Abstract
Objective:
Women with pregnancies complicated by hypertensive disorders of pregnancy (HDP) have increased long-term cardiovascular (CV) risk. We sought to determine if they demonstrate increased short-term CV risk.
Methods:
Using administrative records, all hospital-based deliveries in Florida from 2004 through 2010 and subsequent readmission to any Florida hospital within 3 years of index delivery were identified. Deliveries and clinical diagnoses were determined using ICD-9 CM codes. HDP included pregnancies complicated by gestational hypertension, preeclampsia, or eclampsia. Outcomes were CV readmission (acute myocardial infarction, stroke, or heart failure), non-CV readmission, and any readmission within 3 years of delivery excluding subsequent deliveries. Associations were determined using multivariate logistic regression.
Results:
Among 1,452,926 records from delivering mothers of singleton infants (mean age 27.2 ± 6.2 years; 52% white, 23% African American [AA], 18% Hispanic), there were 4,054 CV and 259,252 non-CV readmissions. Women with HDP had higher CV readmission rates (6.4 vs 2.5/1000 deliveries; p<0.001). AA women had higher rates of CV readmission than whites or Hispanics (6.8 vs 1.7 vs 1.0/1000 deliveries, respectively; p<0.001). Women with HDP had higher multivariate risk of CV readmission (OR 2.41; 95% CI 2.08–2.80) and any readmission (OR 1.13; 95% CI 1.10 – 1.15). Compared with whites, AA women had higher risk for CV readmission (OR 3.60; 95% CI 3.32 – 3.90) after adjustment for HDP.
Conclusion:
Women with HDP had twice the risk of CV readmission within 3 years of delivery, with higher rates among AA women. More work is needed to explore preventive strategies for HDP-associated events.
Keywords: cardiac risk factors and prevention, pregnancy, hypertension, heart disease
INTRODUCTION
Cardiovascular (CV) disease remains the number one killer of women,1 but current risk prediction models and clinical risk calculators poorly predict a woman’s future CV risk.2–4 Obstetric complications and their relationship to underlying vascular health may be an opportunity for improved CV risk prediction. A single pregnancy complicated by a hypertensive disorder of pregnancy (HDP) has been shown to increase long-term CV risk through population studies.5–7 Accordingly, in 2011 the American Heart Association updated clinical guidelines to include HDP as a major risk factor for CV disease in women.8
The definition of HDP includes gestational hypertension – defined as the development of hypertension (HTN) after 20 weeks’ gestation without proteinuria, preeclampsia – defined as the development of HTN after 20 weeks’ gestation with proteinuria or evidence of end-organ damage up to 6 weeks postpartum, and eclampsia – defined as the development of grand mal seizures in a woman with preeclampsia.9 Current estimates show that HDP complicates about 10%−15% of pregnancies10 and represents a spectrum of disease that can progress from less severe (gestational HTN) to more severe (eclampsia). One mechanism for the association between increased CV risk and HDP is that predisposed women manifest with hypertensive phenotypes during pregnancy due to global endothelial dysfunction which unmasks preexisting subclinical vascular disease.11,12,13 Clinically the treatment for HDP is delivery, but many women who develop HDP have higher rates of CV risk factors before14 and after15,16 pregnancy, suggesting CV risk extends beyond gestation. While the majority of available evidence shows increased risk of CV events decades after a pregnancy complicated by HDP, there is growing evidence suggesting women with HDP may have higher short-term CV risk as well.17
Knowledge of the timing and type of CV events that occur in association with HDP could provide valuable insight for future preventive strategies. The purpose of this analysis was to determine if women with a pregnancy complicated by HDP are at increased risk of CV events in the short-term following delivery. We hypothesized women with a singleton pregnancy complicated by HDP would have increased risk of a CV event within 3 years of delivery compared with women who did not have a pregnancy complicated by HDP.
METHODS
Following approval by our institutional review board, we used administrative hospital discharge data from Florida through the Healthcare Cost and Utilization Project (HCUP) State Inpatient Database (SID) and constructed a retrospective cohort that included all in-hospital deliveries from 2004 through 2010. Because data are available publicly, informed consent was waived. Per the HCUP Data Use Agreement, cell sizes under ten were reported as “<10” for privacy protection. Only a single (index) pregnancy was included for each woman in the analysis. Index pregnancy was defined as the first new singleton delivery occurring between the years 2004–2010 regardless of parity. All included records were collected through 2013 to allow 3 years of follow up. We determined demographics, comorbid conditions, procedures performed during admission, and outcomes at the time of discharge from the index admission. Records that listed male sex of the mother or pregnancy with multiples (e.g. twins, triplets, etc.) were excluded. Multiples were excluded because of known higher risk of developing HDP compared with singleton pregnancies.18,19 Race and ethnicity were stratified into four broad categories: white, African American (AA), Hispanic, and other, which included all remaining races and ethnicities due to small sample sizes. Age was evaluated as both a continuous variable and categorical by decade due to potential for bimodal distribution of comorbidities or adverse outcomes at extremes of maternal age. Parity could not be determined due to lack of direct documentation in administrative data, limited time interval of study, and inability to account for births in other states.
Comorbid diagnoses and performed procedures were determined using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes (Supplemental Table 1). Our predictor of interest was HDP, defined as a composite of gestational HTN (ICD-9 CM code 642.3), preeclampsia (642.4, 642.5), and eclampsia (642.6) diagnosed during the index admission for delivery. Creating a composite HDP predictor allowed for inclusion of women reclassified from gestational HTN to preeclampsia following updated preeclampsia guidelines published in 2013.9 Chronic HTN complicating pregnancy (642.0, 642.1, 642.2) was excluded from the HDP exposure group and considered a comorbid condition because it is a known risk factor for CV events.10,20 Additionally, women with individual codes for both chronic HTN and preeclampsia or gestational HTN were excluded from the HDP exposure group because of an inability to verify if women had both conditions. This was felt to be the more conservative approach, as chronic HTN independently predicts CV events10,20 and women misclassified as having HDP might affect the observed association between our primary predictor (HDP) and readmission outcomes. Women with a specific diagnosis of preeclampsia or eclampsia superimposed on chronic HTN (642.7) were included in the HDP exposure group. There were 1391 deliveries double-coded as gestational HTN and preeclampsia, 114 deliveries double-coded as preeclampsia and eclampsia, and 68 deliveries double-coded as gestational HTN and eclampsia, likely representing progression to a more severe form of HDP, but were considered a single case of HDP in our dataset (i.e. women were not double counted). Only women with a diagnosis of HDP prior to hospital discharge for the index delivery were included as we were unable to capture new cases diagnosed in the outpatient setting postpartum. Our primary outcome was CV readmission to any hospital in Florida within 3 years of delivery. Secondary outcomes included all-cause readmission, non-CV readmission, and time to first readmission. Readmissions for subsequent pregnancies and deliveries were excluded. Primary admission diagnoses were used to determine the reason for readmission and stratified by readmission type: CV readmission – defined as a composite of acute myocardial infarction (410.x, 414.12), acute stroke (430, 431, 432.x, 433.x, 434.x, 435.x, 436), and acute heart failure (425.4, 425.8, 428.x, 674.5), non-CV readmission, and no readmission. Time to first readmission was measured from the index delivery and tracked until the first readmission only. Readmissions within the first 42 days postpartum were measured as these were within the diagnostic window and complication period for preeclampsia/eclampsia and could represent complications related to the pregnancy.
