Abstract
Agriculture is an important occupation in Malaysia that generates a major portion of the national revenue. Similar to the rest of the world, pesticides are used to boost agricultural production in Malaysian farms. However, chemical pesticides are associated with human health hazard and are not environment-friendly as they persist in nature for long periods of time. Therefore, pesticide use should be reduced and farmers should be trained on correct and/or alternative ways of pesticide use. In this cross-sectional study, we surveyed 19 palm oil plantations in the Sabah district of Malaysia and evaluated the perception of the workers towards pesticide use and awareness regarding the health effects post-pesticide exposure. Analysis of the survey shows that most of the workers among the 270 respondents were 30-year-old males with average education, and belonged to the low income group. Majority opined that they were aware of the health hazards of pesticide use and suffered from symptoms (with mean duration of three days) such as vomiting, diarrhea, skin irritation, and dizziness. Surprisingly, the opinion was almost equally divided on whether they perceived pesticides to be the cause of their health problems, and a major percentage did not avail medical help. Most of the workers responded that they did not receive any training in pesticide handling and used partial personal protective equipment (glasses, hats, shirt, and gloves) during working hours. Interestingly, a large percentage responded that they would not read the safety material even if it was provided. These observations clearly highlight the urgency of improving the awareness, education, and attitude of these plantation workers towards the short- and long-term effects of pesticide use. They should also be educated about alternative and eco-friendly ways of farming. Finally, the plantation management should intervene and proactively advocate the use of safe farming practices.
Keywords: chemical pesticides, human health hazard, neurobehavioral alterations, plantation management, Malaysia
Introduction
Agriculture is one of the largest sources of livelihood worldwide. Owing to population explosion and the demand for high quality and cosmetically superior food products, recent years have seen an increase in the use of pesticides in the agriculture sector. Pesticides are chemicals used for controlling pests and weeds, and include herbicides, insecticide, fungicide, antimicrobials, rodent repellants, etc. (US Environmental, 2007; Randall et al., 2013; Hillocks, 2012). Most pesticides are used as plant protection agents that protect plants/crops from weeds, fungi, and insects. However, pesticides adversely affect human health, and cause acute and delayed symptoms in exposed people (Hillocks, 2012). Although people are aware of the short-term effect of these pesticides, knowledge regarding its long-term effects is limited. Praneet Vatakul et al. (2013) showed that regular exposure to pesticides can cause serious health issues such as asthma, sperm count reduction, decline in sperm quality, psoriasis, and dermatitis. A systematic review showed that non-Hodgkin lymphoma and leukemia are positively associated with pesticide exposure and suggested that cosmetic use of pesticides should be decreased (Bassil et al., 2007). A growing body of evidence indicates associations between organophosphate insecticide exposure and neurobehavioral alterations (Jurewicz & Hanke, 2008; Weselak et al., 2007; Wigle et al., 2008; Mink et al., 2011). Limited evidence also exist for other negative outcomes from pesticide exposure including neurological defects, birth defects and fetal death (Sanborn et al., 2007).The Food and Agriculture Organization of the United Nations (FAO, 2016) has attempted to control the use of pesticides with its code of conduct by promoting pesticides that require little personal protective equipment. Moreover, the World Health Organization (WHO) has formulated a Recommended Classification of Pesticides by Hazard by categorizing pesticides according to their health hazard, ranging from “extremely hazardous” to “unlikely to present acute hazard”. This is a very useful tool, especially for developing countries, for eliminating extremely toxic pesticides (WHO, 2016).
Pesticides have seen tremulous times in Malaysia. Since organic produce is being promoted globally, pesticide usage is gradually being reduced. The Malaysian government banned the use of Paraquatin 2002, which affected the entire agricultural industry, including Syngenta Malaysia Limited, the largest producer of Paraquat. However, the ban was lifted by the government in 2006 to facilitate an in-depth study on the multiple uses of Paraquat (Watts, 2011). In a detailed survey, Srinivasan (2003) observed that Malaysian farmers are against the ban as they believed that these chemicals are essential for quality farming. The study showed that the farmers were aware of the health and environmental hazards caused by pesticide, in particular, poisonous pesticides like Paraquat and agreed that safe practices should be adopted for pesticide use. However, they believed that an alternative to pesticides should be developed before final banning of such products (Srinivasan, 2003).
The Department of Occupational Safety and Health (DOSH) under the Ministry of Human Resources of Malaysia had recorded 2,648 cases of occupational poisoning and disease in the year 2014, whereas the number stood at 2,588 in 2013, which indicates a rising trend of occupational diseases due to poor working conditions and lack of proper control measures in Malaysia. However, most of the workers are unaware or negligent about the adverse health effects of prolonged pesticide exposure.
Thus, the aim of the study is to understand the perception of farmers towards pesticide use and evaluate the effect of pesticides on worker health. The study will also discuss the clinical issues associated with incorrect pesticide use and investigate whether farmers are aware about these effects. We focused on the palm oil plantations of Papar in the Sabah district of Malaysia, as palm oil is one of the most important agricultural products that have contributed to the economic development of the country. Use of pesticides such as Paraquat in palm oil plantations has eliminated the practice of manual weeding and enabled farmers to focus more on other aspects of farming and marketing. Thus, the response and attitude of palm oil plantation workers and owners is critical for understanding the trend in pesticide use and awareness in Malaysia.
METHODS
Study design
This is a cross-sectional study covering 19 palm oil plantations in Papar, Sabah district of Malaysia, aimed at understanding the pesticide awareness of the plantation workers and its relationship with various demographic, educational, and socio-economic factors.
Study population
The workers in the 19 palm oil plantations were the target of this survey. In total, 950 workers (50 in each plantation) were targeted for the survey.
Inclusion and exclusion criteria
Workers who directly worked with pesticides for minimum six months irrespective of gender and age in any plantation in Papar were included in the study. Workers who were not exposed to pesticide or exposed for less than six months and administrative workers were excluded from the survey.
Sampling method
The random sampling method was adopted for collecting data from the respondents.
Sample size collection
The following formula was used to calculate the sample size:
n ≥ (Z21–α/2xp(1–p))/d2
where α = 0.05 considering 95% confidence level, p is the estimated proportion, and d is the estimated error (0.05 in this case). The prevalence rate is considered as 0.80.
Considering that the total number of workers in 19 plantations is 950 (average 50 workers per plantation), the number of respondents for the sample size was 246. After adding the 10% rate for non-response to the survey questionnaire, the final sample size was 270.
Research data collection methods
We used a survey questionnaire for collecting data from the workers, whereas direct recorded interviews were used for obtaining the views of the plantation managers. The questionnaire was individually administered to the respondents, and was read out in cases where the respondent was not educated enough to complete the survey without assistance.
