Abstract
Purpose
The aim of this study was to analyze and evaluate dental antibiotic prescriptions in Albaha Region, Saudi Arabia.
Patients and Methods
A two-year retrospective cohort study was conducted between September 1, 2017 and September 1, 2019 in children and adults. Data collected from the patients’ medical records were analyzed using SPSS. The Z-test with Bonferroni correction and descriptive proportions were utilized to compare several levels of categorical variables.
Results
Of the 43,255 dental visits, antibiotics were provided during 12,573 (29.1%). The commonly prescribed antibiotics were amoxicillin and amoxicillin combined with metronidazole (56.3% and 16.9%, respectively). Alarmingly, antibiotics were provided in several conditions for which they are medically neither recommended nor indicated; together, they represented 27.8% of those consultations in which antibiotics were prescribed. Female dentists prescribed more antibiotics than male dentists (30%, P = < 0.000), with male patients receiving more antibiotics than female patients (36%, P = <0.0001).
Conclusion
Unnecessary prescription of antibiotics was observed in the present study. Improving knowledge and awareness of Saudi dentists on dental antibiotic prescription is warranted.
Keywords: risk management, health policy, early diagnosis, oral disease, dental service
Introduction
Inappropriate use of antibiotics contributes to the evolution of resistant strains and poses a substantial risk to the health and well-being of individuals and communities.1 The misuse of antibiotics is not only considered a major driver for the elevated frequency of antimicrobial resistance (AMR) but also as a public health issue.2 Thus, more escalations in the AMR level due to the misuse of antibiotics will result in adverse and broad impacts on the individual’s health and well-being.3
Many studies have evaluated the prescription trend of dental antibiotics worldwide.4–9 For instance, in the USA, it was found that dental practitioners and dentists prescribed more than 2.9 million antibiotics per year.5 Moreover, a retrospective study in Croatia showed that antibiotics were prescribed during almost half of the dental emergency visits.8 Similarly, in the UK, a retrospective cohort research revealed that dental antibiotics were prescribed during more than half of dental consultations.9 These findings indicate a negative contribution of medical practitioners toward AMR and paucity of knowledge among the public over-the-counter availability of antibiotics as well as leftover antibiotic usage, which is the hallmark of low- and middle-income countries.
Early dental research conducted on prescribing dental antibiotics in Saudi Arabia generally used questionnaire-based self-reported data. Several studies have evaluated awareness, knowledge, habits, and attitudes in relation to prescribing dental antibiotics among Saudi dental practitioners or dental students.10–14 These studies concluded that poor practice of prescribing dental antibiotics was prevalent among Saudi dentists and dental students.11,14 The studies also highlighted that Saudi dentists lacked knowledge and misused antibiotic prescription in endodontic therapy,12 emphasizing the improvement of knowledge among Saudi dentists regarding odontogenic infection management.13 Moreover, only one literature review has explored the association between dental antibiotics and root canal therapy.15 However, these reports suggest that Saudi dentists lack in implementing an evidence-based dentistry approach when prescribing antibiotics during dental consultations. Interestingly, neither systematic reviews nor retrospective or prospective cohort studies explored the prescription and use of antibiotics within the dental consultations in Saudi Arabia. Notably, no study in the literature has evaluated dental antibiotic prescriptions in the Albaha Region of Saudi Arabia. Hence, the nature of the research conducted on the prescription of antibiotics among dentists and dental practitioners remains misunderstood in Saudi Arabia, particularly in the Albaha Region.
Dental antibiotic prescriptions and practices must be centered on its ability to explore, manage, and reduce possible adverse side effects, impacts, and bacterial resistance caused by the inappropriate use of dental antibiotics. This study, therefore, aims to retrospectively analyze and evaluate dental antibiotic prescriptions in the Albaha Region, Saudi Arabia.
Materials and Methods
Participants and Settings
A two-year cross-sectional retrospective cohort study was conducted in the Albaha Region, Saudi Arabia. Data were collected retrospectively from the patients’ medical records and inputted into a pre-designed computer database. All subjects who attended the dental center between September 1, 2017 and September 1, 2019 were included.
