Abstract
Background
The transgender patient seeking transition from male to female suffers a significant stigma from the prominent male thyroid cartilage. Natal men and women may seek elective reduction of the “Adam's apple” as well. There are various techniques for performing chondrolaryngoplasty, but these techniques and their associated outcomes are poorly described in the literature.
Methods
A literature review was performed for articles related to esthetic chondrolaryngoplasty. Data related to outcomes and complications were extracted. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed. The authors also present the case of a transgender 58 year-old male-to-female patient who underwent chondrolaryngoplasty.
Results
Four case series, including 69 patients who had esthetic chondrolaryngoplasty, were identified that met inclusion criteria. Qualitative assessment of patient satisfaction was reported in two studies (n = 62), with a 98.4% satisfaction rate. The most common complications were odynophagia in 20.3% of patients, hoarseness in 36.2% of patients, and laryngospasm in 1.4% of patients. Of patients that had postoperative hoarseness, 96% had resolution within 20 days. In our patient's case, chondrolaryngoplasty was performed with a tracheal shave in combination with high-speed burring for fine contouring. The patient experienced hoarseness for 1 week postoperatively that self-resolved.
Conclusion
Overall, chondrolaryngoplasty for reduction of the thyroid cartilage appears to be a safe and effective procedure. The complications that occurred in identified case series were mild and self-limiting. Although serious complications are certainly possible, we were not able to identify their occurrence in the literature. Recent modifications in chondrolaryngoplasty involve protecting the anterior commissure tendon to prevent iatrogenic voice modification.
Keywords: Chondrolaryngoplasty, Facial feminization, Male-to-female, Tracheal shave, Transgender
Background
A prominent thyroid cartilage, otherwise referred to as pomusadamus, or “Adam's apple,” contributes to feelings of gender dysphoria in transwomen.4,7 The male larynx is indistinguishable from the female until pubertal growth of the thyroid cartilage in males. Apart from size, anterior borders of the thyroid cartilage also connect at a much sharper angle accentuating the laryngeal prominence.4,7 It is thought of as a “give-away” sign, which despite top and bottom surgery, facial contouring procedures, and psychosocial adaptations, exposes the undesired gender due to its role as a masculine marker in our society. In addition to transwomen, thin natal men and women may seek elective reduction of the “Adam's apple.” Here the authors focus on the transgender patient seeking male-to-female (MtF) affirmation, who suffers a significant stigma from the prominent male thyroid cartilage.
Chondrolaryngoplasty, often given the misnomer “tracheal shave,” was first described by Wolfort and Parry in 19755 and modified by Wolfort in 1990.4 The initial approach was open with perichondrial flaps raised from inside of the lamina and careful excisions of the perichondrium on the external border of the thyroid cartilage. This was followed by the use of a burr as needed for contour refinement.4 Since then, endoscopy-guided external surgical approaches have been carried out, allowing for better visualization of the anatomy, more aggressive reductions without damaging the vocal cords, and potential for improved esthetic outcomes.3,6
There are various techniques for performing chondrolaryngoplasty, but these techniques and their associated outcomes are poorly described in the literature. Therefore, the purpose of this study was to determine the safety of esthetic chondrolaryngoplasty as well as rates of patient satisfaction. Secondary goals were to describe the current approaches and review the senior author's technique.
Methods
A literature review was performed using MEDLINE (PubMed) for articles related to esthetic chondrolaryngoplasty for studies published through October 2018. A comprehensive search through the database was conducted using terms “tracheal shave,” OR “chondrolaryngoplasty,” AND “male-to-female,” OR “transgender.” One reviewer screened the titles, abstracts, and full texts of the articles identified. Additional articles were screened after reviewing references of previously identified articles. The search strategy was designed to include only primary evidence and not reviews of the literature, book chapters, or opinion articles. Articles published in English in any journals were considered. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed. Data related to techniques, patient demographics, complications, outcomes, and patient satisfaction were extracted. A total of 13 titles of potentially relevant publications were identified from the database search. The full texts of the 13 articles were reviewed in detail. Of these articles, 4 met inclusion criteria. The remaining articles were excluded because they did not specifically comment on tracheal cartilage surgery, did not present any clinical cases, or did not comment on outcomes.
