Abstract
Alcohol and alcohol related harm are key public health challenges. Research has shown that individual level factors, such as age and sex, are important predictors of alcohol consumption, but such factors provide only a partial account of the drivers of consumption. In this paper we argue that individual level factors interact with features of the ‘risk environment’ to increase the vulnerability of individuals to such environments. Features of the alcohol ‘risk environment’ include the density of alcohol premises in a neighbourhood. Previous research has shown that neighbourhoods with a higher density of alcohol outlets have higher levels of both alcohol consumption and alcohol related harm. There has however been a distinct lack of attention paid to the differential ways in which particular socio-demographic groups may be more vulnerable to such ‘risk environments’. In this paper we address the risk environment through a primary focus on the local supply and availability of alcohol products (captured using a measure of outlet density) and the relationship with the harmful use of alcohol. Using responses to the Scottish Health Survey (2008-2011) we explore vulnerability through the interaction between individual level socio-economic position, measured using household income, and environmental risk to assess differential social vulnerability to such environments. We report findings showing that those in the lowest income groups may be disproportionately affected by outlet density. This evidence suggests that risk environments may not affect us all equally and that there may be socially differentiated vulnerability to such environments.
Keywords: Alcohol, outlet density, risk, vulnerability and health inequalities
Background
This paper presents research that seeks to expand our knowledge on the geographies of alcohol by taking an integrated perspective, incorporating assessment of geographical dimensions of risk and their relationship to individual behaviour. Recent literature from a health geography perspective emphasises how space can be viewed as constituting risk environments where the built and social dimensions of places can also be manipulated as means of risk governance and minimisation (Herrick 2011). In risk management policy, a distinction has often been made between environmental and lifestyle risks (Gabe 1995; Lupton 1993). Environmental risk management has tended to focus on toxins in the material environment, for example in the case of risks to pulmonary health, these include air pollutants, emissions from landfill waste or those produced by radon gas, or ‘second hand’ tobacco smoke. On the other hand, lifestyle risk risk management has been driven by discourse regarding the individualisation of risk; individuals are expected to regulate their own behaviours.
In this paper we consider alcohol consumption as an individual behaviour that is influenced by environmental factors and report on work to assess how some aspects of the ‘risk environment’ at a local level, which are not subject to very rigorous governance, may interact with individual risk behaviour. Annually, across the globe, in excess of 3 million deaths are attributable to alcohol, with alcohol related to over 200 health conditions (WHO 2014). Within Europe excessive alcohol consumption places a substantial burden on society and national health care systems (Angus et al. 2017). Drinking patterns however vary by country and in the UK per capita consumption of alcohol (age 15+) stands at 11.6 pure litres, whilst falling this remains higher than the European WHO region average of 10.9 litres (WHO 2014). Within the UK there are also differences by country with a fifth more alcohol sold per adult in Scotland than in England and Wales. Alcohol has been identified as a key factor in explaining the significant differences in health outcomes between Scotland and the rest of the UK, and is also implicated in country’s high (and rising) levels of health inequalities. Whilst the focus of this paper is on Scotland, Scotland is not unique in identifying ‘high risk’ drinking as a priority issue for public health. Although in Scotland, since 2009, there has been an 8 percent reduction in alcohol consumption per adult, sufficient alcohol is being sold for each adult in the country to drink more than 20 units each week, which is six units (43 percent) more than the current guidelines (1 unit is roughly equivalent to half a pint (284ml) of 3.5 percent strength beer or a single measure (25ml) of spirit, strength 37.5 percent. Units are calculated as strength (ABV) x volume (ml) ÷ 1,000 = unit). In this paper we examine whether those living in neighbourhoods of high alcohol outlet density exhibit different patterns of alcohol consumption patterns compared to those in areas of low alcohol outlet density. In a novel and significant addition to the literature we explore whether or not the risk environment shapes consumption patterns equally amongst all socioeconomic groups.
Geographers have for some time now been exploring alcohol environments, focussing on the political, economic, social, cultural and spatial processes that shape such environments and responses to them (Jayne et al. 2011). Related research has included both empirical, quantitative measures of the alcogenic environment and its relationship to alcohol-related harm, as well as a critique of such epistemological framing of alcohol as a medical issue (Jayne et al 2011b). Topics such as legislation and policy(Jayne, Valentine & Sarah L Holloway 2011b), the night-time economy (Demant & Landolt 2013), gentrification (Mathews & Picton 2014) and historical patterns of licensing (Beckingham 2012) have been key features of the research as well as those focussing on identity (Nayak 2003), drinking cultures (Jayne, Valentine & Gould 2012), lifestyle and the gendered nature of alcohol (Thurnell-Read 2013).
Whilst geographic literature suggests that ‘place matters’ for alcohol consumption and health-related outcomes, discourse regarding the privatisation of risk has shifted both political and public rhetoric towards individual responsibility and deviance from the ‘norm’ (Glasgow & Schrecker 2016). Although Giddens (1999) and Beck (1992) have been criticised for overemphasising the individual as an autonomous subject, their notions of risk do help us to refocus on positions regarding individual responsibility and risk governance, and to consider the changing dimensions of risk. Giddens argued that we have seen a transition from external risk to ‘manufactured’ risk, with risk moving from that which could be seen as outside the scope of society to that which has been created (Giddens, 1999). Whilst such an argument has been used to explore the rise of technology, it could also be applied to public health and the ways in which we define personal responsibility and unintended consequences of the risk society. Since the 1970s conflicting political, social and industry-related perceptions of risk and governance suggest two broad arguments regarding responsibility. On the one hand the individual is seen as responsible for managing lifestyles and associated health risks. Supporting such a framing of governance the alcohol industry, through Corporate Social Responsibility (CSR) activities, promote initiatives such as responsible alcohol consumption, server responsibility and the dangers of both drink driving and underage drinking (Babor & Robaina 2013). On the other hand, the emergence of a ‘new public health’ in public policy embraces a social determinants model that recognises risks in material and social living conditions, emphasises societal responsibility for these risks and suggests regulatory or statutory interventions at a population level. A more structuralist interventionist approach may therefore include limiting the availability of alcohol, taxation on alcoholic beverages and restrictions on alcohol advertising.
Interventions that focus on the former, embracing individual responsibility and behavioural change adopt theories of ‘rational decision making’ and ‘reasoned action’, seeing risk taking decisions as largely voluntary, products of health beliefs and therefore context free (Rhodes 2002). In such models of behaviour, risk plays a central role but is confined to a subjective cost-benefit analysis based on conscious actions that pay little attention to underlying influences (van der Plight 1998). Behaviour change led interventions have focussed on education, for example on improving public understanding of alcohol units and more recent attempts to highlight the calorie content of alcohol and campaigns to ‘go sober’ (examples from the UK include Macmillian’s ‘Go sober for October’ and Alcohol Concern’s ‘Dry January’). Room (2011) charts the rise of the individualised approach, arguing that commercial interests and free-market ideologies have pushed alcohol, and public health responses to related problems, towards a more open market. This rise resonates with Beck’s view of the economy as a system for the distribution of material benefits and risks (Beck, 1992) and Giddens’ discussion of the shift from external risk to manufactured risk (Giddens, 1999). A free-market view has however failed to recognise the complexity of the drivers behind alcohol misuse and instead creates two distinct camps; the ‘alcoholic’ and the social drinker (Room 2011) with moral values attached to each, negative connotations with the former and positive, socially acceptable values with the latter. Such moralisation of drinking practices, and in particular intoxication, is demonstrated not only in behaviour change interventions, but also in advertising campaigns of the alcohol industry promoting ‘responsible drinking’ thus placing the problem ‘with the use rather than the product’ (Wolburg 2005, p176). Furthermore research suggests that the alcohol industry has misrepresented evidence of risk using three strategies; denial or omission, distortion and distraction, thus misleading the public and policymakers regarding the risk of alcohol (Petticrew et al. 2017). Related to such misrepresentation public health information programmes emphasising responsibility are promoted, with weak evidence supporting their effectiveness (Hawkins et al. 2012). Indeed Babor et al. (2003) found little or no impact of these campaigns on population level alcohol use. Indeed Jayne et al (2012) have argued that the dominance of units in such campaigns is flawed. Their research showed that people chose to ignore units, with their use as a public health tool ‘far removed from the majority of people’s practices and experiences’ (Jayne, Valentine & Holloway 2012, p.838).
