Abstract
Introduction
Gender-affirmation surgery is essential in the management of gender dysphoria. For male-to-female transgender women (transwomen), feminization of the chest is a component in this process. There is minimal literature describing effective and safe techniques for breast augmentation in transwomen. Here we describe our operative techniques and considerations.
Methods
A retrospective review of a single surgeon experience was performed for transwomen who underwent primary breast augmentation between October 1, 2014, and February 1, 2017. Surgical outcomes and complications were analyzed.
Results
Thirty-four patients with an average age of 34.4 years were included in this series (range 19–59 years). Surgical approach was through an inframammary incision with a submuscular pocket and either silicone smooth round (24%) or textured anatomic implants (76%). Six patients experienced postoperative complications (17.6%). Two patients underwent reoperation for implant extrusion (5.9%). Higher BMI and longer preoperative hormonal therapy duration were significantly associated with complications (p = 0.008; p = 0.039, respectively). Feedback from the respondents was overall positive. Most of patients (92.7%) reported being happier and feeling more satisfied with their chest than before their operation. All respondents (100%) reported improvement in their gender dysphoria and would undergo the operation again. Patient dissatisfaction was significantly associated with longer time on preoperative hormones (p = 0.008) and had a trend toward association with higher implant volume (p = 0.083).
Conclusions
Breast augmentation in transwomen is safe and typically leads to high patient satisfaction with improvement of gender dysphoria. Larger, longer term studies are needed to appropriately delineate complication risks and contributing factors.
Keywords: Transgender, Breast augmentation, Outcomes, Patient reported outcomes
Introduction
Gender dysphoria, or the emotional and social distress due to discrepancy between an individual's gender identity and their assigned sex at birth, requires a multidisciplinary approach.1, 2, 3 As such, many individuals benefit from both hormonal and gender-affirmation surgery. Although not all patients with gender dysphoria require surgical intervention, gender-affirmation surgery continues to be recognized as one of the optimal treatments for this patient population.2,4, 5, 6
For male-to-female transgender patients (transwomen), the acquisition of a female appearance is essential to ameliorate the incongruity between gender identity and assigned sex. There are marked differences between the male and female chest. These include differences in the quantity of glandular tissue, as well as a broader breast base diameters and shorter nipple to inframammary fold (IMF) distance in males. In addition, the male nipple-areolar complex (NAC) is smaller, wider spaced, and more ovoid than the female NAC.7,8 A feminized chest is one way for transwomen to present their desired gender in public and private life; it is not surprising that breast augmentation is generally the first, and sometimes only, surgical procedure that transwomen pursue.
Although transwomen typically initiate hormonal therapy before surgical evaluation, there is a wide response range to estrogen therapy. Ultimately, the majority of individuals choose to pursue surgical intervention, with breast augmentation rates reported up to 67% in the transwomen population.9, 10 Importantly, studies have confirmed the positive impact breast augmentation can have for transwomen. Such studies support breast augmentation as a quality-of-life operation and not simply a cosmetic procedure.10, 11
There are many techniques described for primary breast augmentation and implant-based breast reconstruction for the cis-gender population. There is far less literature available describing breast augmentation for transwomen. The purpose of this study is to describe the senior author's preoperative assessment, surgical technique, and surgical limitations of breast augmentation when specifically performed for transwomen along with surgical and patient-reported outcomes.
Methods
The study design was approved by an institutional review board. A retrospective, single-institution, single-surgeon experience was performed for primary breast augmentations that occurred between October 1, 2014, and February 1, 2017. Inclusion criteria for the study were a diagnosis of gender dysphoria, age 18 years or older, and capacity to make informed consent for treatment.
Patient demographic data were compiled, including age, height, weight, body mass index, comorbidities, and pertinent social history. Surgical details including implant characteristics, incision location, and pocket position were reviewed. Surgical outcomes and complications were analyzed. Analysis was performed using Fisher's exact test and Student's unpaired t-test (MedCalc Software, Ostend, Belgium).
