Summary
Background
Lymphedema is a chronic pathology characterized by progressive swelling due to lymphatic dysfunction (1). Literature contains few studies that focus on male genital lymphedema. A variety of surgical techniques as part of the male genital lymphedema therapeutic strategy has been described. Supramicrosurgical lymphatico-venular anastomosis s-LVA, based on connecting lymphatic collectors to venules, has evidenced efficient outcomes thus far. However, the peculiarity of the genital area may lead to an innovative and even more accurate surgical technique as a treatment of male genital lymphedema: lymphatic pre-collectors located superficially over the fascial layer can be used to perform the ultramicrosurgical anastomosis.
Purpose of the study
In this paper, the authors report their experience of this new surgical concept based on anastomosing lymphatic precollectors to venules.
Methods
We performed a retrospective study from 2014 to 2016. Six male patients with primary genital lymphedema underwent ultramicrosurgical lymphatico-venular anastomosis in Siena University Hospital, Italy.
Results
Ultramicrosurgical lymphatico-venular anastomosis has evidenced positive outcomes in terms of prognosis, infectious complications, volume reduction, and quality of life. The average cellulitis rate dropped from 2.5 episodes a year to 0.5 episodes after surgical intervention. The mean satisfaction index passed from 1.33 before the intervention to 2.83.
Conclusion
Ultramicrosurgical lymphatico-venular anastomosis represents a challenging physiological approach for male genital lymphedema with promising outcomes.
Keywords: Lymphedema, Genital lymphedema, Lymphatico-venular anastomosis, Primary male lymphedema, Microsurgery, Supramicrosurgery
Introduction
Lymphedema is a chronic pathology characterized by a subcutaneous accumulation of protein- rich fluid that results in a progressive swelling of the limb due to lymphatic dysfunction.1 The limbs and, second, the genitals are the most frequently affected areas.2 Lymphedema can be primary or, most frequently, secondary (90%).3 Primary lymphedema is an uncommon condition due to congenital lymphatic abnormalities that affect 1.2 per 100,000 persons less than 20 years of age.3 Secondary lymphedema is mostly related to cancer therapies.4 It has been reported that subsequent to such therapies (lymph node dissection and/or radiotherapy), 49% of patients with breast cancer, 20% of those with gynecologic cancer, and 10% of those with genitourinary cancer develop lymphedema.5 The other causes of secondary lymphedema may be the accidental or iatrogenic injury of the lymphatic vessels.1
Primary male genital lymphedema is a rare condition, and its prevalence is still undetermined.3
Penoscrotal affection is the most common manifestation of the disease.3 According to the age of onset, congenital lymphedema may develop at birth (Milroy disease), at the onset of puberty (lymphedema precox/Meigs disease), or lately during adulthood (lymphedema tarda).6
As in the initial stages such edema is pitting, the evolution of the pathology without appropriate intervention leads to greater swelling, tissue and skin changes with a major risk of infection of the affected limb. Lymphedema not only interferes with the quality of life, general functioning, and social interactions of the individual but also exposes the individual to a severe complication, which is cellulitis.7, 8
Surgical treatment of male genital lymphedema has evidenced positive outcomes.3,9 The contribution of the conservative approach, however, is controversial.3 Beyond the divergence of opinions regarding the benefits of compressive therapies in male genital lymphedema, it is though important to highlight the difficulty in wearing such garments in this anatomic area that requires even more commitment from the patient and the family.3 The prevention of infection requires a daily hygiene and skin care. A prophylactic antibiotic treatment may be indicated in patients with three or more cellulitis episodes per year.3
Materials and methods
From 2014 to 2016, 6 male patients with primary genital penoscrotal lymphedema have undergone ultramicrosurgical lymphatico-venular anastomosis associated with physical therapy in Siena University Hospital, Italy. Diagnosis of lymphedema was based on clinical and radiological criteria. Radiological investigation included penoscrotal ultrasound, lymphoscintigraphy, and indocyanine green (ICG) lymphography.
Patient evaluation was performed in pre- and postoperation (Tables 1 and 2). Episodes of cellulitis, quality of life, and penoscrotal volume were assessed in each patient. Quality of life was subjectively evaluated through a satisfaction index that ranges the patient's condition from 1 to 4 (1: not satisfied to 4: extremely satisfied). Penoscrotal characteristics were assessed by ultrasound. However, given the peculiarity of this anatomic area, it is relevant to highlight that determining the global volume of male genitalia is difficult. Thus far, the methods for genitalia volume assessment remain controversial. There are few specific studies with significant and reliable data on the topic.