The survey questionnaire had five parts, namely, demographic profile of the workers, methods of applying pesticides, use of safety measures while applying pesticides, health profile, and perception about the environmental effects of pesticide usage. The questionnaire was translated into Bahasa Melayu by an expert translator and reversely translated to English after completion of the survey. Afterwards, the questionnaires were pre-tested with 40 respondents, where they were asked whether they understood the appropriateness of questions and their relevance to the community; changes to answers, if any, were incorporated in cases of misunderstanding. The corrected and validated questionnaire was used in the study.
Data collection
Four teams of five members each collected the data. All the teams adhered to a standard method of data collection, and they were also briefed on ethical and soft skill methods to smoothly expedite the process.
Data analysis
Data was analyzed using Microsoft Excel and the SPSS software.
Ethical issues
The respondents were informed about the aim of the research. The information was kept confidential and the respondents were never pressurized into participating in the survey or expressing desired views. No monetary or non-monetary incentives were provided to the respondents. All respondents provided informed consent for their participation. All the plantation managers/owners were personally met and verbal consent was obtained before starting the data collection.
RESULTS
Socio-demographic factors
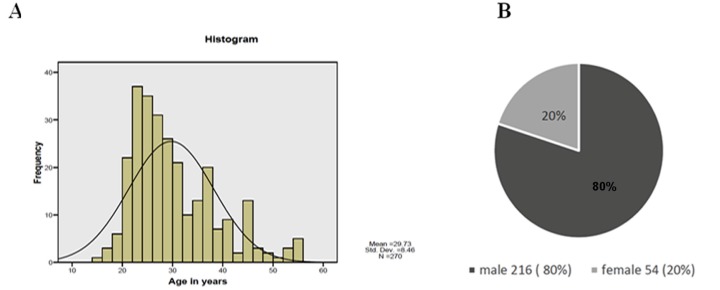
Age and gender: The respondents belonged to different age groups (15–55 years), with 21–35 year-old workers being mainly represented in the survey. The mean age of the respondents was 30 years (Figure 1A). Gender wise, male respondents were in majority (80%) (Figure 1B).
Figure 1.
(A) Age distribution and (B) gender distribution of palm oil workers in Papar, Sabah, Malaysia.
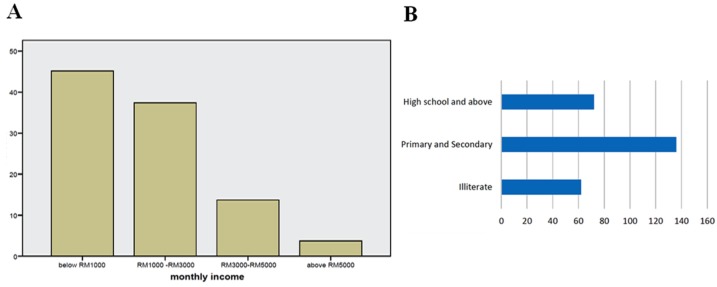
Economic status: The income group statistics presented a mix of all income groups. Some workers owned the farm and hence had higher income, although 82.6% workers belonged to the low-income group, with the income below 3000 Rm (Figure 2A).
Figure 2.
(A) Income distribution and (B) education level of palm oil workers in Papar, Sabah, Malaysia.
Education: Approximately 23% respondents were illiterate, 50.4% could read and write (basic primary school education), and only 26.6% had high school education (Figure 2B).
Pesticide-associated factors
Exposure time: The respondents were exposed to pesticides for a minimum of seven months and maximum of 40 months, with 18.9 months of mean duration of pesticide exposure (Table 1).
Table 1.
Questionnaire and socio-demographic data.
| S No. | Title | Question | Response | |
|---|---|---|---|---|
| 01 | Pesticide application duration. | Duration of applying pesticide? | Minimum 07 months | |
| Maximum 40 months | ||||
| Mean | 18.9 months | |||
| Standard Deviation | 9.7 months | |||
| 02 | Assessment of mixed pesticide usage from the survey questionnaire. | Mix different brands of pesticide? | Yes | 270 |
| No | 0 | |||
| 03 | Perception of pesticide exposure risk awareness from survey questionnaire. | How much risk do you think you are exposed to while using the pesticides? | No risk at all | 16 |
| There is risk | 254 | |||
| Total | 270 | |||
| 04 | Duration of medical symptoms after pesticide exposure. | After how many days of pesticide exposure you have developed the symptoms? | Mean | 3days |
| Standard Deviation | ±0.9 | |||
| 05 | Perception on effects of pesticide use. | Can this usage of pesticide cause any kind of long term or short term health effect? | No effect | 38 (14.1%) |
| I don’t know | 13 (4.8%) | |||
| There is effect | 219 (81.1%) | |||
| 06 | Turn-around time for entering field. | How long duration after applying pesticide do you re-enter the field? | Range | 12–16 hours |
| Mean | 14.8 | |||
| Standard Deviation | ±1.272 | |||
| 07 | Assessment of skin contact with pesticide during pesticide application. | During mixing the pesticide does any part of your body come in contact with the liquid? | Yes | 188 |
| No | 70 | |||
| 08 | Perception on effect of pesticides on the environment | Did you observed any dead animals, frogs, birds, and insects in or around field? | Yes | 178 (64.8%) |
| No | 92 (35.2%) | |||
Mixing of pesticide brands: All the respondents agreed to mixing different brands of pesticide (Table 1). Paraquat was majorly used by most of the farmers.
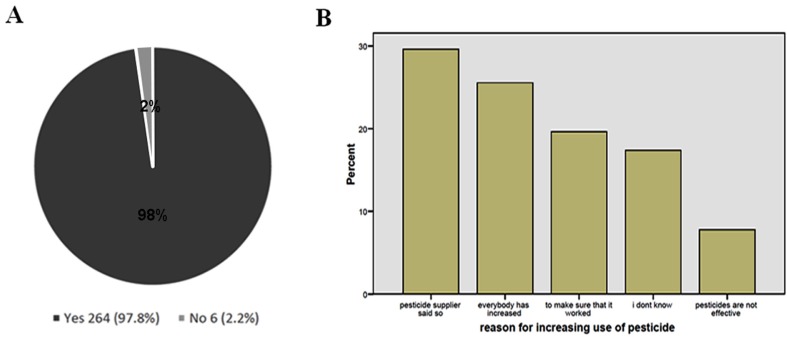
Frequency of pesticide use: Majority (97.8%) of the respondents agreed that the usage of pesticide has increase over time (Figure 3A). The main reasons were: (a) they were told to do so by the manager or pesticide supplier (29.6%) and (b) everybody else had increased (25.6%) pesticide usage (colleague or another plantation) (Figure 3B).
Figure 3.
Frequency of pesticide use.
Risk awareness of pesticide exposure: Surprisingly, 94.1% respondents agreed that they were aware of the risks and toxic side-effects of pesticide usage (Table 1).