Such behaviour led intervention population strategies have been termed ‘superficial’, interventions that simply encourage individuals to change their behaviours (Rose 1992). Most importantly however is the lack of attention paid to health inequalities by such interventions. Behaviour change led approaches fail to appreciate how context within the risk environment, and vulnerability to such environments, interact to produce and reinforce health inequalities (Barnett et al. 2016). Within such interventions ‘responsibility’ has become the buzzword within a system that has been ‘built … around a relatively free availability of alcohol’ (Room, 2011, p. 147). Rhodes (2009) refers to this as ‘contingent causation’ with harm contingent upon social context and the interactions between the individual and the environment. Evidence however would suggest that such interventions can widen inequalities (Buck & Frosini 2012). Here is where alcohol harm poses a particular challenge. Whilst for other health behaviours we see the expected social gradient for consumption, mirrored by the social gradient in harm (e.g. for tobacco lower income groups are more likely to smoke and also more likely to die from smoking related illnesses) for alcohol lower socioeconomic groups report consuming the same or less on average than higher SES groups but suffer more from alcohol related harm when compared with higher SES groups (Lewer et al. 2016). This has become known as the Alcohol Harm Paradox. Several theories have been suggested including that lower SES groups have unique consumption patterns (e.g. more likely to binge drink), disproportionately underreport consumption, have a greater clustering of unhealthy behaviours (e.g. alcohol interacting with smoking and sedentary behaviour) and have poorer access to health care (Bellis et al. 2016). There has however been little focus on how social and material aspects of the broader structural risk environment play a role in shaping unequal drinking behaviours. Mennis et al. (2016) call for research that focuses on ‘inequities in risky substance use environments’ and the implications of this for disparities in related outcomes. Alcohol outlet density may play a role here in shaping particular consumption patterns amongst different income groups. In this paper we analyse four drinking outcomes to explore the association with density by income group for each outcome. An improved understanding of these contextual effects may help drive forward more radical population strategies that change the context in which the behaviours occur. Such ‘radical’ strategies would instead ‘aim to remove the underlying impediments to healthier behaviour, or to control the adverse pressures’ (Rose 1992), p. 100).
Applied to alcohol-related problems a more social determinants informed radical strategy would aim to change the underlying causes, the broader structural drivers of alcohol consumption, and in particular focus on reducing any inequalities in alcohol-related harm. Such radical population strategies may however compete with public values around personal freedom and self-control, nevertheless several countries have begun to pursue interventions regarding pricing and taxation, drink driving and marketing. Since 1999 devolution within the UK (the transfer of powers from central UK government to the regions of Scotland, Wales and Northern Ireland) has allowed Scotland to pass legislation, separate to the rest of the UK, on devolved issues such as health, education and social care. Whilst Scottish alcohol policy emerged from reforms to address problem drinkers and individual responsibility (Katikireddi et al., 2014), most recent attempts at reform has seen Scotland pursue world-leading radical population strategies, such as Minimum Unit Pricing, a reduced alcohol limit for drivers, a ban on multi-buy alcohol promotions and the inclusion of a licensing objective regarding ‘the protection and improvement of public health’ (Licensing Scotland Act, 2005).
Supply side: alcohol outlet density
One further potential area for reform is in the supply and availability of alcohol. Supply controls may be enacted by restricting the physical availability of alcohol, either by limiting opening hours, days of sale or through the location of retail outlets. Three theories have been posited to explain why the physical availability of alcohol may matter. The first theory, availability theory, consists of three possible stages as summarised by Livingston et al. (2007). Firstly, increased availability leads to increased consumption; secondly, as mean alcohol consumption increases so too do the number of heavy drinkers; and thirdly, heavy drinking is associated with adverse health and social outcomes, so as the number of heavy drinkers increases so too do these related problems. The second theory, market dynamics, refers to price competition and the notion that increased outlet density will increase the local competition between retailers, which will lead to price reductions and, in turn, increased levels of consumption. Previous research supporting this theory has shown that reduced price of alcohol is related to increased purchasing and consumption (Cook & Tauchen 1982). Analysis of the relationship between outlet density and price has shown that increased density of, in this case liquor stores, is associated with lower mean prices of alcohol (Treno et al. 2013). A third theory of social norms, proposes a more socio-structural effect at the neighbourhood level suggesting that individual drinking behaviour is shaped by attitudes, norms and behaviours of others in the neighbourhood. These collective norms may be shaped by outlet density and related marketing of products. In neighbourhoods of high density more frequent drinking behaviours may be observed and thus alcohol consumption is ‘normalised’ and such norms are established and perpetuated.
A large body of work has explored the relationship between alcohol outlet density (the concentration of outlets in a specific area), drinking behaviours and/or alcohol-related health outcomes. Research suggests an association between alcohol outlet density and increased levels of crime (Livingston 2008), domestic violence (Livingston 2011) and motor vehicle accidents (Cameron et al. 2012). Research also shows an association between alcohol outlet density, morbidity and mortality. Mortality from alcohol-related harm is higher in areas of highest density compared to areas of low density with evidence from the UK (Richardson et al. 2015), Canada (Stockwell et al. 2011) and Switzerland (Spoerri et al. 2013). Morbidity, including hospitalisations, emergency department visits and injuries have also been found to be higher in areas of highest alcohol outlet density (Cunradi et al. 2012; Morrison et al. 2015; Richardson et al. 2015).
Within research focussing on alcohol outlet density, the tendency has been to treat the population as a homogenous group and measure the effects of the risk environment on the population as a whole. Whilst some research has begun to explore measured differences by subgroups (Ayuka et al., 2014), to date there has been little research exploring the interaction between alcohol outlet density, socio-economic status and alcohol-related outcomes. Most statistical models adjust for individual level characteristics and therefore the results that we see present an environmental effect that has, to some extent, controlled for underlying individual differences. This is despite evidence demonstrating an increased density of alcohol outlets in areas of higher social deprivation (Ayuka et al. 2014; Shortt et al. 2015). This outlet concentration in areas of high deprivation leads us to return to questions of vulnerability and to ask whether such density may have the same affect on all income groups. A new perspective would then explore how individuals with particular characteristics (e.g. sex or low-income) interact with the alcohol environment in different ways, and consider the implications for consumption patterns.
Emerging from a call to consider both social structures and human agency (Jones & Moon 1993), health geographers have begun to demonstrate that “the impact of place is variable, depending on individual attributes” (Curtis & Jones 1998), p.651). If individuals are situated in places where certain ‘choices’ are constrained by the broader structures (and reinforced by those in power) then distinctions need to be made between life choices and life chances (Abel & Frohlich 2012). Life choices, the decisions people make, are embedded in life chances, the opportunities that people have. Such opportunities may be shaped by social situations that include those at the individual level (e.g. socio-economic position, income, gender) and those at the aggregate level (e.g. pollution, presence or absence of civic amenities). Life chances can therefore both enable, and constrain choices, with both neighbourhood and individual level factors interacting to produce outcomes. Such an approach helps to develop the health and place literature by integrating social justice through an exploration, not just of whether or not contextual health risks are distributed inequitably, but also for whom these environments are more risky. A recent review identified the need for health geographers to provide greater attention to those with the greatest need and the fewest resources available to enhance their lives in order to positively affect their health and wellbeing (Rosenberg 2016). In this paper we address the risk environment through a primary focus on the local supply and availability of alcohol products (captured using a measure of outlet density) and the relationship with the harmful use of alcohol. In particular we explore vulnerability through the interaction between individual level socio-economic position and environmental risk to assess differential social vulnerability to such environments. Here we detail our approach to this analysis.
