Significance Statement
Inclusion of injectable medications into an expanded ESKD payment bundle in 2011 led to concerns that dialysis facilities facing higher costs might close, disrupting the delivery of and access to care. The authors analyzed US Renal Data System registry data to compare facility closures before versus after the payment reform and examined whether patient-, facility-, and geography-related factors influenced closures. Closures affected ≤1.1% of dialysis facilities and ≤2221 patients in a given year. The relative likelihood of experiencing a closure decreased by 37% immediately after enactment of the payment bundle and by an additional 6% per year thereafter, indicating that the payment reform did not increase the risk of closures. However, closure risk increased slightly following payment reform for some high-risk populations, whereas it decreased in others.
Keywords: Chronic dialysis, Economic impact, Epidemiology and outcomes, United States Renal Data System, Ethnic minority
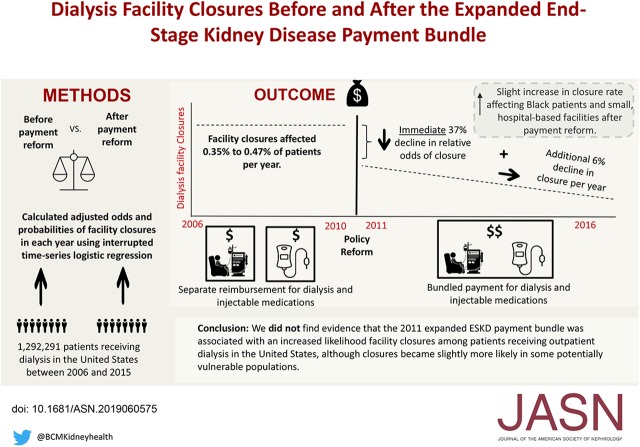
Visual Abstract
Abstract
Background
In 2011, inclusion of injectable medications into an expanded ESKD payment bundle prompted concerns that dialysis facilities facing higher costs might close, disrupting care delivery and access to care. Whether this policy change influenced dialysis facility closures is unknown.
Methods
To examine whether facility closures increased after 2011 and whether factors influencing closures changed, we analyzed US Renal Data System registry data to identify all patients receiving in-center hemodialysis from 2006 through 2015 and to track dialysis facility closures. We used interrupted time series logistic regression models and estimated marginal effects to examine immediate and longer-term changes in the likelihood of being affected by facility closures following payment reform. We also examined whether associations between selected predictors of closures indicating populations at “high risk” of closure (patient characteristics, facility characteristics, and geography-related characteristics) and closures changed after payment reform.
Results
Dialysis facility closures were uncommon over the study period. In adjusted models, the relative odds of experiencing a closure declined by 37% (odds ratio [OR], 0.63; 95% confidence interval [95% CI], 0.59 to 0.67) immediately after payment reform and declined by an additional 6% (OR, 0.94; 95% CI, 0.91 to 0.97) annually thereafter, corresponding to a 0.3% lower absolute probability of closure in 2015 in association with payment reform. Patients who were black and who dialyzed at small, hospital-based facilities experienced slight increases in closures following payment reform, whereas Hispanic and Medicare/Medicaid dual-eligible patients experienced slight decreases in closures.
Conclusions
Expansion of the ESKD payment bundle was not associated with increased closure of dialysis facilities, although the likelihood of closures changed slightly for some higher-risk populations.
Closures of health care facilities may limit access to care among vulnerable patient populations and lead to worse health outcomes.1 Patients with ESKD requiring dialysis are medically complex and suffer from multiple comorbidities. They are more likely to be socioeconomically disadvantaged, and they are more likely to be members of racially and ethnically vulnerable populations.2–4 Hemodialysis is typically delivered three to four times per week in a freestanding dialysis unit where, in addition to dialysis treatments, patients commonly rely on a broad range of multidisciplinary services provided by physicians, nurses, social workers, and dieticians. Patients in the general population may be at risk for negative health outcomes following the transition of care from one setting to another,5,6 and the need for frequent and highly supervised care may put patients on dialysis at risk for complications in the setting of care disruptions and transitions. For example, the temporary closings of dialysis facilities in the setting of natural disasters are associated with worse health outcomes, and facility closures in rural areas may contribute to limited access to dialysis care.7–11
In 2011, in an effort to control Medicare costs while maintaining the quality of care, the Centers for Medicare and Medicaid Services (CMS) reformed reimbursement for dialysis care by bundling injectable medications (which had previously been reimbursed on a fee-for-service basis) together with payment for the dialysis procedure and soon after, implementing a national pay-for-performance program focused on dialysis care. These efforts—referred to as the expanded ESKD payment bundle and the Quality Incentive Program (QIP)—led to concern that costs in excess of reimbursement would force some dialysis facilities to close, especially smaller facilities, facilities serving rural communities, and facilities caring for vulnerable populations.6 In an effort to address these concerns, the CMS instituted payment adjustments to low-volume and rural dialysis units, and it included mechanisms of risk adjustment when evaluating facility performance and when determining payments.12 However, a report published by the Government Accountability Office (GAO) in 2013 suggested that these safeguards may be inadequate.13
It is unknown whether concerns that federal reimbursement policies would increase dialysis facility closures have materialized. Annual reports from the Medicare Payment and Advisory Commission (MedPAC) suggest that dialysis facility closures are relatively rare.14 In this study, we examine whether Medicare’s expanded payment bundle led to an increase in dialysis facility closures. We also examine whether the influence of specific patient, geographic, and dialysis facility characteristics on closures changed following the 2011 payment reform.
Methods
Data Sources and Patient Selection
We used data from the US Renal Data System (USRDS) to identify all patients receiving in-center hemodialysis in the United States between 2006 and 2015 and dialysis facility closures. The USRDS includes information about nearly every United States patient who develops ESKD, including where the patient received outpatient dialysis at each point in time. We ascertained information about patient demographics and medical comorbidities from the CMS Medical Evidence Form (CMS-2728), which nephrologists and case managers complete at the onset of ESKD. Information about dialysis facilities came from annual facility surveys, and health insurance status came from Medicare Enrollment and claims data. Information about dialysis modality came from a combination of Medicare claims, the CMS-2728 form, and information collected by ESKD Networks. We used the zip codes where patients reside to merge patients and dialysis facilities to US Census and Rural Urban Commuting Area data2 to identify socioeconomics and population density, respectively.