Statistical Analysis
Analyses were performed using a chi-square test for categorical variables and Student’s t test for continuous variables. Associations were determined using logistic regression. Kaplan-Meier survival curves were built for time to first readmission with failure defined as first CV readmission and first readmission for any cause. Given the large sample size and anticipation that all covariates would be significant, the multivariate model was built in serial fashion with the following covariates: age, race/ethnicity, obstetric complications (preterm delivery, cesarean delivery, gestational diabetes), diagnoses and complications likely related to the pregnancy (transfusion, anemia, thrombocytopenia, acute renal failure), comorbid conditions (tobacco, alcohol/drug abuse, chronic HTN, coronary artery disease, hyperlipidemia, heart failure, diabetes, chronic kidney disease, obesity, chronic obstructive pulmonary disease, asthma, depression, autoimmune disorder), and payer (Medicare, Medicaid, private, or unknown), which served as a proxy for socioeconomic status. Interaction testing was performed and significant interaction terms were entered into the multivariate model. Statistical significance was set at a p-value of <0.05. All statistical analyses were performed using Stata (StataCorp, College Station, TX) version 14.1.
RESULTS
The overall sample included 1,452,926 singleton in-hospital deliveries that occurred in Florida between the years 2004 to 2010. Over 60% of women were between the ages of 18–29 years (mean 27.2 ± 6.2 years). There were 108,875 pregnancies complicated by HDP (7% gestational HTN, 11% preeclampsia, <1% eclampsia) at the time of index delivery. A summary of baseline demographics and clinical profiles stratified by HDP status from the index admission for delivery are shown in Table 1. Women with HDP were younger and had higher rates of obesity, anemia, preterm delivery, and cesarean delivery. When all women were stratified by readmission status (Table 2), women with CV readmissions were older and had higher rates of obesity, heart failure, anemia, depression, and HDP at the time of index delivery. These women also had higher rates of preterm delivery and cesarean delivery. Of the 4,054 CV readmissions, 701 (17.3%) were women with HDP during the index delivery, giving an event rate of 6.4 CV readmissions per 1,000 women with HDP over 3 years compared with an event rate of 2.5 CV readmissions per 1,000 women without HDP over 3 years.
Table 1.
Characteristics from index admission for delivery by HDP status
| Overall | No HDP | HDP | p-value | ||
|---|---|---|---|---|---|
| Total Pregnancies (n) | 1,452,926 | 1,344,051 | 108,875 | … | |
| Age (years) | No. (% Column) | ||||
| Mean ± SD | 27.2 ± 6.2 | 27.3 ± 6.2 | 26.5 ± 6.4 | <0.001 | |
| <18 | 49,978 (3%) | 44,631 (3%) | 5,347 (5%) | <0.001 | |
| 18–29 | 886,753 (61%) | 817,939 (61%) | 68,814 (63%) | ||
| 30–39 | 476,462 (33%) | 444,862 (33%) | 31,600 (29%) | ||
| 40≤ | 39,733 (3%) | 36,619 (3%) | 3,114 (3%) | ||
| Race & Ethnicity | No. (% Column) | ||||
| White | 750,453 (52%) | 694,781 (52%) | 55,672 (51%) | <0.001 | |
| African American | 339,186 (23%) | 307,674 (23%) | 31,512 (29%) | ||
| Hispanic | 260,624 (18%) | 244,520 (18%) | 16,104 (15%) | ||
| Other | 26,410 (2%) | 25,175 (2%) | 1,235 (1%) | ||
| Unknown | 76,253 (5%) | 71,901 (5%) | 4,352 (4%) | ||
| Payer | No. (% Column) | ||||
| Medicare | 10,908 (1%) | 9,979 (1%) | 929 (1%) | <0.001 | |
| Medicaid | 721,511 (50%) | 666,408 (50%) | 55,103 (51%) | ||
| Private | 640,607 (44%) | 593,026 (44%) | 47,581 (44%) | ||
| Unknown | 79,900 (5%) | 74,638 (6%) | 5,262 (5%) | ||
| *Discharge Diagnoses | No. (% Column) | ||||
| Chronic Hypertension | 12,668 (1%) | 11,733 (1%) | 935 (1%) | NS | |
| Coronary Artery Disease | 137 (<1%) | 122 (<1%) | 15 (<1%) | NS | |
| Heart Failure | 855 (<1%) | 570 (<1%) | 285 (<1%) | <0.001 | |
| Hyperlipidemia | 604 (<1%) | 523 (<1%) | 81 (<1%) | <0.001 | |
| Arial Fibrillation | 354 (<1%) | 313 (<1%) | 41 (<1%) | 0.003 | |
| Obesity | 33,759 (2%) | 27,226 (2%) | 6,533 (6%) | <0.001 | |
| Diabetes Mellitus | 16,226 (1%) | 13,326 (1%) | 2,900 (3%) | <0.001 | |
| COPD | 47,140 (3%) | 42,595 (3%) | 4,545 (4%) | <0.001 | |
| Asthma | 46,781 (3%) | 42,273 (3%) | 4,508 (4%) | <0.001 | |
| Alcohol & Drugs of Abuse | 24,435 (2%) | 22,706 (2%) | 1,729 (2%) | 0.012 | |
| Tobacco | 80,278 (6%) | 74,375 (6%) | 5,903 (5%) | NS | |
| Chronic Kidney Disease | 681 (<1%) | 567 (<1%) | 114 (<1%) | <0.001 | |
| Acute Renal Failure | 676 (<1%) | 481 (<1%) | 195 (<1%) | <0.001 | |
| Anemia | 135,314 (9%) | 120,554 (9%) | 14,760 (14%) | <0.001 | |
| Thrombocytopenia | 10,412 (1%) | 7,730 (1%) | 2,682 (2%) | <0.001 | |
| Transfusion | 12,950 (1%) | 10,562 (1%) | 2,388 (2%) | <0.001 | |
| Anxiety | 12,869 (1%) | 11,247 (1%) | 1,622 (2%) | <0.001 | |