Methods
In order to explore the susceptibility of different socio-demographic groups and the alcohol risk environment, measures of alcohol outlet density for local areas across Scotland were constructed and appended to data on 28,765 respondents from the Scottish Health Survey Series (SHeS) (combined years 2008-2011), designed to document trends in the nation’s health.
Alcohol outlet density (AOD) measures
The development of the AOD measures included three steps. Firstly, addresses and postcodes of all premises licensed to sell alcohol in 2012 (excluding temporary one off ‘party/festival’ licenses) were obtained from individual Scottish Liquor Licensing Boards (n = 32). These licenses were then divided into three categories; those licensed to sell alcohol for consumption on the premises (on-sales, n = 11,359), those licensed to sell alcohol for consumption off the premises (off-sales, n = 4,800) and finally a category containing all licenses (n = 15,159). Secondly, the locations of all outlets were mapped by postcode using ArcMap 10.1 geographic information system (GIS) software (23). Thirdly, kernel density estimation (KDE) was used to transform the locations into a density measure, separately for total, on-sale, and off-sale premises. The KDE technique required the definition of a cell size for the output density data (100m x 100m) and a search radius (we included three for sensitivity testing 400m, 800m, 1,000m). KDE transforms the point locations of premises to a smoothed continuous surface map which models the density of outlets for each cell. For each cell an assessment is made of the number and proximity of outlets within the specified radius. KDE includes a decay function meaning that outlets nearer the centre are given more weight than those closer to the edge. Postcodes were then overlaid on the map as a layer in ArcGIS. A spatial join then allocated the density value to each postcode based on spatial location on the grid. The result is a proximity-weighted estimate of the density of alcohol outlets (separately for total, on-sales and off-sales) per km2 for every postcode in Scotland (n = 152 400) (for more information on the method see (Shortt et al. 2016). Postcodes in Scotland have an average of 16 households and 36 residents. We report results for the 800m buffer, equivalent to a 10-minute walk for adults (King et al. 2012), as sensitivity analysis for the other buffers (800m and 1,000m) did not alter the results substantially. A more detailed description of the development of the three outlet density measures can be found elsewhere (Shortt et al. 2015).
The KDE-density values were categorised into five groups to minimise disclosure risk when linking these measures to the SHeS respondents. The first density category included all zero KDE-values. All remaining KDE-values above zero were grouped into equal quartiles. Based on their postcode of residence, these density categories were then linked to the SHeS respondents (n = 28,785). Due to small numbers of respondents in the zero-density category, this group was combined with the lowest density quartile. For subsequent analyses, this lowest outlet density category was used as the reference group. The postcodes of 20 respondents were uniquely identifiable, so they were excluded from subsequent analysis to protect confidentiality. The final linked dataset comprised 28,765 adults, for ethical and disclosure reasons any unique identifiers (including postcodes) were stripped from the data by the data holders before the linked dataset was returned to us.
Individual-level drinking outcomes
All individual-level drinking measures were derived from the SHeS. A detailed description of the SHeS methodology can be found elsewhere (Rutherford et al. 2013). The survey design was clustered collecting nationwide data from individuals living in private households randomly selected from address files within postcode sectors. Between 2008 - 2011 the survey was carried out annually, we combined the data for these years providing a large study sample enabling detailed analysis of population subgroups. The adult core-sample included all adults aged 16 and above (n = 28,765). All data from the core-sample was collected via personal interviewing.
Four widely used binary indicators of ‘high-risk’ drinking (as defined in the public health literature) were selected. These were based on a range of questions in the health survey that asked respondents to recount their drinking of various alcoholic beverages over the week prior to the interview. Based on this the number of units consumed over the 7 days could be calculated. The last variable refers to drinking experiences in the three months prior to interview. The variable ‘exceeding recommendations’ identified all respondents drinking above the weekly and/or daily recommended upper drinking limits (men = 21 units/week & 4 units/day; women = 14units/week & 3 units/day) (as defined at the time of this study, we recognise that the recommendations have since changed for men. 14 units is equivalent to six pints of average strength beer or ten small glasses of low strength wine). ‘Harmful drinking’ was chosen as an indicator of weekly excessive drinking (men 51+ units/week; women 36+ units/week), and ‘binge drinking’ as a measure of daily excessive drinking (men 8+ units/day; women 6+ units/day). ‘Problem drinking’ characterised the respondent’s relationship with alcohol using the CAGE questionnaire. This indicator is based on six variables including individual perceptions on the need to cut down, feeling ashamed, being annoyed by criticism about drinking, having shaky hands, drinking first thing in the morning, and being unable to stop drinking. Respondents were categorised as problem drinkers when they stated that they had experienced at least two of these drinking-related problems (Corbett et al. 2008).
Individual, household and area-level covariates
The SHeS includes a range of covariates known to be associated with alcohol consumption; individual (sex, age, religion, marital status, education); household (equivalized household income – adjusting income for household size and composition) and area-level (urban/rural status). We included each of these in our overall model. Equivalized household income was grouped into tertiles of: low (<£16 339), medium (£16 339–£31 707), high >£31 707) allowing sufficient numbers in each tertile to enable us to explore differences by income group. The Scottish Government urban/rural classification comprised primary cities (population >25,000), larger urban areas (population >10,000 and <25,000), small accessible and remote towns (population >3,000 and <10,000), as well as accessible and remote rural areas (population <3,000). Based on previous research, we know that there is as strong relationship between alcohol outlet density and area level deprivation in Scotland (Shortt et al. 2015), as we are controlling for individual level socioeconomic position we did not further control for area level deprivation, as argued elsewhere (Pearce et al. 2015).
Missing values and temporal coverage
Of the adult study sample included (n = 28, 765), 14 percent of the values were missing for household income (n=4164) and 13 percent of the values for problem drinking (n=3624). A smaller number of missing values were observed for some of the other variables included. In total 4178 cases were deleted resulting in n = 24,587 (the figure in table 1 differs slightly due to weighting). Excluding the missing values for age, gender, marital status, religion, urban/rural indicator resulted in proportional differences of <4.0 percent between the categories of the original and reduced sample. As the exclusion of the missing values did not change the composition of the sample considerably, we followed the example of previous research not to impute the missing values and report results based on the reduced sample (Carpenter & Kenward n.d.; Shortt et al. 2014; Vogl et al. 2012).