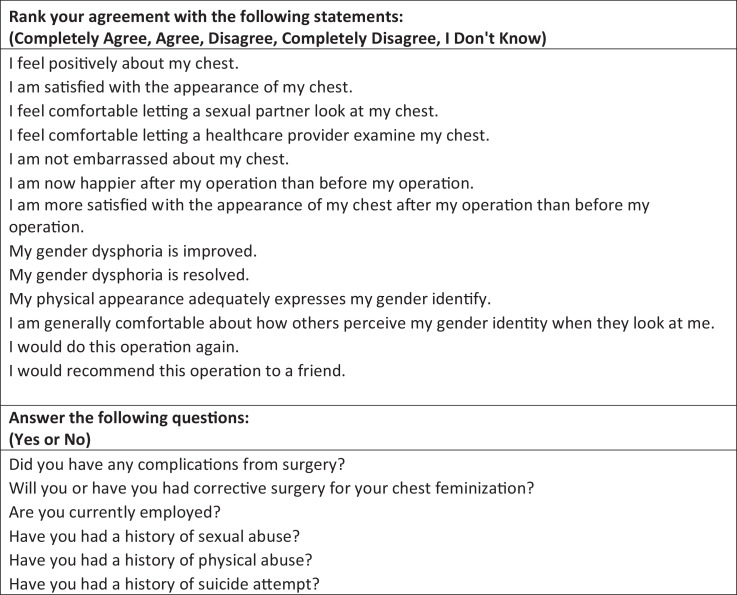
Patient-reported outcome measures (PROMs) were evaluated with a 19-item inventory adapted from previous transgender studies that was delivered electronically (Figure 1).12,13 To date, there have been no validated PROMs for breast augmentation in transwomen. Thus, our inventory attempted to assess not only patient satisfaction but also changes in quality-of-life, psychosocial well-being, and gender dysphoria postoperatively.
Figure 1.
Patient-reported outcome measures were assessed using a 19-item inventory developed by our study team.
Technique
Preoperative assessment
A complete history is obtained and physical examination is made with careful assessment for comorbidities. Patients are instructed to avoid aspirin and other antiplatelet medications if not medically contraindicated. Patients are also instructed to abstain from nicotine products for four weeks before surgery and four weeks after surgery.
The majority of patients are treated with hormonal therapy before undergoing breast augmentation, but this is not mandatory. There is evidence to suggest an increased risk of deep venous thrombosis in transgender women receiving hormonal therapy.14 While we did not routinely ask our patients to stop taking these medications in the perioperative period due to the potential negative emotional and physiological changes experienced by the patient, it was important for the patient to be educated and to understand these risks before proceeding with breast augmentation.
Unlike traditional breast augmentation, the World Professional Association for Transgender Health Standards of Care (WPATH SOC) recommends at least one referral letter from a mental health professional before chest/breast surgery.15 While some argue this may place undue strain on this patient population, it is important to adhere to current WPATH SOC guidelines and request appropriate medical-legal documentation.16, 17
The breast augmentations were performed in the submuscular plane with textured anatomic or smooth round breast implants. We prefer this technique due to the lack of overlying glandular tissue and to provide naturally shaped feminine breasts without the appearance of overly full superior pole. Implant size is determined using a combination of patient preference and surgeon experience in conjunction with patient characteristics including breast base width, height, weight, soft tissue thickness, and preoperative asymmetries. Although described for cis-patients, the authors have found Tebbett's methodology in determining planned implant size and new IMF placement a helpful guide in the trans population.18
Special considerations
As previously mentioned, there are notable anatomic differences between male and female chests, many of which cannot be overcome completely with current reconstructive procedures and devices. Males tend to have wider chests with laterally displaced NACs. When placing an implant, it can be placed either directly behind the NAC (which allows for only limited cleavage) or placed slightly more medial (which will ultimately lead to nipples located more lateral on the breast mound). Fat grafting can help to smooth or fill the medial breast, but it is often difficult to obtain sufficiently feminine cleavage. In addition, we have found that the differences in male and female NAC size and shape tend to be ameliorated when the tissue is placed on stretch from the underlying device. Overall, individuals must be counseled on these differences to offer realistic expectations and discuss the aforementioned tradeoffs before proceeding with surgery.
