Abstract
This case report presents a 34-year-old woman who was referred to our regional plastic surgery unit following a 32-year history of a progressively enlarging mass overlying the left maxilla. The mass was initially diagnosed and treated as a low-flow vascular malformation. However, subsequent histopathological assessment confirmed the diagnosis of a cutaneous neurofibroma. To the best of our knowledge, there are only two other reported cases of a solitary neurofibroma arising from the soft tissue of the face, and this is the first reported case in the United Kingdom (UK). This article highlights difficulties in pre-operative diagnosis of solitary facial neurofibromas. We present our experience in managing this unusual case, discuss radiological clues to aid diagnosis and provide a review of the literature.
Keywords: Neurofibroma, Face, Solitary
Introduction
Neurofibromas are benign nerve sheath tumours and are classified into solitary, diffuse or plexiform lesions.1 Plexiform neurofibromas are pathognomonic of (NF) type 1 and involve long segments of peripheral nerves and their branches.1 Solitary neurofibromas arising from the soft tissue of the face outside of NF is a rare clinical entity. The majority of described facial neurofibromas reported in the literature describe plexiform lesions. We present our experience managing this case and highlight the difficulty of pre-operative diagnosis of solitary neurofibromas and discuss the clinical and radiological differences between neurofibromas and vascular malformations.
Case
A 34-year-old midwife was referred to our regional plastic surgery unit for assessment and management of a lesion overlying her left maxilla. The lesion was first noticed at two years of age and appeared as a small, discolored macule. It grew into a palpable lump during puberty and increased in size again during two pregnancies. It continued to grow slowly throughout her adult life. The lesion was initially painless, but became more painful from age 18. She had magnetic resonance imaging (MRI) of the lesion at that stage, which had been reported as showing a vascular malformation confined to subcutaneous tissues and skin, with a single vascular pedicle. When initially reviewed in our department, the patient chose not to undergo excision, but over the course of one year, she has had increasing pain and swelling of the lesion triggering her to seek further medical advice.
The patient has a background of polycystic ovarian syndrome and takes norethisterone oral contraceptive. She has no family history of NF.
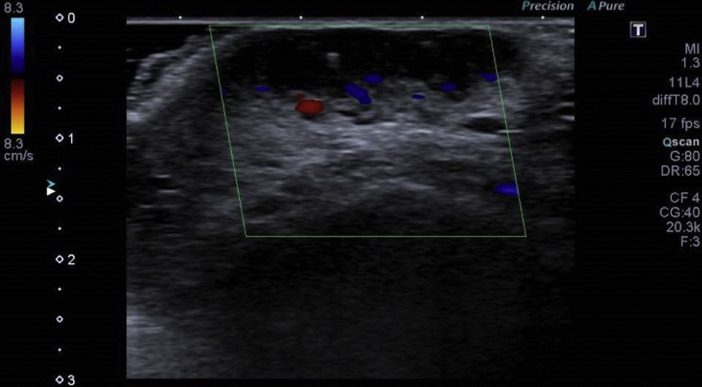
On examination a 3 × 2 cm soft palpable lump was evident over the left maxilla (Figure 1). She had no diagnostic clinical stigmata of neurofibromatosis (NF). Ultrasound confirmed a soft spongy lesion containing vascular spaces with low-flow (Figure 2).
Figure 1.
Clinical photography of the lesion prior to any intervention.
Figure 2.
The lesion was imaged with gray-scale ultrasound and color Doppler. On increasing pressure the lesion could be compressed, but could not be fully emptied, with slow flow in parts of the lesion.