The study was conducted in a governmental dental center in the Albaha Region, which was selected randomly for this study. This dental center is provided by the Saudi Ministry of Health and consists of 22 dental clinics. It provides various dental treatments during working hours (8.00 AM to 4.00 PM, Sunday–Thursday), including, but not limited to, dental fillings, root canal treatments, periodontal treatments, pediatric dental therapies, oral surgeries, dental implants, orthodontic rehabilitations, and fixed and removable prosthodontics, but it does not provide emergency dental services.
Ethical Considerations
This study was approved by the Ethics Committee of the Education Training Center and Academic Affairs at the Saudi Ministry of Health “Albaha branch” (Approval Number: 19/0910). Moreover, it can be confirmed that the study was conducted in full accordance with the Saudi Ministry of Health Ethical Standards and the World Medical Association Declaration of Helsinki.
Data Collection
Data were collected retrospectively between August 1, 2019 and November 1, 2019. During the data collection stage, several variables were obtained, including a patient’s age and gender, a dentist’s gender, a dentist’s main specialty, dental diagnoses, and antibiotics prescribed. Dentists’ main specialties were categorized into periodontics, endodontics, prosthodontics, orthodontics, oral surgery, oral medicine, operative dentistry, and pediatric dentistry. Diagnoses were established on the evaluation of the dental practitioner who admitted the patient and classified periodontitis, gingivitis, chronic apical abscess, acute apical abscess, symptomatic apical periodontitis, periapical cyst, pericoronitis, reversible pulpitis, pulpal necrosis, irreversible pulpitis, extraction, and dental caries. Nevertheless, several types of antibiotics were included: amoxicillin, amoxicillin/clavulanic acid, metronidazole, and cephalosporin.
Statistical Analysis
Data analysis was conducted using the Statistical Package for the Social Sciences® (SPSS) version 20.0; the significance level was adjusted at 0.05. The Z-test with a Bonferroni correction and descriptive proportions were utilized to compare several levels of categorical variables. Moreover, the frequency of antibiotic prescription was investigated and described as the number of dental consultations in which an antibiotic was provided divided by the total number of dental consultations for different levels of other variables.
Results
A total of 43,255 dental visits were included in this study. Of these, 12,573 were prescribed antibiotics, representing 29.1% of total dental visits. The prescribing of dental antibiotics without providing any dental therapy was recorded in 4038 dental consultations, representing 9.3% of all dental consultations and 32.1% of dental consultations in which antibiotics were prescribed.
Participants included in the study were from different age groups and genders, visited different dental specialists, had different dental diagnoses, and received dissimilar dental therapies, which may indicate the diversity of the study sample. Table 1 summarizes the characteristics of dental consultations.
Table 1.
Summary of the Dental Consultations Characteristics
| Characteristics | n | % |
|---|---|---|
| Patient’s Age (Years) | ||
| Children < 10 | 3327 | 7.7 |
| Children between 11 and 17 | 5391 | 12.5 |
