Summary
Background
Heterotopic ossification (HO) occurs frequently in the elbow in burn patients, and extends beyond the anatomical structure. HO of the elbow can cause joint contracture and adversely affect activities of daily living.
Currently, there is no effective prophylaxis for HO as the precise underlying mechanism remains unknown. Therefore, there is no choice but to treat HO after it has developed. To date, however, no effective standard treatment has been reported, and therefore treatment methods vary between different facilities. Surgical resection is widely accepted as the only therapeutic option once HO limits functional mobility of the elbow.
Purposes
Based on past reports, we examined our cases and recommend effective therapeutic strategies. We posed the following three questions: (1) Is the surgical intervention effective or detrimental for elbow ankylosis due to HO? (2) What is the best timing for the intervention? (3) What is the most effective postoperative rehabilitation plan?
Methods
We treated three patients with complete ankylosis of the elbow due to HO after severe burn injury using different protocols.
Results
Surgery was performed in two cases and rehabilitation therapy was commenced immediately from the first postoperative day. Both patients showed improvement in the active range of motion in their elbow joints. The other patient did not undergo surgery, and his elbows became fixed in the completely extension position.
Conclusion
Surgical resection is beneficial for elbow ankylosis due to HO after burn injury. Although the exact surgical timing is still controversial, we recommend that surgery should be performed as soon as possible after improving the skin condition around the elbow and confirming the maturation of HO on radiographs. Early rehabilitation and pain control are also important after surgery.
Keywords: Heterotopic ossification, Burn, Surgical resection, Elbow, Rehabilitation, Ectopic bone
Introduction
Heterotopic ossification (HO) occurs frequently in the elbow after burn injury,1, 2 and can cause elbow ankylosis. Surgical resection was suggested to be the only therapeutic option for this condition.3, 5 Based on past reports, we examined our cases and recommend an effective therapeutic protocol for this condition.
Case series
Three patients with burn injuries received surgical debridement and skin grafting several times, including both elbows. Nonsteroidal antiinflammatory agents had been administered orally from the beginning of the hospitalization period. Radiation therapy was not used.
In cases 1 and 2, surgical resection of HO was performed after closure of skin ulcers around the elbow. There were no postoperative complications, and rehabilitation treatments were commenced on the first postoperative day. The patients received passive assisted range of motion exercises, followed by gradual adoption of active exercise.
Case 1
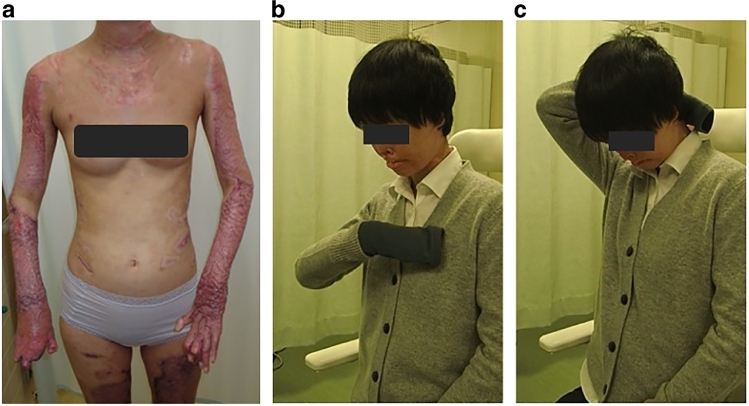
A 20-year-old woman sustained 43% total body surface area (%TBSA) full-thickness flame burn mainly to her face and upper extremities. At 9 weeks post-burn, her elbows were ankylosed in −40° extension position with pain, (Figure 1a) and HO was seen on the extensor side of both elbows on X-rays. (Figures 2a, 3a)
Figure 1.
(a). Nine weeks after the injury. Elbows were ankylosed in extension position. (b), (c): Six months postoperatively. She could touch the anterior chest and the back of her head.