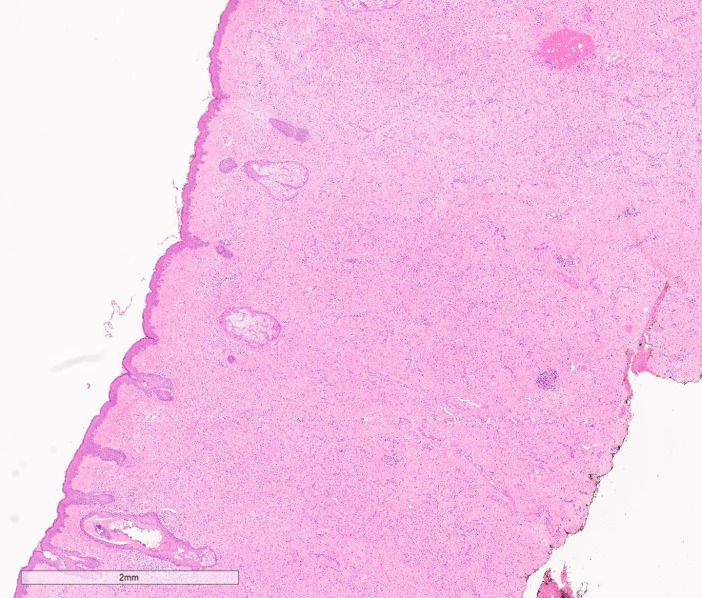
Multidisciplinary discussion between plastic surgery and interventional radiology concluded that the lesion was suitable for direct stick percutaneous sclerotherapy, and that this should be attempted in the first instance to avoid the inherent operative morbidity associated with surgical excision with reconstruction. She underwent sclerotherapy using 3% Fibro-Vein® complexed with air and contrast in a ratio of 1:1:1 as a foam under ultrasound and fluoroscopic control. There were no intra- or post-procedural complications. At the first session 1 mL of sclerosant complex was used. Following sclerotherapy, the lesion remained the same size but the severity of pain did decrease. A second session of sclerotherapy was attempted but placing the needle within the vascular anomaly resulted in arterial puncture showing a fine capillary network filling the lesion. There was reflux into the adjacent facial artery and further attempts at gaining access to the venous component of the anomaly were unsuccessful. The lesion was therefore deemed not suitable for further sclerotherapy, so the patient was listed for excision under general anaesthetic. The aim of surgery was to debulk the lesion to provide better facial contour and symptomatic relief whilst preserving the aesthetic subunit. Prior to skin incision 4ml of 1% lignocaine with 1:200,000 adrenaline was infiltrated around the lesion to facilitate haemostasis. During the dissection it was noted by the operating surgeon (RPW) that the appearance of the tissue, and the pattern of bleeding was different from that expected for a vascular malformation. The lesion was excised intra-lesionally in two piecemeal skin ellipses measuring 25 × 10 × 5 mm and 10 × 5 × 2 mm. The post-operative period was uncomplicated and she was discharged the same day. Histology revealed a benign tumour comprised of spindle cells infiltrating the dermis and surrounding the adnexal structures (Figure 3). Scattered mast cells were present within the tumour and there were no areas of atypia or necrosis to indicate malignant transformation. Overall the appearances were of a benign cutaneous neurofibroma.
Figure 3.
Histology revealed a benign neurofibroma which had the classical appearances of bland spindle cells surrounding the dermal adnexal structures.
Discussion
Neurofibromas are benign nerve sheath tumours of the peripheral nervous system consisting of Schwann cells, perineurial cells and endoneurial fibroblasts.1 They can be solitary, as in this case, diffuse or plexiform. Solitary neurofibromas arise from cutaneous nerves. Diffuse neurofibromas are infiltrative lesions involving the skin and subcutaneous tissues. Plexiform neurofibromas are pathognomonic of NF type 1 (NF-1) and involve long segments of peripheral nerves and their branches.1 The aetiology of sporadic solitary neurofibromas outside the settings of NF-1 currently remains unknown, but some authors consider them to be hyperplastic and hamartomatous in nature rather than neoplastic.2
Sporadic solitary neurofibromas can arise in the face, as in this case, or from the intra-ocular region, eyelid, oral cavity, sinonasal tract, palatine tonsils, thyroid capsule, scalp, frontal bone and mandible. Clinically, the lesion presents with symptoms relating to the size and site of the tumour. Superficial, cutaneous lesions cause a visible mass that deforms the surface, and deeper masses can cause destruction of nearby structures due to pressure. Both can cause neurological symptoms due to compression of the involved nerve. Radiologically, MRI signal characteristics are iso- or hypo-intense on T1-weighted images, and iso- or hyper-intense on T2-weighted images with heterogenous contrast uptake.3 It is recognised that diffuse and plexiform neurofibromas may show imaging characteristics which may be shared with vascular malformations such as iso- or hypo-intensity on T1 weighted MRI, hyper-intensity on T2-weighted and STIR images, diffuse homogeneous enhancement on contrast-enhanced images and presence of flow voids.4 The central dark focus, termed the target sign and present in plexiform neurofibroma on T2-weighted or STIR images, can also mimic phleboliths, which are common in venous malformation.4 To radiologically delineate between these similarities MRI should include T1, T2, STIR and contrast enhanced sequences through the lesion, and all sequences should be congruent with the proposed diagnosis. Other strategies include use of adjunctive 2D gray-scale ultrasound and colour duplex studies. An x-ray of the affected site can be helpful to differentiate a phlebolith from a presumed target sign seen on MRI.4
Macroscopically, neurofibromas are not encapsulated.1 Microscopically, they are immunoreactive for S-100 protein and vimentin, although immunohistochemistry was not carried out in this case as there were classical histological appearances.1
Differential diagnoses include soft tissue sarcoma, schwannoma, lymphatic and vascular malformations. The shared clinical and radiological features of neurofibromas and vascular malformations can make distinguishing between the two difficult. Complete surgical resection is the treatment of choice, although monitoring is required because the lesion may recur. Solitary neurofibromas rarely become malignant, in contrast to plexiform neurofibromas.1
We performed a PubMed literature search using the MeSH headings “solitary”, “neurofibroma” and “face” which yielded 15 titles. After excluding duplicates and cases related to NF, six reports of isolated neurofibroma of the face were identified (Table 1). Of these cases, only two report solitary sporadic facial neurofibromas.5, 6
Table 1.