| Depression | 21,131 (1%) | 18,955 (1%) | 2,176 (2%) | <0.001 | |
| Autoimmune | 5,698 (<1%) | 4,928 (<1%) | 770 (1%) | <0.001 | |
| Stroke | 80 (<1%) | 27 (<1%) | 53 (<1%) | <0.001 | |
| TIA | 59 (<1%) | 50 (<1%) | <10 (<1%) | NS | |
| ICH | 56 (<1%) | 35 (<1%) | 21 (<1%) | <0.001 | |
| Obstetric Diagnoses | No. (% Column) | ||||
| Gestational Diabetes | 16,001 (1%) | 13,128 (1%) | 2,873 (3%) | <0.001 | |
| Preterm Delivery | 112,560 (8%) | 94,904 (7%) | 17,656 (16%) | <0.001 | |
| Stillbirth | <10 (<1%) | <10 (<1%) | <10 (<1%) | NS | |
| Cesarean Delivery | 542,269 (37%) | 487,132 (36%) | 55,137 (51%) | <0.001 | |
| Assisted Pregnancy | 338 (<1%) | 310 (<1%) | 28 (<1%) | NS | |
Discharge diagnoses from the index admission for delivery; NS = Not Significant
HDP = Hypertensive Disorder of Pregnancy; COPD = Chronic Obstructive Pulmonary Disease; ICH = Intracerebral Hemorrhage; TIA = Transient Ischemic Attack
Table 2.
Breakdown of characteristics from index admission for delivery by readmission status
| CV Readmission | Non-CV Readmission | No Readmission | p-value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Total Pregnancies (n) | 4,054 | 259,252 | 1,189,620 | … | |||||
| Age (years) | No. (% Column) | ||||||||
| Mean ± SD | 28.4 ± 6.3 | 25.6 ± 5.9 | 27.5 ± 6.2 | <0.001 | |||||
| Race & Ethnicity | No. (% Column) | ||||||||
| White | 1,265 (31%) | 126,489 (49%) | 622,699 (52%) | <0.001 | |||||
| African American | 2,296 (57%) | 82,283 (32%) | 254,607 (21%) | ||||||
| Hispanic | 263 (6%) | 39,005 (15%) | 221,356 (19%) | ||||||
| Other | 64 (2%) | 2,174 (1%) | 24,172 (2%) | ||||||
| Unknown | 166 (4%) | 9,301 (3%) | 66,786 (6%) | ||||||
| Payer | No. (% Column) | ||||||||
| Medicare | 135 (4%) | 6,875 (3%) | 3,898 (<1%) | <0.001 | |||||
| Medicaid | 2,677 (66%) | 168,798 (65%) | 550,036 (46%) | ||||||
| Private | 1,068 (26%) | 72,010 (28%) | 567,529 (48%) | ||||||
| Unknown | 174 (4%) | 11,569 (4%) | 68,157 (6%) | ||||||
| *Discharge Diagnoses | No. (% Column) | ||||||||
| Chronic Hypertension | 32 (1%) | 2,216 (1%) | 10,420 (1%) | NS | |||||
| Coronary Artery Disease | 23 (1%) | 72 (<1%) | 42 (<1%) | <0.001 | |||||
| Heart Failure | 244 (6%) | 309 (<1%) | 302 (<1%) | <0.001 | |||||
| Hyperlipidemia | 21 (1%) | 206 (<1%) | 377 (<1%) | <0.001 | |||||
| Arial Fibrillation | <10 (<1%) | 198 (<1%) | 151 (<1%) | <0.001 | |||||
| Obesity | 490 (12%) | 10,683 (4%) | 22,586 (2%) | <0.001 | |||||
| Diabetes Mellitus | 290 (7%) | 7,762 (3%) | 8,174 (1%) | <0.001 | |||||
| COPD | 310 (8%) | 16,001 (6%) | 30,829 (3%) | <0.001 | |||||
| Asthma | 286 (7%) | 15,840 (6%) | 30,655 (3%) | <0.001 | |||||
| Alcohol & Drugs of Abuse | 216 (5%) | 11,790 (5%) | 12,429 (1%) | <0.001 | |||||
| Tobacco | 385 (10%) | 24,888 (10%) | 55,005 (5%) | <0.001 | |||||
| Chronic Kidney Disease | 55 (1%) | 520 (<1%) | 106 (<1%) | <0.001 | |||||
| Acute Renal Failure | 61 (2%) | 471 (<1%) | 144 (<1%) | <0.001 | |||||
| Anemia | 763 (19%) | 37,125 (14%) | 97,426 (8%) | <0.001 | |||||
| Thrombocytopenia | 61 (2%) | 2,270 (1%) | 8,081 (1%) | <0.001 | |||||
| Transfusion | 122 (3%) | 5,845 (2%) | 6,983 (1%) | <0.001 | |||||
| Anxiety | 48 (1%) | 4,883 (2%) | 7,938 (1%) | <0.001 | |||||
| Depression | 191 (5%) | 8,063 (3%) | 12,877 (1%) | <0.001 | |||||
| Autoimmune | 59 (1%) | 3,126 (1%) | 2,513 (<1%) | <0.001 | |||||
| Stroke | <10 (<1%) | 51 (<1%) | 28 (<1%) | <0.001 | |||||
| TIA | <10 (<1%) | 27 (<1%) | 31 (<1%) | <0.001 | |||||
| ICH | <10 (<1%) | 24 (<1%) | 32 (<1%) | <0.001 | |||||
| Pneumonia | 31 (1%) | 1,003 (<1%) | 740 (<1%) | <0.001 | |||||
| Obstetric Diagnoses | No. (% Column) | ||||||||
| Hypertensive Disorder of Pregnancy | |||||||||
| Gestational Hypertension‡ | 270 (7%) | 11,042 (4%) | 44,080 (4%) | <0.001 | |||||
| Preeclampsia‡ | 443 (11%) | 13,168 (5%) | 39,911 (3%) | <0.001 | |||||
| Eclampsia‡ | <10 (<1%) | 482 (<1%) | 1,044 (<1%) | <0.001 | |||||
| Gestational Diabetes | 289 (7%) | 7,714 (3%) | 7,998 (1%) | <0.001 | |||||
| Preterm Delivery | 753 (19%) | 35,394 (14%) | 76,413 (6%) | <0.001 | |||||
| Stillbirth | <10 (<1%) | <10 (<1%) | <10 (<1%) | 0.011 | |||||
| Cesarean Delivery | 2,059 (51%) | 105,144 (41%) | 435,066 (37%) | <0.001 | |||||
Discharge diagnoses from the index admission for delivery
COPD = Chronic Obstructive Pulmonary Disease; ICH = Intracerebral Hemorrhage; TIA = Transient Ischemic Attack; NS = non-significant
Some women carried more than one HDP diagnosis (e.g. gestational hypertension + preeclampsia)
Kaplan-Meier curves showing percent survival without readmission over the 3 years of follow up are shown in Figure 1. Overall, only 32.7% of all first readmissions occurred within the first year postpartum and less than 3% occurred in the immediate 42-day postpartum period (Figure 2). This was also true for CV readmissions, where only 35.7% of first CV readmissions occurred within the first year following delivery.