| 18 to 30 | 17,626 | 40.7 |
| 31 to 40 | 7685 | 17.8 |
| 41 to 50 | 4045 | 9.4 |
| 51 to 60 | 2807 | 6.5 |
| 61 to 70 | 1707 | 3.9 |
| >71 | 667 | 1.5 |
| Patient’s Gender | ||
| Male | 16,673 | 38.5 |
| Female | 26,582 | 61.5 |
| Dentist’s Specialty | ||
| Endodontics | 14,027 | 32.4 |
| Operative Dentistry | 3256 | 7.5 |
| Oral Medicine | 7439 | 17.2 |
| Oral Surgery | 4762 | 11.0 |
| Orthodontics | 3021 | 7.0 |
| Pediatric Dentistry | 3805 | 8.8 |
| Periodontics | 2846 | 6.6 |
| Prosthodontics | 4099 | 9.5 |
| Diagnosis | ||
| Acute Apical Abscess | 19,502 | 45.1 |
| Chronic Apical Abscess | 2991 | 6.9 |
| Dental Caries | 801 | 1.9 |
| Extraction | 725 | 1.7 |
| Gingivitis | 4167 | 9.6 |
| Irreversible Pulpitis | 344 | 0.8 |
| Oral Surgery | 36 | 0.1 |
| Symptomatic Apical Periodontitis | 4121 | 9.5 |
| Pericoronitis | 386 | 0.9 |
| Periodontitis | 593 | 1.4 |
| Preapical Cyst | 2567 | 5.9 |
| Pulpal Necrosis | 172 | 0.4 |
| Reversible Pulpitis | 855 | 2.0 |
| Not mentioned (others) | 5995 | 13.9 |
| Antibiotic Prescribed | ||
| No antibiotic prescribed | 30,682 | 70.9 |
| Amoxicillin | 7080 | 16.4 |
| Amoxicillin + Amoxicillin/clavulanic acid | 32 | 0.1 |
| Amoxicillin + Metronidazole | 2128 | 4.9 |
| Amoxicillin/clavulanic acid | 1392 | 3.23 |
| Amoxicillin/clavulanic acid + Metronidazole | 1460 | 3.4 |
| Cephalosporin | 297 | 0.7 |
| Metronidazole | 184 | 0.4 |
Of those dental consultations in which antibiotics were prescribed, amoxicillin was the most commonly prescribed antibiotics (56.3%). Amoxicillin + metronidazole, amoxicillin/clavulanic acid + metronidazole, amoxicillin/clavulanic acid alone, and cephalosporin alone were less commonly prescribed (16.9%, 11.6%, 11%, and 2.4%, respectively). However, the frequency of prescribing metronidazole alone was less than 1.5% of the total dental consultations. Nevertheless, with great interest, there were 32 cases (<0.3% of the consultations) in which amoxicillin and amoxicillin/clavulanic acid were prescribed simultaneously. Notably, all these cases were seen by periodontists and oral surgeons. Table 2 is a summary of the dosage and duration of antibiotics prescribed.
Table 2.
Summary of Dosage and Duration of Antibiotic Prescribed
| Antibiotic Prescribed | Adult’s Dosage | Child’s Dosage | Duration |
|---|---|---|---|
| Amoxicillin | 500 mg | 250mg/5mL | 5 to 7 Days |
| Amoxicillin/clavulanic acid | 625 mg | 156mg/5mL | 5 to 7 Days |
| Metronidazole | 500 mg | 125mg/5mL | 5 to 7 Days |
| Cephalosporin | 500 mg | 250mg/5mL | 5 to 7 Days |
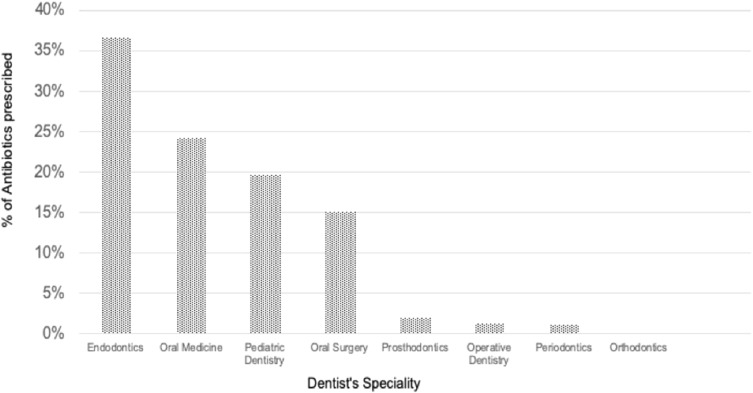
The findings of this study revealed an obvious variation in prescribing antibiotics based on dentists’ specialties (Figure 1). Of the dental visits in which antibiotics were prescribed, endodontists, oral medicine specialists, and pediatric dentists were most frequently prescribing antibiotics than other dental specialists (36.6%, 24.2%, and 19.7%, respectively). It is noteworthy that prosthodontists, operative dentistry specialists, periodontists, and orthodontists less often prescribed dental antibiotics (1.9%, 1.2%, 1.1%, and 0.1%, respectively). Although the regularity of prescribing antibiotics varied dramatically among different dental specialists, the preference for specific categories of antibiotics was alike among different dental specialists, with amoxicillin most often prescribed (43.6% to 89.5% of all antibiotics).