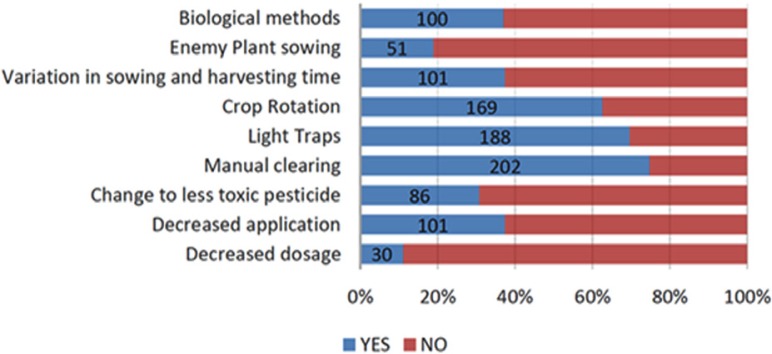
Alternatives to pesticides: Awareness about the following alternatives to pesticide use was probed: decreased dosage of existing pesticides, decreased application of pesticides and change to less toxic pesticides, manual clearing, use of light traps and crop rotation, variation in sowing and harvesting time, cultivation of “enemy” plants, and use of biological methods of pest control. Among these, the workers preferred the use of manual clearing (74.8%), crop rotation (62.6%), and light traps (69.6%), whereas the percentage of workers who preferred using the other alternatives was low (Figure 4).
Figure 4.
Alternative pest control methods.
Health effects of pesticides
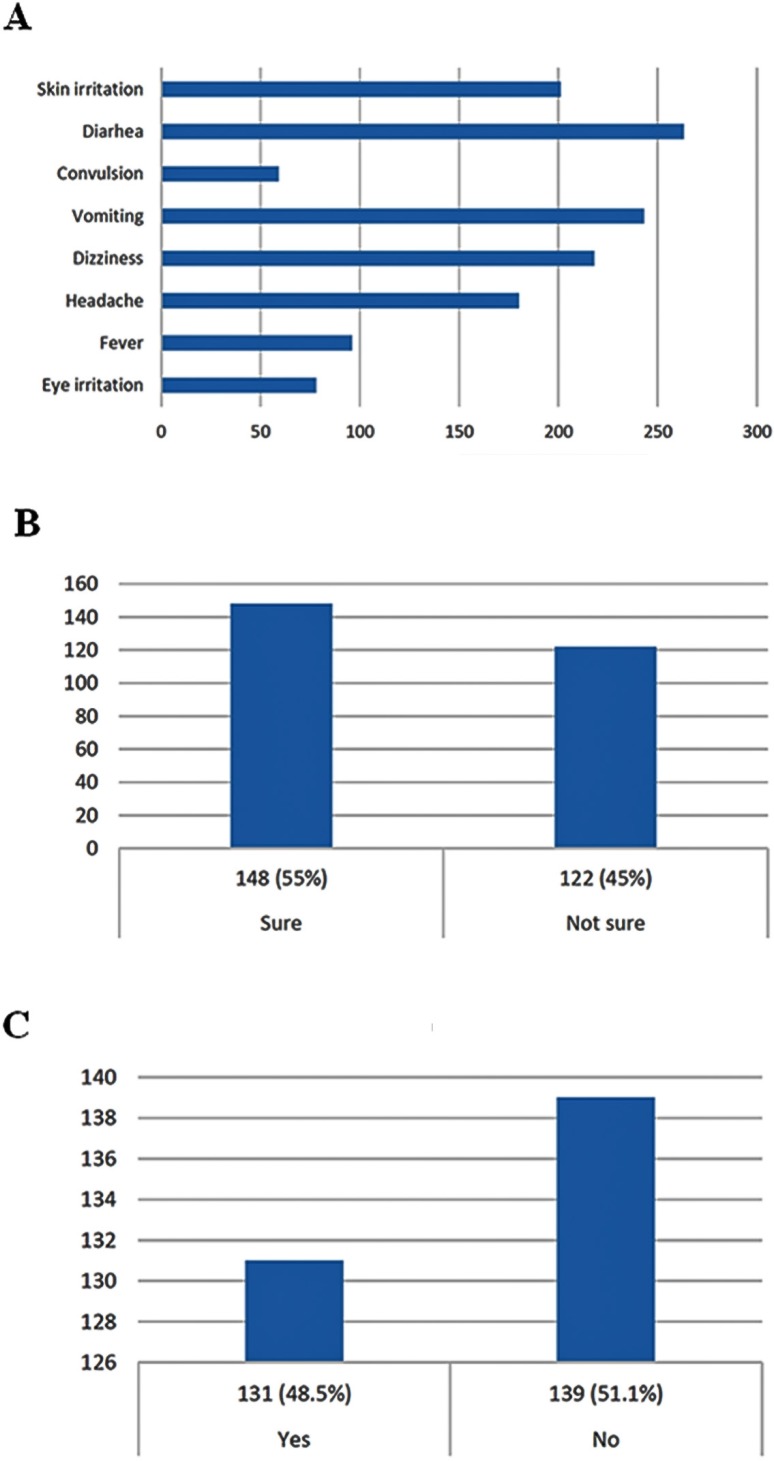
All the workers mentioned suffering from at least one type of ailment during the course of pesticide usage. Skin irritation (74.4%), vomiting (90%), diarrhea (97.4%), head ache (66.7%), and dizziness (80.7%) were the most common symptoms, which mostly lasted for three days (± 0.9) (Figure 5A, Table 1). However, opinion regarding the involvement of pesticides in the emergence of these symptoms was divided; 55% of the respondents opined that they were sure that the pesticides were responsible for their ailments, whereas 45% were not sure (Figure 5B). Among these, only 48.5% respondents said that they visited the doctor when ill, which indicated that either they did not have access to basic health care or were averse to availing medical treatment for their condition (Figure 5C).
Figure 5.
Health effects after pesticide exposure.
Perception on effects of pesticide use
When asked whether pesticide use can cause long- or short-term effects, most workers (81.1%) agreed that pesticides exerted harmful effects, whereas 14.1% answered by negative and 4.8% were unsure about the health effects of pesticides (Table 1).