We collected information about patients receiving dialysis on the first day of each calendar year and patients who newly initiated ESKD treatment with dialysis in each calendar year, yielding ten cohorts corresponding to the 10 years of follow-up. We updated information about patient health insurance, dialysis modality, age, time on dialysis, and dialysis facilities in each calendar year, and then, we aggregated the ten calendar year cohorts. Patients who received dialysis over multiple calendar years could appear in the aggregated study cohort multiple times.
Identifying Patients Affected by Facility Closures
To identify dialysis facility closures, we ascertained information about the facilities where patients received hemodialysis throughout the study period. We defined a facility closure as occurring when all patients left a facility and no patients received dialysis at the facility for at least 6 consecutive months. When examining facility closures, we observed that facilities affiliated with transplant centers and some small dialysis facilities had intermittent periods where no patients received dialysis for >6 months, despite consistently submitting annual facility surveys. This suggests that small facilities and transplant facilities may experience periods when they remain open for dialysis referrals but do not have anyone receiving care at that time. In contrast, identified closures of other dialysis facilities more commonly corresponded with the absence of a facility survey in the subsequent year. Consequently, we excluded transplant facilities and those with fewer than five patients from all analyses. Additionally, we did not consider a facility to have closed if a majority of patients at the facility transitioned to a single new dialysis facility that was located at the same address because this scenario more likely represents a merger, acquisition, or paired closure and opening.
For each identified dialysis facility closure, we assigned a “closure date” on the basis of the day when the last patient received dialysis at that facility. We then identified all patients receiving dialysis at that facility in the 6 months prior to the closure date as being affected by the facility closure. We chose 6 months because that was when we observed that patients began leaving closed facilities at increasing frequency. Finally, we assigned an indicator to each patient-year record in our cohort to indicate whether the patient was affected by a closure in a given calendar year. Within this framework, a given facility closure could only affect a patient in 1 year (Supplemental Material).
Study Outcome, Exposure, and Covariates
The primary study outcome was whether a patient was affected by a dialysis facility closure in a given calendar year. The primary study exposure was whether a patient received dialysis before versus after enactment of the expanded ESKD payment bundle. In additional analyses, we examined whether selected predictors of dialysis facility closures indicating populations at a “high risk” of closure changed after payment reform. In these additional analyses, the exposures were the following predictors of facility closures among patients and dialysis facilities in the years after 2010: black race, Hispanic ethnicity, dual Medicare/Medicaid eligible, private group health insurance, small dialysis facility (<25 and 25–50 patients), hospital-based facility, and rural/small town facilities. In all analyses, covariates of interest included patient, dialysis facility, and geographic characteristics listed in Table 1. We used comorbidities reported at the onset of dialysis in the CMS-2728 form to assign a comorbidity score that we derived from a Charlson Comorbidity Index adapted for use in patients with ESKD.15 We include this score as a categorical value in regression models along with time since starting dialysis (“vintage”), which we updated annually for each patient (Supplemental Material).
Table 1.
Baseline characteristics
| Characteristics | Before PPS | After PPS | ||
|---|---|---|---|---|
| Facility Closed | Facility Did Not Close | Facility Closed | Facility Did Not Close | |
| Patient demographic and socioeconomic characteristics | ||||
| Age group, yr, %a | ||||
| <50 | 20.5 | 20.5 | 18.5 | 19.3 |
| 50–64 | 34 | 33.3 | 34.2 | 34.2 |
| 65–74 | 22.2 | 23.2 | 23.8 | 24.3 |
| 75+ | 23.2 | 23.1 | 23.4 | 22.2 |
| Women, % | 45 | 45.2 | 44.1 | 43.9 |
| Race, % | ||||
| White | 59.8 | 59 | 56.7 | 59.2 |
| Black | 36.2 | 34.9 | 38.4 | 34.4 |
| American Indian or Alaska Native | 1 | 1.3 | 1 | 1.1 |
| Native Hawaiian or Pacific Islander | 0.4 | 0.9 | 1 | 1.1 |
| Asian or other | 2.5 | 3.9 | 3 | 4.2 |
| Documented Hispanic, %b | 12.2 | 14.1 | 9.8 | 15.4 |
| Dual eligible, %a,c | 37.1 | 31.2 | 36.8 | 33.4 |
| Medicare advantage/HMO, %a | 8.5 | 10.5 | 13.1 | 14 |
| Private insurance, %a | 5.2 | 6.4 | 4.1 | 5.4 |
| Poverty rate per 100 residents, mean (SD)a | 19.1 (10.6) | 18.5 (10.6) | 18.8 (10.7) | 18.3 (10.4) |
| Median household income ($1000)a | 47.9 (20.0) | 49.8 (20.2) | 49.2 (20.8) | 50.1 (20.0) |
| Patient health characteristics | ||||
| Comorbidity score, % | ||||
| ≤1 | 53.7 | 52.5 | 52.9 | 56.5 |
| 2–3 | 27.4 | 28 | 30.4 | 27.1 |
| 4–6 | 16.2 | 16.8 | 14.7 | 14.2 |
| ≥7 | 2.7 | 2.7 | 2 | 2.1 |
| Year since dialysis, %a | ||||
| <1c,b | 13 | 22.7 | 9.7 | 19.6 |
| 1–3c,b | 37 | 34.1 | 34.1 | 31 |
| ≥3 | 50 | 43.1 | 56.2 | 49.3 |
| Home dialysis, %a | 6.1 | 8.8 | 9.7 | 10.9 |
| Immobility, % | 4.3 | 4.3 | 4.9 | 4.5 |
| Alcohol or drug use, % | 3 | 2.4 | 2.7 | 2.3 |
| Tobacco use, % | 6.8 | 6.2 | 6.7 | 6.3 |
| Institutionalized, % | 3.7 | 3.8 | 5.8 | 4.9 |
| Facility and geographic characteristics | ||||
| Facility size, %a | ||||
| <25b,c | 18.3 | 3.6 | 22.2 | 3.3 |
| 25–50 | ||||
| 51–99c | 31.4 | 39.6 | 37.9 | 39.4 |
| ≥100b,c | 14.6 | 42.9 | 15 | 44 |
| Nonprofit, %a,b,c | 23.7 | 17.4 | 22.4 | 13.4 |
| Hospital based, %a,b,c | 17.6 | 9.2 | 18.8 | 5.9 |
| Chain facility, %a,b,c | 62.9 | 74.2 | 58.4 | 80 |
| Large dialysis organization, %a,b,c | 54 | 64.1 | 46.6 | 70 |
| Population density, %a | ||||
| Metropolitanc | 77.5 | 85.2 | 81.7 | 85.3 |
| Micropolitanc | 14.6 | 10.3 | 9.7 | 10.1 |
| Small townc | 6.9 | 3.7 | 5.9 | 3.8 |
| Rural areab | 1 | 0.7 | 2.6 | 0.7 |
| County-year unemployment rate, mean (SD)a | 6.9 (3.1) | 7.2 (3.2) | 7.6 (2.2) | 7.6 (2.5) |
PPS, prospective payment system; HMO, health maintenance organization.
