- 3.Rettinger G. Aktuelle Aspekte der Septorinoplastik. Otorhinolaryngol Nova. 2005;84:2–42. [Google Scholar]
- 4.Samad I, Stevens HE, Maloney A. The Efficacy of nasal septal surgery. J Otolaryngol (Canada) 1992;21:88–91. [PubMed] [Google Scholar]
- 5.Silver WE, Zuliani GF. Management of the overprojected nose and ptotic nasal tip. Aesthet Surg J. 2009;29(3):253–8. doi: 10.1016/j.asj.2009.01.020. https://doi.org/10.1016/j.asj.2009.01.020 PMid:19608076. [DOI] [PubMed] [Google Scholar]
- 6.Kridel RW, Konior RJ. Dome truncation for management of the overprojected nasal tip. Ann Plast Surg. 1990;24(5):385–96. doi: 10.1097/00000637-199005000-00001. https://doi.org/10.1097/00000637-199005000-00001 PMid:2350149. [DOI] [PubMed] [Google Scholar]
- 7.Sands NB, Adamson PA. Nasal tip deprojection with crural cartilage overlap:the M-arch model. Facial Plast Surg Clin North Am. 2015;23(1):93–104. doi: 10.1016/j.fsc.2014.09.007. https://doi.org/10.1016/j.fsc.2014.09.007 PMid:25430931. [DOI] [PubMed] [Google Scholar]
- 8.Sykes JM. Management of the middle nasal third in revision rhinoplasty. Facial Plast Surg. 2008;24(3):339–47. doi: 10.1055/s-0028-1083087. https://doi.org/10.1055/s-0028-1083087 PMid:18951320. [DOI] [PubMed] [Google Scholar]
- 9.Gubisch W, Eichhorn-Sens J. The sliding technique:a method to treat the overprojected nasal tip. Aesthetic Plast Surg. 2008;32(5):772–8. doi: 10.1007/s00266-008-9211-1. https://doi.org/10.1007/s00266-008-9211-1 PMid:18661172. [DOI] [PubMed] [Google Scholar]
- 10.Foda HM. Alar setback technique:a controlled method of nasal tip deprojection. Arch Otolaryngol Head Neck Surg. 2001;127(11):1341–6. doi: 10.1001/archotol.127.11.1341. https://doi.org/10.1001/archotol.127.11.1341 PMid:11701071. [DOI] [PubMed] [Google Scholar]
- 11.Funk E, Chauhan N, Adamson PA. Refining vertical lobule division in open septorhinoplasty. Arch Facial Plast Surg. 2009;11(2):120–5. doi: 10.1001/archfacial.2008.527. https://doi.org/10.1001/archfacial.2008.527 PMid:19289685. [DOI] [PubMed] [Google Scholar]
- 12.Pedroza F, Pedroza LF, Achiques MT, Felipe E, Becerra F. The tripod graft:nasal tip cartilage reconstruction during revision rhinoplasty. JAMA Facial Plast Surg. 2014;16(2):93–101. doi: 10.1001/jamafacial.2013.2348. https://doi.org/10.1001/jamafacial.2013.2348 PMid:24458140. [DOI] [PubMed] [Google Scholar]
- 13.Gubisch W, Eichhorn-Sens J. Overresection of the lower lateral cartilages:a common conceptual mistake with functional and aesthetic consequences. Aesthetic Plast Surg. 2009;33(1):6–13. doi: 10.1007/s00266-008-9267-y. https://doi.org/10.1007/s00266-008-9267-y PMid:19037690. [DOI] [PubMed] [Google Scholar]
- 14.Alexander AJ, Shah AR, Constantinides MS. Alar retraction:etiology, treatment, and prevention. JAMA Facial Plast Surg. 2013;15(4):268–74. doi: 10.1001/jamafacial.2013.151. https://doi.org/10.1001/jamafacial.2013.151 PMid:23619765. [DOI] [PubMed] [Google Scholar]
- 15.Menick FJ. Aesthetic and reconstructive rhinoplasty:a continuum. J Plast Reconstr Aesthet Surg. 2012;65(9):1169–74. doi: 10.1016/j.bjps.2012.04.017. https://doi.org/10.1016/j.bjps.2012.04.017 PMid:22554677. [DOI] [PubMed] [Google Scholar]
- 16.Givens V, Sykes J. The Tripoid Concept of the Upper Nasal Third. Facial Plast Surg. 2019;21(6):498–503. doi: 10.1001/jamafacial.2019.0884. https://doi.org/10.1001/jamafacial.2019.0884 PMid:31647524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Menick FJ, Salibian A. Primary intranasal lining injury cause, deformities, and treatment plan. Plast Reconstr Surg. 2014;134(5):1045–56. doi: 10.1097/PRS.0000000000000694. https://doi.org/10.1097/PRS.0000000000000694 PMid:25347637. [DOI] [PubMed] [Google Scholar]
- 18.Weber SM, Baker SR. Management of cutaneous nasal defects. Facial Plast Surg Clin North Am. 2009;17(3):395–417. doi: 10.1016/j.fsc.2009.05.005. https://doi.org/10.1016/j.fsc.2009.05.005 PMid:19698919. [DOI] [PubMed] [Google Scholar]
- 19.Soliemanzadeh P, Kridel RW. Nasal tip overprojection:algorithm of surgical deprojection techniques and introduction of medial crural overlay. Arch Facial Plast Surg. 2005;7(6):374–80. doi: 10.1001/archfaci.7.6.374. https://doi.org/10.1001/archfaci.7.6.374 PMid:16301456. [DOI] [PubMed] [Google Scholar]