Figure 1.
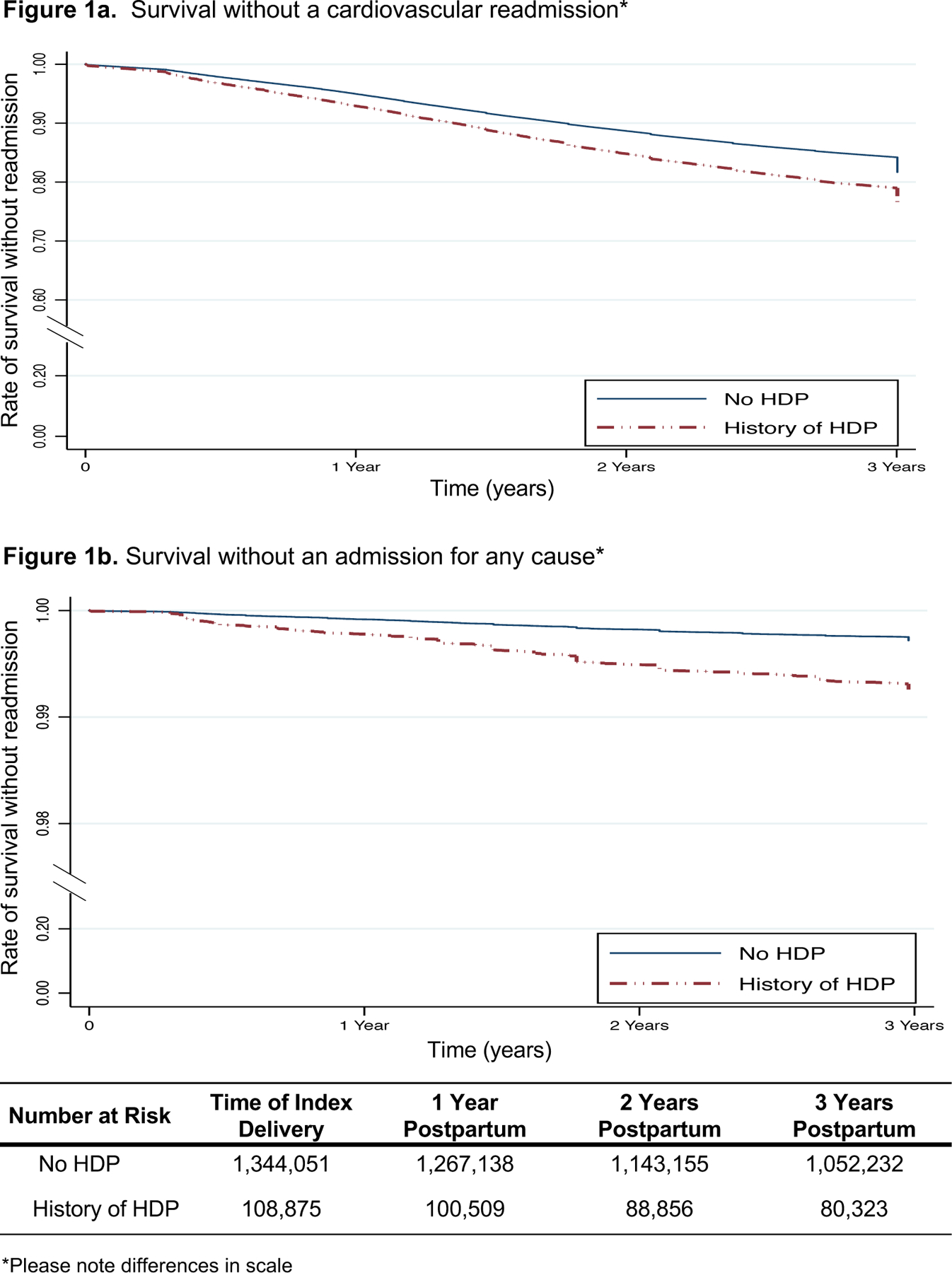
Kaplan-Meier curves showing percent survival without a first readmission over 3 years of follow up
Figure 2.