Figure 1.
Association between dentist’s specialty and frequency of prescribing antibiotics.
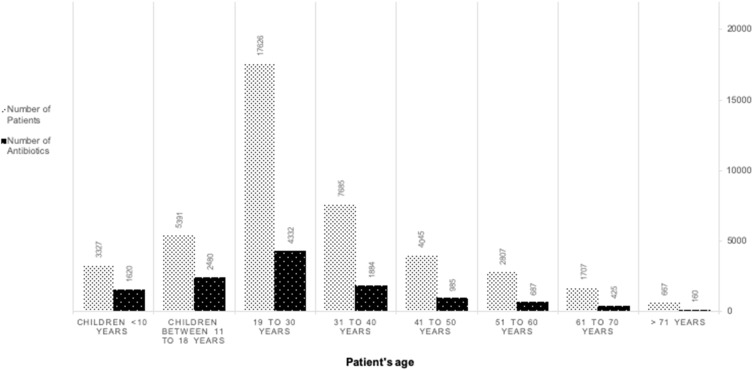
The distribution of participants according to their age and frequency of prescribed antibiotics is described in Figure 2. Participants aged 18 to 30 years consisted of 41% of all participants and showed a high frequency of receiving antibiotics (34.5%) compared to other age groups. This increased use of antibiotic prescriptions might be because oral diseases are more frequent in those ages. Patients under 18 years and between 31 and 40 years received 32.6% and 15% of prescribed antibiotics, respectively.
Figure 2.
Participants’ age and frequency of prescribing antibiotics.
Female dentists admitted and examined slightly more patients than male dentists (50.7% and 49.3%, respectively), and they also prescribed significantly more antibiotics than male dentists (30% and 28%, P = <0.0001, of the total dental consultations, respectively). Additionally, male patients received significantly more antibiotics than female patients (36% and 25%, P = <0.0001, of the total dental consultations, respectively).
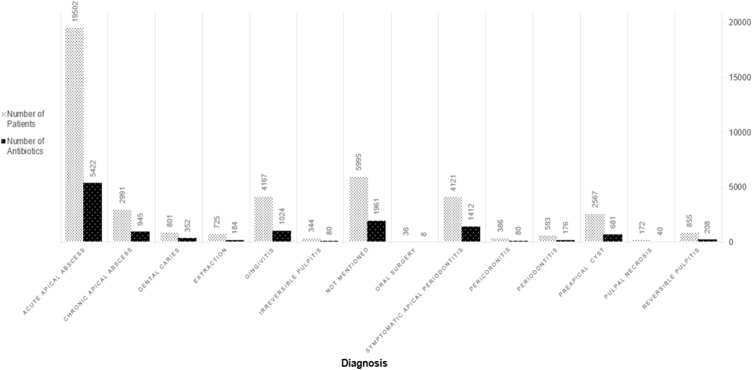
Acute apical abscess, gingivitis, and symptomatic apical periodontitis were the most common diagnoses within all dental consultations (45.1%, 9.6%, and 9.5%, respectively). Figure 3 describes the number of antibiotics prescribed and the number of patients for each dental diagnosis. Remarkably, dentists’ diagnoses were not recorded in (n = 5995, 13.9%) of all dental visits.
Figure 3.
Association between patients’ diagnoses and frequency of prescribing antibiotics.
This study found that antibiotics were occasionally prescribed for clinical conditions in which they are neither inappropriate nor typically unnecessary, as some dentists prescribed antibiotics for patients who had dental caries, periodontitis, pulpal necrosis, and reversible and irreversible pulpitis, together representing 6.8% of those consultations in which antibiotics were prescribed. Likewise, patients who were diagnosed with gingivitis, chronic apical abscess, and preapical cysts were more exposed to malpractices in the prescription of antibiotics than other patients (8.1%, 7.5%, and 5.4%, respectively).