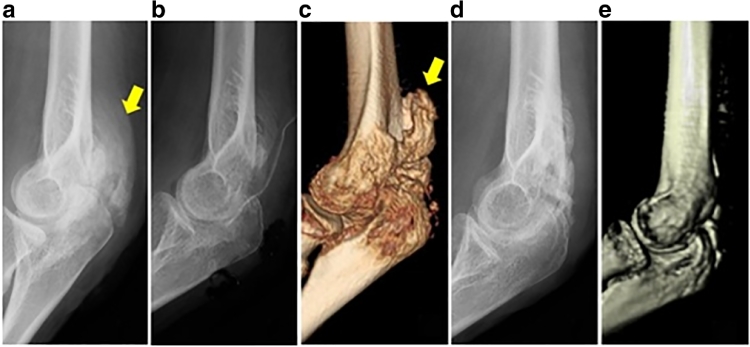
Figure 2.
The progress of the HO on X-ray or Three dimensional computed tomography (3DCT) images of the left elbow. (a). (9 weeks after the injury) The border of HO (yellow arrow) was irregular. (b). (14 weeks after the injury, immediately after the operation) The HO was all resected. (c). (17 weeks after the injury, 3 weeks postoperatively) The HO recurred (yellow arrow). (d). (21 weeks after the injury, 7 weeks postoperatively) The recurrent HO was resolving spontaneously. (e). (30 weeks after the injury, 16 weeks postoperatively) Recurrent HO was absent. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
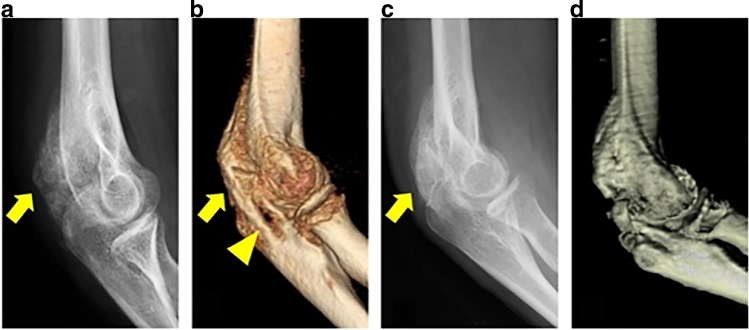
Figure 3.
The progress of the HO on X-ray or 3DCT images of the right elbow. (a). (9 weeks after the injury) The border of HO (the yellow arrow) was irregular. (b). (17 weeks after the injury) A continuous osseous bridge between humerus and ulna (the yellow arrow), and bone resorption of ulnar (the yellow triangle) were seen. (c). (21 weeks after the injury) The well-defined margin of the HO was identified (the yellow arrow). (d). (30 weeks after the injury, 7 weeks postoperatively) No recurrence was seen. (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
Surgery was performed on the left side at 14 weeks post-burn without confirming the maturation of HO on X-rays. The HO was seen to be sparse and soft during the operation. Therefore, it was easy to determine the margins and remove from the normal host bone. The articular capsule was normal.
Surgery was performed on the right side at 23 weeks post-burn after confirming the maturation of HO on X-rays. The HO was hard and similar to the native bone, which made it difficult to determine the margins and expose the ulnar nerve. In addition, HO was seen around the articular capsule, and initial capsulotomy was needed. (Figure 4)
Figure 4.
The right elbow treated surgically at 23 weeks after the injury. After an initial capsulotomy, abnormal macroscopic findings were not found in joint cartilage.
During the immediate postoperative period, her upper extremities were anesthetized with axial nerve block to relieve pain.
Six months postoperatively, the active arc of motion had improved from 0° to 90° (extension −30°, flexion 120°) on the right side and from 0° to 35° (extension −80°, flexion 115°) on the left side. (Figures 1b, 1c)
Case 2
A 20-year-old woman presented with deep dermal and full-thickness burns (50%TBSA). Eight weeks post-burn, the right elbow was ankylosed in 90° flexion position with pain, and HO was seen on the flexor side of the elbow on X-rays.