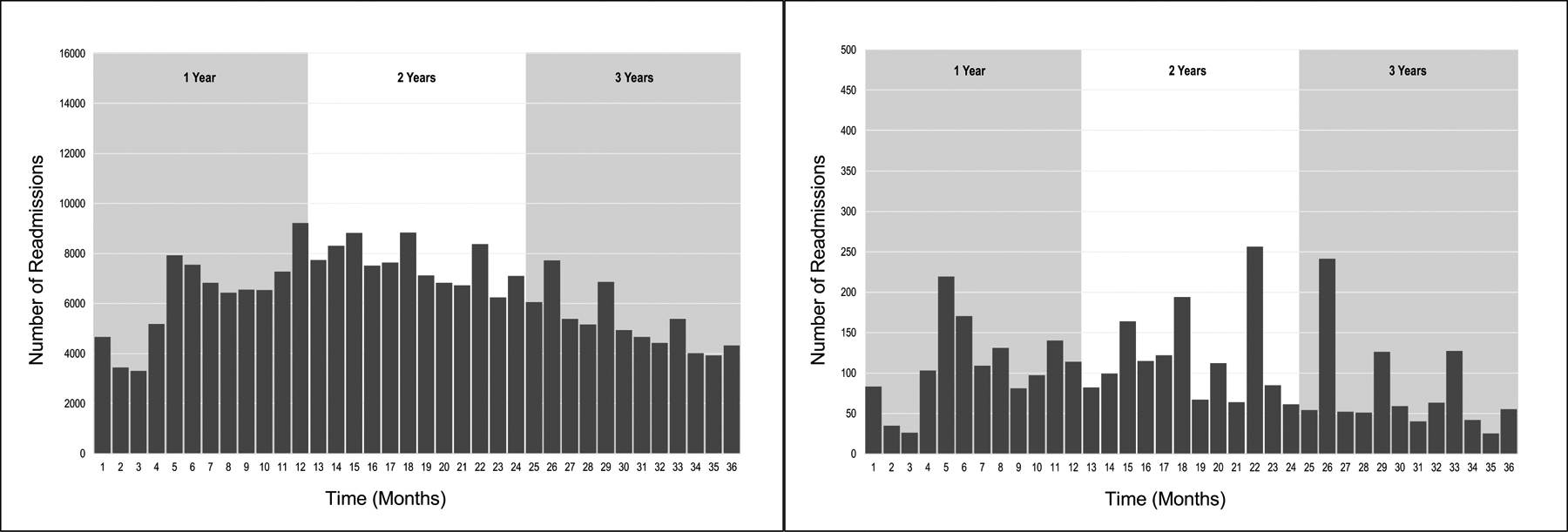
Time to first readmission following index delivery.
Figure 2a. Time to first readmission for any cause
*Dotted line represents readmissions within the first 42 days
Figure 2b. Time to first cardiovascular readmission – defined as acute myocardial infarction, stroke, or heart failure
*Dotted line represents readmissions within the first 42 days
Heart failure was the most common reason for CV readmission accounting for 78.6% of all CV readmissions and 84.4% of CV readmissions in women with HDP. A breakdown of CV event type is shown in Supplemental Table 2. African American women made up 57% of the CV readmissions for an event rate of 6.8 CV readmissions per 1000 pregnancies in AA women compared with an event rate of 1.7 and 1.0 CV readmissions per 1000 pregnancies for white and Hispanic women, respectively (p<0.001 overall). Of the event types, AA women made up 62% of all heart failure readmissions (1,986 of 3,188; p<0.001 overall) and white women made up 52% of acute MI readmissions (205 of 394; p<0.001 overall).
The results for the logistic regression model are shown in Table 3. In the unadjusted model, HDP was a significant predictor of CV readmission with an odds ratio (OR) of 2.59 (95% confidence interval [CI] 2.39 – 2.81; p <0.001). This relationship was only slightly attenuated in the fully adjusted model (OR 2.41, 95% CI 2.08 – 2.80; p <0.001). HDP was also found to be a significant predictor of non-CV readmission (OR 1.11, 95% CI 1.09 – 1.14; p <0.001) and for any readmission (OR 1.13, 95% CI 1.10 – 1.15; p <0.001). Significant predictors for CV readmission in the full multivariate model are shown in Figure 3. Heart failure was the strongest predictor for CV readmission (OR 28.75; 95% CI 23.87 – 34.64). Young age (<18 years) and asthma were associated with reduced risk of CV readmission. In the fully adjusted multivariable model, AA women had the highest risk for CV readmission (OR 3.60; 95% CI: 3.32 – 3.90) and Hispanic women had the lowest risk (OR 0.59; 95% CI 0.51 – 0.68) when compared with white women after adjustment for HDP (Figure 3).
Table 3.
Risk of readmission for women with a pregnancy complicated by HDP compared with women without HDP
| Outcome | Unadjusted OR (95% CI) |
p-value | Covariate Adjusted OR (95% CI) |
p-value |
|---|---|---|---|---|
| CV Readmission | 2.59 (2.39 – 2.81) | <0.001 | 2.41 (2.08 – 2.80) | <0.001 |
| Non-CV Readmission | 1.36 (1.34 – 1.38) | <0.001 | 1.11 (1.09 – 1.14) | <0.001 |
| Any Readmission | 1.39 (1.37 – 1.41) | <0.001 | 1.13 (1.10 – 1.15) | <0.001 |
Covariates in the multivariate logistic regression model: Age, Race/Ethnicity, Preterm Delivery, Cesarean Delivery, Transfusion, Anemia, Thrombocytopenia, Gestational Diabetes, Acute Renal Failure, Tobacco, Alcohol/Drug Abuse, Chronic Hypertension, Coronary Artery Disease, Hyperlipidemia, Heart Failure, Diabetes, Chronic Kidney Disease, Obesity, Chronic Obstructive Pulmonary Disease, Asthma, Depression, Autoimmune Disorder, Payer.
CV = Cardiovascular; OR = Odds Ratio; CI = Confidence Interval
Figure 3.