Discussion
Inappropriate antibiotic administration and use were observed in the present study. Interestingly, no retrospective cohort studies in the dental literature have evaluated the prescription of antibiotics within dental consultations in Saudi Arabia, particularly in the Albaha Region. However, some self-reported data and questionnaire-based studies have evaluated awareness, knowledge, habits, and attitudes in relation to prescribing dental antibiotics among Saudi dentists or dental students.10–14 The current study, first of its kind, evaluated and analyzed a total of 43,255 dental visits over a two-year period. It identified factors such as the prescription of antibiotics in dental consultations, including patients’ age and gender, dentists’ gender, dentists’ specialty, and dentists’ diagnoses.
Our findings revealed that the most commonly prescribed antibiotic is amoxicillin (56.3%), corroborating other national and international studies conducted in Saudi Arabia, the United States, Turkey, and Croatia, in which Amoxicillin was regarded as the first-choice antibiotic in dental consultations (60%, 61%, 67.8%, and 70.5%, respectively).8,12,16,17 Moreover, in 32 cases, periodontists and oral surgeons prescribed amoxicillin in combination with amoxicillin/clavulanic acid for treating symptomatic apical periodontitis or acute apical abscess. However, no evidence has demonstrated any superior effectiveness of combining these two antibiotics for treating odontogenic infection.17,18 This overprescription might be contributed to dentists’ lack of knowledge, differences in work experience, and insufficient understanding of applying evidence-based dentistry approaches concerning antibiotic prescriptions. Regardless of the reason behind this misuse of antibiotic prescriptions, these findings highlight the urgent need for effective mentoring, a governing strategy, and a system that ensures dental antibiotics are appropriately prescribed by Saudi dentists.
Interestingly, neither antivirals nor antifungals were recorded in all dental prescriptions. Likewise, neither viral infections nor fungal infections were diagnosed in all dental consultations. These findings indicated that diagnosing patients with viral or fungal infections appear to not be a common practice. Nevertheless, although the policy and guidelines of the Saudi Ministry of Health emphasize writing the diagnosis in all prescriptions, around 15.6% of antibiotics were prescribed without written diagnoses in the prescriptions. Consequently, developing an effective strategy for implementing the Saudi Ministry of Health policy and guidelines in all dental consultations beyond an operative process for auditing dentists’ performance in prescribing dental antibiotics may be suggested.
The present study found that dentists’ specialty influenced their prescription of antibiotics. Endodontists, oral medicine specialists, and pediatric dentists more often prescribe antibiotics than other dental specialists (36.6%, 24.2%, and 19.7%, respectively). Therefore, it was expected that endodontists and oral medicine practitioners would prescribe more antibiotics than other dentists, as the majority of the patients in this study were diagnosed with acute apical abscess. However, pediatric dentists should not frequently prescribe antibiotics. This contradicts other works in India in which pediatric dentists prescribed significantly fewer antibiotics than other dentists.19 Those dentists could potentially have lacked an understanding of what the national guidelines say about prescribing antibiotics to children. However, developing decision aids consistent with international and national guidelines on antibiotic prescription may be recommended.
Female dentists prescribed significantly more antibiotics than male dentists (30% and 28%, P = <0.0001, respectively). Likewise, Croatian female dentists prescribed significantly more antibiotics than male dentists (50.8% and 46.8%, P = <0.001, respectively),8 while dentists’ gender did not influence the prescription of antibiotics in the United States.16 Moreover, our study concluded that male patients received significantly more antibiotics than female patients (36% and 25%, P = <0.0001, respectively). Similarly, other works conducted in Kosovo found that male patients received more antibiotics than female patients (52% and 48%, respectively), but this difference in prescribing antibiotics was not significant.20 In contrast, no gender differences in prescribing dental antibiotics were found among Croatian and British Columbian patients.8,21 Indeed, it might be a challenge to explain why gender differences in both dentists and patients influence antibiotic prescriptions in the present study. The data obtained in this study might not be sufficient to describe this difference. However, several factors may contribute to this difference, including dentists’ qualifications (undergraduate or postgraduate), dentists’ clinical experiences and situations, the duration of symptoms, fear of spreading infection, advance care plans, use of diagnostic resources and patient expectations.22–24
The findings of this study revealed that antibiotics were provided in several conditions for which they are medically not recommended, including gingivitis, chronic apical abscess, preapical cysts, dental caries, periodontitis, pulpal necrosis, and reversible and irreversible pulpitis. These findings are consistent not only with the recent report of a national survey of antibiotic use by American endodontists16 but also with a survey conducted in Brazil.25 However, antibiotics ought not to be prescribed for the diagnoses mentioned above, pain reduction, and odontogenic infection unless there was evidence of systematic disease involvement or the spreading of an infection such as fever or swelling or both of them.26–28 Nevertheless, the possible explanation for this wrong practice of excessively prescribing dental antibiotics might have several components, including the following: 1) patient’s expectations, preferences, and requests; 2) lack of cooperation from the patient; 3) inappropriate dental diagnoses aimed at preventing possible complications but with no definitive indications; 4) dentists’ workload and number of patients seen.6,29,30 To ensure optimal antimicrobial management within Saudi dental centers, the periodic review and audit of dental antibiotic prescriptions in Saudi dental centers may be advocated.