Covariate is updated for patients in each calendar year.
Indicates that standardized difference is >10% after the PPS.
Indicates that standardized difference is >10% before the PPS.
Study Design
When describing baseline characteristics in the periods prior to and following enactment of the expanded ESKD payment bundle, we used a 10% standardized difference to identify potentially meaningful differences in characteristics between patients affected by closures and those not affected by closures.16 We assessed for differences prior to and following payment reform.
We used a series of nested interrupted time series logistic regression models to examine whether facility closures changed after enactment of the expanded ESKD payment bundle in 2011. Interrupted time series is a common method used for policy analysis, and it can be conducted using longitudinally collected data at the aggregate level or—as was the case in our study—at the level of the individual patient.17,18 In the interrupted time series model, the odds of being affected by a facility closure were examined as a function of calendar year (represented as a linear numeric variable), a variable indicating receipt of dialysis after 2010, and a variable indicating the number of years since 2010. To understand how different characteristics (e.g., race, ethnicity, health, poverty, geographic location, and facility type) influence facility closures, the nested models sequentially adjusted for the demographic and socioeconomic characteristics, the patient health characteristics, and the facility and geographic characteristics listed in Table 1.
Within the segmented regression model, there are two ways in which payment reform could influence facility closures. First, payment reform could lead to an immediate change in the likelihood of being affected by a closure. This would be identified in the estimated coefficient corresponding to time after 2010. Second, payment reform could lead to a longer-term change in the likelihood of facility closures. A change in the longer-term trend is identified in the estimated coefficient corresponding to the number of years since 2010 (Supplemental Material).
In all analyses, we used generalized estimating equations with an unstructured variance-covariance matrix and cluster-robust SEMs to account for repeated measures within patients.19 We used a P value of 0.05 as a measure of statistical significance. To graphically illustrate trends, we plotted the predicted marginal probabilities of closures over time in the setting of an expanded ESKD payment bundle and in a counterfactual scenario where the policy reform did not happen.
In an additional analysis, we used our fully adjusted regression model to examine whether the odds of closures changed in 2008 when the Medicare Improvements for Patients and Providers Act of 2008 (MIPPA) directed the CMS to enact the expanded ESKD payment bundle. We also examined the sensitivity of findings from the fully adjusted interrupted time series regression model to (1) the use of Medicare claims for comorbidity adjustment, (2) the requirement that facilities close for only 6 months, and (3) more granular adjustment for differences in patient follow-up time.
Changing Influence of High-Risk Factors Associated with Facility Closures
Concerns about dialysis facility closures have primarily focused on specific “high-risk” (and/or vulnerable) patients, facilities, and geographic regions. We examined whether the associations among selected high-risk characteristics and dialysis facility closures changed after enactment of the expanded ESKD payment bundle. High-risk characteristics of interest included black race, Hispanic ethnicity, dual Medicare/Medicaid eligibility, hospital-based facility, smaller facility sizes, and remote location. We also examined the potential protective effect of patients with private group health insurance. We used separate multivariable regression models for each characteristic, and we used linear combinations of coefficients to calculate changes in the estimated odds of being affected by a facility closure associated with each characteristic before versus after payment reform. Because we were not interested in longer-term time trends when examining changing influences of characteristics, we represented calendar year as separate dummy variables in these models. We present estimated differences in relative odds and predicted probabilities (Supplemental Material).
Results
Baseline Characteristics
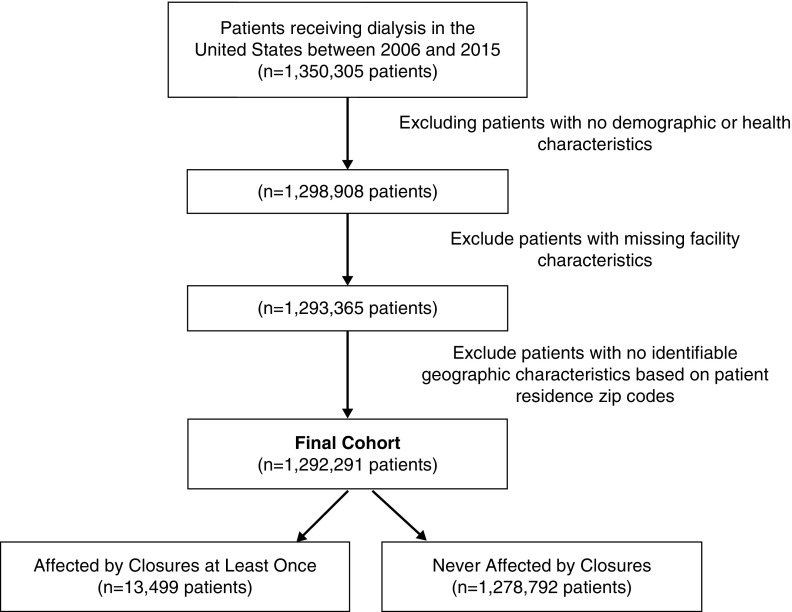
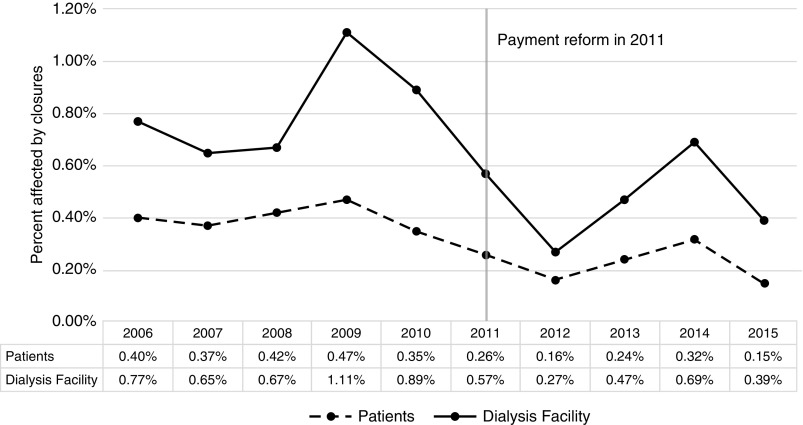
We identified 1,292,291 patients receiving dialysis between 2006 and 2015 at 7080 dialysis facilities (Figure 1). Among selected patient-years, the mean age was 62 years old, 45% were women, 35% were black, 15% were Hispanic, and 32% were dual eligible for Medicare and Medicaid. There were 405 dialysis facility closures over the study period that affected 13,593 patients receiving dialysis. This represented between 0.3% and 1.1% of all facilities and between 0.2% and 0.5% of all patients in a given year, and it is comparable with the magnitude of closure frequencies reported by MedPAC14 (Figure 2).