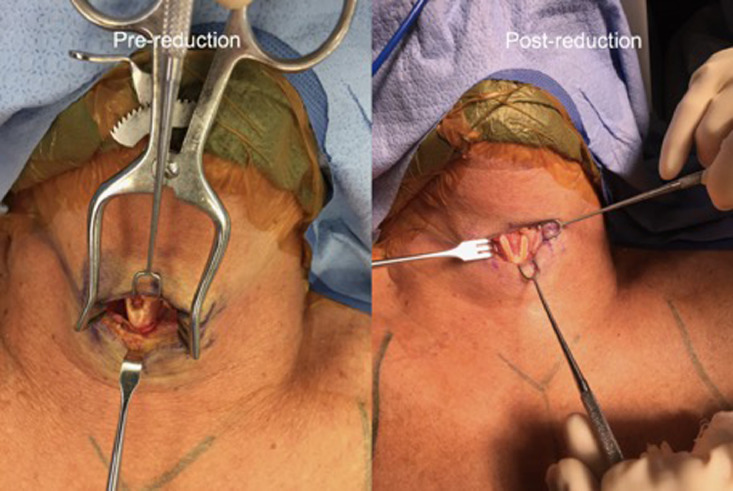
Technique: Authors present the case of a 58 year-old male-to-female transgender patient who underwent chondrolaryngoplasty. We generally perform these cases under general anesthesia with an oral RAE or reinforced endotracheal tube setup, especially when other facial cosmetic procedures or facial feminizing procedures are being performed at the same time. We approach the thyroid cartilage prominence from either a submental incision, entailing a slightly more difficult dissection and less direct visualization of the thyroid cartilage, or a direct incision in the cervicomental crease, as in this case (Figures 1 and 2). The neck strap muscles are identified on either side of the thyroid cartilage, dissected off, and gently retracted laterally. A sharp incision is made through the perichondrium and blunt dissection is performed anterior and posteriorly to raise perichondrial flaps. Under 3.5x loupe magnification, a no. 11 blade is used to serially shave down the thyroid prominence (see Video 1). Once the appropriate volume has been removed, a pineapple burr is used to smooth and contour the edges of the cut thyroid cartilage prominence (see Video 2). This is a particularly important part of the procedure for older patients who have calcified thyroid cartilages that are difficult to cut through. The perichondrial flaps are reapproximated over the thyroid cartilage prominence. The skin is redraped to confirm that a good contour has been achieved and that no further resection is needed. Skin is then closed.
Figure 1.
Lateral preoperative (left) and postoperative view (right) of 58 year-old male-to-female transgender patient who underwent chondrolaryngoplasty with a tracheal shave in combination with high-speed burring for fine contouring.
Figure 2.
Intraoperative view of chondrolaryngoplasty before (left) and after contouring (right).
Results
The investigation did not reveal any systematic reviews or randomized or prospective studies that focused exclusively on chondrolaryngoplasty. Four case series, including 69 patients who had esthetic chondrolaryngoplasty performed, were identified that met inclusion criteria. Of those patients, 84.1% (n = 58) were transgender patients seeking transition from male to female. The mean age of patients was only recorded in two case series. In those case series, 36.2% of patients (n = 25) had multiple procedures performed at the time of chondrolaryngoplasty. Some of these procedures were for additional facial feminization or cosmetic procedures to treat facial aging, but the publication did not report the specifics of these procedures. Mean follow-up was only reported in two of these case series. See Table 1 for additional results.
Table 1.
Characteristics of patients having esthetic chondrolaryngoplasty (NR = not recorded).
| References | Patients (n) | Transgender (n) | Mean age (years) | Additional procedures (n) | Mean follow-up (months) |
|---|---|---|---|---|---|
| Al-Jassim et al. (2006)1 | 1 | 1 (100%) | 49 | 0 | 0.5 |
| Lin et al. (1994)2 | 6 | 6 (100%) | NR | 0 | NR |
| Spiegel et al. (2008)3 | 31 | 31 (100%) | 41 (range 20–67) | 25 (80.6%) | NR |
| Wolfort et al. (1990) | 31 | 20 (64.5%) | NR | 0 | 120 (4–204) |
| Total | 69 | 58 (84.1%) | – | 25 (36.2%) | – |
The most common complications after chondrolaryngoplasty were odynophagia in 20.3% of patients, hoarseness in 36.2% of patients, and laryngospasm in 1.4% of patients. Of patients that had postoperative hoarseness, 96% had resolution within 20 days. Qualitative assessment of patient satisfaction was reported in three studies (n = 63), with a 98.4% satisfaction rate. See Table 2 for additional outcome results.