There are four key limitations in the present study. First, no emergency dental visits are recorded in this study because there is limited information based on our data. Yet, regular dental services differ from emergency dental services, with the latter covering only simple dental procedures and the referral of patients to regular services for all dental therapy. Abuse of the prescription of antibiotics in emergency dental services has been well documented in the dental literature.8,31 Consequently, future research might evaluate the prescription of dental antibiotics in both regular and emergency dental services. A second limitation of this study is a lack of evaluation of other factors that may contribute to the prescribing of dental antibiotics, such as dentists’ qualifications (undergraduate or postgraduate), dentists’ experience, dentists’ workload, and time of the day in which antibiotics were prescribed. Nevertheless, the emphasis of this study is on evaluating and analyzing dental antibiotic prescriptions in the Albaha Region, Saudi Arabia. A third limitation of the present study is the non-evaluation of other prescribed non-antibiotic drugs. The use of some non-antibiotic agents may influence the choice of antibiotics in dental treatments. Lastly, although this was a two-year cross-sectional retrospective study and included data from only one governmental dental center, it provides insight into the evaluation of dental antibiotic prescriptions in the Albaha Region, Saudi Arabia.
Conclusions
The amoxicillin and amoxicillin combined with metronidazole were the most commonly prescribed antibiotics. Female dentists not only prescribed significantly more antibiotics than male dentists but also male patients received significantly more antibiotics than female patients. We also observed unnecessary antibiotic prescriptions, including excessive, noncritical, and inappropriate indications by Saudi dentists. This inappropriate antibiotic use can drive to increase the risk of managing the AMR in the Albaha Region of Saudi Arabia. Establishing an effective continuing educational strategy that could support improving knowledge and awareness of Saudi dentists concerning dental antibiotic prescription may be recommended. Future research direction may focus on evaluating the prescription of antibiotics in both regular and emergency dental services, including evaluating the possible factors contributing to the prescription of dental antibiotics, such as dentists’ qualifications and experiences, dentists’ workload, and time of the day in which antibiotics were prescribed. Conducting a comprehensive study that focuses on evaluating dental antibiotic prescriptions and covering the entirety of Saudi Arabia may also be highlighted.
Acknowledgments
We would like to acknowledge the Education Training Center and Academic Affairs at the Saudi Ministry of Health ‘Albaha branch,’ for their cooperation and helping to facilitate this study.
Data Sharing Statement
The data supporting the findings of the article are available upon request from the main author, Dr Alzahrani, email: aahalzahrani@bu.edu.sa.
Disclosure
The authors report no conflict of and/or competing interest in this work.