Surgery was performed at 28 weeks post-burn after confirming the maturation of HO on X-rays. The medial collateral ligament was ossified and the ulnar nerve was embedded in the HO.
Rehabilitation was performed using a continuous passive motion machine. Eighteen months postoperatively, the active arc of motion had improved from 0° to 50° (extension −70°, flexion 120°).
Case 3
A 40-year-old man sustained 40%TBSA full-thickness flame burn injury. Eight weeks post-burn, his elbows were ankylosed in −30° extension position with pain, and HO was seen on the extensor side of the elbow on X-rays.
He was planned to receive surgery after improving general condition and confirming the maturation of HO on radiographs. However, muscle atrophy and joint contracture had progressed beyond our expectation in one year. He was not operated because postoperative improvement of range of motion (ROM) could not be expected. Thereafter, not only his elbows but also his shoulders and knees were ankylosed because of the HO, and he required assistance in daily activities.
Discussion
Clinical features
HO develops clinically and radiologically after median periods of 37 days and 49 days,2 and its formation is promoted by inflammation.4 The clinical symptoms and signs of elbow HO include decreased ROM, joint pain, localized swelling, and ulnar nerve palsy with intrinsic muscle weakness.6 Findings of well-defined HO with no increase in dimensions on X-ray suggest its maturation.7 In addition, since High-frequency spectral ultrasound can visualize HO one week post-burn,8 ultrasound is useful for early diagnosis.
The risk factors for development of HO are greater %TBSA and joint burns, especially requiring skin grafting.2 All our cases required skin grafting on both elbows with over 40%TBSA and could be classified as high-risk group.
Usefulness of surgery
The major structures that cause joint contracture in burn patients are skin, muscle, and the joint capsule.10 HO bridging a joint on radiographs may actually preserve the articular cartilage. 7 Therefore, the ROM of the elbow will be improved once the heterotopic bone and contracted elbow capsule are resected.11
Based on our case 3, with completely ankylosed elbows after conservative care, surgical treatment is desirable when HO limits functional mobility of the elbow.
Timing of surgery
We consider that muscle atrophy and joint contracture due to a delay in surgery are more problematic than the risks of increased postoperative recurrence rate due to early surgical intervention. Even if HO recurs postoperatively, re-operations can obtain acceptable results.6, 9
Tsionos et al.9 reported that about 71% (25/35 elbows) of cases recurred on early postoperative radiography (median delay, 9.5 months). However, functional impairment appeared in four cases (11.4%, 4/35 elbows), and these were defined as “true recurrence”. Other authors reported rates of 30% (3/10 elbows, median delay of 4 months)1 and 5.4% (8/148 patients, average delay of 13 months, range, 8 – 17 months).11
From the above reports, although there may have been differences in postoperative treatment, it seems that shorter time between burn injury and operation was associated with a higher “true recurrence” rate. This is because HO may be newly generated postoperatively if resection is performed too early, as ectopic bone is still being formed with the remaining inflammation.
In case 1, the left elbow was treated surgically without preoperative confirmation of HO maturation on X-rays (Figure 2). Although the HO was found to have recurred on early postoperative radiographs, it resolved spontaneously over time without any clinical symptoms. Tsionos et al.9 also reported this phenomenon in about 5.7% of cases (2/35 elbows).
The right elbow in cases 1 and 2, treated surgically after confirming the maturation of HO on X-rays preoperatively, did not recur either radiographically or clinically (Figure 3). This was probably because once the inflammation of the burned site had decreased, HO formation was stopped and stabilized. In addition, mobile skin over the elbow can prevent postoperative wound complications.5
Considering the postoperative improvement of ROM in cases 1 and 2, however, the exact surgical timing is still controversial.