Table 1. Sample distributions and prevalence of high alcohol consumption, Scottish Health Survey 2008-2011.
| †nweighted | % of sample | †nweighted | % Exceeding recommendations | †nweighted | % Harmful drinking | †nweighted | % Binge drinking | †nweighted | % Problem drinking | |
|---|---|---|---|---|---|---|---|---|---|---|
| Sex | ||||||||||
| Male | 11,872 | 48.3 | 5,732 | 48.3 | 681 | 5.7 | 3,057 | 25.8 | 1,274 | 10.7 |
| Female | 12,686 | 51.7 | 4,947 | 39.0 | 428 | 3.4 | 2,159 | 17.0 | 830 | 6.5 |
| Total | 24,557 | 100.0 | 10,679 | 43.5 | 1,109 | 4.5 | 5,215 | 21.2 | 2,104 | 8.6 |
| Missing | 0 | 0.0 | 639 | 2.6 | 359 | 1.5 | 465 | 1.9 | 3,423 | 13.9 |
| Design-based F-statistic (p-value) | 71.5 | (p<0.01) | 25.0 | (p<0.01) | 83.5 | (p<0.01) | 84.4 | (p<0.01) | ||
| Age group | ||||||||||
| 16-24 | 3,362 | 13.7 | 1,445 | 43.0 | 256 | 7.6 | 964 | 28.7 | 444 | 13.2 |
| 25-34 | 3,912 | 15.9 | 1,990 | 50.9 | 148 | 3.8 | 1,173 | 30.0 | 497 | 12.7 |
| 35-44 | 4,512 | 18.4 | 2,257 | 50.0 | 207 | 4.6 | 1,185 | 26.3 | 405 | 9.0 |
| 45-54 | 4,546 | 18.5 | 2,297 | 50.5 | 228 | 5.0 | 1,093 | 24.1 | 397 | 8.7 |
| 55-64 | 3,752 | 15.3 | 1,598 | 42.6 | 154 | 4.1 | 579 | 15.4 | 238 | 6.3 |
| 65+ | 4,474 | 18.2 | 1,092 | 24.4 | 117 | 2.6 | 221 | 4.9 | 123 | 2.8 |
| Total | 24,557 | 100.0 | 10,679 | 43.5 | 1,109 | 4.5 | 5,215 | 21.2 | 2,104 | 8.6 |
| Missing | 0 | 0.0 | 639 | 2.6 | 359 | 1.5 | 465 | 1.9 | 3,423 | 13.9 |
| Design-based F-statistic (p-value) | 254.7 | (p<0.01) | 94.4 | (p<0.01) | 243.3 | (p<0.01) | 41.8 | (p<0.01) | ||
| Religion | ||||||||||
| None | 10,307 | 42.1 | 5,036 | 48.9 | 580 | 5.6 | 2,708 | 26.3 | 1,063 | 10.3 |
| Church of Scotland | 7,807 | 31.9 | 3,116 | 39.9 | 300 | 3.8 | 1,356 | 17.4 | 536 | 6.9 |
| Roman Catholic | 3,646 | 14.9 | 1,645 | 45.1 | 149 | 4.1 | 805 | 22.1 | 340 | 9.3 |
| Other Christian | 2,076 | 8.5 | 732 | 35.2 | 68 | 3.3 | 289 | 13.9 | 133 | 6.4 |
| Other | 635 | 2.6 | 137 | 21.6 | 11 | 1.7 | 47 | 7.4 | 29 | 4.6 |
| Total | 24,471 | 100.0 | 10,665 | 43.6 | 1,107 | 4.5 | 5,205 | 21.3 | 2,102 | 8.6 |
| Missing | 86 | 0.3 | 653 | 2.7 | 361 | 1.5 | 475 | 1.9 | 3,425 | 13.9 |
| Design-based F-statistic (p-value) | 100.9 | (p<0.01) | 110.9 | (p<0.01) | 107.4 | (p<0.01) | 30.8 | (p<0.01) | ||
| Marital status | ||||||||||
| Single | 5,601 | 22.8 | 2,465 | 44.0 | 404 | 7.2 | 1,565 | 28.0 | 777 | 13.9 |
| Married/living as married | 15,292 | 62.3 | 7,033 | 46.0 | 549 | 3.6 | 3,168 | 20.7 | 1,059 | 6.9 |
| Divorced/separated/dissolved civil partnership | 2,013 | 8.2 | 846 | 42.0 | 114 | 5.7 | 399 | 19.8 | 209 | 10.4 |
| Widowed/surviving partner | 1,645 | 6.7 | 335 | 20.4 | 42 | 2.6 | 83 | 5.0 | 59 | 3.6 |
| Total | 24,552 | 100.0 | 10,679 | 43.5 | 1,109 | 4.5 | 5,215 | 21.2 | 2,104 | 8.6 |
| Missing | 5 | <0.1 | 639 | 2.6 | 359 | 1.5 | 465 | 1.9 | 3,423 | 13.9 |
| Design-based F-statistic (p-value) | 194.7 | (p<0.01) | 81.7 | (p<0.01) | 145.3 | (p<0.01) | 41.7 | (p<0.01) | ||
| Highest educational qualification | ||||||||||
| Higher National Diploma or higher | 6,304 | 25.8 | 1,900 | 30.1 | 236 | 3.7 | 782 | 12.4 | 407 | 6.5 |
| Standard or higher grade | 9,125 | 37.3 | 4,221 | 46.3 | 549 | 6.0 | 2,359 | 25.9 | 963 | 10.6 |
| None or other school | 9,032 | 36.9 | 4,542 | 50.3 | 325 | 3.6 | 2,066 | 22.9 | 731 | 8.1 |
| Total | 24,461 | 100.0 | 10,663 | 43.6 | 1,109 | 4.5 | 5,207 | 21.3 | 2,101 | 8.6 |
| Missing | 96 | 0.4 | 655 | 2.7 | 359 | 1.5 | 474 | 1.9 | 3,426 | 13.9 |
| Design-based F-statistic (p-value) | 256.3 | (p<0.01) | 184.0 | (p<0.01) | 230.2 | (p<0.01) | 92.8 | (p<0.01) | ||
| Equalised household income group (tertiles) | ||||||||||
| 1 (<£16,339) | 7,783 | 31.7 | 2,578 | 33.1 | 392 | 5.0 | 1,293 | 16.6 | 759 | 9.8 |
| 2 (£16,339-£31,707) | 8,122 | 33.1 | 3,398 | 41.8 | 315 | 3.9 | 1,625 | 20.0 | 635 | 7.8 |
| 3 (>£31,707) | 8,652 | 35.2 | 4,703 | 54.4 | 403 | 4.7 | 2,297 | 26.6 | 710 | 8.2 |
| Total | 24,557 | 100.0 | 10,679 | 43.5 | 1,109 | 4.5 | 5,215 | 21.2 | 2,104 | 8.6 |
| Missing | 0 | 0.0 | 639 | 2.6 | 359 | 1.5 | 465 | 1.9 | 3,423 | 13.9 |
| Design-based F-statistic (p-value) | 95.3 | (p<0.01) | 7.1 | (p<0.01) | 30.8 | (p<0.01) | 51.0 | (p<0.01) | ||
| Urban/rural indicator‡ | ||||||||||
| Primary cities (population >125,000) | 9,283 | 37.8 | 4,228 | 45.6 | 422 | 4.6 | 2,186 | 23.6 | 922 | 15.0 |
| Urban (population >10,000 & ≤125,000) | 7,483 | 30.5 | 3,234 | 43.2 | 372 | 5.0 | 1,566 | 20.9 | 644 | 14.0 |
| Small accessible towns (population >3,000 & ≤10,000) | 2,270 | 9.2 | 926 | 40.8 | 101 | 4.4 | 457 | 20.1 | 181 | 13.6 |
| Small remote towns (population >3,000 & ≤10,000) | 854 | 3.5 | 338 | 39.6 | 44 | 5.1 | 172 | 20.2 | 60 | 13.1 |
| Accessible rural (population <3,000) | 3,041 | 12.4 | 1,316 | 43.3 | 112 | 3.7 | 593 | 19.5 | 209 | 12.2 |
| Remote rural (population <3,000) | 1,626 | 6.6 | 638 | 39.2 | 59 | 3.6 | 241 | 14.8 | 88 | 12.2 |
| Total | 24,557 | 100.0 | 10,679 | 43.5 | 1,109 | 4.5 | 5,215 | 21.2 | 2,104 | 8.6 |
| Missing | 0 | 0.0 | 639 | 2.6 | 359 | 1.5 | 465 | 1.9 | 3,423 | 13.9 |
| Design-based F-statistic (p-value) | - | - | 3.0 | (p<0.01) | 1.2 | (p=0.31) | 4.9 | (p<0.01) | 5.5 | (p<0.01) |
| Total alcohol outlet density | ||||||||||
| AOD 1 (lowest AOD, including areas with AOD = 0) | 7,775 | 31.7 | 3,382 | 43.5 | 313 | 4.0 | 1,543 | 19.8 | 560 | 7.2 |