Preoperative markings and operative technique
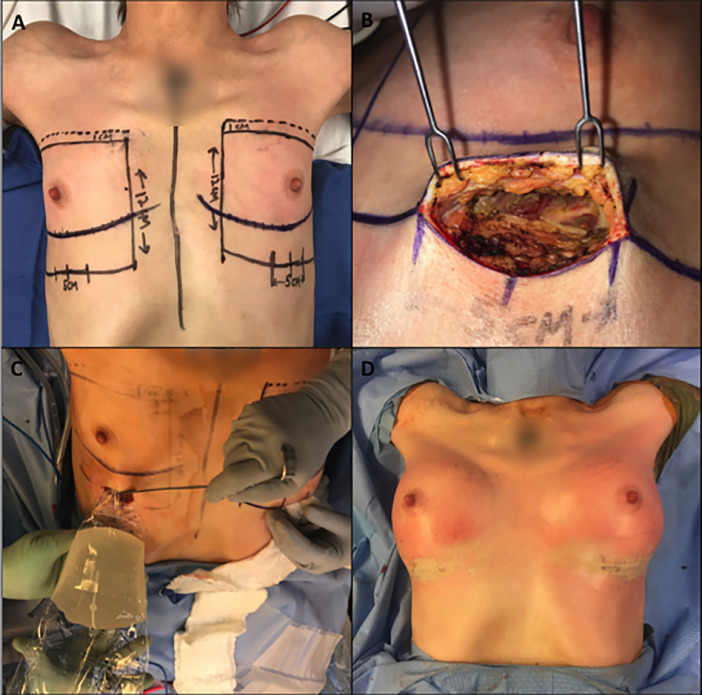
Before surgery, the midline and IMF are marked. Breast diameters are then confirmed. A 3-cm zone between the breasts is marked to avoid undermining in an effort to prevent medial implant migration. The new IMF can be planned according to the desired implant size as noted above. (Figure 2A) In determining the new IMF placement, the authors advocate erring on the incision possibly riding up slightly onto the breast rather than onto the chest; patients tolerate scars on the inferior breast mound better than one visible in a bathing suit or brassiere.
Figure 2.
Preoperative markings (A), surgical plane (B), implant insertion (C), on table result (D).
The procedure is then performed in similar fashion to that of an inframammary, submuscular augmentation in a cis patient (Figure 2B). Notably, the access incision in most circumstances needs to be significantly below the native IMF. In contrast to a cis patient, however, pocket location must be predetermined based on the desire for optimized cleavage vs. nipple position. Care must be taken to dissect a pocket to the exact dimensions of the chosen implant to avoid possible implant migration or rotation. The authors prefer to utilize triple antibiotic solution for irrigation when the pocket has been established.19
Preferably, the implant should be chosen during preoperative consultation. If there is some degree of uncertainty intraoperatively, especially of the overlying skin envelope, saline sizers can be used. These devices should be used with caution to prevent overdissection of the pocket. In rare instances, lateral relaxing incisions may be required.
An implant insertion funnel is typically used for larger implants. (Figure 2C) If there is concern for downward migration, a three-point fixation stitch is used to tack Scarpa's fashion down to the chest wall. The incision is closed in a layered fashion, and a sterile dressing is placed. Immediate postoperative results are shown in Fig. 2D. Preoperative and 1-year postoperative results are shown in Figure 3, Figure 4.
Figure 3.
Preoperative (top) and 1-year postoperative (bottom).
Figure 4.
Preoperative (top) and 1-year postoperative (bottom).
Postoperative care
At the conclusion of the procedure, a circumferentially placed elastic wrap is used for compression. When not medically contraindicated, these procedures are performed as outpatient surgery. At follow-up, the patient is instructed to wear a sports bra for four weeks and to avoid strenuous activities to prevent implant migration.
Additional approaches and adjunctive procedures
While our results have been promising using a single-stage augmentation, there may be utility for a two-stage approach with tissue expansion in select patients. In addition, fat grafting can be performed as an adjunct procedure, especially to the medial and superior poles of the breast to help camouflage widely spaced breasts. Further, NACs that are not sufficiently large can be tattooed to increase the apparent size.
Results
A total of 34 patients who met inclusion criteria for the study were identified. Representative postoperative results are shown in Figures 3 and 4. Patient demographics and implant characteristics are detailed in Table 1. Patient age ranged from 19 to 59 years at the time of operation, with an average age of 34.4 years old. The average follow-up period since time of surgery was 15.9 months (range 0.5–38.7 months). Two patients were lost to follow-up postoperatively. Over one quarter of patients (26.5%) had documented medical comorbidities at the time of operation, and over half (55.9%) had a history of a mental health diagnosis. All implants used were silicone based. The average implant size was 520 cc with a range of 350 to 700 cc. The majority of implants were textured, anatomic devices.
Table 1.