Consequently, we recommend earlier surgical intervention after improving the skin condition around the elbow and confirming the maturation of HO on radiographs.
Rehabilitation
Some authors reported commencing rehabilitation of patients on the first postoperative day and obtained good results.1, 5 We followed this protocol for several reasons: (1) to decrease risk of HO development in burn patients because the period of inactivity is the main risk factor2; (2) to minimize the progression of postoperative muscle atrophy and joint contracture; and (3) to allow the patient to recognize improvement of the elbow joint ROM during the early postoperative period and encourage them to participate in treatment.
“Pain control” is very important in rehabilitation, and we provided good pain control using axially nerve block and rehabilitation equipment. To maintain the passive assisted ROM of the elbow a little beyond the range of maximum articulation that can be flexed and extended, active exercise was adopted gradually while observing progress.
Cooperation between the elbow joint and other joints is also important for performing activities of daily living.
Conclusions
Although the exact surgical timing is still controversial, we recommend that elbow ankylosis due to HO after burn injury should be treated surgically as soon as possible after improving the skin condition around the elbow and confirming the maturation of HO on radiographs. In addition, early rehabilitation and pain control are important after surgery.
Acknowledgments
Conflict of interest
None.
Funding
None.
References
- 1.Medina A, Shankowsky H, Savaryn B. Characterization of heterotopic ossification in burn patients. J Burn Care Res. 2014;35:251–256. doi: 10.1097/BCR.0b013e3182957768. [DOI] [PubMed] [Google Scholar]
- 2.Orchard GR, Paratz JD, Blot S. Risk factors in hospitalized patients with burn injuries for developing heterotopic ossification – a retrospective analysis. J Burn Care Res. 2015;36:465–470. doi: 10.1097/BCR.0000000000000123. [DOI] [PubMed] [Google Scholar]
- 3.Hastings H, 2nd, Graham TJ. The classification and treatment of heterotopic ossification about the elbow and forearm. Hand Clin. 1994;10:417–437. [PubMed] [Google Scholar]
- 4.Peterson JR, De La Rosa S, Eboda O. Treatment of heterotopic ossification through remote ATP hydrolysis. Sci Transl Med. 2014;6:255ra132. doi: 10.1126/scitranslmed.3008810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ring D, Jupiter JB. Excision of heterotopic bone around the elbow. Tech Hand Up Extrem Surg. 2004;8:25–33. doi: 10.1097/00130911-200403000-00007. [DOI] [PubMed] [Google Scholar]
- 6.Chen HC, Yang JY, Chuang SS. Heterotopic ossification in burns: our experience and literature reviews. Burns. 2009;35:857–862. doi: 10.1016/j.burns.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 7.Evans EB. Heterotopic bone formation in thermal burns. Clin Orthop Relat Res. 1991;263:94–101. [PubMed] [Google Scholar]
- 8.Ranganathan K, Hong X, Cholok D. High-frequency spectral ultrasound imaging (SUSI) visualizes early post-traumatic heterotopic ossification (HO) in a mouse model. Bone. 2018;109:49–55. doi: 10.1016/j.bone.2018.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsionos I, Leclercq C, Rochet JM. Heterotopic ossification of the elbow in patients with burns. J Bone Joint Surg. 2004;86:396–403. doi: 10.1302/0301-620x.86b3.14480. [DOI] [PubMed] [Google Scholar]
- 10.Evans EB, Larson DL, Yates S. Preservation and restoration of joint function in patients with severe burns. JAMA. 1968;204:843–848. [PubMed] [Google Scholar]
- 11.Veltman ES, Lindenhovius AL, Kloen P. Improvements in elbow motion after resection of heterotopic bone: a systematic review. Strat Trauma Limb Reconstr. 2014;9:65–71. doi: 10.1007/s11751-014-0192-0. [DOI] [PMC free article] [PubMed] [Google Scholar]