Figure 1.
Patient selection diagram illustrates selection of 13,499 patients affected by dialysis facility closures and 1,278,792 unnaffected patients.
Figure 2.
Percentages of patients and dialysis facilities affected by closures trends downward slightly over time prior to statistical adjustment.
Prior to the 2011 payment reform, patients who were dual eligible for Medicare/Medicaid, those with longer duration of dialysis (“vintage”), patients at smaller and hospital-based facilities, and those living in small towns and micropolitan areas were more likely to be affected by facility closures. Patients at for-profit facilities, patients at chain-owned facilities, and those living in metropolitan areas were less likely to be affected by facility closures. All of these characteristics continued to be observed more (or less) commonly with facility closures after payment reform except for patients with Medicare/Medicaid and those in micropolitan and small town facilities, who were not more likely to be affected by closures after payment reform. In the period following payment reform, Hispanic patients were less likely to be affected by closures, whereas patients living in rural facilities were more likely to be affected by closures (Table 1).
Regression Results
In an interrupted time series regression model that did not adjust for changes over time in patient, dialysis facility, and geographic characteristics, there was a 38% reduction in the relative odds of facility closures immediately after enactment of the expanded ESKD payment bundle (95% confidence interval [95% CI], −33% to −42%). Each year after 2011, the relative odds of closure declined by an additional 3% (95% CI, −1% to −6%). In models where we sequentially added adjustment for patient demographic and socioeconomic characteristics and patient health characteristics, changes in the odds of facility closures following enactment of the expanded ESKD payment bundle were not different compared with the unadjusted model. In the (“fully adjusted”) model where we also accounted for changes over time in facility and geographic characteristics, the odds of closure declined by 37% (95% CI, −33% to −41%) immediately after the 2011 payment reform, and they declined by an additional 6% (95% CI, −3% to −9%) each year thereafter (Table 2).
Table 2.
Multivariable regression results examining the odds of being affected by facility closures
| Covariates | Time-Related Covariates | + Patient Demographic and Socioeconomic Characteristics | + Patient Health Characteristics | + Facility and Geographic Characteristicsa | ||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Year since 2005 | 1.00 | 0.98 to 1.01 | 1.00 | 0.99 to 1.02 | 0.99 | 0.98 to 1.01 | 1.02 | 1.00 to 1.04 |
| Post-PPSb | 0.62 | 0.58 to 0.67 | 0.62 | 0.58 to 0.67 | 0.62 | 0.58 to 0.67 | 0.63 | 0.59 to 0.67 |
| Year since the PPSb | 0.97 | 0.94 to 0.99 | 0.97 | 0.94 to 0.99 | 0.97 | 0.95 to 0.99 | 0.94 | 0.91 to 0.97 |
| Patient demographic and socioeconomic characteristics | ||||||||
| Age group, yr | ||||||||
| <50 | Reference | Reference | Reference | |||||
| 50–64 | 1.05 | 1.00 to 1.10 | 1.03 | 0.98 to 1.08 | 1.11 | 1.06 to 1.17 | ||
| 65–74 | 1.01 | 0.96 to 1.06 | 0.98 | 0.93 to 1.04 | 1.05 | 1.00 to 1.11 | ||
| 75+ | 1.07 | 1.02 to 1.13 | 1.03 | 0.97 to 1.09 | 1.10 | 1.04 to 1.17 | ||
| Women | 0.96 | 0.93 to 1.00 | 0.97 | 0.94 to 1.01 | 0.97 | 0.93 to 1.00 | ||
| Race | ||||||||
| White | Reference | Reference | Reference | |||||
| Black | 0.93 | 0.90 to 0.97 | 0.89 | 0.85 to 0.93 | 1.11c | 1.07 to 1.16 | ||
| American Indian or Alaska Native | 0.72 | 0.61 to 0.86 | 0.69 | 0.59 to 0.82 | 0.68 | 0.57 to 0.81 | ||
| Native Hawaiian or Pacific Islander | 0.62 | 0.50 to 0.77 | 0.60 | 0.49 to 0.75 | 0.89 | 0.72 to 1.11 | ||
| Asian or other | 0.64 | 0.58 to 0.72 | 0.64 | 0.58 to 0.71 | 0.89 | 0.79 to 0.99 | ||
| Documented Hispanic | 0.68 | 0.64 to 0.72 | 0.66 | 0.62, 0.70 | 0.87 | 0.81 to 0.92 | ||
| Dual eligible | 1.26 | 1.22 to 1.31 | 1.15 | 1.10 to 1.19 | 1.19 | 1.15 to 1.24 | ||
| HMO | 0.86 | 0.81 to 0.91 | 0.90 | 0.85 to 0.95 | 0.97 | 0.91 to 1.03 | ||
| Private insurance | 0.82 | 0.76 to 0.89 | 0.80 | 0.74 to 0.87 | 0.81 | 0.74 to 0.88 | ||
| Poverty rate per 100 residents | 1.00 | 1.00 to 1.00 | 1.00 | 1.00 to 1.00 | 1.01 | 1.01 to 1.02 | ||
| Median household income ($1000) | 1.00 | 1.00 to 1.00 | 1.00 | 1.00 to 1.00 | 1.00 | 1.00 to 1.00 | ||
| Patient health characteristics | ||||||||
| Comorbidity score | ||||||||
| ≤1 | Reference | Reference | ||||||
| 2–3 | 1.04 | 1.00 to 1.08 | 1.01 | 0.97 to 1.05 | ||||
| 4–6 | 0.98 | 0.93 to 1.03 | 0.91 | 0.86 to 0.96 | ||||
| ≥7 | 0.98 | 0.88 to 1.10 | 0.91 | 0.81 to 1.01 | ||||
| Years since dialysis | ||||||||
| <1 | 0.50 | 0.47 to 0.53 | 0.39 | 0.37 to 0.42 | ||||
| 1–3 | Reference | Reference | ||||||
| ≥3 | 1.04 | 1.00 to 1.08 | 1.08 | 1.04 to 1.12 | ||||
| Home dialysis | 0.79 | 0.74 to 0.85 | 0.86 | 0.81 to 0.92 | ||||
| Immobility | 1.03 | 0.94 to 1.13 | 0.93 | 0.85 to 1.02 | ||||
| Alcohol or drug use | 1.13 | 1.02 to 1.25 | 1.16 | 1.04 to 1.29 | ||||
| Tobacco use | 1.00 | 0.93 to 1.07 | 1.00 | 0.93 to 1.07 | ||||
| Institutionalized | 1.11 | 1.01 to 1.21 | 0.98 | 0.89 to 1.07 | ||||
| Facility and geographic characteristics | ||||||||
| Facility size | ||||||||
| <25 | 7.25 | 6.86 to 7.66 | ||||||
| 25–50 | 2.91 | 2.79 to 3.04 | ||||||
| 51–99 | Reference | |||||||
| ≥100 | 0.33 | 0.31 to 0.35 | ||||||
| Nonprofit | 0.70 | 0.66 to 0.75 | ||||||
| Free standing | 0.56 | 0.52 to 0.61 | ||||||
| Chain facility | 0.70 | 0.66 to 0.75 | ||||||
| Large dialysis organization | 0.81 | 0.76 to 0.86 | ||||||
| Population density | ||||||||
| Metropolitan | Reference | |||||||
| Micropolitan | 0.80 | 0.76 to 0.85 | ||||||
| Small town | 0.70 | 0.65 to 0.76 | ||||||
| Rural area | 0.79 | 0.69 to 0.91 | ||||||
| County-year unemployment rate | 0.99 | 0.98 to 1.00 | ||||||
OR, odds ratio; 95% CI, 95% confidence interval; PPS, prospective payment system; HMO, health maintenance organization.