Table 1.
Clinical characteristics of our sample.
| Patients |
Age |
Age of onset |
Evolution of lymphedema | Pre-op cellulitis rate |
Post-op cellulitis rate | Pre-op life quality |
Post-op life quality | ICG pattern |
Pre-op physiotherapy | Post-op physiotherapy |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 20 | 4 | 16 | 1 | 0 | 1 | 4 | Splash pattern | Yes | Yes |
| 2 | 35 | 27 | 8 | 2 | 0 | 1 | 3 | Star dust pattern | No | Yes |
| 3 | 17 | 2 | 15 | 3 | 1 | 2 | 3 | Splash pattern | Yes | Yes |
| 4 | 28 | 10 | 18 | 3 | 1 | 1 | 2 | Diffuse pattern | Yes | Yes |
| 5 | 30 | 11 | 19 | 2 | 0 | 2 | 4 | Diffuse pattern | Yes | Yes |
| 6 | 22 | 7 | 15 | 4 | 1 | 1 | 2 | Splash pattern | No | Yes |
⁎Patients’ life quality:
1↔ not satisfied
2↔ moderately satisfied
3↔satisfied
4↔ extremely satisfied
Table 2.
Pre-operative and post-operative evolution of cellulitis rates.
| Episodes/year | N Patients | % |
|---|---|---|
| Pre-operative cellulitis rate | ||
| 1 | 1 | 16.7 |
| 2 | 2 | 33.3 |
| 3 | 2 | 33.3 |
| 4 | 1 | 16.7 |
| Post-operative cellulitis rate | ||
| 0 | 3 | 50 |
| 1 | 3 | 50 |
In the following study, penoscrotal volume evaluation relied on the subjective evaluation of the patient (macroscopic aspect and volume of genitalia, underwear size). Penoscrotal ultrasound provided further data regarding the characteristics of genitalia.
Lymphedema was then categorized as light, moderate, and severe according to the amount of swelling and genital volume.
Starting from the 3rd week, patients were asked to resume physical therapy.
Postoperative outcomes were assessed at the 2nd week and at the 1st, 3rd, 6th, 12th, and 24th months.
Anesthesiologic consideration
Surgery was performed under local anesthesia.
Local anesthesia was performed by adopting a mixture of 2% lidocaine and epinephrine at a dilution of 1:200,000. As the intervention requires immobility, deep sedation was adopted to increase the patient's comfort. Propofol (2 mg/kg/h) and remifentanil (0.015 mcg/kg/min) were used while maintaining spontaneous breathing. Oxygen was administrated at 4 l/min through a nasal cannula or Venturi's mask. Patients were premedicated with midazolam (0.02 mg/kg). Antibiotic prophylaxis, gastric protection, and antiemetic were used. Patients were monitored during the surgical procedure. Adequate postoperative analgesia was obtained with paracetamol 1 g every 8 h for the first 24 h.
Surgical technique
Preoperatively, lymphatic flow was assessed by ICG lymphography.
ICG lymphography enabled evidencing the lymphatic dysfunction/obstacle and locating the functional lymphatic vessels to determine the elective site for incision and anastomosis. Indocyanine green Pulsion® 0.1 cc was injected subcutaneously into the scrotum. Afterwards, using infrared camera system PDE (Photodynamic Eye; Hamamatsu Photonics, Hamamatsu City, Shizuoka, Japan), lymphatic drainage was assessed.
Venous mapping was realized using Accu Vein (Accu Vein Inc, Huntington, NY). It enabled locating superficial venules.
Local anesthesia was administered in the cutaneous incision sites.
Scrotal linear incisions of 2 cm were performed. The elective incision sites were selected on the basis of preoperative mapping.
Microscopic dissection under a 12.5X magnification microscope (Zeiss) was performed to identify lymphatic precollectors and venules located over the fascial layer.
End-to-end ultramicrosurgical anastomoses were realized using 12.0 nylon sutures. A mean of 4 anastomoses was performed in each patient. After anastomosis, milk test was performed to evaluate anastomoses patency and evidenced lymphatic flow into the venules. Skin was sutured with absorbable sutures. Patients were discharged one day after the surgical procedure. Three days of rest and oral antibiotic therapy were prescribed. Postoperative outcomes have been evaluated at 2 weeks, 1 month, 3 months, and 6 months periodically after the surgical procedure. Sutures were removed 2 weeks after the procedure.