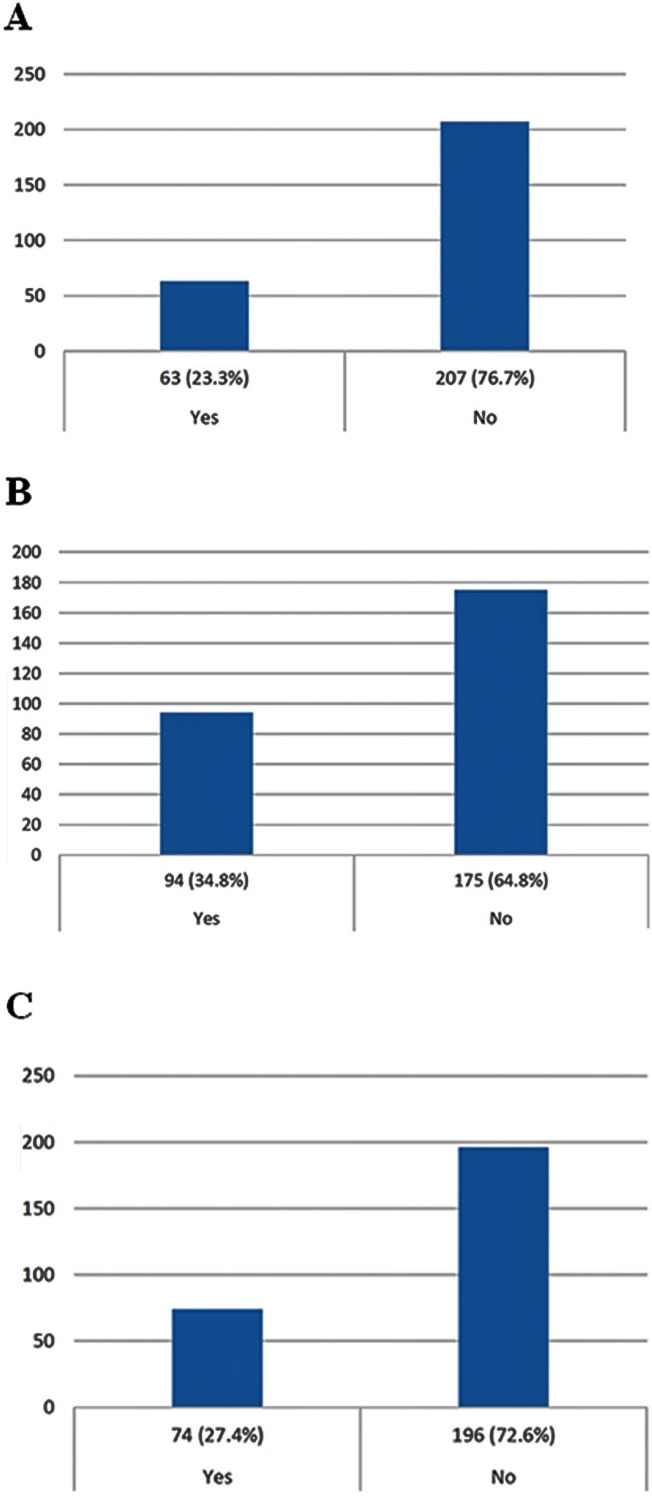
Pesticide handling
Training and attitude: When asked whether they were provided with pesticide handling training, 76.7% respondents said that they did not receive any training prior to pesticide application (Figure 6A) and 68.1% claimed that they were not provided with CSDS or equivalent safety documentation (Figure 6B). The questionnaire further inquired whether the respondents would read the CSDS sheet if it was provided (Figure 6C). Surprisingly 73% claimed that they would not, which shows that attitude also plays a role in safe handling of pesticides.
Figure 6.
Assessment of pesticide handling. (A) training, (B) CSDS availability, (C) willingness to read CSDS.
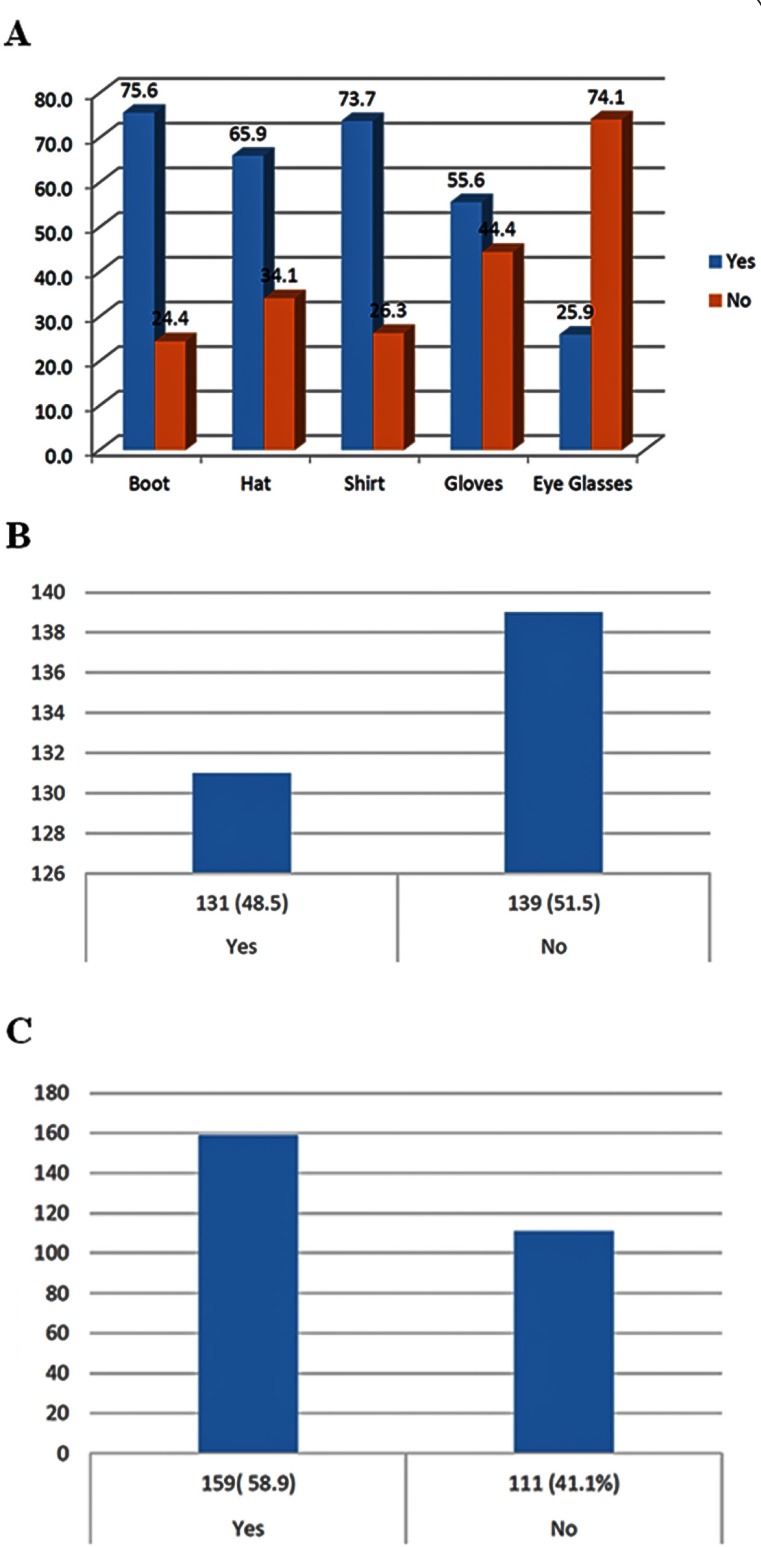
Use of personal protective equipment (PPE): The respondents were asked whether they used safety boots, hats, gloves, shirts, and eyeglasses while working with pesticides. Unfortunately, most respondents wore partial PPE as some PPE items were deemed unnecessary or as sources of uneasiness. Eyeglasses were the least favorite PPE (73.7% did not wear protective glasses), followed by gloves (44.8%) and hat (34.1%) (Figure 7A). A large majority (69.6%) also claimed that the pesticides came in contact with their skin while mixing (Table 1).