References
- 1.World Health Organization. Antimicrobial Resistance: Global Report on Surveillance. World Health Organization; 2014. Availabe form: https://apps.who.int/iris/handle/10665/112642. Accessed October18, 2019. [Google Scholar]
- 2.Davies J, Davies D. Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev. 2010;74(3):417–433. doi: 10.1128/MMBR.00016-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Degeling C, Johnson J, Iredell J, et al. Assessing the public acceptability of proposed policy interventions to reduce the misuse of antibiotics in Australia: A report on two community juries. Health Expect. 2018;21(1):90–99. doi: 10.1111/hex.12589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stein K, Farmer J, Singhal S, Marra F, Sutherland S, Quinonez C. The use and misuse of antibiotics in dentistry: a scoping review. J Am Dent Assoc. 2018;149(10):869–884. doi: 10.1016/j.adaj.2018.05.034 [DOI] [PubMed] [Google Scholar]
- 5.Durkin MJ, Hsueh K, Sallah YH, et al. An evaluation of dental antibiotic prescribing practices in the United States. J Am Dent Assoc. 2017;148(12):878–886. doi: 10.1016/j.adaj.2017.07.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cope AL, Francis NA, Wood F, Chestnutt IG. Antibiotic prescribing in UK general dental practice: a cross-sectional study. Community Dent Oral Epidemiol. 2016;44(2):145–153. doi: 10.1111/cdoe.12199 [DOI] [PubMed] [Google Scholar]
- 7.Lalloo R, Solanki G, Ramphoma K, Myburgh NG. Antibiotic-prescribing patterns of South African dental practitioners following tooth extractions. J Investig Clin Dent. 2017;8(4):e12247–e12253. doi: 10.1111/jicd.12247 [DOI] [PubMed] [Google Scholar]
- 8.Bjelovucic R, Par M, Rubcic D, Marovic D, Prskalo K, Tarle Z. Antibiotic prescription in emergency dental service in Zagreb, Croatia–a retrospective cohort study. Int Dent J. 2019;69(4):263–280. doi: 10.1111/idj.12460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cope AL, Chestnutt IG, Wood F, Francis NA. Dental consultations in UK general practice and antibiotic prescribing rates: a retrospective cohort study. Br J Gen Pract. 2016;66(646):e329–e336. doi: 10.3399/bjgp16X684757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abu-mostafa NA, Al-mejlad NJ, Al-yami AS, Al-sakhin FZ, Al-mudhi SA. A survey of awareness related to the use of antibiotics for dental issues among non-medical female university students in Riyadh, Saudi Arabia. J Infect Public Health. 2017;10(6):842–848. doi: 10.1016/j.jiph.2017.01.015 [DOI] [PubMed] [Google Scholar]
- 11.Baskaradoss JK, Alrumaih A, Alshebel A, et al. Pattern of antibiotic prescription among dentists in Riyadh, Saudi Arabia. J Investig Clin Dent. 2018;9(3):1–7. doi: 10.1111/jicd.12339 [DOI] [PubMed] [Google Scholar]
- 12.AlRahabi MK, Abuong ZA. Antibiotic abuse during endodontic treatment in private dental centers. Saudi Med J. 2017;38(8):852–856. doi: 10.15537/smj.2017.8.19373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Al-sebaei MO, Jan AM. A survey to assess knowledge, practice, and attitude of dentists in the Western region of Saudi Arabia. Saudi Med J. 2016;37(4):440–445. doi: 10.15537/smj.2016.4.15019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.AboAlSamh A, Alhussain A, Alanazi N, Alahmari R, Shaheen N, Adlan A. Dental students’ knowledge and attitudes towards antibiotic prescribing guidelines in Riyadh, Saudi Arabia. Pharmacy (Basel). 2018;6(2):e42–e48. doi: 10.3390/pharmacy6020042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.AlRahabi MK. Root canal treatment in elderly patients: a review and clinical considerations. Saudi Med J. 2019;40(3):217–223. doi: 10.15537/smj.2019.3.23769 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Germack M, Sedgley CM, Sabbah W, Whitten B. Antibiotic use in 2016 by members of the American Association of Endodontists: report of a national survey. J Endod. 2017;43(10):1615–1622. doi: 10.1016/j.joen.2017.05.009 [DOI] [PubMed] [Google Scholar]