ESKD Network indicator variables are not presented.
Compared with a counterfactual scenario with no payment reform, the OR for closure was 0.59 (95% CI, 0.55 to 0.63) in 2011 (Supplemental Figures 1 and 2).
Adjustment for facility size strongly influenced the estimated coefficient for black race. In a fully adjusted model without facility size, the estimated coefficient for black race was 0.95 (95% CI, 0.91 to 0.99) (Supplemental Material).
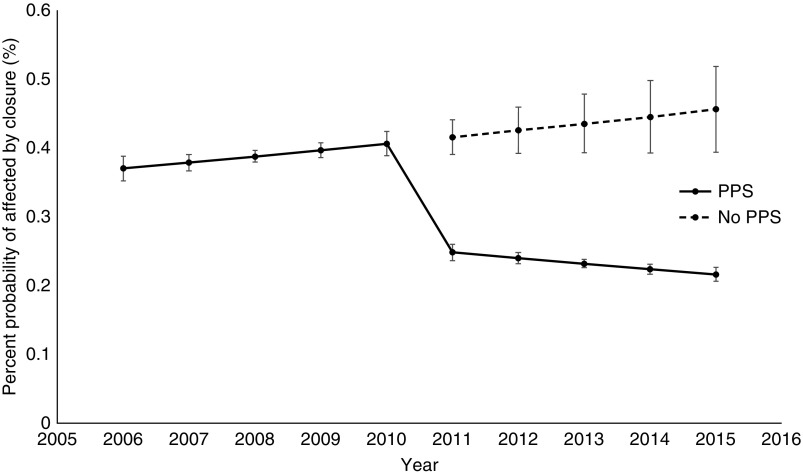
On the basis of the fully adjusted regression results, the predicted probability of facility closures was 0.2% in 2015. If findings from the analysis characterized the causal influence of payment reform on facility closures, the probability of closures would have been 0.5% in the absence of the expanded ESKD payment bundle, representing a 0.3% lower absolute probability of closure in association with the payment reform (Figure 3).
Figure 3.
Predicted probabilities of facilities closures are lower after bundled ESKD payments than before, relative to predicted probabilities of facilitiy closures that would have occurred in absence of bundled ESKD payments. PPS, prospective payment system.
In an additional analysis, we assessed whether changes in dialysis facility closures began in 2008 when the MIPPA directed the CMS to implement an expanded ESKD payment bundle. In a fully adjusted model, the relative odds of facility closures increased by 33% (95% CI, 22% to 45%) in 2008 and did not change over time in 2009 and 2010. The relative odds of facility closures then decreased by 34% (95% CI, −29% to −38%) in 2011, offsetting the increase observed in 2008, and it remained at the lower level after 2010. This indicates that any temporary increase in the likelihood of closures that occurred in 2008 did not persist into the period following implementation of the policy reform.
Findings from the fully adjusted interrupted time series regression model were not sensitive to (1) the use of Medicare claims for comorbidity adjustment, (2) a requirement that facilities close for at least 12 months, and (3) quarterly adjustment for differences in individual patient follow-up time (Supplemental Material).