Figure 7.
Use of safety and hygiene measures during pesticide handling. (A) personal protective equipment, (B) bathing, and (C) changing clothes.
Hygienic practices after pesticide use: We observed that 51.5% did not bathe (Figure 7B) and 41.4% did not change clothes after using pesticides (Figure 7C), highlighting that awareness about persistence of pesticide residues on the skin was moderate.
Turn-around time for re-entering the field: The turn-around time for re-entering the field ranged between 12–16 h, with a mean of 14.8 h (Table 1).
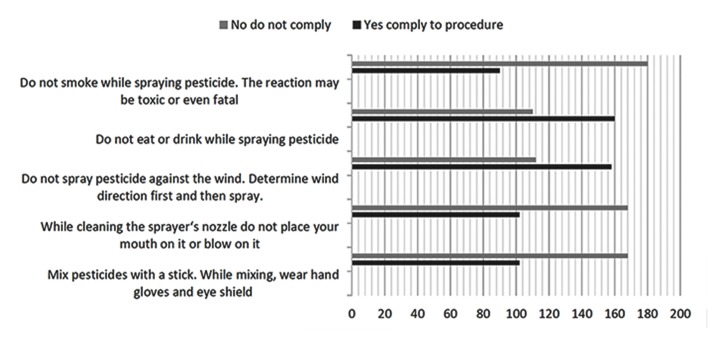
Compliance with standard application procedure: When asked if the workers mixed pesticides with a stick while using full PPE (hand gloves and eye shield) 62.2% responded that they do not comply with this method. Next, they were asked whether they did not place their mouths on the spray nozzle while cleaning, and surprisingly, 62.2% claim they do not comply with this rule. Similarly, 66.7% opined that they did not comply with the “no smoking at work” rule, and 41.5% did not obey the “do not spray against the wind” rule (Figure 8).
Figure 8.
Compliance with standard safety measures while applying pesticides.
Perception on effect of pesticides on the environment
The last part of the questionnaire probed awareness regarding the effect of pesticides on the environment. Respondents were asked whether they had seen any dead animals, birds, and insects at their spraying location, to which 64.8% replied in affirmative (Table 1).
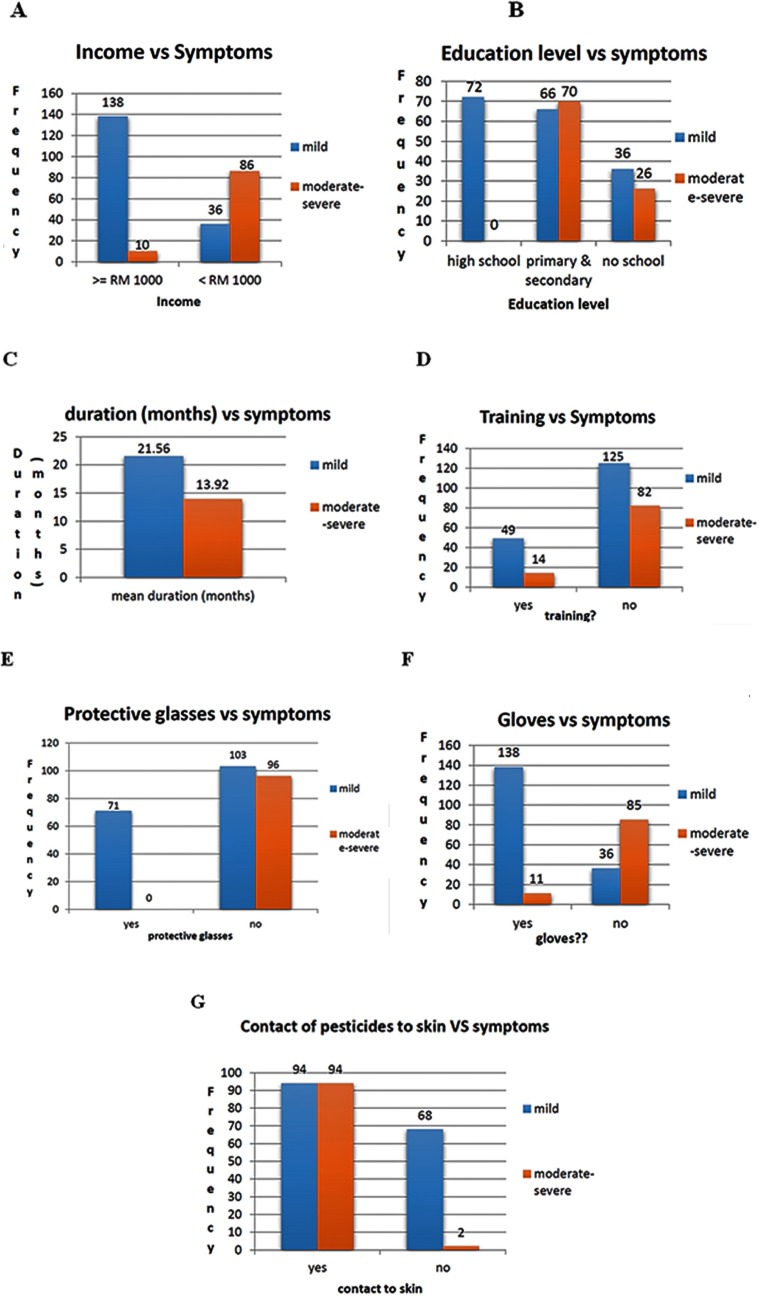
Classification according to severity of symptoms
The respondents were divided into two groups based on the severity of physical ailment symptoms, namely the mild symptom (174 cases) and moderate-severe symptom groups (96 cases). Next, we ascertained the association of various above-mentioned factors with the severity of symptoms using statistical tests. The severity of the symptoms was not significantly associated with gender (data not shown). The chi-square test showed a significant association between the income of the workers and the elicited symptoms, with lesser income being associated with severe symptoms (p=0.000) (Figure 9A). Similarly, there was a significant association between the literacy level of the workers and the severity of symptoms, with higher education being associated with mild symptoms (p=0.000) (Figure 9B). An independent t-test showed that longer duration of pesticide usage was associated with mild symptoms (p=0.000) (Figure 9C), whereas skin contact was directly associated with severe symptoms (Figure 9G). An inverse relationship was observed between training and symptom severity, with trained workers showing lesser symptoms (mild plus severe) than untrained ones (p=0.000) (Figure 9D). Use of PPE (glasses, shirts, and gloves) also correlated with occurrence of milder symptoms (p=0.000) (Figures 9E and F).
Figure 9.