Patient demographics and implant characteristics.
| Demographics | Count |
|---|---|
| Patients | 34 |
| Average (Range) | |
| Age (years) | 34.4 (19–59) |
| Patient Weight (lbs) | 182.2 (120–275) |
| Patient Height (in) | 70 (64–76) |
| BMI | 26.1 (19.4–39.5) |
| Hormone Therapy Period (years) | 3.1 (0–18) |
| Follow-Up Time (months) | 15.9 (0.43–48.7) |
| Count (%) | |
| Medical comorbidities | 9 (26.5) |
| Mental health history | 19 (55.9) |
| Prior chest surgery | 3 (8.8) |
| Tobacco use | 7 (20.6) |
| Illegal drug use | 7 (20.6) |
| Comorbidity Type | Count |
| Diabetes | 3 |
| HIV infection | 4 |
| Hypertension | 4 |
| Heart disease | 1 |
| Implant Characteristics | |
| Average (Range) | |
| Size (cc) | 520 (350–700) |
| Count (%) | |
| Smooth, round | 16 (24%) |
| Textured, anatomic | 52 (76%) |
Our patients experienced an overall complication rate of 17.6%. Complications included hematoma (n = 1), infection (n = 1), extrusion (n = 2), excessive scarring (n = 1), asymmetry (n = 1), hypersensitivity (n = 1), and numbness (n = 1). (Table 2) Two patients underwent reoperation for implant extrusion. Four patients expressed dissatisfaction with their postoperative result.
Table 2.
Surgical outcomes.
| Count (%) | |
|---|---|
| Patients with complications | 6 (17.6%) |
| Specific complications | |
| Hematoma | 1 |
| Infection | 1 |
| Extrusion | 2 |
| Scarring | 1 |
| Asymmetry | 1 |
| Hypersensitivity | 1 |
| Numbness | 1 |
| Patients undergoing reoperation | 2 (5.9%) |
On univariate analysis correlating surgical complications with comorbidities (Table 3), patients with comorbid conditions were not found to be at higher risk of complication (OR=0.5, p = 0.55). Similarly, smoking (OR 2.3, p = 0.40), implant type (OR 0.57, p = 0.63), and age (p = 0.86) were not found to be statistically significant predictors of complications. Interestingly, higher BMI and longer preoperative hormonal therapy were significant predictors of complications in this series (p = 0.008; p = 0.039, respectively). Increased implant size did trend toward significance for higher rates of complication (p = 0.058).
Table 3.
Analysis of characteristics associated with surgical complications.
|
Complications | |||
|---|---|---|---|
| Patient Factor | Odds ratio (p-value) | ||
| Medical Comorbidity | 0.5 (0.55) | ||
| Smoker | 2.3 (0.40) | ||
| Prior chest surgery | 0.75 (0.75) | ||
| Mental health history | 0.56 (0.71) | ||
| Factor | Complication | No Complication | p-value |
|---|---|---|---|
| Age (yrs) | 34.3 | 33.7 | 0.86 |
| BMI | 29.3 | 25.4 | 0.008 |
| Hormonal Therapy Period (mo) | 74.1 | 29.4 | 0.039 |
| Implant size (cc) | 601 | 504 | 0.058 |
When stratifying results by satisfied versus dissatisfied patients (Table 4), comorbidities, smoking, implant type, mental health history, history of abuse, history of suicide attempt, age, and BMI were not significant between the two groups. However, time of hormonal therapy was significant between satisfied and unsatisfied patients (p = 0.008), with longer preoperative hormonal therapy associated with patient dissatisfaction. Increased implant size again appeared to trend toward significance (p = 0.083), with higher implant size associated with patient dissatisfaction.
Table 4.
Analysis of characteristics associated with patient dissatisfaction.
| Patient Factor | Odds ratio (p-value) | ||
|---|---|---|---|
| Medical comorbidity | 0.29 (0.42) | ||
| Smoker | 0.34 (0.5) | ||
| Implant type | 0.26 (0.22) | ||
| Mental health history | 0.56 (0.71) | ||
| History of physical abuse | 2.18 (0.65) | ||
| History of sexual Abuse | 2.18 (0.65) | ||
| History of suicide attempt | 6.7 (0.35) | ||
| Factor | Satisfied | Dissatisfied | p-value |
|---|---|---|---|
| Age (yrs) | 34.2 | 34.75 | 0.93 |
| BMI | 25.7 | 29 | 0.3 |
| Hormonal Therapy Period (mo) | 29.5 | 96 | 0.008 |
| Implant size (cc) | 509 | 614 | 0.083 |
A total of twelve patients (35.3%) responded to the postoperative survey. Feedback from the respondents was overall positive. Most patients (92.7%) reported being happier and feeling more satisfied with their chest after their operation than before their operation. All patients (100%) reported improvement in their gender dysphoria and expressed they would choose to undergo the operation again. Some patients (25%) reported they would seek revisionary surgery after their chest feminization. (Table 5)
Table 5.