| AOD 2 | 6,501 | 26.5 | 2,704 | 41.6 | 266 | 4.1 | 1,296 | 19.9 | 521 | 8.0 |
| AOD 3 | 5,932 | 24.2 | 2,538 | 42.8 | 278 | 4.7 | 1,280 | 21.6 | 547 | 9.2 |
| AOD 4 (highest AOD) | 4,349 | 17.7 | 2,055 | 47.3 | 252 | 5.8 | 1,096 | 25.2 | 476 | 11.0 |
| Total | 24,557 | 100.0 | 10,679 | 43.5 | 1,109 | 4.5 | 5,215 | 21.2 | 2,104 | 8.6 |
| Missing | 0 | 0.0 | 639 | 2.6 | 359 | 1.5 | 465 | 1.9 | 3,423 | 13.9 |
| Design-based F-statistic (p-value) | 3.3 | (p<0.01) | 2.2 | (p<0.05) | 4.9 | (p<0.01) | 7.3 | (p<0.01) | ||
| On-sale alcohol outlet density | ||||||||||
| AOD 1 (lowest AOD, including areas with AOD = 0) | 8,815 | 35.9 | 3,764 | 42.7 | 369 | 4.2 | 1,750 | 19.9 | 635 | 7.2 |
| AOD 2 | 6,170 | 25.1 | 2,582 | 41.8 | 247 | 4.0 | 1,244 | 20.2 | 540 | 8.8 |
| AOD 3 | 5,516 | 22.5 | 2,416 | 43.8 | 249 | 4.5 | 1,198 | 21.7 | 487 | 8.8 |
| AOD 4 (highest AOD) | 4,056 | 16.5 | 1,918 | 47.3 | 244 | 6.0 | 1,023 | 25.2 | 442 | 10.9 |
| Total | 24,557 | 100.0 | 10,679 | 43.5 | 1,109 | 4.5 | 5,215 | 21.2 | 2,104 | 8.6 |
| Missing | 0 | 0.0 | 639 | 2.6 | 359 | 1.5 | 465 | 1.9 | 3,423 | 13.9 |
| Design-based F-statistic (p-value) | - | - | 3.0 | (p<0.05) | 2.5 | (p<0.05) | 4.4 | (p<0.01) | 5.0 | (p<0.01) |
| Off-sale alcohol outlet density | ||||||||||
| AOD 1 (lowest AOD, including areas with AOD = 0) | 8,675 | 35.3 | 3,825 | 44.1 | 353 | 4.1 | 1,731 | 20.0 | 624 | 7.2 |
| AOD 2 | 5,834 | 23.8 | 2,432 | 41.7 | 246 | 4.2 | 1,185 | 20.3 | 489 | 8.4 |
| AOD 3 | 5,568 | 22.7 | 2,351 | 42.2 | 248 | 4.5 | 1,189 | 21.4 | 491 | 8.8 |
| AOD 4 (highest AOD) | 4,479 | 18.2 | 2,072 | 46.3 | 262 | 5.9 | 1,110 | 24.8 | 499 | 11.1 |
| Total | 24,557 | 100.0 | 10,679 | 43.5 | 1,109 | 4.5 | 5,215 | 21.2 | 2,104 | 8.6 |
| Missing | 0 | 0.0 | 639 | 2.6 | 359 | 1.5 | 465 | 1.9 | 3,423 | 13.9 |
| Design-based F-statistic (p-value) | - | - | 4.3 | (p<0.01) | 2.6 | (p<0.05) | 6.5 | (p<0.01) | 7.6 | (p<0.01) |
Totals & percentages weighted for non-response.
Accessible small towns and rural areas are within a 30-minute drive of a settlement of 10,000 or more. For remote small towns and rural areas the driving time exceeds 30 minutes.
There is the temporal mismatch between the outlet density measure (2012) and the health surveys used (2008-2011). The change in the number of licensed premises over a short time period is likely however to be relatively small. We have since collected data for 2016 showing the national level change between 2012 and 2016 to be 3 percent over the 4-year period.
Analysis
All statistical analysis was conducted in Stata/IC 12.1. We first used descriptive statistics to examine the univariate associations between the four drinking outcomes, the covariates and the three AOD measures. Second, we ran fully adjusted binary logistic regression models (applying the complex survey design function accounting for the clustered sampling design and weighting for non-response) separately for each of our four outcome variables to quantify the magnitude of associations between outlet densities (total, on-sale and off-sale) and different types of weekly and daily high-risk drinking. Additionally, we tested for trends in the associations between high-risk drinking and different outlet densities by modelling the four outlet density categories as continuous variables. We then calculated predicted probabilities of all outcome variables, respectively.
Finally, we ran fully adjusted interaction models to analyse whether the effect of AOD on individual-level drinking outcomes differed by equivalized household income group. The statistical significance of the interactions was assessed via a postestimation Wald test.
Results
In the week prior to data collection 43.5 percent of the respondents reported alcohol consumption ‘exceeding recommendations’, 4.5 percent reported ‘harmful’ drinking and 21.2 percent ‘binge’ drinking. In the three months prior to data collection 8.6 percent reported ‘problem drinking’. There was a clear gradient in the prevalence of ‘exceeding recommendations’ and ‘binge drinking’ across the income groups; compared to those in the lowest income group, those in the highest income group were most likely to report exceeding recommendation (33.1 percent v 51.4 percent) and more episodes of binge drinking (16.6 percent v 26.6 percent). Those in the lowest income group were most likely to report ‘harmful drinking’ and ‘problem drinking’ although the trend observed was less clear (Table 1).
The relationships between drinking outcomes and AOD were also as expected. For all drinking variables, we observed a positive trend, indicating that that higher outlet density was associated with increased probabilities of high-risk drinking (Table 1). For all outcomes, across all categories of outlet density (total, on-sales and off sales) we observed the expected gradient; higher reporting in areas of highest density. For total outlet density, ‘exceeding recommendations’ increased from 43.5 percent to 47.3 percent (p <0.01), ‘harmful drinking’ increases from 4.0 percent to 5.8 percent (p <0.05), ‘binge drinking’ increases from 19.8 percent to 25.2 percent (p <0.01) and ‘problem drinking’ increases from 7.2 percent to 11.0 percent (p <0.01).