The associations of various factors with the severity of symptoms.
Co-relationship between use of PPE and symptoms
Significant association between the usage of gloves by workers and symptoms were observed post statistical analysis. From the survey it was found that 149 farmers put on the gloves and 121 do not use gloves while handling pesticides. Out of 149 farmers 138 used to develop mild while 11 developed moderate symptoms. In the same way out of 121 gloves non-users, 36 farmers developed mild and 85 developed moderate symptoms. Chi square and probability value were 115.170 and 0.000 respectively. Hence usage of gloves can significantly reduce the occurrence of symptoms in workers. Likewise notable association between the usage of protective shirt and symptoms were found. Usage of protective shirt can reduce the symptoms (Chi-Square test value at 1 degree of freedom was found to be 26.692, and p-value at 5% level of significance was 0.000). Similar result was observed between protective eyeglass and symptom analysis. Chi-Square test value and p value were found to be 53.149 and 0.000 respectively. Hence usage of PEE during pesticide application can reduce the risk of developing symptoms of serious health hazards in farmers.
Discussion
In this cross-sectional study, we surveyed 19 oil palm plantations in the Sabah district of Malaysia and evaluated the perception of the workers towards pesticide use and awareness regarding the health effects post-pesticide exposure. We observed that most of the workers among the 270 respondents were approximately 30-year-old males with average education and belonged to the low income group. The majority opined that they were aware of the health hazards of pesticide use and suffered from symptoms such as vomiting, diarrhea, skin irritation, and dizziness. Surprisingly, the opinion was almost equally divided on whether they perceived pesticides to be the cause of their health problems, and a major percentage did not avail of medical help. Most of the workers responded that they did not receive any training in pesticide handling and used partial personal protective equipment (glasses, hats, shirt, and gloves) during working hours. Interestingly, a large percentage responded that they would not read the safety material even if it was provided. These observations clearly highlight the urgency of improving the awareness, education, and attitude of these plantation workers towards the short- and long-term effects of pesticide use.
Occupational pesticide poisoning is a major health issue among field and agricultural workers, (Hossain, 2010). Previous field studies from Indonesia, India, Vietnam, China, and South Korea have reported that occupational pesticide has a prevalence rate of 8.8% to 31% based on self-reporting, although the study period and definition of poisoning varies between studies (Bertolote et al., 2006). Approximately 200,000–300,000 people die worldwide from pesticide poisoning every year with the majority of deaths occurring in developing countries (Gunnell et al., 2007). Studies in Asian countries have highlighted the use of unauthorized pesticides and a lack of advice on alternatives to pesticide use (Konradsen, 2007), which contributes to pesticide poisoning. Gangemi S et al., 2016, had critically reviewed the effect of pesticides on human health leading to immunotoxicity and the impact of cytokine levels on health, resulting in the development of numerous chronic ailments. In another study Fenga C, et al., 2014, studied the effect of pesticide on the levels of IL-17 and IL-22 in serum of greenhouse workers. They found a significant augment in IL-22 concentration in the exposed subjects compared to controls. This fact confirmed that exposure to pesticide perhaps reduce host defense against cancer and infections. A study was conducted (Costa C et al., 2015) to estimate the common genetic polymorphisms of the paraoxonase 1 (PON1) gene in a group of 55 farmers who were exposed to pesticides. Polymorphism of PON1 gene leads to atherosclerosis. In another experiment by Costa C et al., 2013, immunotoxicity of the synthetic pyrethroid α-cypermethrin (αCYP) was evaluated in 30 green house workers who are occupationally exposed to pyrethroid. It was concluded from the study that pyrethroid exposure in green house may lead to decreased immune system in farmers. Experiment on hair sample by Knipe DW et al., 2016, revealed the presence of diethyl phosphates (organophosphates) in more than 80% of the subjects from rural area of Sri Lanka. This was due to the expose of pesticide in fields. Koureas M et al., 2016, estimated the levels of organochlorine pesticides (OCs) in general population residing in Larissa, Greece. They used optimized headspace solid-phase microextraction GC-MS, to detect and quantify OC levels in serum samples of 103 volunteers. The result revealed the presence of p,p΄-DDE (frequency 99%, median: 1.25 ng/ml) and hexachlorobenzene (frequency 69%, median: 0.13 ng/ml) in the serum samples.
Therefore, the use of pesticides in developing countries should be further investigated and clarified for providing guidance to the respective governments and international organizations during policy making. Many workers in Sabah are small-scale field workers with a property value of less than a few acres per household, who have formed organizations for promoting worker benefits and exchanging knowledge on plantation practices (Rajasuriar et al., 2007).
In most cases, the increase in the percentage of pesticide intoxication is mainly because of the lack of knowledge regarding pesticide exposure, pesticide handling techniques, and misuse (or no use) of protective equipment. (Eddleston et al., 2008). However, Yassin et al. (2002) observed that even though the farmers in the Gaza strip were knowledgeable about the health impact of pesticides, they did not practice safe handling measures. Therefore, change in attitude via intense awareness campaigns should also be considered. Other factors that may be responsible for pesticide poisoning are poor income and educational status, and poor quality of life of the workers.
The majority of oil plantation workers had not received any training and briefing about the harmful effects of pesticides and the preventive measures required to protect themselves and the environment from these effects, which has led to hazardous pesticide management practices. These results corroborate those of Austin et al. (2001), who observed that a large percentage of the laborer class work without any awareness about the hazards and threats associated with their profession. Therefore, training programs for farmers and pesticide applicators should be formulated, and a wide range of media, including radio, newspapers, posters, communication with extension officers, etc. should be used to communicate the relevant information to pesticide users. In addition, educating women, children, and health workers on good stewardship practices may influence pesticide applicators for safe and effective handling of pesticides.
We observed that even though 71% of the workers had received some form of formal education, only 23.3% workers had received training on pesticide management and handling, which corroborates the results of Dasgupta & Meisner (2005) in Bangladesh. In addition, the workers who did not receive training and show moderate-severe ailment symptoms is approximately twice (40%) of those who received training and show moderate-severe symptoms (21%). Therefore, we concluded that training positively affects workers’ health. In addition, education plays a key role in augmenting the understanding of the health risks associated with pesticides. Byrness & Byrness indicated in their 1978 study that education enhances one’s ability to receive, decode and understand information. Therefore, an educated worker would have the intellect to understand the usage and dosage of pesticides and its different components. In contrast, a poorly educated farmer may perform some critical and specialized tasks (e.g. calibration of sprayers, measurement and mixing of pesticides) with difficulty. Since, majority of the oil plantation workers had some form of formal education, there is a likelihood that they will better understand the principles of correct pesticide usage. Anang et al. (2013) and Boateng et al. (2014), reported an increase in the literacy rate and education level among cocoa farmers in Ghana, which might be because of education policy reforms and should also be introduced in the Malaysian system. Our results show that the education level of a worker is significantly associated with the severity of ailment symptoms. Higher education level correlated with awareness regarding the consequences of pesticide application, which decreased the severity of the symptoms.