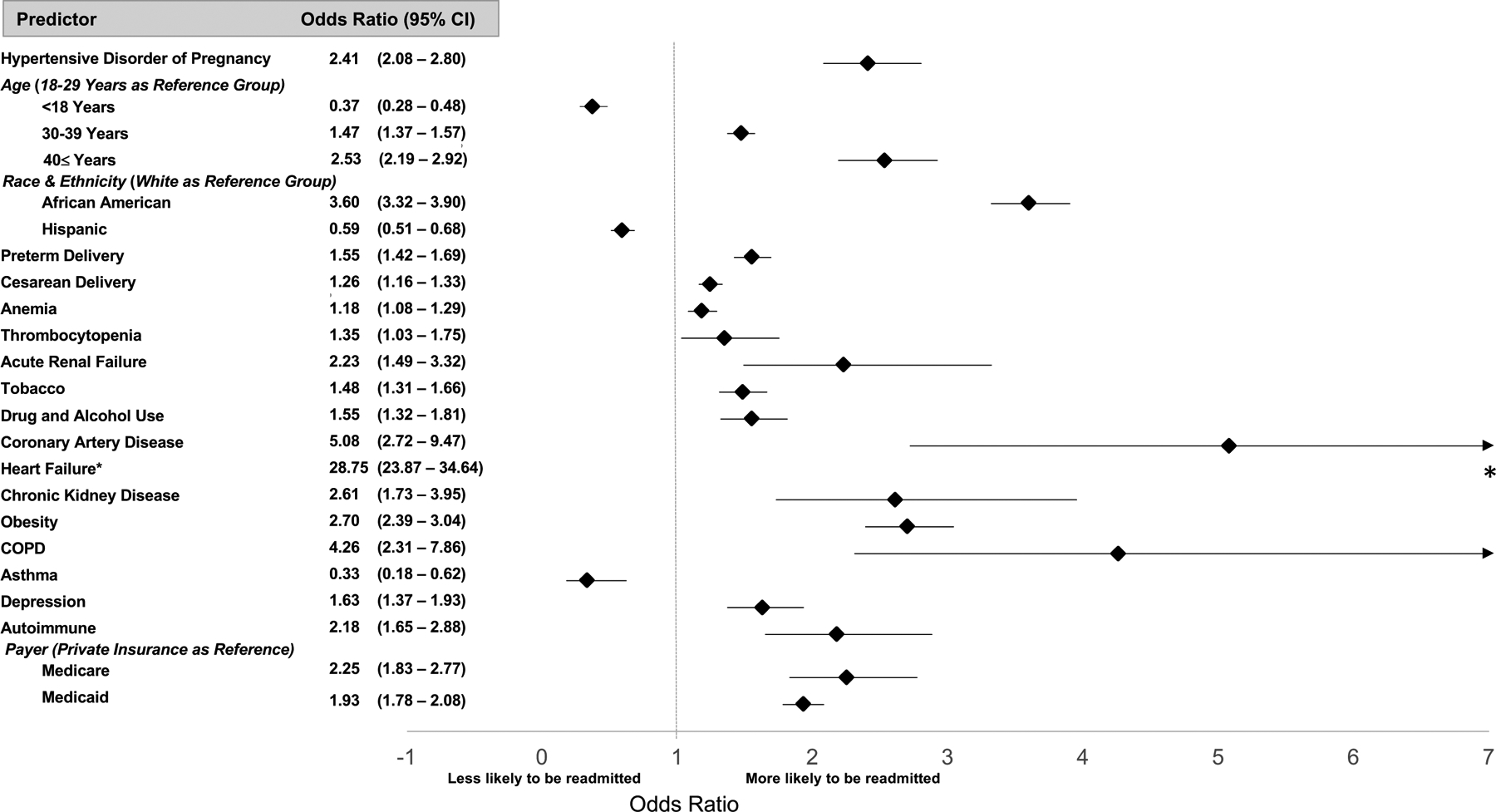
Risk of cardiovascular readmission within 3 years of delivery for individual predictors.
All ORs presented were calculated in the full multivariate model that included interaction terms. Reference group values are not illustrated. Only predictors that were statistically significant are illustrated.
Covariates included in the model that did not reach statistical significance (not illustrated): Other Race/Ethnicity, Transfusion, Gestational DM, Chronic Hypertension, Diabetes
*Odds ratio value was too large for current scale. CI = Confidence Interval
Significant interactions were found between race/ethnicity and HDP (p<0.001) and obesity and HDP (p<0.001). The risk of CV readmission for HDP among white women was 2.96 (95% CI 2.57 – 3.41) compared with 1.74 (95% CI 1.55 – 1.96) in AA women, and 2.41 (95% CI 1.65 – 3.44) among Hispanic women. The risk of CV readmission estimated for HDP among obese women was 1.25 (95% CI 1.01 – 1.55) in comparison with 2.55 (95% CI 2.33 – 2.79) among non-obese women.
DISCUSSION
In this study of over 1.4 million diverse women, those who experienced a pregnancy complicated by HDP had twice the risk of CV readmission within 3 years of delivery compared with women without a history of HDP. Most readmissions occurred after the first year postpartum, suggesting observed CV events were unrelated to direct complications from pregnancy. There were significant racial/ethnic differences in the patterns and risk of CV readmission, such that AA women had higher rates of heart failure and were at 3-fold greater risk for CV readmission compared with white women after adjustment for HDP. Pregnancy is an ideal time to risk stratify women because 4 out of 5 US women will have at least one pregnancy in her lifetime.21 HDP complicates between 10–15% of pregnancies,5,10 and with almost 4 million births in the US each year,22 hundreds of thousands of mothers could be risk stratified without further cost or testing. By recognizing HDP as a risk factor for short and long-term CV disease, women can be educated about risk, lifestyle modification, and surveillance with more aggressive risk factor management postpartum and beyond.
Our findings suggest higher short-term risk for CV events following a pregnancy complicated by HDP. Similar findings were reported by Black, et al.23 who used Kaiser Permanente data and found women free of preexisting HTN or prehypertension who experienced HDP had twice the risk for developing HTN within 1 year of delivery (relative risk 2.33; 95% CI 1.94 – 2.80). A recent study used a statewide linked database to investigate short-term CV outcomes over 5 years in women free of comorbidities after a pregnancy complicated by a placental syndrome (preeclampsia, eclampsia, gestational HTN, placental abruption, and placental infarction).17 Here, women with placental syndromes had increased risk of CV events (HR 1.19; 95% CI 1.07 – 1.32) which compounded when placental syndromes occurred with preterm birth and/or small for gestational age neonate (HR 1.45; 95% CI 1.24 – 1.71), likely signaling more severe vascular dysfunction.17 Unlike our study, only healthy women were included in the previous work. However, even those very low-risk women demonstrated increased risk of a CV event after a pregnancy complicated by HDP. Additionally, we found significant racial/ethnic differences in the risk and type of CV readmissions, such that AA women were at greater risk for CV events compared with white women. Racial differences in hypertensive disorders, both during and outside of pregnancy, have been observed by prior investigators,24,25 but associations between race and CV readmission are not well elucidated.