Multivariate models
Results from the fully adjusted models (adjusted for age, sex, religion, marital status, household income, education, neighbourhood urban/rural status) are presented in Table 2. The table presents the predicted probabilities of all four outcomes in relation to AOD for each category of outlet type. For total outlet density, we observe a positive gradient in the probability of reporting all outcome variables. Compared to those living in areas of low density, in areas of highest density we see the probabilities of reporting exceeding recommendations increase by 4 percent, of harmful drinking increase by 1 percent, of binge drinking by 3 percent and of problem drinking by 2 percent. All of these results reached statistical significance and all trends are positive and significant. These results are reflected in on-sale outlet density with exceeding recommendations increasing by 5 percent in areas of highest density, harmful drinking by 1 percent, binge drinking by 4 percent and problem drinking by 2 percent. Again, all reach statistical significance with significance positive trends. Results for off-sales are weaker with only harmful drinking and binge drinking showing significant increase (1 percent and 2 percent respectively) and only binge drinking showing significant trend across the density groups
Table 2. Summary non-stratified fully adjusted models‡.
| Exceeding recommendations | Harmful drinking | Binge drinking | Problem drinking | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 95% CI | 95% CI | 95% CI | 95% CI | |||||||||
| dy/dx† | lower | upper | dy/dx† | lower | upper | dy/dx† | lower | upper | dy/dx† | lower | upper | |
| Total alcohol outlet density (AOD) | ||||||||||||
| 1 (lowest, including areas with AOD = 0) [reference group] | ||||||||||||
| 2 | 0.00 | -0.02 | 0.02 | 0.00 | -0.01 | 0.01 | 0.00 | -0.02 | 0.02 | 0.00 | -0.01 | 0.02 |
| 3 | 0.02 | -0.01 | 0.04 | 0.00 | -0.01 | 0.02 | 0.02 | 0.00 | 0.04 | 0.01 | 0.00 | 0.03 |
| 4 (highest AOD) | 0.04 | 0.01 | 0.06 | 0.01 | 0.00 | 0.03 | 0.03 | 0.01 | 0.05 | 0.02 | 0.00 | 0.03 |
| Trend | 0.01 | 0.01 | 0.02 | 0.00 | 0.00 | 0.01 | 0.01 | 0.00 | 0.02 | 0.01 | 0.00 | 0.01 |
| On-sale alcohol outlet density (AOD) | ||||||||||||
| 1 (lowest, including areas with AOD = 0) [reference group] | ||||||||||||
| 2 | 0.01 | -0.01 | 0.03 | 0.00 | -0.01 | 0.01 | 0.01 | -0.01 | 0.02 | 0.02 | 0.00 | 0.03 |
| 3 | 0.02 | 0.00 | 0.04 | 0.00 | -0.01 | 0.01 | 0.02 | 0.00 | 0.04 | 0.01 | 0.00 | 0.03 |
| 4 (highest AOD) | 0.05 | 0.02 | 0.07 | 0.01 | 0.00 | 0.03 | 0.04 | 0.01 | 0.06 | 0.02 | 0.01 | 0.04 |
| Trend | 0.01 | 0.01 | 0.02 | 0.00 | 0.00 | 0.01 | 0.01 | 0.01 | 0.02 | 0.01 | 0.00 | 0.01 |
| Off-sale alcohol outlet density (AOD) | ||||||||||||
| 1 (lowest, including areas with AOD = 0) [reference group] | ||||||||||||
| 2 | -0.01 | -0.03 | 0.01 | 0.00 | -0.01 | 0.01 | 0.00 | -0.02 | 0.02 | 0.00 | -0.01 | 0.02 |
| 3 | 0.01 | -0.02 | 0.03 | 0.00 | -0.01 | 0.01 | 0.01 | -0.01 | 0.03 | 0.00 | -0.01 | 0.02 |
| 4 (highest AOD) | 0.02 | 0.00 | 0.05 | 0.01 | 0.00 | 0.02 | 0.02 | 0.00 | 0.04 | 0.01 | 0.00 | 0.03 |
| Trend | 0.01 | 0.00 | 0.02 | 0.00 | 0.00 | 0.01 | 0.01 | 0.00 | 0.01 | 0.00 | 0.00 | 0.01 |
p < 0.01; p < 0.05
Adjusted for age, sex, religion, marital status, household income, education, neighbourhood urban/rural status
Interaction models
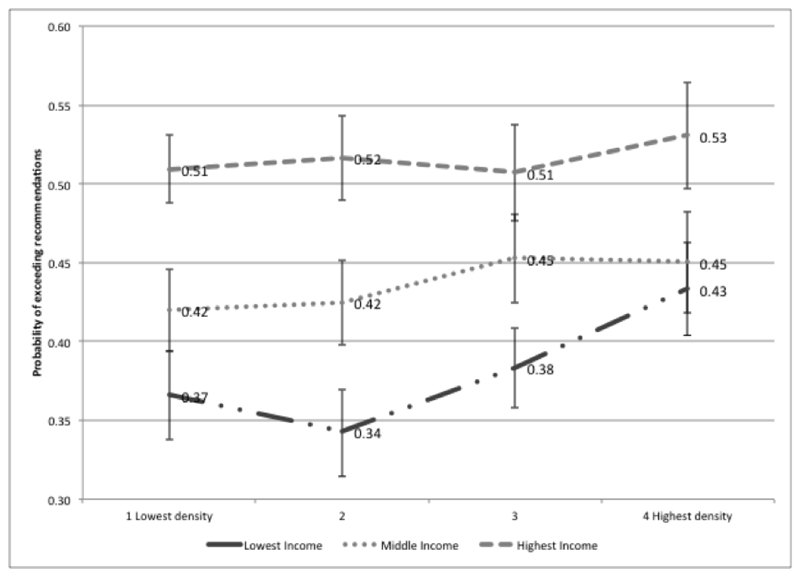
To explore whether each income group was equally affected by outlet density across our four outcomes, we examined the interactions between AOD and our outcomes, stratified by tertiles of household income (Figures 1 to 4). As there are four outcomes across three outlet density categories (total sales, on-sales and off-sales) we present the results for total outlet density and where they differ for either on-sales or off-sales we note this. Significant results are those for which the 95 percent confidence intervals do not overlap.
Exceeding recommendations
Across all AOD categories the highest income groups are most likely to exceed recommendations. The probability of exceeding recommendations increases for all income groups with increasing AOD (Figure 1). Most of the differences between the income groups reach statistical significance (95 percent confidence intervals [CIs] do not overlap). It is, however, clear that those in the lowest income tertile are most strongly affected by outlet density for this outcome. The probability of exceeding recommendations rose from 36.6 percent for the lowest income tertile in areas of lowest density to 43.3 percent in areas of highest density, a significant increase of 6.7 percent compared to 3.1 percent increase in the mid tertile and a 2.1 percent increase in the highest income tertile (both non-significant). Whilst the gap between the lowest and highest income tertiles reduces from 14.3 percent in the lowest density areas to 9.7 percent in the highest density areas, this is largely due to the sharp increase in those in the lowest income tertile exceeding recommendations rather than a reduction in any income tertile. Postestimation Wald tests were significant (p < 0.05).
Figure 1.
Adjusteda interactive effects of total alcohol outlet density (AOD)b on individual-level reporting of exceeding recommendationsc by household income, Scottish Health Survey 2008-2011 (nweighted = 24,116).
Note: amodel includes design variables (to account for sample stratification and nonresponse), alcohol outlet density and equalised household income, controlling for sex, age, religion, marital status, education and neighbourhood urban/rural status. bAOD 1: median of kernel density estimation values (KDE) = 0,6/km2; AOD 2: median KDE = 3,8/km2; AOD 3: median KDE = 7,5/km2; AOD 4: median KDE = 23,4/km2; cReference group: respondents not exceeding the drinking recommendations.
Considering AOD subcategories, a similar pattern is reflected for on-sales and off-sales where there is a clear positive gradient in the risk of exceeding recommended consumption as AOD rises across all of the income tertiles, and again the gradient is steepest for the lowest income tertile.