- 17.Koyuncuoglu CZ, Aydin M, Kirmizi NI, et al. Rational use of medicine in dentistry: do dentists prescribe antibiotics in appropriate indications? Eur J Clin Pharmacol. 2017;73(8):1027–1032. doi: 10.1007/s00228-017-2258-7 [DOI] [PubMed] [Google Scholar]
- 18.Palmer N. Antimicrobial Prescribing for General Dental Practitioners. Wales (UK): Faculty of General Dental Practitioners FGDP; 2016. [Google Scholar]
- 19.Konde S, Jairam LS, Peethambar P, Noojady SR, Kumar NC. Antibiotic overusage and resistance: a cross-sectional survey among pediatric dentists. J Indian Soc Pedod Prev Dent. 2016;34(2):145–151. doi: 10.4103/0970-4388.180444 [DOI] [PubMed] [Google Scholar]
- 20.Haliti N, Krasniqi S, Begzati A, et al. Antibiotic prescription patterns in primary dental health care in Kosovo. Family Med Prim Care Rev. 2017;19(2):128–133. doi:doi. 10.5114/fmpcr.2017.67866 [DOI] [Google Scholar]
- 21.Marra F, George D, Chong M, Sutherland S, Patrick DM. Antibiotic prescribing by dentists has increased: why? J Am Dent Assoc. 2016;147(5):320–327. doi: 10.1016/j.adaj.2015.12.014 [DOI] [PubMed] [Google Scholar]
- 22.van Buul LW, van der Steen JT, Doncker SM, et al. Factors influencing antibiotic prescribing in long-term care facilities: a qualitative in-depth study. BMC Geriatr. 2014;14:136–147. doi: 10.1186/1471-2318-14-136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lum EPM, Page K, Whitty JA, Doust J, Graves N. Antibiotic prescribing in primary healthcare: dominant factors and trade-offs in decision-making. Infect Dis Health. 2018;23(2):74–86. doi: 10.1016/j.idh.2017.12.002 [DOI] [PubMed] [Google Scholar]
- 24.Vardhan T, Lakhshmi N, Haritha B. Exploring the pattern of antibiotic prescription by dentists: a questionnaire-based study. J NTR Univ Health Sci. 2017;6(3):149–153. doi: 10.4103/jdrntruhs.jdrntruhs_30_17 [DOI] [Google Scholar]
- 25.Bolfoni MR, Pappen FG, Pereira-cenci T, Jacinto RC. Antibiotic prescription for endodontic infections: a survey of Brazilian Endodontists. Int Endod J. 2018;51(2):148–156. doi: 10.1111/iej.12823 [DOI] [PubMed] [Google Scholar]
- 26.Martin MV, Longman L, Palmer N. Adult Antimicrobial Prescribing in Primary Dental Care for General Dental Practitioners. 2nd ed. Wales (UK): Faculty of General Dental Practitioners; 2016. [Google Scholar]
- 27.Aminoshariae A, Kulild JC. Evidence-based recommendations for antibiotic usage to treat endodontic infections and pain: a systematic review of randomized controlled trials. J Am Dent Assoc. 2016;147(3):186–191. doi: 10.1016/j.adaj.2015.11.002 [DOI] [PubMed] [Google Scholar]
- 28.Agnihotry A, Fedorowicz Z, van Zuuren EJ, Farman AG, Al-langawi JH. Antibiotic use for irreversible pulpitis. Cochrane Database Syst Rev. 2016;5(2):4969–4975. doi: 10.1002/14651858.CD004969 [DOI] [PubMed] [Google Scholar]
- 29.Cope A, Francis N, Wood F, Mann MK, Chestnutt IG. Systemic antibiotics for symptomatic apical periodontitis and acute apical abscess in adults. Cochrane Database Syst Rev. 2014;9(6):10136–10143. doi: 10.1002/14651858.CD010136 [DOI] [PubMed] [Google Scholar]
- 30.Chate RA, White S, Hale LR, et al. The impact of clinical audit on antibiotic prescribing in general dental practice. Br Dent J. 2006;201(10):635–641. doi: 10.1038/sj.bdj.4814261 [DOI] [PubMed] [Google Scholar]
- 31.Roberts RM, Hersh AL, Shapiro DJ, Fleming-dutra KE, Hicks LA. Antibiotic prescriptions associated with dental-related emergency department visits. Ann Emerg Med. 2019;74(1):45–49. doi: 10.1016/j.annemergmed.2018.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]