Abstract
Fingertip amputations are a very common form of injury seen in the emergency departments. Various techniques have been described for the management of these injuries including simple dressings, skin grafts, homodigital, heterodigital and regional flaps and also free flaps. We present our experience with 10 cases of unilateral V-Y flaps raised on a perforator vessel and advanced in a modified fashion to cover the entire tip with a single flap. The technique is quick and easy to perform under loupe magnification, has minimal donor site morbidity and achieves good results in terms of healing, hand function, sensory recovery, appearance and patient satisfaction.
Keywords: V-Y fingertip flap, Homodigital perforator flap, Unilateral V-Y perforator flap, Fingertip reconstruction, Digital artery perforator flap, VY perforator flap
Introduction
Fingertip amputations are very common injuries especially in the young and in manual workers. Various treatment options have been described including terminalisation, healing by secondary intention, skin grafts, homodigtal, heterodigital and regional flaps as well as free flaps. Homodigital flaps are relatively easy to perform, limit the donor site morbidity to the same finger and achieve comparable or better outcomes than the other methods. We describe our experience with the unilateral V-Y flap, similar to the Kutler flap, but mobilised on a perforator and advanced in a modified manner to achieve full tip coverage with a single flap.
Materials and methods
A total of 10 fingers in 10 patients had this procedure performed between 2013 and 2018. There were 8 adults and 2 children. The average age was 26.5 years (range 1 to 52) with 6 males (60%) and 4 females (40%). Two of the ten patients were active smokers. None of the patients suffered from any known vascular diseases or other significant comorbidities. There were 3 index, 3 middle and 4 little fingers involved. Nine were crush injuries (8 in doors and one in a printing machine) and one was a sharp amputation from a metal sheet. All cases selected were Allen classification type 3 amputations with significant exposed distal phalanx where it would not be possible to achieve closure without significant shortening or a flap procedure . More proximal amputations and more distal amputations with only pulp loss and no exposed bone, were excluded. All flaps were performed under 4x wide field surgical loupe magnification. All cases were done under local anaesthetic digital block except for the two paediatric cases, which were performed under general anaesthetic.
Surgical technique
After debridement of the stump to healthy tissue and removal of any protruding or contaminated tip of distal phalanx, a unilateral V-Y flap is designed on the radial or ulnar aspect (depending on the injury configuration and tissue availability), with the apex at the DIP crease (Figure 1A, Figure 2A). The posterior marking is along the mid lateral line and the anterior limb of the V is marked to correspond to the width of the amputated tip defect or slightly narrower. This results in a narrow long flap (Figure 1B, Figure 2B). The dorsal incision is made down to the periosteum. The volar incision is made just beyond the dermis and the fascial strands are dissected carefully looking for tiny perforator vessels to the flap, at least one of which is preserved (Figure 3A, B). Once the flap is isolated on the perforator, the volar pulp skin and fat is elevated off the flexor tendon sheath. This permits transposition of the pedicle and flap across the finger rather than the usual sliding advancement to achieve a transverse lie of the flap across the tip defect, adequately covering the defect (Figure 1C, Figure 2C. Where a perforator cannot be identified (which was not the case in our series), a cuff of fat should be preserved at the base of the flap. This however, will reduce the mobility of the flap. The flap is inset with absorbable or non-absorbable sutures. The donor site closes directly as it is a narrow flap (Figure 1E, Figure 2F). A non-adherent dressing is applied. Patients were followed up in 5–7 days and sutures were removed in 10–14 days if non-absorbable. Standard post-operative physiotherapy included range of motion exercises and scar management. At final follow up, range of movement, tip sensitivity, sensation and patient satisfaction were assessed.
Figure 1.
Case 1 showing (A) Unilateral V-Y flap marking, (B) flap elevated on perforator, (C,D) flap inset into defect and (E) donor site closed.
Figure 2.
Case 2 showing (A) Unilateral V-Y flap marking, (B) flap elevated on perforator, (C–E) flap inset into defect and (F) donor site closed.