Table 2.
Postoperative esthetic chondrolaryngoplasty procedure outcomes from case reports/case series that met inclusion criteria (NR = not reported).
| References | Patients (n) | Complications (n) | Time to resolution | Patient satisfaction |
|---|---|---|---|---|
| Al-Jassim et al. (2006)1 | 1 | Hoarseness 3 (100%) | 2 days | 100% |
| Lin et al. (1994)2 | 6 | Hoarseness 3 (50%) | 20 days | NR |
| Spiegel et al. (2008)3 | 31 | Laryngospasm 1 (3.2%) | NR | 96.8% |
| Wolfort et al. (1990) | 31 | Hoarseness 21 (68%) | 65% at <20 days | 100% |
| 3% at 6 months | ||||
| Odynophagia 14 (45%) | 2–3 days | |||
| Total | 69 | Total 42 (60.9%) | 96% at <20 days | 98.4% |
| Hoarseness 27 (39.1%) | ||||
| Laryngospasm 1 (1.5%) | ||||
| Odynophagia 14 (20.3%) |
Discussion
With the current changes in the healthcare landscape, particularly with increasing insurance coverage for gender-affirming surgery, the demand for chondrolaryngoplasty is expected to rise. It is important for plastic surgeons to have knowledge and practice in this procedure to best meet the needs of their transfemale patients.
Various techniques using fine rongeurs for external resection of the superior aspect of the thyroid cartilage5 stemmed from the original procedure described by Wolfort and Parry.5 Wolfort himself modified this approach by adding the use of a burr for contouring.4 In older patients with ossified cartilage, the use of a blade for resection was found to be inconvenient; however, the use of an 11-blade scalpel has been documented without functional complications.4, 5, 7 In this case, a malleable retractor was placed deep to the posterior surface of the thyroid cartilage to prevent injury to any internal structures and dissections were made along the rims of the superior thyroid notch without extending too far posteriorly (>2.5 cm) to avoid damage to the superior laryngeal nerve.7 Alternatively, using shear cartilage cutting forceps was shown to allow more extensive resection and contouring without internal damage.1 In our experience, we have found that “shaving” can result in an excellent outcome, especially when performed with loupe magnification (Video 1). In older patients the cartilage is calcified; hence, using a high-speed burr with concomitant cold irrigation is critical in achieving a smooth contour (Video 2).
Adjuncts to improve visualization of critical anatomy have also been attempted with regard to chondrolaryngoplasty. In a study using laryngeal mask airway (LMA), flexible laryngoscopy, and endoscopy-guided translaryngeal needle placement to identify the level of the anterior commissure, the only dissatisfied patient wanted further reduction of the thyroid cartilage.3 In this case, it would have not been possible due to the risk of anterior commissure displacement that would have resulted in lowering of the voice, an unwanted outcome in the setting of a MtF transgender surgery. Ways to reconstruct the anterior commissure in these patients could be further explored to achieve more optimal esthetic results. In the future, one could consider combining this procedure with cricothyroid approximation to correct pitch changes incurred during aggressive thyroid cartilage reduction, or simply to raise the pitch of voices of MtF transgender patients.8 The current literature does not give us much information with regard to safety of performing concomitant vocal pitch surgery. The results from our study, however, suggest that performing other facial-feminizing or cosmetic procedures at the same time as chondrolaryngoplasty appears to be safe.