Patient-reported outcomes after breast augmentation in transwomen.
| Survey statement (%) | CA | A | D | CD | IDK |
|---|---|---|---|---|---|
| I feel positively about my chest. | 66.7 | 25 | 0 | 8.3 | 0 |
| I am satisfied with the appearance of my chest. | 66.7 | 16.7 | 8.3 | 8.3 | 0 |
| I feel comfortable letting a sexual partner look at my chest. | 83.3 | 8.3 | 0 | 0 | 8.3 |
| I feel comfortable letting a healthcare provider examine my chest. | 83.3 | 16.7 | 0 | 0 | 0 |
| I am not embarrassed about my chest. | 66.7 | 25 | 0 | 8.3 | 0 |
| I am happier now after my operation than before my operation. | 66.7 | 25 | 8.3 | 0 | 0 |
| I am more satisfied with the appearance of my chest now after my operation than before my operation. | 83.3 | 8.3 | 8.3 | 0 | 0 |
| My gender dysphoria is improved. | 58.3 | 41.7 | 0 | 0 | 0 |
| My gender dysphoria is resolved. | 33.3 | 8.3 | 50 | 0 | 0 |
| My physical appearance adequately expresses my gender identity. | 50 | 41.7 | 8.3 | 0 | 0 |
| I am generally comfortable with how others perceive my when they look at me. | 50 | 50 | 0 | 0 | 0 |
| I would do this operation again. | 83.3 | 16.7 | 0 | 0 | 0 |
| I would recommend this operation to a friend. | 66.7 | 33.3 | 0 | 0 | 0 |
| Survey question (%) | Yes | No |
|---|---|---|
| Will you or have you had corrective surgery for your chest feminization? | 25 | 75 |
| Are you currently employed? | 66.7 | 33.3 |
| Have you had a history of sexual abuse? | 16.7 | 83.3 |
| Have you had a history of physical abuse? | 25 | 75 |
| Have you had a history of suicide attempt? | 25 | 75 |
CA = ``Completely Agree,'', A = ``Agree,'' D = ``Disagree,'' CD = ``Completely Disagree,'' IDK = ``I Don't Know''.
Discussion
Despite a large body of literature dedicated to esthetic breast augmentation, there is a paucity of data dedicated specifically to breast augmentation in transwomen. Further, the majority of literature dates back to the 1990s or earlier.10,20, 21, 22 A more recent study has offered data showing improvement in breast satisfaction and psychosocial and sexual well-being for transwomen who have undergone breast augmentation, highlighting the medical necessity of this procedure.11
In our experience, we encountered distinct technical challenges related to differences in male and female anatomy when performing breast augmentation in transwomen. As previously mentioned, there are differences in quantity of glandular tissue, shape and size of chest sternum and chest wall, nipple to IMF distances, and shape and size of NACs.7,8 Further training in the care of transgender patients and gender-affirming surgeries may allow providers to more effectively address the technical challenges in these procedures.23, 24, 25, 26, 27
Despite the fact that the majority of our patients had been taking hormonal therapy for greater than 12 months before undergoing breast augmentation, there was infrequently enough subcutaneous tissue in both the superior and inferior pole to safely support an implant. For that reason, all of our reconstructions required a submuscular plane. This is in contrast to some of the findings of previous studies; Kanhai and colleagues document a preference for the subglandular approach to better “fill” the breast as opposed to a submuscular or dual plane approach.28 Of note, the aforementioned study reported a trend toward larger implants with an average prosthesis volume of 165 cc in 1979 and 287 cc in 1996 28. The apparent trend toward larger implants continues, as our study had an average size of 520 cc, which also favors our preference for a submuscular rather than subglandular approach.
Based on our experience, we have noted a distinct limitation related to chest wall and NAC position. Males tend to have wider chests with laterally displaced NACs. When planning the operation, a decision must be made regarding implant placement relative to the NAC. In our experience, patients prefer to have their nipples centered on their breast mound, often making it difficult to obtain sufficient feminine cleavage, even with adjunctive procedures like fat grafting. This balance needs to be underscored at the preoperative consultation to allow the patient to make the decision regarding these tradeoffs.