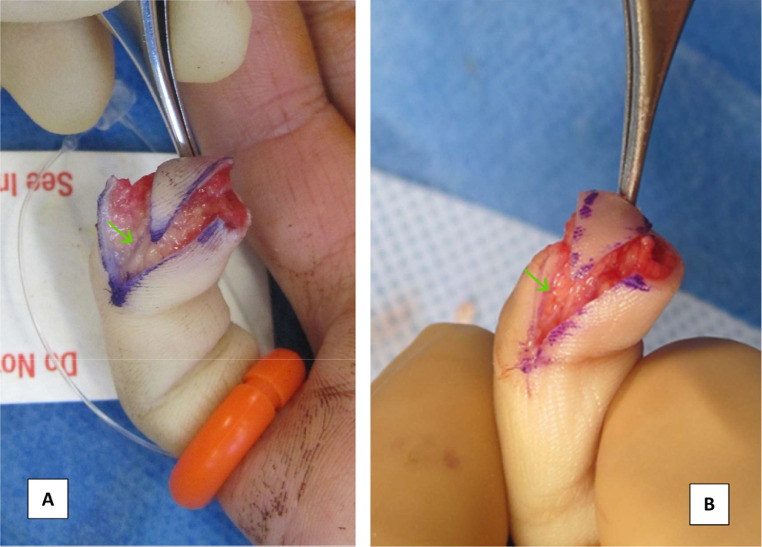
Figure 3.
Two cases demonstrating perforator vessel (marked by green arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article).
Results
All flaps survived and healed without any wound complications. The average follow up was 92.4 days (range 28 to 234 days). 7 patients had a minimum 6 months follow up and reported good sensation (static 2-point discrimination over the pulp and the flap in the range of 3–4 mm) and were free of any sensitivity of the tip. One of these patients had persistent sensitivity for 4 months needing continued desensitization therapy, but this settled at 6 months. The size of the flaps ranged from 14 to 80 mm2. All the 7 patients with longer follow up were very satisfied with the functional outcome and appearance except one patient who had significant parrot beaking and was not happy with the appearance but did not want any further intervention. The flaps stretched over the tip over time and resulted in an aesthetically appealing round contour of the fingertip (Figures 4 and 5).
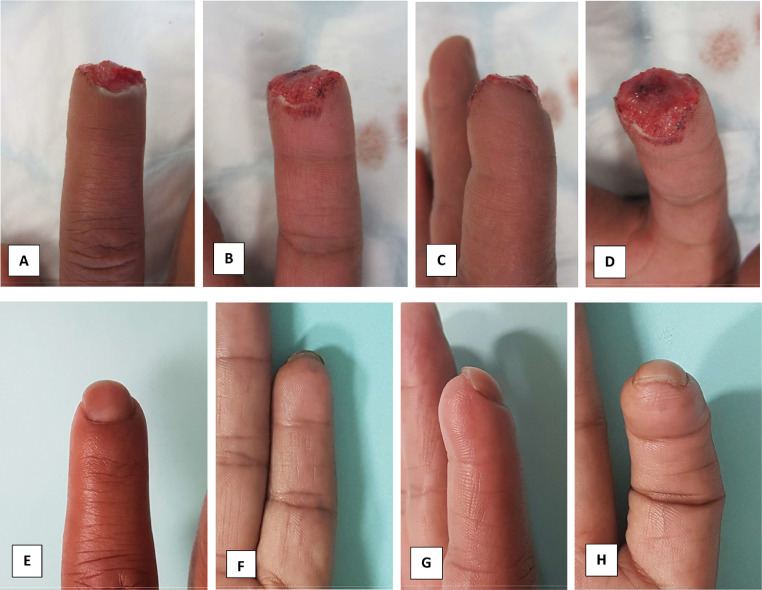
Figure 4.
Preop (A–D) and 2-year postop (E–H) photos of Case 1 in Figure 1, showing limited scarring, good pulp contour and no scar related contracture.
Figure 5.
Preop (A–C) and 1-year postop (D–G) photos of Case 2 in Figure 2, showing good contour, minimal scarring and no scar related contracture.