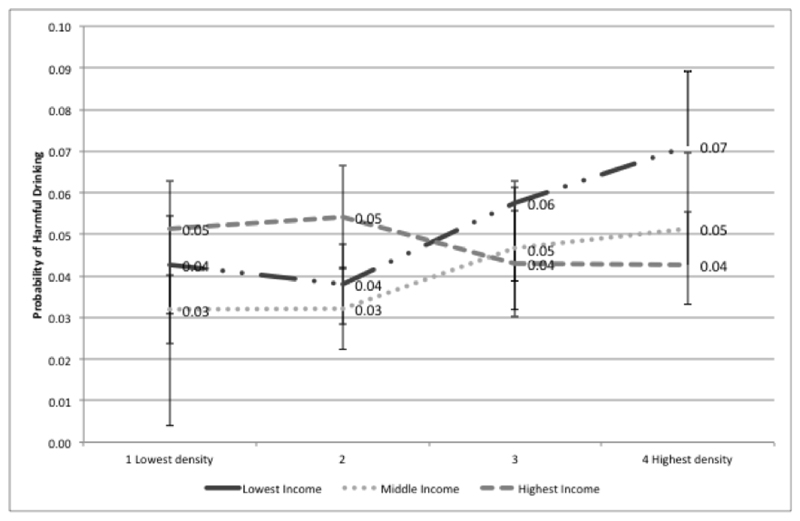
Harmful drinking
As with exceeding recommendations, Figure 2 shows that the largest increase in the predicted probabilities of harmful drinking are seen in the lowest income tertile. For the highest income tertile there is a non-significant reduction in the probability of harmful drinking, falling from 5.1 percent in areas of lowest density to 4.3 percent in areas of highest density. Conversely for the lowest income tertile this rises from 4.3 percent in the lowest density group to 7.1 percent in the highest density group (though this is non-significant).
Figure 2.
Adjusted interactive effects of total alcohol outlet density (AOD) on individual-level reporting of harmful drinkingc by household income, Scottish Health Survey 2008-2011 (nweighted = 24,279).
Adjustments and AOD ranges as per Figure 1. Reference group: those not reporting harmful drinking.
Again, the pattern is broadly similar for other density categories. For on-sales the probability of harmful drinking rises for the lowest income tertile (4.1 percent to 7.7 percent, significant) and falls for the highest income tertile (5.2 percent to 4.2 percent non-significant). For off-sales once again the probability rises for the lowest income tertile (3.5 percent to 6.9 percent significant) and falls for the highest income tertile (5.7 percent to 4.4 percent, non-significant). Again, all postestimation Wald tests were significant (p = < 0.05).
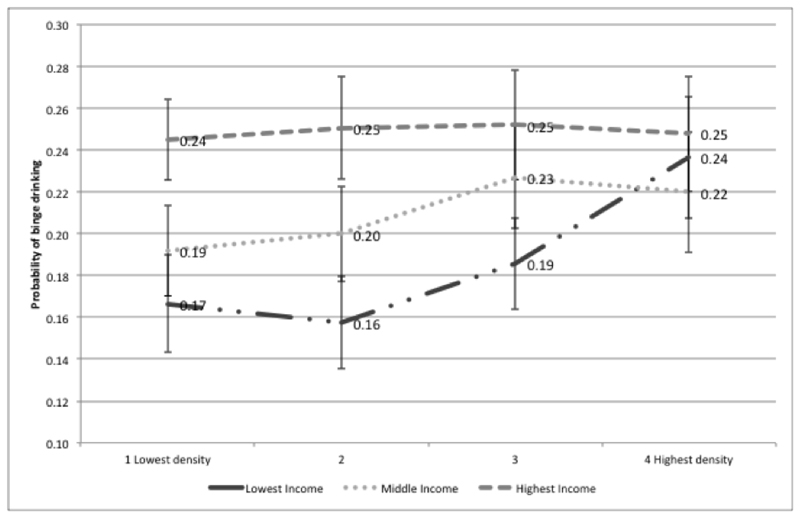
Binge drinking
The probability of binge drinking increases significantly across total outlet density groups for the lowest income tertile (17 percent to 24 percent) but remains relatively static for the highest income tertile (24 percent to 25 percent). For on-sales and off-sales the patterns are similar, the probability of binge drinking in the lowest income tertile rises significantly from 15 percent in the lowest density group to 23 percent in the highest density group for on sales and from 18 percent to 23 percent for off-sales with little or no change in the highest income tertile. Postestimation Wald tests were significant (p = < 0.05).
Figure 3.
Adjusted interactive effects of total alcohol outlet density (AOD) on individual-level reporting of binge drinkingc by household income, Scottish Health Survey 2008-2011 (nweighted = 24,237).
Adjustments and AOD ranges as per Figure 1. Reference group: respondents not reporting binge drinking.
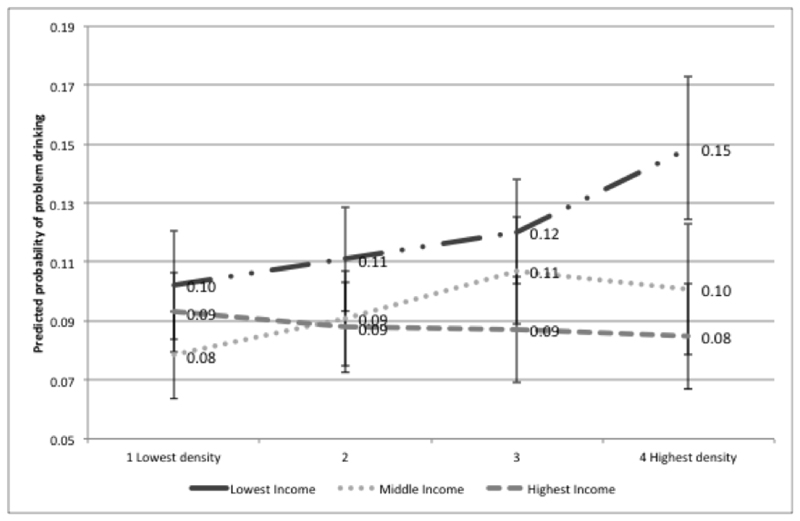
Problem drinking
Unlike the other outcomes, the probability of problem drinking is highest for those in the lowest income tertile across all total density groups. For the lowest income group the probability of problem drinking rises significantly from 10 percent to 15 percent. For the highest income tertile we see a non-significant fall (9 percent to 8 percent). Both the on-sales and off-sales patterns reflect the total sales pattern. For off-sales the predicted probability for the lowest income tertile in the highest density group (15 percent) is almost double that of the highest income tertile in the highest density group (8 percent). Postestimation Wald tests were significant (p = < 0.05).
Figure 4.
Adjusteda interactive effects of total alcohol outlet density (AOD)b on individual-level reporting of problem drinking c by household income, Scottish Health Survey 2008-2011 (nweighted = 20,914).
Adjustments and AOD ranges as per Figure 1. Reference group: respondents not reporting problem drinking.
Discussion
In this paper we examined the alcohol risk environment. In particular, we examined whether those living in neighbourhoods of high alcohol outlet density exhibit different patterns of alcohol consumption compared to those in areas of low alcohol outlet density. We also explored whether or not the risk environment shapes consumption patterns equally amongst all socioeconomic groups. We focussed on four drinking behaviours; ‘exceeding recommendations’, ‘harmful’ drinking, ‘binge’ drinking and ‘problem’ drinking. In univariate analysis we found that the probability of reporting such behaviours increases with increased outlet density. In fully adjusted models this increase remained for all outcomes, with increasing density of both total and on-sales outlets and for harmful drinking and binge drinking with increasing density of off-sales outlets. These findings suggest that alcohol outlet density is associated with greater probability of reporting episodes of heavier drinking or problem drinking.
To explore whether or not all income groups were equally affected by outlet density we examined the interactions between outlet density and household income tertiles across all four outcomes. We found evidence that those in the highest income groups are more likely to report binge drinking or exceeding recommendations in all density categories. Those in the lowest income groups were more likely to report problem drinking across all density categories. For harmful drinking there was a different pattern between the density categories with probability highest for the highest income group for areas of low density and highest for the lowest income group in areas of highest density. However, when we explore the impact of increasing alcohol outlet density on drinking outcomes by income group we see different results for high-income and low-income groups. For those in the highest income group the probability of all outcomes remained relatively static as density increased. However, for those in the lowest income group outlet density mattered with the probability of all outcomes rising as density increased (significant for exceeding recommendations, binge drinking and problem drinking). In particular, in the highest density neighbourhoods those on the lowest incomes have the highest levels of harmful drinking and problem drinking. These results suggest that lower income groups may be disproportionately affected by outlet density.