Analyses of Selected High-Risk Characteristics Associated with Dialysis Facility Closures
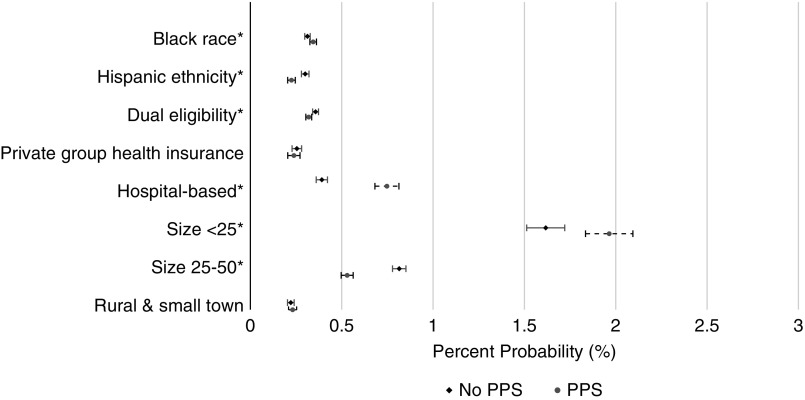
The associations among facility closures and all selected patient demographic, socioeconomic, facility, and geographic characteristics changed slightly following enactment of the expanded ESKD payment bundle. Prior to the payment reform, black race was associated with a 7% (95% CI, 2% to 13%) higher odds of facility closures. After payment reform, black race was associated with an 18% (95% CI, 11% to 25%) higher odds of closures (P value for difference =0.009). Prior to payment reform, Hispanic ethnicity was not significantly associated with facility closures. After payment reform, Hispanic ethnicity was associated with a 27% (95% CI, −34% to −25%) lower relative odds of closure (P value for difference <0.001). Patients who were dual eligible for Medicare/Medicaid were 25% (95% CI, 19% to 31%) more likely to be affected by closures prior to payment reform compared with 12% (95% CI, 6% to 18%) after reform (P value for difference =0.003). Patients at hospital-based facilities had a 40% (95% CI, 28% to 53%) increase in the odds closures prior to payment reform compared with a 2.7-fold increase (odds ratio [OR] 95% CI, 2.5 to 3.0) after reform (P value for difference <0.001). Patients at facilities with <25 patients were at a 6.7-fold (OR 95% CI, 6.2 to 7.1) higher odds of closure prior to reform and 8.2-fold (OR 95% CI, 7.6 to 8.8) higher odds after reform (P value for difference <0.001). In contrast, increased risk of closure among patients at facilities with 25–50 patients became less pronounced after payment reform. Patients in rural and small town facilities were 29% (95% CI, −35% to −23%) less likely to be affected by closures prior to reform, and this did not change following payment reform (P value for difference =0.50). Patients with private insurance were less likely to be affected by closures both before and after payment reform. (Supplemental Table 1)
Despite substantial changes in the relative odds of closure among some selected high-risk and vulnerable populations, associated differences in absolute probabilities of being affected by closures were small. The change in absolute probability of closure only exceeded 0.1% per year among hospital-based facilities (increase of 0.4%) and small facilities (increase of 0.3% for facilities with <25 patients and decrease of 0.3% for those with 25–50 patients) (Figure 4).
Figure 4.
Predicted differences in the absolute probabilities of closure varied by selected patient and facility characteristics. PPS, prospective payment system.
Discussion
Overall, dialysis facility closures were infrequent between 2006 and 2015, and patients receiving dialysis were not more likely to be affected by dialysis facility closures in the initial 5 years following enactment of the expanded ESKD payment bundle in 2011. In fact, the overall likelihood of being affected by a facility closure decreased after the payment reform. These findings suggest that many concerns regarding the potential effects of the expanded ESKD payment bundle on access to maintenance dialysis care among high-cost patient populations did not materialize. However, associations between dialysis facility closures and black race, Hispanic ethnicity, dual Medicare/Medicaid eligibility, and hospital-based and smaller dialysis units changed slightly following enactment of payment reform, suggesting that the risk of being affected by a facility closure changed for some patient populations.
There are several possible explanations for the absence of an overall association between enactment of the expanded ESKD payment bundle and increased dialysis facility closures. First, the MIPPA, which was the federal law requiring that the CMS transition to an expanded ESKD payment bundle, required that payments remain close to budget neutral. Specifically, after accounting for changes in input prices, aggregate per patient payment for dialysis services (including injectable medications) was not supposed to decrease by >1% of the amount on December 31, 2009.20 The relatively small magnitude of this overall decrease in reimbursement combined with continued growth in dialysis markets, ongoing changes in the composition of dialysis providers and suppliers through mergers and acquisitions, and consistent revenues streams from patients with private health insurance may have enabled many high-cost facilities to avoid closures.21–23
Declining use of injectable medications may have also helped high-cost dialysis facilities to continue operating after enactment of the expanded ESKD payment bundle. A goal of combining formerly separately billable injectable medications and the dialysis procedure into a single bundled payment was to encourage more efficient use of expensive injectable medications, such as erythropoietin-stimulating agents (ESAs) or injectable medications, to treat CKD-associated mineral-bone disease.24,25 After injectable medications became a part of the ESKD payment bundle, economic incentives shifted from encouraging more use of these medications to less by using them for fewer patients and also, at a lower dose. At the same time, two clinical trials highlighting safety concerns associated with ESA use led the Food and Drug Administration to revise its black box warning about the use of ESAs in kidney disease.26–28 In the face of changing clinical and economic landscapes, the use of ESAs declined from 95% to 85% between 2010 and 2012, whereas administered ESA doses declined by even more.25,29 Administration of injectable medications to treat CKD-associated mineral-bone disease also declined after enactment of the expanded ESKD payment bundle due to acceptance of higher parathyroid hormone levels among clinicians and possible substitution to oral alternatives.30–32 Lower costs due to declining use of injectable medications may have more than offset payment reductions to some high-cost facilities.
Finally, the 2011 payment reform incorporated several mechanisms to adjust payment for certain patients and facilities expected to incur higher costs.33 The reimbursement policy includes mechanisms of patient mix adjustment, where facilities caring for patients who are expected to incur higher costs are reimbursed at a higher rate. It also includes an outlier payment mechanism, where facilities incurring particularly high costs of care receive additional reimbursement. Finally, additional payment add ons for low-volume dialysis facilities and rural facilities may have offset higher operating costs in these settings. Although each of these mechanisms has faced criticism in how effectively it has “leveled the playing field” among dialysis providers,13,34 their combined effects may have been to prevent some dialysis facilities from closing.
The relative change in risk of closure associated with implementation of the expanded ESKD payment bundle varied for different vulnerable and high-risk patient groups. For example, the risk of being affected by a closure increased among blacks, which may be due to a higher requirement of ESAs and mineral-bone disease medications compared with in nonblack patients. One study found that black patients continued to receive higher doses of ESAs following reimbursement reform.35 Because patient mix adjustment proposed by the CMS does not account for race, these facilities would have potentially experienced an operating loss. In contrast, patients of Hispanic ethnicity and those who were dual eligible for Medicare/Medicaid experienced relative decreases in the risk of being affected by closures on or after the 2011. The finding that closures decreased among patients of Hispanic ethnicity and those who are dual eligible is reassuring when considering findings that populations with higher “social risk”—including racial and ethnic minorities and patients who are dual eligible—preform worse on many of Medicare’s pay-for-performance quality measures, including the ESKD QIP.36
It is reassuring that patients in rural areas and small towns did not experience significant changes in the independent risk of closure after the expanded ESKD payment bundle and that patients living in areas with more poverty and lower household incomes were not more likely to be affected by closures when considered across the entire study period. Yet, closures became even more common among the smallest dialysis facilities (those with <25 patients) and among hospital-based facilities, and closures remained more than twofold more common in facilities with 25–50 patients following the enactment of reimbursement reform. This supports concerns raised by the GAO that payment adjustments for small-volume facilities may be inadequate.13 It will be important for future studies to examine whether closures of small and hospital-based facilities influence patient health and/or access to care.