Results
The average age of our sample of 6 patients was 25.33 years, with minimum of 17 years and maximum of 35 years. Genital lymphedema is commonly developed during childhood, with an average onset age of 10.17 years. Only one patient in our sample presented lymphedema tarda with early adulthood onset at the age of 27 years. The condition has been evolving for a mean of 15.17 years.
Patients have reported a compromised quality of life before the intervention, with an average satisfaction index of 1.33. More than 2 episodes of cellulitis a year have been recorded in half of the sample, with an average of 2.5 episodes per year preoperatively. Postoperative evaluation has evidenced positive outcomes in terms of infectious complications, volume reduction, and quality of life. The average cellulitis rate dropped from 2.5 episodes a year to 0.5 episodes after the surgical procedure. The reduction of cellulitis rates was observed already from the first year of postoperative follow-up and confirmed during the second year. Penoscrotal volume reduction was reported by all patients. Furthermore, patients reported a subjective melioration of the macroscopic aspect of genitalia (less tense and softer tissues). Patients have reported a more satisfying quality of life, with a mean satisfaction index of 2.83.
Discussion
Diagnosis of lymphedema is based on clinical criteria.10 Particularly, in male genital lymphedema, the enlargement of the genitalia is the principal symptom.3 Further, somatic symptoms such as cellulitis, lymphorrhea, cutaneous changes, and genito-urinary symptoms are also reported.3,11 Imaging is also a fundamental step of the diagnostic approach. Imaging techniques such as lymphoscintigraphy, indocyanine green (ICG), lymphography, or magnetic resonance lymphography (MRL) have been reported as efficient and useful means.12,13
The staging of lymphedema, on which depends the therapeutic strategy, is based on the amount of swelling and the condition of the tissues.
The treatment of lymphedema has largely benefited from the improvement of surgical techniques that tend to be minimally invasive. The surgical approach is categorized as “physiological” and “excisional” procedures.10
The physiological procedures are the microsurgical procedures that create new lymphatic anastomosis and, consequently, better lymphatic flow.10 These procedures include supramicrosurgical lymphatico-venular anastomosis (s-LVA) and vascularized lymph node transfer (VLNT).10
Supramicrosurgery, as a therapeutic approach of lymphedema, was first reported in 1996 by Koshima. Such a technique, which allows the manipulation of inframillimetric structures, is based on creating anastomosis between lymphatic collectors and veins to bypass an underlying lymphatic flow abnormality. It is one of the lymphatico-venular derivation techniques that is most commonly used to treat limb lymphedema.
These physiological procedures have led to not only a decrease in daily requirement of physical therapy (compression garments and lymphedema therapy) during the postoperative follow-up but also a significant reduction in the incidence of cellulitis in all patients, in all lymphedema stages after the surgical intervention.1,14
In fact, Gennaro et al. have reported a significant difference between preoperative and postoperative cellulitis rates in patients who have undergone the s-LVA.1 Therefore, a significant reduction in cellulitis incidence has been underlined in all lymphedema stages: a decrease to 0 cases the year after s-LVA per stages 1, 2a, 3, and a reduction from 3.3 cases the year before to 0.3 cases after the intervention in stage 2b lymphedema.1
Such outcomes are supported in other studies.14, 15, 16 Grangzow et al. reported in their paper that per an average postoperative follow-up of 25 months, severe cellulitis incidence decreased 3.8 times (from 58% to 15%) after surgical treatment.14
While these techniques are mostly used in early stages of lymphedema, as they address the fluid phases14, the excisional procedures target the solid component of chronic lymphedema and consist of removing excess tissues.10,14 Such procedures allow a greater circumference reduction but do not remedy to the underlying lymphatic flow dysfunction.10 Suction-assisted protein lipectomy (SAPL) is one of these procedures; it is based on modern techniques of liposuction to remove the excess tissue with minor morbidity and brief recovery.10 It has been reported that 106% and up to 75% volume reduction has been achieved, respectively, in upper and lower limb lymphedema in patients who have undergone SAPL combined with compressive postoperative therapy.10,17,18 Therefore, a decrease in the risk of cellulitis has been stated with such surgical approach.19 Another technique is the “staged cutaneous/subcutaneous excision” (reduction) used for genital lymphedema. 10 General functioning and well-being, assessed by the Glasgow Benefit Inventory, improved in a group of patients who had undergone surgical treatment combiend with complex decongestive physiotherapy.9 However, such a technique was correlated to a high operative morbidity and a long recovery period.10 Genital lymphedema recurrence (scrotum) has also been reported.9 A less invasive intervention in the case of male genital lymphedema could represent an interesting approach, as it is an anatomic area with favorable characteristics from a surgical point of view. (Figures 1 and 2)
Figure 1.