Correct pesticide handling and post-handling hygiene play important roles in containing pesticide pollution. For example, the majority of the workers do not consider the direction of wind while spraying pesticides, which exposes the farmers to the health risk of pesticide intoxication, as the wind may blow the chemical towards the body, including the face of the farmer. This may also pollute the environment (soil and nearby water bodies) due to spray drift. Ntow et al. (2006) observed that poor spraying practices increased the exposure of farmers to chemicals via both skin contact and inhalation. Disposal of chemical containers, left-over spray solutions, and waste water from sprayer equipment also play important role in dermal pesticide persistence. Farmers commonly dispose empty pesticide containers, unwanted pesticides or left over spray solutions, and the water used for washing spraying equipment in unsafe ways, including disposal near water bodies. This represents a pollution problem for those who drink directly from these water sources as well as aquatic systems which are sources of livelihood for some communities (Antwi-Agyakwa et al., 2013; Lekei et al., 2014; Afari-Sefa et al., 2015).
Operational habits during and after pesticide application, such as scooping or stirring pesticides with bare hands, chewing gum or stick, singing, receiving visitors, talking, removing/ blowing/sucking blockages in sprayer nozzles with mouth, eating, drinking water or alcohol, whistling, and smoking cigarette/tobacco pipes, also determines the extent of pesticide contact with skin/body. These practices readily expose the palm plantation workers to contamination through oral and dermal routes. Similar operational habits during pesticide application have been reported in other studies in developing countries (Lawal et al., 2005; Tijani 2006).
Pesticides enter the human body by inhalation or dermal contact. Therefore, use of PPE during pesticide application has been recommended by the International Labor Organization (ILO) and the World Health Organization (WHO). We observed that majority of the palm oil plantation workers used partial PPE, with use of eyeglasses being the least. Therefore, rigorous training and stringent implementation of safety measures should be considered to improve PPE awareness among the workers, especially because PPE use was inversely related to severity of health symptoms.
In this study, we observed that the pesticide sprayers followed hygiene measures such as changing clothes, washing hands, and showering after spraying pesticides. This contrasts the findings of other studies (Jørs et al., 2008) which documented a low percentage of farmers following appropriate hygiene measures. This difference might be related to availability of water or it might reflect the hygiene behavior of the general population.
We also observed that income plays an important role in deciding the effect of pesticides on worker’s health and the workers’ awareness about such effects. Workers in high income group can either buy better and less toxic pesticides or can purchase bigger land, resulting in an increase in pesticide usage. Furthermore, workers with higher income can purchase safety equipment, avail of higher education, or afford to pay doctor’s fees when ill. Approximately 55% of the plantation workers in this study earn below RM1000 and there is a significant association between household income and the severity of symptoms, indicating that workers with better income have lower chances of developing severe symptoms.
CONCLUSIONS
In conclusion, we found that a sizable population of the working staff of the palm oil plantations was severely affected by pesticide exposure, and the health hazards ranged from mild skin irritations to lung cancer. The following measures should be implemented to stem pesticide poisoning-mediated health problems. First, the industry management should provide the workers with adequate safety measures such as at least two sets of PPE, one of which can be worn when the other one is being sterilized. Proper sterilization procedures must be made available in the campus to facilitate effective cleanup of the pesticide residue. The staff must be put on rotational shifts, in order to prevent over exposure to pesticides. They must be also given adequate leaves and breaks upon sensing any symptoms of pesticide toxicity. Regular health checkups must be made mandatory to identify any symptoms of pesticide poisoning in the early stages, thereby ensuring good health of the workers. Second, the workers should be encouraged to regularly practice hygienic measures after each shift in the field and use protective clothing and equipment irrespective of any inconvenience. Upon any physical discomfort, immediate medical help must be obtained and a break must be sought from work, if required. Overall, extensive educational and training programs have to be initiated to improve the worker’s perception on pesticides and attitude towards use of safe and hygienic measures during and after pesticide application.
REFERENCES
- Afari-Sefa V, Asare-Bediako E, Kenyon L, Micah JA. Pesticide use practices and perceptions of vegetable farmers in the cocoa belts of the Ashanti and Western Regions of Ghana. Adv Crop Sci Tech. 2015;3:174. [Google Scholar]
- Anang BT, Mensah F, Asamoah A. Farmers’ assessment of the government spraying program in Ghana. J Econ Sustain Dev. 2013;4:92–99. [Google Scholar]
- Antwi-Agyakwa AK. Susceptibility of field populations of cocoa mirids,sahlbergella singularis haglund and distantiella theobroma (distant) to bifenthrin. (Unpublished Master’s thesis) Kumasi, Ghana: Kwame Nkrumah University of Science and Technology; 2013. [Google Scholar]
- Austin C, Arcury T, Quandt S, Preisser JS, Cabrera L. Training farmworkers about pesticide safety: issues of control. J Health Care Poor Underserved. 2001;12:236–249. doi: 10.1353/hpu.2010.0744. [DOI] [PubMed] [Google Scholar]
- Antwi-Agyakwa AK, Osekre EA, Ninsin KD, Adu-Acheampong R. Insecticide handling in cocoa production in four regions in Ghana. Journal of Science Education and Technology (Ghana. 2016;36:1–9. [Google Scholar]
- Bassil KL, Vakil C, Sanborn M, Cole DC, Kaur JS, Kerr KJ. Cancer health effects of pesticides: Systematic review. Can Fam Physician. 2007;53:1704–1711. [PMC free article] [PubMed] [Google Scholar]
- Bertolote JM, Fleischmann A, Eddleston M, Gunnell D. Deaths from pesticide poisoning: a global response. Br J Psychiatry. 2006;189:201–203. doi: 10.1192/bjp.bp.105.020834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boateng DO, Nana F, Codjoe Y, Ofori J. Impact of illegal small scale mining (Galamsey) on cocoa production in Atiwa district of Ghana. Int J Adv Agric Res. 2014;2:89–99. [Google Scholar]