Although the relative risk of being affected by closures varied after reimbursement reform among certain high-risk populations and facilities, differences in absolute probabilities of closure associated with payment reform were small in nearly all high-risk and vulnerable populations. This is consistent with our primary finding that there was not an overall increase in facility closures in the first 5 years following reimbursement reform. However, ongoing reforms to dialysis reimbursement may place these high-risk populations at a risk for future closures. A report from the GAO in 2012 indicated that initial bundled payments were too high after accounting for decreased use of injectable medications.37 Subsequent legislation required that the CMS rebase (decrease) the bundled payment for dialysis beginning in 2014.38 Meanwhile, dialysis facilities experienced temporary payment reductions from sequestering, faced financial penalties of up to 2% for poor performance in the ESKD QIP, and faced ongoing administrative costs associated with reporting for the QIP. If the economic burdens associated with these recent policies lead to increased facility closures, it will be important to monitor access to care in the high-risk groups that we identified.
This study has several limitations. We only had data through 2015 and were unable to identify more recent trends in facility closures. Our study design assumed that no other unobserved factors influenced facility closures at the time that the expanded ESKD payment bundle was enacted, and we relied on information from the CMS-2728 form for the ascertainment of comorbidities in our primary analysis, which has limitations. Aside from the ESKD QIP, which began affecting payment in 2012, we are unaware of other changes that occurred at that time. However, we cannot exclude the possibility that other unobserved factors (e.g., changes in the cost of labor and dialysis supplies and regional changes in population growth) influenced closures, and we cannot fully disentangle the effects of the expanded ESKD payment bundle from those of the QIP. Finally, this study focused on the likelihood of being affected by dialysis facility closures. Although closures may have led to immediate care disruptions among affected patients, future studies will need to examine the effects of facility closures on patient health outcomes and access to dialysis care.
In conclusion, we did not find evidence that the 2011 expansion of the ESKD payment bundle was associated with an increased effect of facility closures on patients receiving outpatient dialysis in the first 5 years. However, the likelihood of being affected by closures changed slightly for some high-risk patient groups. Although it is reassuring that the 2011 payment reform did not increase closures, ongoing reimbursement reforms highlight the need for continued monitoring of dialysis facility closures and access to dialysis care among vulnerable patient groups.
Disclosures
Dr. Winkelmayer reports personal fees from Akebia, personal fees from Amgen, personal fees from AstraZeneca (includes ZS Pharma), personal fees from Bayer, personal fees from Daichii-Sankyo, personal fees from Janssen, and personal fees from Vifor FMC Renal Pharma (includes Relypsa) outside the submitted work. Dr. Ho is a board member of Community Health Choice. Dr. Erickson reports grants from the American Society of Nephrology during the conduct of the study, personal fees from Acumen LLC, personal fees from DCI Inc., and other from Satellite Dialysis outside the submitted work. All remaining authors have nothing to disclose.
Funding
This project was funded American Society of Nephrology Foundation for Kidney Research Carl W. Gottschalk Research Scholar Grant.
Supplementary Material
Acknowledgments
This work was conducted under a data use agreement between Dr. Winkelmayer and the National Institutes for Diabetes and Digestive and Kidney Diseases (NIDDK). An NIDDK officer reviewed the manuscript and approved it for submission.
The data reported here have been supplied by the US Renal Data System. The interpretation and reporting of these data are the responsibility of the author(s) and in no way should be seen as an official policy or interpretation of the US Government.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
Supplemental Material
This article contains the following supplemental material online at http://jasn.asnjournals.org/lookup/suppl/doi:10.1681/ASN.2019060575/-/DCSupplemental.
Supplemental Material. Exhibits 1–6: identifying and validating dialysis facility closures, calculating a comorbidity score, interrupted time series regression, estimating changes in facility closures among high-risk and vulnerable groups after payment reform, sensitivity analyses, and examining the estimated effects of black race and facility closures, respectively.
Supplemental Figure 1. Compare two identification methods, facility survey and RXHIST, on percentage of patients affected by facility closure.
Supplemental Figure 2. Logistic regression estimates with and without the expanded ESKD prospective payment system.
Supplemental Table 1. Results from analyses of effect modification.
References
- 1.Castle NG, Engberg J, Lave J, Fisher A: Factors associated with increasing nursing home closures. Health Serv Res 44: 1088–1109, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Banerjee T, Crews DC, Wesson DE, Dharmarajan S, Saran R, Ríos Burrows N, et al.; CDC CKD Surveillance Team: Food insecurity, CKD, and subsequent ESRD in US adults. Am J Kidney Dis 70: 38–47, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Crews DC, Charles RF, Evans MK, Zonderman AB, Powe NR: Poverty, race, and CKD in a racially and socioeconomically diverse urban population. Am J Kidney Dis 55: 992–1000, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nicholas SB, Kalantar-Zadeh K, Norris KC: Socioeconomic disparities in chronic kidney disease. Adv Chronic Kidney Dis 22: 6–15, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Forster AJ, Clark HD, Menard A, Dupuis N, Chernish R, Chandok N, et al.: Adverse events among medical patients after discharge from hospital. CMAJ 170: 345–349, 2004. [PMC free article] [PubMed] [Google Scholar]
- 6.Bhat P, Sokolowski W, Bhat JG: Projected impact of the proposed “bundled” ESRD payment system on a small dialysis organization. Nephrol News Issues 23: 46–52, 2009. [PubMed] [Google Scholar]
- 7.Stephens JM, Brotherton S, Dunning SC, Emerson LC, Gilbertson DT, Harrison DJ, et al.: Geographic disparities in patient travel for dialysis in the United States. J Rural Health 29: 339–348, 2013. [DOI] [PubMed] [Google Scholar]