Intraoperative image of lymphatics and venules before (left) and after (right) anastomosis. Mean diameter of these vessels was 0.3 mm; 11.0 suture was adopted.
Figure 2.
Clinical appearance of male primary genital lymphedema before ultra-microsurgery (left) and after, at D14 post-op (right).
Normally, lymphatic collectors are identified by fluoroscopy with the PDE system. It is to underline though that these lymphatic vessels are not always visualized in genital lymphedema. In fact, in genital lymphedema, it occurs due to lack of a linear pattern in fluoroscopy, a sign that allows to identify the lymphatic collectors. It is though common to observe, after scrotal or penial injection of indocyanine green (ICG), a splash pattern lymphography20 (Figure 3). A deep study of such outcomes may evidence REROUTING: the lymph, at the level of the lymphatic dysfunction/obstacle, reaches the derma dilating the lymphatic pre-collectors that follow a different route to the subcutaneous layers.21
Figure 3.
After scrotal injection of ICG we see a splash type lymphography.
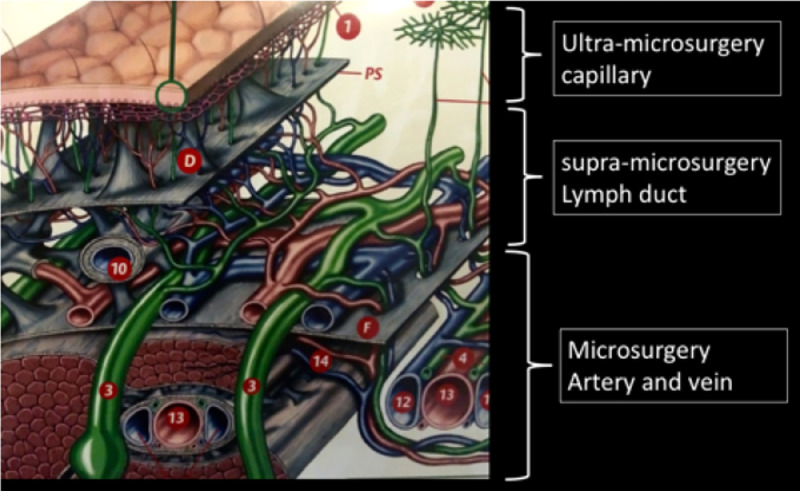
It is possible, when visualized, to anastomose such lymphatic precollectors located superficially to the venules. In fact, our experience has shown that it is possible to identify lymphatic precollectors and venules located over the fascial layer (Figure 4). These lymphatic vessels have a mean diameter of 0.3 mm. The superficial venules with low pressure, as demonstrated by the absence of backflow, are appropriate for the ultramicrosurgical LVA. It is important to perform endoluminal anastomosis.
Figure 4.
Anatomical sections of lymphatic vascular system.
The authors introduce here the concept of ultramicrosurgery as we progress from manipulating lymphatic collectors to manipulating even thinner structures, which are the precollectors. Such pre-collectors may also have an adequate flow as fluoroscopy usually evidences a high pressure, sufficient enough to drain the lymph. Conventional supramicrosurgical LVA, which has been widely described as an effective treatment for upper and lower limb lymphedema, is based on the use of lymphatic collectors for the anastomoses. These collectors are normally located under the fascial layer.
Conversely, the anatomical peculiarity of the penoscrotal area is that lymphatic precollectors are located over the fascial layer. Ultramicrosurgery enables surgeons to manipulate these superficial precollectors to create anastomoses. Here lies the innovative approach that the authors introduce for treating male genital lymphedema.
The authors assume that in the genital area, superficial lymphatic precollectors may represent adequate structures for lymphatico-venular anastomosis, as they microscopically seem less altered by lymphedema and characterized by a pressure sufficient enough to drain the lymph.
The results of the following study comfort the hypothesis that such a procedure actually could represent a promising approach for the treatment of male primary genital lymphedema. In fact, the rate of infectious complications of lymphedema has dropped in all patients. Subjective melioration of macroscopic aspect and volume of genitalia was highlighted by all patients in the study sample. Nonetheless, these preliminary results need to be extended by further studies with a larger patient number, long-term follow-up to confirm the initial outcomes.