While our results were relatively favorable, our group did experience complications in 6 of the 34 patients (17.6%). Specifically, we experienced hematoma (n = 1), infection (n = 1), poor scarring (n = 1), asymmetry (n = 1), hypersensitivity (n = 1), and numbness (n = 1). Further, we had two patients who experienced implant extrusion: one who developed a hematoma with superimposed infection and one who was diagnosed with Ehlers-Danlos syndrome postoperatively. In our analysis, we found that BMI and length of hormone therapy beore operation were significantly higher in individuals who experienced complications. BMI has been correlated with adverse surgical outcomes in many fields, and thus,s this is not surprising.29, 30, 31, 32 Our group is uncertain why the length of hormonal therapy was correlated with complications, but we do note that there were several outliers who had been on hormonal therapy for greater than a decade, potentially confounding results.
Additionally, longer time on hormonal therapy preoperatively was associated with higher dissatisfaction. Once again, the reason is unknown. One could speculate that patients who have been on hormonal therapy for a longer time may have been living in their desired gender role for longer, with potentially a higher degree of dysphoria and higher preoperative expectations. In addition, patients who may have been on hormonal therapy longer preoperatively may have more breast development, and thus, surgical breast augmentation may not seem as dramatic as compared to patients who had minimal breast tissue. This highlights one shortcoming in this study that preoperative breast volumes were not assessed in our patients. Additionally, endocrine therapy also may stimulate the growth of axillary breast tissue, and this may be contributory to dissatisfaction in appearance, although none of the patients in the study expressed this as a concern. Axillary liposuction/lipectomy was not performed in this patient cohort.
In this series, four patients were found to be dissatisfied with their size with 50% wanting to be larger. Interestingly, the two patients who wished to have larger implants were initially augmented with 600cc implants, which was the higher end of the range of this study and the upper limit of what their breast pocket could tolerate at the time of surgery. Although not statistically significant in our study, we found that larger implant sizes trended toward a higher rate of complications and patient dissatisfaction. Given this finding, our group has continued to stress the size limitations to our patients during preoperative counseling and education. There may be a role for a staged procedure with a tissue expander for patients who desire a size that far exceeds their available breast pocket.
Based on our PROMs data, we found a high level of satisfaction and improvement in our patients’ quality of life following breast augmentation. (Table 5) In addition, 100% of respondents either completely agreed or agreed that their gender dysphoria was improved following breast augmentation. Complete resolution of gender dysphoria following breast augmentation was minimal. This is not surprising, as there are many aspects of gender-affirmation beyond chest appearance. Yet, these are valuable data supporting the efficacy of this procedure. Further studies are needed to determine validated, standardized patient-reported outcome measures for gender-affirming surgery, and these data will continue to alter considerations in these procedures.33, 34, 35
Despite these promising early results, our study has several limitations. First, this is a single-institution, single-surgeon experience. While different types of implants were used, a similar submuscular technique was employed for all patients. We understand that there are several ways to perform this operation, but in the senior author's hands, this technique offers safe, reliable, and replicable results. Additionally, this study is limited by the relatively small sample size and variable follow-up times. To date, few surgeons offer dedicated care to transgender patients; hence, a significant portion of the senior author's practice is made up of patients who travel long distances for care. Thus, it is not surprising that several of the patients in this study were lost to follow-up or were unable to be contacted to perform the PROM inventory. Finally, the PROM inventory was not completed by any of the six patients who experienced a complication. This may lead to some level of response bias in our PROM data but unlikely to negate the overall positive responses from patients who participated in this portion of our study. Despite these limitations, this study offers insight into the preoperative planning, intraoperative strategy, postoperative complications, overall limitations, and the clinical value and efficacy of breast augmentation in transwomen.
Conclusions
Breast augmentation in transwomen poses technical challenges unique to this patient population. While there are strategies to cope with the anatomic differences between male and female chests and NACs, certain characteristics are difficult to overcome and hence should be discussed with patients before proceeding with surgery. Overall, this operation is clinically meaningful, and additional research is needed to continue to offer this population optimal and reliable results.
Acknowledgments
Acknowledgments
This study was not sponsored, and the content herein is wholly the work of the included authors.
Disclosure
The authors have no financial interest to declare in relation to the content of this work.