Large population studies have shown increased long-term risk for CV disease in women with HDP. A 2001 study using Norwegian medical registries found women with preeclampsia had a 20% higher risk of CV death over 25 years compared with women without preeclampsia.5 In a meta-analysis, preeclampsia was associated with a relative risk of 2.16 (95% CI 1.86 – 2.52) for ischemic heart disease over 12 years of mean follow up and a relative risk of 3.70 (95% CI 2.70 – 5.05) for HTN over 14 years of mean follow up.26 More recently, investigators used 50 years of follow up data in California and found early-onset preeclampsia (before 34 weeks’ gestation), late-onset preeclampsia (after 34 weeks’ gestation), and small for gestational age delivery significantly predicted premature CV death in women (HR 3.6, 95% CI: 1.04 – 12.19; HR 2.0, 95% CI: 1.18 – 3.46; and HR 1.6, 95% CI: 1.02 – 2.42, respectively).10 In that analysis, risk of CV death associated with paired pregnancy complications was highest in women with preterm delivery plus preexisting HTN (HR 7.1; 95% CI: 3.49 – 14.55), preeclampsia plus preexisting HTN (HR 5.6; 95% CI: 2.09 – 15.18), and gestational HTN plus preterm delivery (HR 5.0; 95% CI: 2.64 – 9.60)10 – illustrating how multiple complications in a single pregnancy likely reflects more severe vascular dysfunction and compounded risk for the mother. These findings and the results of our study demonstrate increased CV risk in women with HDP beginning soon after delivery and persisting decades later. However, more work is needed to understand the mechanisms underlying HDP and how it relates to future CV disease, including investigation of risk modification in women with HDP and how it impacts CV risk.
There are important limitations to any study utilizing administrative data. ICD-9 CM codes have variable diagnostic accuracy, but have been found to be sufficient for population research.27 Reliably determining parity was not possible using the current database and future efforts should seek to collect this information. In addition, we did not have access to the participants’ obstetrical histories, specifically whether a previous pregnancy was complicated by HDP. To avoid including women with chronic HTN who were misclassified as HDP, we excluded women with individual diagnostic codes for both chronic HTN and HDP from the exposure group. We felt this was the more conservative approach, as chronic HTN is estimated to effect only about 2% of pregnancies10 but is independently associated with CV events.10,20 A sensitivity analysis excluding all women with chronic HTN from the entire cohort was performed and yielded similar results (CV readmission OR 2.44, 95% CI 2.11 – 2.83, p<0.001; non-CV readmission OR 1.11, 95% CI 1.09 – 1.14, p<0.001; any readmission OR 1.13, 95% CI 1.10 – 1.15, p<0.001). Women with pre-existing cardiac conditions, such as heart failure and coronary artery disease, were included in these analyses and could have driven some of the observed CV risk. However, rates for preexisting cardiac conditions were overall very low (<1% each for heart failure and coronary artery disease) and likely had a limited effect on the observed associations. Only women with a diagnosis of HDP at the time of the index delivery were included in our exposure group, which may have resulted in a smaller HDP sample size because new cases of HDP diagnosed postpartum or in subsequent pregnancies (new or recurrent) were not included. This might account for the lower HDP rate in our study (7% of all deliveries) compared with prior studies showing rates of 10–15%.10 We could not evaluate recurrent HDP cases in our analysis, although women with HDP have a 9–14% risk of recurrent HDP during subsequent pregnancies28 and recurrent HDP may be associated with higher CV risk.29 Our data are limited to in-hospital deliveries and events only. We did not have access to socioeconomic information such as household income or education level, and so a proxy measure of insurer/payer was used. Due to the large sample size, there were many statistically significant differences in clinical characteristics that may not be clinically significant. Some, including anemia, obesity, diabetes, COPD/asthma, and depression have previously been associated with CV risk. However, elaboration of their role in HDP-associated CV risk was beyond the scope of this analysis, and targeted investigation of potential interactive mechanisms is warranted.
CONCLUSION
In this diverse sample, women with HDP had twice the risk of short-term CV readmission within 3 years of delivery compared with women without HDP, demonstrating that increased CV risk associated with HDP appears soon after pregnancy and persists for decades with higher risk in AA women. More work is needed to explore the types and mechanisms of HDP-associated CV events for potential preventive strategies.
Supplementary Material
KEY POINTS.
What is already known about this subject?
Preeclampsia and gestational hypertension are known cardiovascular risk factors for women, but little is known about how soon after delivery these women are at risk for cardiovascular events.
What does this study add?
Our study used hospital admission data to identify women with singleton deliveries complicated by a hypertensive disorder of pregnancy (HDP) and followed them for CV readmissions within 3 years postpartum. We found women with HDP had over twice the risk of CV readmission (OR 2.41; 95% CI 2.08–2.80) within 3 years of delivery compared with women without HDP.
How might this impact clinical practice?
Women with pregnancies complicated by HDP can be risk stratified, educated, and followed more closely by healthcare providers for CV risk factor management while ongoing efforts continue to learn more about the timing, pathophysiology, and types of CV events these women experience.
FUNDING SOURCES
Dr. Jarvie was supported by a T32 teaching grant [grant number 5T32HL007822].
Dr. Metz is supported by the National Institute on Child Health and Human Development under award number 5K12HD001271-18. The content is solely the responsibility of the authors and does not necessarily represent the official view of the National Institute of Health.
Dr. Kao is supported by the Jacqueline’s Research fund from the Jacqueline Marie Leaffer Foundation at the University of Colorado Center for Women’s Health Research and by NIH grant 1K08HL125725.
Footnotes
The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article (if accepted) to be published in HEART editions and any other BMJPGL products to exploit all subsidiary rights.