The use of general anesthesia and endotracheal intubation has been safely reported.4 However, endotracheal intubation limits the use of flexible laryngoscopes for localization and marking of the anterior commissure tendon. Laryngeal mask airway (LMA) has been proposed as an alternative to endotracheal intubation in chondrolaryngoplasty, as it allows advancement of the endoscope through the LMA until the anterior commissure becomes visible for marking. Local anesthesia also works well, but may lead to a more difficult surgery due to reflexive coughing or swallowing in poorly cooperative patients.3
Regardless of the technique utilized, the anterior commissure tendon must be guarded throughout the length of the procedure, as damage to this structure would result in a lower voice, which would be an unwanted male characteristic in a transwoman.3,8 Removal of the tracheal cartilage prominence is performed above the level of the anterior commissure until the ideal cosmetic goal is achieved, or more importantly, until concerns for injury to the true vocal cords arise. Care must also be taken to remain along the rim of the thyroid cartilage to avoid damage to the thyrohyoid membrane and, in turn, the superior laryngeal nerve and cause laryngeal anesthesia and/or aspiration.1,4 Similarly, thyroepiglottic ligament damage can make the epiglottis unstable and requires reconstruction of its attachment sites to the thyroid cartilage.1 Despite surgeons’ concern for injury to these critical structures, the results from our study demonstrate that the incidence of such injuries is either low or underreported.
It is important to note that although the results of this study are promising, there are drawbacks to the data. Only four of the articles reviewed met inclusion criteria, as many case series did not report patient data or outcomes. Larger studies should be carried out in the future, as feminizing procedures such as chondrolaryngoplasty become more common. As the literature becomes more robust, we will be better able to describe and determine ways to prevent the complications that may accompany esthetic chondrolaryngoplasty.
Overall, chondrolaryngoplasty for reduction of the thyroid cartilage appears to be a safe and effective procedure. Modifications from the original description by Wolfort and Parry5 involve protecting the anterior commissure tendon to prevent voice changes. The complications that occurred in identified case series were mild and self-limiting. Although serious complications are certainly possible, we were not able to identify their occurrence in the literature.
Declaration of Competing Interest
No conflict of interests or funding to disclose.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.jpra.2019.07.002.
Appendix. Supplementary materials
Intraoperative serially shaving of the thyroid cartilage prominence performed under loupe magnification.
Intraoperative burring of the thyroid cartilage edges in an older patient with a partially calcified prominence.
References
- 1.Al-Jassim A.H.H., Lesser T.H.J. Reduction of Adam's apple for appearance. Ind J Otolaryngol Head Neck Surg. 2006;58(2):172–173. doi: 10.1007/BF03050778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin Z., He Q., Zhao Y. Chondrolaryngoplasty. Zhongua Zheng Xing Shao Shang Wai Ke ZaZhi. 1994;10(1):55–57. [PubMed] [Google Scholar]
- 3.Spiegel J.H., Rodriguez G. Chondrolaryngoplasty under general anesthesia using a flexible fiberoptic laryngoscope and laryngeal mask airway. Arch Otolaryngol Head Neck Surg. 2008;134(7):704–708. doi: 10.1001/archotol.134.7.704. [DOI] [PubMed] [Google Scholar]
- 4.Wolfort F.G., Dejerine E.S., Romas D.J., Parry R.G. Chondrolaryngoplasty for appearance. Plast Reconstr Surg. 1990;86(3):464–469. [PubMed] [Google Scholar]
- 5.Wolfort F.G., Parry R.G. Laryngeal chondroplasty for appearance. Plast Reconstr Surg. 1975;56(4):371–374. doi: 10.1097/00006534-197510000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Conrad K., Yoskovitch A. Endoscopically facilitated reduction laryngochondroplasty. Arch Facial Plast Surg. 2003;5(4):345–348. doi: 10.1001/archfaci.5.4.345. [DOI] [PubMed] [Google Scholar]
- 7.Giraldo F., de Grado J., Montes J. Aesthetic reductive thyroid chondroplasty. Int J Oral Maxillofac Surg. 1997;26(1):20–22. doi: 10.1016/s0901-5027(97)80840-5. [DOI] [PubMed] [Google Scholar]
- 8.Brown M., Perry A., Cheesman A.D., Pring T. Pitch change in male-to-female transsexuals: has phonosurgery a role to play? Int J Lang Comm Dis. 2002;35(1):129–136. doi: 10.1080/136828200247296. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Intraoperative serially shaving of the thyroid cartilage prominence performed under loupe magnification.
Intraoperative burring of the thyroid cartilage edges in an older patient with a partially calcified prominence.