Discussion
Distal finger flaps transferred from adjacent tissue to the amputated tip have the advantages of being simple and quick to perform and limit donor site morbidity. However, the commonly used Volar V-Y advancement (Atasoy or Tranquilli-Leali), the Venkataswamy and Subramanian obilque V-Y flaps, Segmuller flaps and reverse digital artery island flaps involve incision on and advancement of a significant portion of the volar digital skin, resulting in potential sensory alterations in the functionally critical pulp skin and more risk of contractures because they cross skin creases.1 Also, flap failure in these cases causes a significant morbidity and a much larger defect that the original, making further reconstruction more complicated. The bilateral Kutler flap is based on the neurovascular bundle and due to limited dissection, does not achieve much advancement for a single flap to cover the whole defect2 and significantly denervates the pulp. The use of a unilateral version of the Kutler flap to reconstruct the tip defect was described by Biddulph in 1975.3 Recent advances in the understanding of perforator vessels has lead to the description of many perforator based distal finger flaps.4, 5, 6 The anatomy of the digital artery perforators has been studied and described by Koshima et al. in detail, using arterial embalming techniques.5 They identified many perforators from the digital arteries in the mid-lateral aspect of the digits which perforate the thin fascia and adipose tissue and terminate multiple arterioles into the subdermal layer. Numerous perforating arterioles and venules exist between these perforators in the subcutaneous tissue through the mid lateral line of the fingers. The digital artery usually has no concomitant vein but sometimes has double or single concomitant veins. The drainage venules connect to the dorsal and volar cutaneous venous systems in the subcutaneous tissue. Mobilisation of the tiny flap on the skin perforator and leaving behind the main digital nerves has the advantage of not disturbing the pulp nerve supply and not interrupting the main digital arterial supply. Also, the unilateral flap causes minimal scarring to the rest of the finger, except for the small donor site scar distal to the DIP crease. Arpaci et al. described the super Kutler flap which however is a bilateral flap based on the digital artery perforators with more extensive dissection of the neurovascular bundle and hence not a pure perforator flap.7
In our series, we have modified the Kutler flap and the Biddulph flap, raising a single flap on a perforating vessel and facilitating the advancement by elevating the pulp tissues off the flexor sheath. This allows for ease of advancement and transposition of the flap across the volar aspect of the distal phalanx to increase the reach of the flap and achieves cover across the amputated tip. We have found the flap to be suitable for oblique or transverse amputations of the finger distal to the lunula. In case of larger defects, it is enough to cover the critical area of exposed bone and allow the rest to heal by secondary intention. The flap is not suitable for very large defects, in which case, other options will have to be used. The donor site is closed primarily leaving no secondary defect and in the rare case where the flap is unsuccessful, which we have not seen in our series, there is no increase in size of the defect to be treated.
Conclusion
The Unilateral V-Y perforator flap is a useful method for treating selected distal fingertip amputations with exposed bone. It has minimal donor site morbidity and is easy to perform under magnification. Within the small sample size in our series, it demonstrably achieves good results in terms of healing, recovery of hand function, sensory recovery and patient satisfaction with appearance.
Declaration of Competing Interest
None.
Funding
None.
References
- 1.Usami S., Kawahara S., Yamaguchi T., Hirase Y. Homodigital artery flap reconstruction for fingertip amputation: a comparative study of the oblique triangular neurovascular advancement flap and the reverse digital artery island flap. J Hand Surg (Eur) 2015;40(3):291–297. doi: 10.1177/1753193413515134. [DOI] [PubMed] [Google Scholar]
- 2.Kutler W. A new method for fingertip amputation. JAMA. 1947;133(1):29–30. doi: 10.1001/jama.1947.62880010007007. [DOI] [PubMed] [Google Scholar]
- 3.Biddulph S.L. The neuro vascular flap in finger tip injuries. Hand. 1979;11(1):59–63. doi: 10.1016/s0072-968x(79)80011-x. [DOI] [PubMed] [Google Scholar]
- 4.Mitsunaga N, Mihara M, Koshima I. Digital artery perforator (DAP) flaps: Modifications for fingertip and finger tump reconstruction. J Plast Reconstr Aesthet Surg. 2010;63:1312–1317. doi: 10.1016/j.bjps.2009.07.023. [DOI] [PubMed] [Google Scholar]
- 5.Koshima Isao, Urushibara K, Fukuda N. Digital artery perforator flaps for fingertip reconstructions. Plast Reconstr Surg. 2006;118(7):1579–1584. doi: 10.1097/01.prs.0000232987.54881.a7. [DOI] [PubMed] [Google Scholar]
- 6.Kim K S. Digital artery perforator flaps. Arch Reconstr Microsurg. 2015;24(2):50–55. [Google Scholar]
- 7.Arpaci E., Unlu R.E., Altun S., Ertas N.M. Super kutler flap: an alternative technique for reconstruction of fingertip defects. J Hand Surg (Eur) 2017;42E(6):626–632. doi: 10.1177/1753193416686884. [DOI] [PubMed] [Google Scholar]