DISCLOSURES
Jarvie – None; Metz – None; Davis – None; Ehrig – None; Kao – None
REFERENCES
- 1.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart Disease and Stroke Statistics - 2016 Update: A Report From the American Heart Association. Circulation. 2015;133:e38–e360. [DOI] [PubMed] [Google Scholar]
- 2.Ridker PM, Buring JE, Rifai N, Cook NR. Development and Validation of Improved Algorithms for the Assessment of Global Cardiovascular Risk in Women: The Reynolds Risk Score. JAMA. 2007;297(6):611–619. [DOI] [PubMed] [Google Scholar]
- 3.Michos ED, Vasamreddy CR, Becker DM, et al. Women With A Low Framingham Risk Score And A Family History of Premature Coronary Heart Disease Have a High Prevalence of Subclinical Coronary Atherosclerosis. Am Heart J. 2005;150(6):1276–1281. [DOI] [PubMed] [Google Scholar]
- 4.Defilippis AP, Young R, Carrubba CJ, et al. An Analysis of Calibration and Discrimination Among Multiple Cardiovascular Risk Scores in a Modern Multiethnic Cohort. Ann Intern Med. 2015;162(4):266–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Irgens HU, Reisaeter L, Irgens LM, Lie RT. Long Term Mortality of Mothers and Fathers After Pre-Eclampsia: Populatio Based Cohort Study. BMJ. 2001;323:1213–1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith GCS, Pell JP, Walsh D. Pregnancy Complications and Maternal Risk of Ischaemic Heart Disease: A Retrospective Cohort Study of 129 290 Births. Lancet. 2001;357(9273):2002–2006. [DOI] [PubMed] [Google Scholar]
- 7.Skjaerven R, Wilcox AJ, Klungsoyr K, et al. Cardiovascular Mortality After Pre-eclampsia in One Child Mothers: Prospective, Population Based Cohort Study. BMJ. 2012;345:e7677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Executive Writing Committee, Mosca Lori, Benjamin EJ, et al. Effectiveness-Based Guidelines for the Prevention of Cardiovascular Disease in Women 2011 Update: A Guideline From the American Heart Association. Circulation. 2011;123:1243–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.American College of Obstetricians and Gynecologists Task Force on Hypertension in Pregnancy. Hypertension in Pregnancy: Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstetr Gynecol. 2013;122(5):1122–1131. [DOI] [PubMed] [Google Scholar]
- 10.Cirillo PM, Cohn BA. Pregnancy Complications and Cardiovascular Disease Death: 50-Year Follow-Up of the Child Health and Development Studies Pregnancy Cohort. Circulation. 2015;132(13):1234–1242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sattar N. Do Pregnancy Complications and CVD Share Common Antecedents? Atheroscler Suppl. 2004;5(2):3–7. [DOI] [PubMed] [Google Scholar]
- 12.Savvidou MD, Hingorani AD, Tsikas D, Frolich JC, Vallance P, Niolaides KH. Endothelial Dysfunction and Raised Plasma Concentrations of Asymmetric Dimethylarginine in Pregnant Women Who Subsequently Develop Pre-Eclampsia. Lancet. 2003;361(9368):1511–1517. [DOI] [PubMed] [Google Scholar]
- 13.Paradisi G, Biaggi A, Savone R, et al. Cardiovascular Risk Factors in Healthy Women With Previous Gestational Hypertension. J Clin Endocrinol Metab. 2006;91(4):1233–1238. [DOI] [PubMed] [Google Scholar]
- 14.Magnussen EB, Vatten LJ, Lund-Nilsen TI, Salvesen KA, Smith GD, Romundstad PR. Prepregnancy Cardiovascular Risk Factors as Predictors of Pre-eclampsia: Population Based Cohort Study. BMJ. 2007;335:978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Magnussen EB, Vatten LJ, Smith GD, Romundstad PR. Hypertensive Disorders in Pregnancy and Subsequently Measured Cardiovascular Risk Factors. Obstetr Gynecol. 2009;114(5):961–970. [DOI] [PubMed] [Google Scholar]
- 16.Berends AL, de Groot CJM, Sijbrands EJ, et al. Shared Constitutional Risks for Maternal Vascular-Related Pregnancy Complications and Future Cardiovascular Disease. Hypertension. 2008;51(4):1034–1041. [DOI] [PubMed] [Google Scholar]
- 17.Cain MA, Salemi JL, Tanner JP, Kirby RS, Salihu HM, Louis JM. Pregnancy As a Window To Future Health: Maternal Placental Syndromes and Short-Term Cardiovascular Outcomes. Am J Obstetr Gynecol. 2016;215:484.e481–484.e414. [DOI] [PubMed] [Google Scholar]
- 18.Duckitt K, Harrington D. Risk Factors for Pre-eclampsia at Antenatal Booking: Systematic Review of Controlled Studies. BMJ. 2005;330:565–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Skupski DW, Nelson S, Kowalik A, et al. Multiple Gestations From In Vitro Fertilzation: Successful Implantation Alone Is Not Associated With Subsequent Preeclampsia. Am J Obstetr Gynecol. 1996;175(4):1029–1032. [DOI] [PubMed] [Google Scholar]
- 20.Stokes JI, Kannel WB, Wolf PA, D’Agnostino RB, Cupples LA. Blood Pressure as a Risk Factor for Cardiovascular Disease: The Framingham Study - 30 Years of Follow-Up. Hypertension. 1989;13(5):I-13–I-18. [DOI] [PubMed] [Google Scholar]
- 21.Martinez G, Daniels K, Chandra A, Division of Vital Statistics Fertility of Men and Women Aged 15–44 Years in the United States: National Survey of Family Growth, 2006–2010. Vol 51 Hyattsville, MD: National Center for Health Statistics; 2012: http://www.cdc.gov/nchs/data/nhsr/nhsr051.pdf. [PubMed] [Google Scholar]
- 22.Hamilton BE, Martin JA, Osterman MJK, Curtin SC, Matthew TJ, Division of Vital Statistics. Births: Final Data for 2014. Nat Vital Stat Rep. 2015;64(12):1–64. Accessed December 23, 2015. [PubMed] [Google Scholar]
- 23.Black MH, Zhou H, Sacks DA, et al. Hypertensive Disorders First Identified in Pregnancy Increase Risk For Incident Prehypertension and Hypertension in the Year After Delivery. J Hypertens. 2016;34(4):728–735. [DOI] [PubMed] [Google Scholar]
- 24.Ashaye MO, Giles WH. Hypertension in Blacks: A Literature Review. Ethn Dis. 2003;13(4):456–462. [PubMed] [Google Scholar]
- 25.Tanaka M, Jaamaa G, Kaiser M, et al. Racial Disparity in Hypertensive Disorders of Pregnancy in New York State: A 10-Year Longitudinal Population-Based Study. Am J Public Health. 2007;97(1):163–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bellamy L, Casas J-P, Hingorani AD, Williams DJ. Pre-Eclampsia and Risk of Cardiovascular Disease and Cancer in Later Life: Systematic Review and Meta-Analysis BMJl. 2007:974–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Burns EM, Rigby E, Mamidanna R, et al. Systematic Review of Discharge Coding Accuracy. J Public Health. 2012;34(1):138–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van Oostwaard MF, Langenveld J, Schuit E, et al. Recurrence of Hypertensive Disorders of Pregnancy: An Individual Patient Data Metaanalysis. Am J Obstetr Gynecol. 2015;212:624.e621–624.e617. [DOI] [PubMed] [Google Scholar]
- 29.Auger N, Fraser WD, Schnitzer M, Leduc L, Healy-Profitos J, Paradis G. Recurrent Pre-Eclampsia and Subsequent Cardiovascular Risk. Heart. 2017;103(3):235–243. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