- Byrness FC, Byrness KJ. Agricultural extension and education in developing countries. Rural Dev a Chang World. 1978:54–67. [Google Scholar]
- Costa C, Gangemi S, Giambò F, Rapisarda V, Caccamo D, Fenga C. Oxidative stress biomarkers and paraoxonase 1 polymorphism frequency in farmers occupationally exposed to pesticides. Molecular Medicine Reports. 2015;12:6353–6357. doi: 10.3892/mmr.2015.4196. [DOI] [PubMed] [Google Scholar]
- Costa C, Rapisarda V, Catania S, Di Nola C, Ledda C, Fenga C. Cytokine patterns in greenhouse workers occupationally exposed to α-cypermethrIn: an observational study. Environ Toxicol Pharmacol. 2013;36(3):796–800. doi: 10.1016/j.etap.2013.07.004. [DOI] [PubMed] [Google Scholar]
- Dasgupta S, Meisner C. Pesticide traders’ perception of health risks: evidence from Bangladesh. Washington, DC: World Bank Publications; 2005. [Google Scholar]
- Eddleston M, Buckley NA, Eyer P, Dawson AH. Management of acute organophosphorus pesticide poisoning. Lancet. 2008;371:597–607. doi: 10.1016/S0140-6736(07)61202-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food and Agricultural Organization [webpage on the Internet] Food and Agricultural Organization of the United Nations [cited 2016] Retrieved 08 09, 2016. Available from: http://www.fao.org/home/en/
- Fenga C, Gangemi S, Catania S, De Luca A, Costa C. IL-17 and IL-22 serum levels in greenhouse workers exposed to pesticides. Inflamm. Res. 2014;63:895. doi: 10.1007/s00011-014-0769-6. [DOI] [PubMed] [Google Scholar]
- Gangemi S, Gofita E, Costa C, Teodoro M, Briguglio G, Nikitovic D, Fenga C. Occupational and environmental exposure to pesticides and cytokine pathways in chronic diseases (Review) International Journal of Molecular Medicine. 2016;38(4):1012–1020. doi: 10.3892/ijmm.2016.2728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D, Eddleston M, Phillips MR, Konradsen F. The global distribution of fatal pesticide self-poisoning: systematic review. BMC Public Health. 2007;7:357. doi: 10.1186/1471-2458-7-357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hillocks R. Farming with fewer pesticides: EU pesticide review and resulting challenges for UK agriculture. Crop Prot. 2012;31:85–93. [Google Scholar]
- Hossain F. Effects of pesticide use on semen quality among farmers in rural areas of Sabah, Malaysia. J Occup Health Psychol. 2010;52:353–360. doi: 10.1539/joh.l10006. [DOI] [PubMed] [Google Scholar]
- Jørs E, Morant RC, Aguilar GC, Huici O, Lander F, Baelum J, Konradsen F. Occupational pesticide intoxications among farmers in Bolivia: a cross-sectional study. Environ Health. 2006;2006(21):5–10. doi: 10.1186/1476-069X-5-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jurewicz J, Hanke W. Prenatal and childhood exposure to pesticides and neurobehavioral development: review of epidemiological studies. Int J Occup Med Environ Health. 2008;21:121–132. doi: 10.2478/v10001-008-0014-z. [DOI] [PubMed] [Google Scholar]
- Knipe D. W, Jayasumana C, Siribaddana S, Priyadarshana C, Pearson M, Gunnell D, Tsatsakis A.M. Feasibility of hair sampling to assess levels of organophosphate metabolites in rural areas of Sri Lanka. Environmental Research. 2016;147:207–211. doi: 10.1016/j.envres.2016.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Konradsen F. Acute pesticide poisoning–a global public health problem. Dan Med Bull. 2007;54:58–59. [PubMed] [Google Scholar]
- Lawal BO, Torimiro DO, Banjo AD, Joda AO. Operational habits and health hazards associated with pesticide usage by cocoa farmers in Nigeria: lessons for extension work. J Hum Ecol. 2005;17:191–195. [Google Scholar]
- Lekei EE, Ngowi AV, London L. Farmers’ knowledge, practices and injuries associated with pesticide exposure in rural farming villages in Tanzania. BMC Public Health. 2014;14:389. doi: 10.1186/1471-2458-14-389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mink PJ, Mandel JS, Lundin JI, Sceurman BK. Epidemiologic studies of glyphosate and non-cancer health outcomes: a review. Regul Toxicol Pharmacol. 2011;61:172–184. doi: 10.1016/j.yrtph.2011.07.006. [DOI] [PubMed] [Google Scholar]
- Ntow WJ, Gijzen HJ, Kelderman P, Drechsel P. Farmer perceptions and pesticide use practices in vegetable production in Ghana. Pest Manag Sci. 2006;62:356–365. doi: 10.1002/ps.1178. [DOI] [PubMed] [Google Scholar]
- Praneetvatakul S, Schreinemachers P, Pananurak P, Tipraqsa P. Pesticides, external costs and policy options for Thai agriculture. Environ Sci Policy. 2013;27:103–113. [Google Scholar]
- Rajasuriar R, Awang R, Hashim SB, Rahmat HR. Profile of poisoning admissions in Malaysia. Hum Exp Toxicol. 2007;26:73–81. doi: 10.1177/0960327107071857. [DOI] [PubMed] [Google Scholar]
- Randall C, Hock W, Crow E, Hudak-Wise C, Kasai J. National Pesticide Applicator Certification Core Manual. Washington, DC: National Association of State Departments of Agriculture Research Foundation; 2013. [Google Scholar]
- Sanborn M, Kerr KJ, Sanin LH, Cole DC, Bassil KL, Vakil C. Non-cancer health effects of pesticides: Systematic review and implications for family doctors. Can Fam Physician. 2007;53:1712–1720. [PMC free article] [PubMed] [Google Scholar]
- Srinivasan P. Paraquat: A Unique Contributor to Agriculture and Sustainable Development [cited 2016 May 25] 2003. Available from: http://paraquat.com/sites/default/files/Paraquat%20a%20unique%20contributor_0.pdf [webpage on the Internet]
- Tijani AA. Pesticide use practices and safety issues: the case of cocoa. Farmers in Ondo State, Nigeria. J Hum Ecol. 2006;19(3):183–190. [Google Scholar]
- US Environmental Protection Agency . Pesticides: Health and Safety. 2007. [PubMed] [Google Scholar]
- US Environmental . What is a pesticide? epa.gov [cited 2007 September 15] 2007. [Google Scholar]
- Watts M. Paraquat [cited 2016 May 28] 2011. Available from: http://www.panna.org/sites/default/files/Paraquat%20monograph%20final%202011-1.pdf.
- Weselak M, Arbuckle TE, Foster W. Pesticide exposures and developmental outcomes: the epidemiological evidence. J Toxicol Environ Health B Crit Rev. 2007;10:41–80. doi: 10.1080/10937400601034571. [DOI] [PubMed] [Google Scholar]
- WHO World Health Organization [cited 2016 September 08] 2016. Available from: http://www.who.int/en/
- Wigle DT, Arbuckle TE, Turner MC, Bérubé A, Yang Q, Liu S, Krewski D. Epidemiologic evidence of relationships between reproductive and child health outcomes and environmental chemical contaminants. J Toxicol Environ Health B Crit Rev. 2008;11:373–517. doi: 10.1080/10937400801921320. [DOI] [PubMed] [Google Scholar]
- Yassin MM, Abu Mourad TA, Safi JM. Knowledge, attitude, practice, and toxicity symptoms associated with pesticide use among farm workers in the Gaza Strip. Occup Environ Med. 2007;59:387–393. doi: 10.1136/oem.59.6.387. [DOI] [PMC free article] [PubMed] [Google Scholar]