References
- 1.Association AP . (5th edition) Washington D.C.; American Psychiatric Association: 2013. Diagnostic and statistical maunal of mental disorders. [Google Scholar]
- 2.Selvaggi G., Bellringer J. Gender reassignment surgery: An overview. Nat Rev Urol. 2011;8:274–282. doi: 10.1038/nrurol.2011.46. [DOI] [PubMed] [Google Scholar]
- 3.Morrison S.D., Chen M.L., Crane C.N. An overview of female-to-male gender-confirming surgery. Nat Rev Urol. 2017;14:486–500. doi: 10.1038/nrurol.2017.64. [DOI] [PubMed] [Google Scholar]
- 4.Wilson S.C., Morrison S.D., Anzai L. Masculinizing top surgery: A systematic review of techniques and outcomes. Ann Plast Surg. 2018;80(6):679–683. doi: 10.1097/SAP.0000000000001354. [DOI] [PubMed] [Google Scholar]
- 5.Remington AC, Morrison SD, Massie JP, et al. Outcomes after Phalloplasty: Do transgender patients and multiple urethral procedures carry a higher rate of complication?Plast Reconstr Surg2018: 141: 220E–29E. [DOI] [PubMed]
- 6.Morrison S.D., Vyas K.S., Motakef S. Facial feminization: Systematic review of the literature. Plast Reconstr Surg. 2016;137:1759–1770. doi: 10.1097/PRS.0000000000002171. [DOI] [PubMed] [Google Scholar]
- 7.Beckenstein M.S., Windle B.H., Stroup R.T. Anatomical position for the nipple position and areolar diameter in males. Ann Plast Surg. 1996;36:33–36. doi: 10.1097/00000637-199601000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Shulman O., Badani E., Wolf Y., Hauben D.J. Appropriate location of the nipple-areola complex in males. Plast Reconstr Surg. 2001;108:348–351. doi: 10.1097/00006534-200108000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Orentrei. N., Durr N.P. Mammogenesis in transsexuals. J Invest Dermatol. 1974;63:142–146. doi: 10.1111/1523-1747.ep12678272. [DOI] [PubMed] [Google Scholar]
- 10.Kanhai R.C., Hage J.J., Asscheman H., Mulder W.J., Hage J. Augmentation mammaplasty in male-to-female transsexuals. Plast Reconstr Surg. 1999;104:542–549. doi: 10.1097/00006534-199908000-00039. [DOI] [PubMed] [Google Scholar]
- 11.Weigert R., Frison E., Sessiecq Q., Al Mutairi K., Casoli V. Patient satisfaction with breasts and psychosocial, sexual, and physical well-being after breast augmentation in male-to-female transsexuals. Plast Reconstr Surg. 2013;132:1421–1429. doi: 10.1097/01.prs.0000434415.70711.49. [DOI] [PubMed] [Google Scholar]
- 12.Morrison S.D., Satterwhite T., Grant D.W. Long-Term outcomes of rectosigmoid neocolporrhaphy in male-to-female gender reassignment surgery. Plast Reconstr Surg. 2015;136:386–394. doi: 10.1097/PRS.0000000000001459. [DOI] [PubMed] [Google Scholar]
- 13.Massie JP M.S., Van Maasdam J., Satterwhite T. Predictors of patient satisfaction and post-operative complications in penile inversion vaginoplasty. Plast Reconstr Surg. 2018;141(6):911e–921e. doi: 10.1097/PRS.0000000000004427. [DOI] [PubMed] [Google Scholar]
- 14.Gooren L.J. Care of transsexual persons. N Engl J Med. 2011;364:1251–1257. doi: 10.1056/NEJMcp1008161. [DOI] [PubMed] [Google Scholar]
- 15.Coleman E., Bockting W., Botzer M. Standards of care for the health of transsexual, transgender, and gender-nonconforming people, version 7. Int J Transgenderism. 2012;13:165–232. [Google Scholar]
- 16.Salgado C.J., Fein L.A. Breast augmentation in transgender women and the lack of adherence amongst plastic surgeons to professional standards of care. J Plast Reconst Aesthet Surg. 2015;68:1471–1472. doi: 10.1016/j.bjps.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 17.Latham J. Ethical issues in considering transsexual surgeries as aesthetic plastic surgery. Aesthet Plast Surg. 2013;37:648–649. doi: 10.1007/s00266-013-0100-x. [DOI] [PubMed] [Google Scholar]
- 18.Tebbetts J.B., Adams W.P. Five critical decisions in breast augmentation using five measurements in 5 minutes: The high five decision support process. Plast Reconstr Surg. 2005;116:2005–2016. [PubMed] [Google Scholar]