- 20.Solomon P, Rival R, Mabini A, Boyd J. Transfixion incision as an initial technique in nasal tip deprojection. Can J Plast Surg. 2008;16(4):224–227. doi: 10.1177/229255030801600412. https://doi.org/10.1177/229255030801600412 PMid:19949502 PMCid:PMC2691028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huizing E. Implantation and transplantation in reconstructive nasal surgery. Rhinology. 1974;12:93–106. [PubMed] [Google Scholar]
- 22.Huizing E, de Groot JAM. Functional reconstructive nasal surgery. Thieme; 2003. https://doi.org/10.1055/b-0034-40789. [Google Scholar]
- 23.Tardy ME, Jr, et al. Micro-osteotomy in Rhinoplasty. Facial Plast Surg. 1984;1:137–145. 29. https://doi.org/10.1055/s-0028-1085244. [Google Scholar]
- 24.Jacobson WE, et al. Psychiatric evaluation of male patients seek in cosmetic surgery. Plast. Reconstr. Surg. 1950;26:356. doi: 10.1097/00006534-196010000-00003. https://doi.org/10.1097/00006534-196010000-00003 PMid: 13718613. [DOI] [PubMed] [Google Scholar]
- 25.Killian G. The submucous window resection of the nasal septum. Ann Otol Rhinol Laryngol. 1905;14:363. https://doi.org/10.1177/000348940501400210. [Google Scholar]
- 26.Lemmens W, Lemkens P. Septal suturing following nasal septoplasty, a valid alternative for nasal packing. Acta Otorhinolaryngol Belg. 2001;55:215–221. [PubMed] [Google Scholar]
- 27.Mladina R, Krajina Z. The influence of the caudal process on the formation of septal deformities. Rhinology. 1999;27:113–118. [PubMed] [Google Scholar]
- 28.Seltzer A. The nasal septum:plastic repair of the deviated septum associated with deflected tip. Arch Otolaryngol. 1996;40:433–444. https://doi.org/10.1001/archotol.1944.00680020563001. [Google Scholar]
- 29.Rettinger G, Steininger H. Lipogranulomas as Complications of Septorhinoplasty. Arch Otolaryngol Head Neck Surg. 1997;123:809–814. doi: 10.1001/archotol.1997.01900080041003. https://doi.org/10.1001/archotol.1997.01900080041003 PMid:9260544. [DOI] [PubMed] [Google Scholar]
- 30.Rettinger G, Kirsche H. Complications in septoplasty. Facial Plast Surg. 2006;22:289–297. doi: 10.1055/s-2006-954847. https://doi.org/10.1055/s-2006-954847 PMid:17131271. [DOI] [PubMed] [Google Scholar]
- 31.Tardy ME, Jr, Kron TK, Younger R, Key M. The Cartilaginous Pollybeak:Etiology, Prevention, and Treatment. Facial Plast Surg. 1989;6:113–120. doi: 10.1055/s-2008-1064718. https://doi.org/10.1055/s-2008-1064718 PMid:2487866. [DOI] [PubMed] [Google Scholar]
- 32.Murakami CS, Larrabee WF., Jr Comparison of Osteotomy Techniques in the Treatment of Nasal Fractures. Facial Plast Surg. 1992;8:209–219. doi: 10.1055/s-2008-1064652. https://doi.org/10.1055/s-2008-1064652 PMid:1286831. [DOI] [PubMed] [Google Scholar]
- 33.Sheen JH. Spreader Graft:A Method of Reconstructing the Roof of the Middle Nasal Vault Following Rhinoplasty. Plastic and Reconstructive Surgery. 1984;73(2):230–239. https://doi.org/10.1097/00006534-198402000-00013. [PubMed] [Google Scholar]
- 34.Toriumi DM, Josen J, Weinberger M, Tardy ME Jr. Use of Alar Batten Grafts for Correction of Nasal Valve Collapse. Arch Otolarnygol Head Neck Surg. 1997;123:802–808. doi: 10.1001/archotol.1997.01900080034002. https://doi.org/10.1001/archotol.1997.01900080034002 PMid:9260543. [DOI] [PubMed] [Google Scholar]
- 35.Menger DJ. Lateral Crus Pull-up. Arch Facial Plast Surg. 2006;8:333–337. doi: 10.1001/archfaci.8.5.333. https://doi.org/10.1001/archfaci.8.5.333 PMid:16982991. [DOI] [PubMed] [Google Scholar]
- 36.McCollough EG, Mangat D. Systematic Approach to Correction of the Nasal Tip in Rhinoplasty. Arch Otolaryngol. 1981;107:12–6. doi: 10.1001/archotol.1981.00790370014002. https://doi.org/10.1001/archotol.1981.00790370014002 PMid:7469873. [DOI] [PubMed] [Google Scholar]
- 37.Adamson PA, Litner JA. Applications of the M-arch Model in Nasal Tip Refinement. Facial Plast Surg. 2006;22:42–48. doi: 10.1055/s-2006-939951. https://doi.org/10.1055/s-2006-939951 PMid:16732503. [DOI] [PubMed] [Google Scholar]
- 38.Adamson PA, Funk E. Nasal tip dynamics. Facial Plast Surg Clin North Am. 2009;17:29–49. doi: 10.1016/j.fsc.2008.09.008. https://doi.org/10.1016/j.fsc.2008.09.008 PMid:19181279. [DOI] [PubMed] [Google Scholar]
- 39.Byrd HS, Andochick S, Copit S, Walton KG. Septal Extension Grafts:A Method of Controlling Tip Projection Shape. Plast Reconstr Surg. 1997;100:999–1010. doi: 10.1097/00006534-199709001-00026. https://doi.org/10.1097/00006534-199709001-00026 PMid:9290671. [DOI] [PubMed] [Google Scholar]