Review of neurofibroma of the face listed in chronological order of publication.
| Author | Age /Sex | Presentation | Subtype | Location |
|---|---|---|---|---|
| Kobus and Wójcicki (2009)7 | 15/M | Painless swelling with facial disfigurement | Plexiform | Entire left face |
| He et al. (2011)6 | 8/M | Painless swelling | Solitary | Right cheek and infra-temporal fossa |
| Maheshwari et al. (2011)8 | 40/M | Painless swelling | Plexiform | Right parotid |
| Huang and Chong (2013)9 | Middle aged/F | Painless swelling with facial disfigurement | Plexiform | Right supraorbital and periauricular region |
| Rai and Kumar (2015)10 | 36/M | Painless swelling | Plexiform | Right parotid |
| Nilesh et al. (2017)5 | 10/F | Painless swelling with facial disfigurement | Solitary | Left oral commissure to the preauricular region |
M, male; F, female.
The remaining four cases describe facial plexiform neurofibromas, which are pathognomonic of NF-1.7, 8, 9, 10 These cases can therefore be considered part of NF-1 and distinct from sporadic solitary neurofibromas.11
Solitary neurofibromas arising from the soft tissue of the face outside of NF is a rare clinical entity, and this is the first case reported in the UK. The majority of facial neurofibromas reported in the literature describe plexiform lesions. This case highlights the difficulty of pre-operative diagnosis of neurofibromas and the clinical and radiological similarities to the more common vascular malformations which can be mimicked. We outline radiological strategies which may aid diagnosis in equivocal cases. Solitary neurofibromas exacerbate the diagnostic challenge when characteristic clinical features of neurofibromatosis are not present. In cases where diagnostic uncertainty persists, or a presumed venous vascular malformation does not respond as expected to radiological intervention, we advocate tissue biopsy to obtain a definitive histopathologic diagnosis.
Consent
The patient provided written informed consent for the publication and the use of their images.
Financial support
None.
Conflicts of interest
The authors declare that there is no conflict of interest regarding the publication of this paper.
Ethical approval
The study was performed in accordance with the principles of the Declaration of Helsinki.
References
- 1.Rodriguez F.J., Folpe A.L., Giannini C., Perry A. Pathology of peripheral nerve sheath tumors: diagnostic overview and update on selected diagnostic problems. Acta Neuropathol. 2012;123(3):295–319. doi: 10.1007/s00401-012-0954-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marocchio L.S., Oliveira D.T., Pereira M.C., Soares C.T., Fleury R.N. Sporadic and multiple neurofibromas in the head and neck region: a retrospective study of 33 years. Clin Oral Invest. 2007;11(2):165–169. doi: 10.1007/s00784-006-0096-6. [DOI] [PubMed] [Google Scholar]
- 3.Majoie C.B., Hulsmans F.J., Castelijns J.A., Sie L.H., Walter A., Valk J., Albrecht K.W. Primary nerve-sheath tumours of the trigeminal nerve: clinical and MRI findings. Neuroradiology. 1999;41(2):100–108. doi: 10.1007/s002340050713. [DOI] [PubMed] [Google Scholar]
- 4.Yilmaz S., Ozolek J.A., Zammerilla L.L., Fitz C.R., Grunwaldt L.J., Crowley J.J. Neurofibromas with imaging characteristics resembling vascular anomalies. Am J Roentgenol. 2014;203(6):W697–W705. doi: 10.2214/AJR.13.12409. [DOI] [PubMed] [Google Scholar]
- 5.Nilesh K., Naniwadekar R.G., Vande A.V. Large solitary neurofibroma of face in a paediatric patient. J Clin Diagnos Res JCDR. 2017;11(6):ZD04. doi: 10.7860/JCDR/2017/25991.9996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.He Y., Wang J., Zhang Z., Yang H., Fu H. Solitary neurofibroma arising from the infratemporal fossa in a child. J Paediatr Surg. 2011;46(7):E13–E16. doi: 10.1016/j.jpedsurg.2011.03.009. [DOI] [PubMed] [Google Scholar]
- 7.Kobus K., Wójcicki P. Gigant facial neurofibroma. Pol J Surg. 2009;81(1):53–57. [Google Scholar]
- 8.Maheshwari V., Varshney M., Alam K., Khan R., Jain A., Gaur K. Neurofibroma of parotid. BMJ Case Rep. 2011;10:1136. doi: 10.1136/bcr.05.2011.4172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huang W., Chong W.S. Facial plexiform neurofibroma: is it truly just skin deep? BMJ Case Rep. 2013;2013 doi: 10.1136/bcr-2013-200716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arpita Rai A., Kumar A. Neurofibroma of facial nerve presenting as parotid mass. J Maxillofac Oral Surg. 2015;14(Suppl 1):465–468. doi: 10.1007/s12663-014-0681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.National Institutes of Health Consensus Development Conference statement: neurofibromatosis Arch Neurol. 1988;45:575–578. [PubMed] [Google Scholar]