- 19.Adams W.P., Rios J.L., Smith S.J. Enhancing patient outcomes in aesthetic and reconstructive breast surgery using triple antibiotic breast irrigation: Six-year prospective clinical study. Plast Reconstr Surg. 2006;118:46S–52S. doi: 10.1097/01.prs.0000185671.51993.7e. (Reprinted from Plast. Reconstr. Surg., vol 117(1), pg 30, 2006) [DOI] [PubMed] [Google Scholar]
- 20.Ratnam S., Lim S. Augmentation mammoplasty for the male transsexual. Singap Med J. 1982;23:107–109. [PubMed] [Google Scholar]
- 21.Hidalgo D.A. Breast augmentation: Choosing the optimal incision, implant, and pocket plane. Plast Reconstr Surg. 2000;105:2202–2216. doi: 10.1097/00006534-200005000-00047. [DOI] [PubMed] [Google Scholar]
- 22.Hage J.J., Karim R.B., Kanhai R.C.J. Augmentation mammaplasty in male-to-female trans-sexuals: Facts and figures from Amsterdam. Scand J Plast Reconstruct Surg Hand Surg. 2001;35:203–206. doi: 10.1080/028443101300165354. [DOI] [PubMed] [Google Scholar]
- 23.Morrison S.D., Chong H.J., Dy G.W. Educational exposure to transgender patient care in plastic surgery training. Plast Reconstr Surg. 2016;138:944–953. doi: 10.1097/PRS.0000000000002559. [DOI] [PubMed] [Google Scholar]
- 24.Morrison S.D., Dy G.W., Chong H.J. Transgender-Related education in plastic surgery and urology residency programs. J Grad Med Educ. 2017;9:178–183. doi: 10.4300/JGME-D-16-00417.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morrison S.D., Wilson S.C., Smith J.R. Are we adequately preparing our trainees to care for transgender patients? J Grad Med Educ. 2017;9 doi: 10.4300/JGME-D-16-00712.1. 258–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith J.R., Morrison S.D., Gottlieb L.J. Are surgical residents prepared for fellowship training in gender-confirming surgery? J Sex Med. 2017;14:1066–1067. doi: 10.1016/j.jsxm.2017.05.017. [DOI] [PubMed] [Google Scholar]
- 27.Morrison S.D., Smith J.R., Mandell S.P. Are surgical residents prepared to care for transgender patients? JAMA Surg. 2018;153:92–93. doi: 10.1001/jamasurg.2017.4024. [DOI] [PubMed] [Google Scholar]
- 28.Kanhai R.C.J., Hage J.J., Asscheman H., Mulder J.W. Augmentation mammaplasty in male-to-female transsexuals. Plast Reconstr Sur. 1999;104:542–549. doi: 10.1097/00006534-199908000-00039. [DOI] [PubMed] [Google Scholar]
- 29.Conner SN, Tuuli MG, Longman RE, et al. Impact of obesity on incision-to-delivery interval and neonatal outcomes at cesarean delivery. Am J Obstet Gynecol2013: 209. [DOI] [PMC free article] [PubMed]
- 30.Bhashyam N., De la Garza Ramos R., Nakhla J. Impact of body mass index on 30-day outcomes after spinopelvic fixation surgery. Surg Neurol Int. 2017;8 doi: 10.4103/sni.sni_115_17. 176–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Giordano S.A., Garvey P.B., Baumann D.P., Liu J., Butler C.E. The impact of body mass index on abdominal wall reconstruction outcomes: A comparative study. Plast Reconstr Surg. 2017;139:1234–1244. doi: 10.1097/PRS.0000000000003264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rao S., Stolle E.C., Sher S. A multiple logistic regression analysis of complications following microsurgical breast reconstruction. Gland Surg. 2014;3:226–231. doi: 10.3978/j.issn.2227-684X.2014.10.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Morrison S.D., Massie J.P., Crowe C.S., Smith J.R. Patient-reported outcomes needed for chest masculinization. Ann Plast Surg. 2018;80:90–91. doi: 10.1097/SAP.0000000000001130. [DOI] [PubMed] [Google Scholar]
- 34.Massie JP, Morrison SD, Smith JR, Wilson SC, Satterwhite T. Patient-reported outcomes in gender confirming surgery. Plast Reconstr Surg 2017: 140: 236E–37E. [DOI] [PubMed]
- 35.Cho D.Y., Massie J.P., Morrison S.D. Ethnic considerations for rhinoplasty in facial feminization. JAMA Facial Plast Surg. 2017;19 doi: 10.1001/jamafacial.2017.0223. 243–243. [DOI] [PubMed] [Google Scholar]