As already stated, the surgical treatment conforms with the conservative approach, which represents an important step in the therapeutic strategy. In fact, it may not only enhance the positive outcomes of surgical treatment in a synergic impact on lymphatic dysfunction1 but also facilitate the surgery itself.9 It is to underline though that the benefits of the conservative therapy in male genital lymphedema are controversial.3 Nonetheless, it has shown positive and engaging outcomes, especially when performed postoperation, in a variety of studies.3,6,9
The nonoperative treatment of lymphedema is based on static compression (static garments, pneumatic compression, and compressive bandaging), manual lymphatic drainage, and skin care to reduce volume and prevent cellulitis.10
Conclusions
Primary male genital lymphedema is a rare condition with psychosocial and somatic morbidity. The therapeutic approach may benefit from this innovative surgical technique: the ultramicrosurgical lymphatico-venular anastomosis. This study has evidenced promising outcomes in terms of reduction of cellulitis episodes and, in particular, improvement of quality of life. Although further studies are needed, ultramicrosurgical LVA seems to be efficient and less invasive in treating male genital lymphedema.
Conflict of interest and funding
None declared.
References
- 1.Gennaro P., Gabriele G., Salini C., Chisci G., Cascino F., Xu J.F., Ungari C. Our supramicrosurgical experience of lymphaticovenular anastomosis in lymphoedema patients to prevent cellulitis. Eur Rev Med Pharmacol Sci. 2017;21(4):674–679. PubMed PMID: 28272717. [PubMed] [Google Scholar]
- 2.Maclellan R.A., Couto R.A., Sullivan J.E., Grant F.D., Slavin S.A., Greene A.K. Management of primary and secondary lymphedema: analysis of 225 referrals to a center. Ann Plast Surg. 2015;75(2):197–200. doi: 10.1097/SAP.0000000000000022. PubMed PMID: 24691335. [DOI] [PubMed] [Google Scholar]
- 3.Schook C.C., Kulungowski A.M., Greene A.K., Fishman S.J. Male genital lymphedema: clinical features and management in 25 pediatric patients. J Pediatr Surg. 2014;49(11):1647–1651. doi: 10.1016/j.jpedsurg.2014.05.031. PubMed PMID: 25475811. [DOI] [PubMed] [Google Scholar]
- 4.Olszewski W. On the pathomechanism of development of postsurgical lymphedema. Lymphology. 1973;6(1):35–51. PubMed PMID: 4691971. [PubMed] [Google Scholar]
- 5.Granzow J.W., Soderberg J.M., Kaji A.H., Dauphine C. Review of current surgical treatments for lymphedema. Anna Surg Oncol. 2014;21(4):1195–1201. doi: 10.1245/s10434-014-3518-8. PubMed PMID: 24558061. [DOI] [PubMed] [Google Scholar]
- 6.Garaffa G., Christopher N., Ralph D.J. The management of genital lymphoedema. BJU Int. 2008;102(4):480–484. doi: 10.1111/j.1464-410X.2008.07559.x. PubMed PMID: 18325055. [DOI] [PubMed] [Google Scholar]
- 7.McWayne J., Heiney S.P. Psychologic and social sequelae of secondary lymphedema: a review. Cancer. 2005;104(3):457–466. doi: 10.1002/cncr.21195. PubMed PMID: 15968692. [DOI] [PubMed] [Google Scholar]
- 8.Simon M.S., Cody R.L. Cellulitis after axillary lymph node dissection for carcinoma of the breast. Am J Med. 1992;93(5):543–548. doi: 10.1016/0002-9343(92)90583-w. PubMed PMID: 1364813. [DOI] [PubMed] [Google Scholar]
- 9.Torio-Padron N., Stark G.B., Foldi E., Simunovic F. Treatment of male genital lymphedema: an integrated concept. J Plast Reconstr Aesthet Surg JPRAS. 2015;68(2):262–268. doi: 10.1016/j.bjps.2014.10.003. PubMed PMID: 25456280. [DOI] [PubMed] [Google Scholar]