- 8.Kenney RJ: Emergency preparedness concepts for dialysis facilities: Reawakened after Hurricane Katrina. Clin J Am Soc Nephrol 2: 809–813, 2007. [DOI] [PubMed] [Google Scholar]
- 9.Kopp JB, Ball LK, Cohen A, Kenney RJ, Lempert KD, Miller PE, et al. : Kidney patient care in disasters: Lessons from the hurricanes and earthquake of 2005. Clin J Am Soc Nephrol 2: 814–824, 0 [DOI] [PubMed] [Google Scholar]
- 10.Lin CJ, Pierce LC, Roblin PM, Arquilla B: Impact of Hurricane Sandy on hospital emergency and dialysis services: A retrospective survey. Prehosp Disaster Med 29: 374–379, 2014. [DOI] [PubMed] [Google Scholar]
- 11.Lurie N, Finne K, Worrall C, Jauregui M, Thaweethai T, Margolis G, et al.: Early dialysis and adverse outcomes after hurricane sandy. Am J Kidney Dis 66: 507–512, 2015. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Medicare & Medicaid Services, HHS : Medicare Program: End-Stage Renal Disease Prospective Payment System, Baltimore, MD, Centers for Medicare and Medicaid Services, 2010, pp 49030–49214 [Google Scholar]
- 13.Government Accountability Office : End-Stage Renal Disease: CMS Should Improve Design and Strengthen Monitoring of Low-Volume Adjustment, Washington, DC, Government Accountability Office, 2013 [Google Scholar]
- 14.Medicare Payment Advisory Commission : March 2015 Report to Congress: Medicare Payment Policy, Washington, DC, Medicare Payment Advisory Commission, 2015 [Google Scholar]
- 15.Hemmelgarn BR, Manns BJ, Quan H, Ghali WA: Adapting the Charlson Comorbidity Index for use in patients with ESRD. Am J Kidney Dis 42: 125–132, 2003. [DOI] [PubMed] [Google Scholar]
- 16.Austin PC: Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28: 3083–3107, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wagner AK, Soumerai SB, Zhang F, Ross-Degnan D: Segmented regression analysis of interrupted time series studies in medication use research. J Clin Pharm Ther 27: 299–309, 2002. [DOI] [PubMed] [Google Scholar]
- 18.Card D, Dobkin C, Maestas N: Does medicare save lives? Q J Econ 124: 597–636, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huber PJ: The behavior of maximum likelihood estimates under nonstandard conditions. Proceedings of the Fifth Berkley Symposium on Mathematical Statistics and Probability. Statistics 1: 221–233, 1967 [Google Scholar]
- 20.The Medicare Improvements for Patients and Providers Act of 2008 (MIPPA), Pub. L. No. 110-275, 2008
- 21.PRNewsWire : DaVita completes acquisition of renal ventures, Denver, CO, Davita Kidney Care, 2017 [Google Scholar]
- 22.BainCapital : US renal care to be acquired by investor group, Plano, TX, U.S. Renal Care, 2019 [Google Scholar]
- 23.Bannow T: Fresenius Medical Care closes $2 billion NxStage acquisition, Chicago, IL, Modern Healthcare, 2019 [Google Scholar]
- 24.Charytan C: Bundled-rate legislation for Medicare reimbursement for dialysis services: Implications for anemia management with ESAs. Clin J Am Soc Nephrol 5: 2355–2362, 2010. [DOI] [PubMed] [Google Scholar]
- 25.Hirth RA, Turenne MN, Wheeler JR, Nahra TA, Sleeman KK, Zhang W, et al.: The initial impact of Medicare’s new prospective payment system for kidney dialysis. Am J Kidney Dis 62: 662–669, 2013. [DOI] [PubMed] [Google Scholar]
- 26.Drüeke TB, Locatelli F, Clyne N, Eckardt KU, Macdougall IC, Tsakiris D, et al.; CREATE Investigators: Normalization of hemoglobin level in patients with chronic kidney disease and anemia. N Engl J Med 355: 2071–2084, 2006. [DOI] [PubMed] [Google Scholar]
- 27.Singh AK, Szczech L, Tang KL, Barnhart H, Sapp S, Wolfson M, et al.; CHOIR Investigators: Correction of anemia with epoetin alfa in chronic kidney disease. N Engl J Med 355: 2085–2098, 2006. [DOI] [PubMed] [Google Scholar]
- 28.US Food & Drug Administration : Information on erythropoiesis-stimulating agents (ESA) epoetin alfa (marketed as procrit, epogen), darbepoetin alfa (marketed as Aranesp), Washington, DC, US Food & Drug Administration, 2017 [Google Scholar]
- 29.Chertow GM, Liu J, Monda KL, Gilbertson DT, Brookhart MA, Beaubrun AC, et al.: Epoetin alfa and outcomes in dialysis amid regulatory and payment reform. J Am Soc Nephrol 27: 3129–3138, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tentori F, Zepel L, Fuller DS, Wang M, Bieber BA, Robinson BM, et al.: The DOPPS practice monitor for US dialysis care: PTH levels and management of mineral and bone disorder in US hemodialysis patients. Am J Kidney Dis 66: 536–539, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tentori F, Fuller DS, Port FK, Bieber BA, Robinson BM, Pisoni RL: The DOPPS practice monitor for US dialysis care: Potential impact of recent guidelines and regulatory changes on management of mineral and bone disorder among US hemodialysis patients. Am J Kidney Dis 63: 851–854, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spoendlin J, Schneeweiss S, Tsacogianis T, Paik JM, Fischer MA, Kim SC, et al.: Association of Medicare’s bundled payment reform with changes in use of vitamin D among patients receiving maintenance hemodialysis: An interrupted time-series analysis. Am J Kidney Dis 72: 178–187, 2018. [DOI] [PubMed] [Google Scholar]
- 33.MEDPAC : Outpatient dialysis services payment system. 2016. Available at: http://www.medpac.gov/docs/default-source/payment-basics/medpac_payment_basics_16_dialysis_final.pdf. Accessed April 10, 2019
- 34.University of Michigan Kidney Epidemiology and Cost Center : End stage renal diseasepayment system: Results of research on case-mix adjustment for an expanded bundle. 2008. Available at: https://kecc.sph.umich.edu/sites/default/files/attachments/publications/UM_KECC_ESRD_Bundle_Report.pdf. Accessed February 2, 2019
- 35.Turenne MN, Cope EL, Porenta S, Mukhopadhyay P, Fuller DS, Pearson JM, et al.: Has dialysis payment reform led to initial racial disparities in anemia and mineral metabolism management? J Am Soc Nephrol 26: 754–764, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation : Report to Congress: Social Risk Factors and Performance under Medicare’s Value-Based Purchasing Programs, Washington, DC, Department of Health and Human Services, 2016 [Google Scholar]
- 37.GOA : End-stage renal disease: Reduction in drug utilization suggests bundled payment is too high. 2012. Available at: https://www.gao.gov/products/GAO-13-190R. Accessed April 10, 2019
- 38.Wish D, Johnson D, Wish J: Rebasing the Medicare payment for dialysis: Rationale, challenges, and opportunities. Clin J Am Soc Nephrol 9: 2195–2202, 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.