- 10.Maclellan R.A., Greene A.K. Lymphedema. Semin Pediatr Surg. 2014;23(4):191–197. doi: 10.1053/j.sempedsurg.2014.07.004. PubMed PMID: 25241097. [DOI] [PubMed] [Google Scholar]
- 11.Schook C.C., Mulliken J.B., Fishman S.J., Grant F.D., Zurakowski D., Greene A.K. Primary lymphedema: clinical features and management in 138 pediatric patients. Plast Reconstr Surg. 2011;127(6):2419–2431. doi: 10.1097/PRS.0b013e318213a218. PubMed PMID: 21617474. [DOI] [PubMed] [Google Scholar]
- 12.Gennaro P., Borghini A., Chisci G., Mazzei F.G., Weber E., Tedone Clemente E., Guerrini S, Gentili F., Gabriele G., Ungari C., Mazzei M.A. Could MRI visualize the invisible? An Italian single center study comparing magnetic resonance lymphography (MRL), super microsurgery and histology in the identification of lymphatic vessels. Eur Rev Med Pharmacol Sci. 2017;21(4):687–694. PubMed PMID: 28272715. [PubMed] [Google Scholar]
- 13.Gennaro P., Chisci G., Mazzei F., Gabriele G. Magnetic resonance lymphangiography: how to prove it? J Magn Reson Imag JMRI. 2016;44(2):509–510. doi: 10.1002/jmri.25147. PubMed PMID: 26752609. [DOI] [PubMed] [Google Scholar]
- 14.Granzow J.W., Soderberg J.M., Kaji A.H., Dauphine C. An effective system of surgical treatment of lymphedema. Ann Surg Oncol. 2014;21(4):1189–1194. doi: 10.1245/s10434-014-3515-y. PubMed PMID: 24522988. [DOI] [PubMed] [Google Scholar]
- 15.Gennaro P., Gabriele G., Mihara M., Kikuchi K., Salini C., Aboh I., Cascino F., Chisci G., Ungari C. Supramicrosurgical lymphatico-venular anastomosis (LVA) in treating lymphoedema: 36-months preliminary report. Eur Rev Med Pharmacol Sci. 2016;20(22):4642–4653. PubMed PMID: 27906440. [PubMed] [Google Scholar]
- 16.Mihara M., Hara H., Furniss D., Narushima M., Iida T., Kikuchi K., Ohtsu H., Gennaro P., Gabriele G., Murai N. Lymphaticovenular anastomosis to prevent cellulitis associated with lymphoedema. Br J Surg. 2014;101(11):1391–1396. doi: 10.1002/bjs.9588. PubMed PMID: 25116167. [DOI] [PubMed] [Google Scholar]
- 17.Greene A.K., Slavin S.A., Borud L. Treatment of lower extremity lymphedema with suction-assisted lipectomy. Plast Reconstr Surg. 2006;118(5):118e–121e. doi: 10.1097/01.prs.0000237020.29209.22. PubMed PMID: 17016168. [DOI] [PubMed] [Google Scholar]
- 18.Brorson H., Ohlin K., Olsson G., Svensson B., Svensson H. Controlled compression and liposuction treatment for lower extremity lymphedema. Lymphology. 2008;41(2):52–63. PubMed PMID: 18720912. [PubMed] [Google Scholar]
- 19.Miller T.A., Wyatt L.E., Rudkin G.H. Staged skin and subcutaneous excision for lymphedema: a favorable report of long-term results. Plast Reconstr Surg. 1998;102(5):1486–1498. doi: 10.1097/00006534-199810000-00022. discussion 99-501. PubMed PMID: 9774002. [DOI] [PubMed] [Google Scholar]
- 20.Mihara M., Hara H., Kikuchi K., Yamamoto T., Iida T., Narushima M., Araki J., Murai N., Mitsui K., Gennaro P., Gabriele G., Koshima I. Scarless lymphatic venous anastomosis for latent and early-stage lymphoedema using indocyanine green lymphography and non-invasive instruments for visualising subcutaneous vein. J Plast Reconstr Aesthet Surg JPRAS. 2012;65(11):1551–1558. doi: 10.1016/j.bjps.2012.05.026. PubMed PMID: 22817883. [DOI] [PubMed] [Google Scholar]
- 21.Belgrado J.P., Vandermeeren L., Vankerckhove S., Valsamis J.B., Malloizel-Delaunay J., Moraine J.J., Liebens F. Near-infrared fluorescence lymphatic imaging to reconsider occlusion pressure of superficial lymphatic collectors in upper extremities of healthy volunteers. Lymphat Res Biol. 2016;14(2):70–77. doi: 10.1089/lrb.2015.0040. PubMed PMID: 27167187; PubMed Central PMCID: PMCPMC4926199. [DOI] [PMC free article] [PubMed] [Google Scholar]