Evidence points to the features of the risk environment having an influence on health, health behaviours and health inequalities. It is clear that risk environments may not affect us all equally and that there may be socially differentiated vulnerability to such environments. In alcohol research there is limited evidence on how place-based influences may differ between different sociodemographic groups. This research addresses that in an original approach and extends previous work that explored the differential impact of the alcohol environment on gender, age and ethnicity (Ayuka et al 2014). In a significant addition to the literature we have shown that low-income respondents are more vulnerable to alcohol outlet density than higher income groups. There are many possible reasons for this including mobility constraints and daily patterns of movement. Using data from the Whitehall study of British civil servants, Stafford and Marmot (2003) have argued that the impact of neighbourhood deprivation is greater for those in lower socioeconomic positions. Further research has shown that lower socio economic groups may spend more time in their local neighbourhoods (Forrest & Kearns 2001), tend to walk around their neighbourhoods more (Macintyre & Ellaway 1998), travel shorter distances on a daily basis (Morency et al. 2011), be more reliant on resources in their local vicinity (Ivory et al. 2015) and that their health ‘choices’ may be more readily influenced by the environments in which they live (Shortt et al., 2014). As a result those from lower socioeconomic groups may be more constrained, and indeed bounded by, their environments and thus more vulnerable to the risks presented. Furthermore, those in lower income groups may see alcohol as a coping mechanism for psychological distress (Mulia et al. 2008) and an increased availability of alcohol may contribute. Individuals of differing social groups may therefore be both differentially exposed to risk environments by type, but also differentially reliant on their own residential environments in a temporal sense – a double burden of low income and risk environments. Linked to Max Weber’s notions of ‘life chances’ residential neighbourhoods can therefore be seen as spaces that constrain or enable choices, with individual circumstances, in this case socio-economic status, interacting with context (alcohol outlet density) to affect behaviour and health outcomes.
This convergence of low socio-economic position, the risk environment and vulnerability is troubling, given the persistent health inequalities in Scotland and evidence of the alcohol harm paradox. These results suggest that behaviour-led interventions that ignore the broader context in which behaviours take place, are unlikely to make substantial improvements to population health or reduce inequalities. Drawing upon tobacco control research we know that such ‘downstream’ policies, such as media campaigns, risk increasing social inequalities (Hill et al. 2014). Instead, as highlighted by Rose (1992), radical policies are required, policies that address inequalities; both the drivers of unequal risk environments and the social, political and economic drivers of persistent poverty.
Whilst considering structural change we must also consider the broader drivers of risk environments and in particular manufactured risk. The risk environments explored in this paper are shaped by wider economic and social determinants. Adapting the analogy of a ‘vector’, Gilmore et al. (2011) identify the role of the host (the consumer), agent (the product, in this case alcohol), the environment (e.g. density) and the disease vector (the corporations) in shaping the risk environment. This analogy has been used effectively in tobacco control, leading to a concerted effort to explore and restrain corporate influence (e.g. Article 5.3 of the Framework Convention on Tobacco Control). Despite claims regarding ‘tobacco exceptionalism’, arguments can also be made with respect to alcohol availability contributing towards the risk environment for alcohol consumption. Here we concur with Gilmore et al. (2011) who argue that Big Alcohol (and Big Food) act in similar ways to Big Tobacco (e.g. privatising risk and focussing on personal responsibility, individual liberty and self-regulation) making it more difficult to enact effective, ‘radical’, health policies concerning availability and supply.
Our research has some limitations. First, our database of alcohol outlets allowed us to distinguish between on-sales and off-sales premises and to group these into a measure for total outlet density. Whilst this allowed us to test for differences between on-sales and off-sales the measure itself could be seen as rather crude. The category of on-sales includes all premises that are licenced to sell alcohol for consumption on the premises. Such premises range from restaurants to pubs, bars and large vertical drinking establishments (such as a club with 4 floors and a bar on each floor). We have no information on size of premises, opening hours or nature of the establishment. To date the majority of the research in this area has explored differences between on-sales and off-sales outlet density but there has been little, if any, exploration of the association between type of on-sales premise, alcohol related harm and drinking behaviours. In contrast research exploring assault and alcohol outlet density has assessed whether or not all types of licensed premises are equal contributors, concluding that hotels and nightclubs (Briscoe & Donnell 2003) brand bars and off-sales (Gruenewald & Remer, 2006) were the most problematic premises. Future work could explore how distinction by premise type is related to consumption patterns. Second, our analysis was cross-sectional, measured at one point in time. As such we can report only associations and whilst we can infer causation, we cannot prove it. In order to determine whether or not there is a causative pathway we would need, at the very least, to explore these results over time and utilise change in the alcohol environment as a ‘natural experiment’. We intend to do this in a future programme of work. Third, there may be an element of underrepresentation of alcohol consumption in the health survey, both through underreporting of alcohol consumption and under-representation of groups associated with heavy drinking (men, younger population and those from more deprived groups) (Gray et al. 2013). As such we may be understating the strength of the association between outlet density and drinking behaviours, particularly in relation to off-sales where low prices may promote excessive drinking (Pattoni et al. 2007) and where previous research has found strongest associations between off-sales density and alcohol related harm (Richardson et al., 2014). Finally, our research explored the individual’s home environment. We know that individuals move between neighbourhoods and future analysis could also include non-residential environments (Perchoux et al. 2013).
Reducing alcohol related harm is a key goal in public health but has been described as a ‘wicked issue’ that requires complex solutions (Hunter 2009). Any privatisation of risk will inevitably lead to a focus on lifestyle change and given that it has been argued that our level of societal acceptability for alcohol risk is high, it is particularly difficult to shift the neoliberal rhetoric from individual blame to societal responsibility. Whilst such a shift towards more radical interventions may be apparent in some national contexts, Scotland as an example, there are many others who continue to argue the case for personal responsibility. In this paper however we have challenged the notion of personal responsibility by showing that the environment matters and that the alcohol environment has a differential effect upon social groups, potentially contributing to socioeconomic inequalities in health outcomes. Inevitably this then begs the question ‘for whom does the environment matter?’ (Forest and Kearns, 2001, p2136).
Neighbourhoods, as opportunity structures (Macintyre et al. 2002), may be more or less conducive to health but there are policy options to shape and change the risk environment. In the ‘Global Strategy to Reduce the Harmful Use of Alcohol’ the World Health Organisation identify 10 recommended target areas for policy options and interventions (WHO 2010). The more radical strategies, those that aim to change the context in which drinking behaviours are shaped, include action on the availability of alcohol, the marketing of alcohol and the price of alcohol. Scotland has just become the first country in the world to establish Minimum Unit Pricing. Such a radical move, after a hard fought battle through the courts, should be applauded. Price however is not a magic bullet and will not solve all alcohol related problems immediately. Further interventions, at a population level, require us to consider the places in which alcohol is consumed and in which health related outcomes are realised. The interaction between place and behaviour, and importantly household income, is critical and as such the vectors of these risk environments need to be challenged.
Acknowledgements
Many thanks to colleagues who commented on earlier drafts including Catherine Tisch, Elizabeth Richardson, Helena Tunstall, Tom Clemens and Mark Cherrie. Thanks also to Julie Landsberg and other SHeS personnel. This work was supported by the Scottish Collaboration for Public Health Research and Policy and the European Resarch Council (ERC-2010-StG Grant 263501). Richard Mitchell’s contribution was also funded by the UK Medical Research Council as part of the Neighbourhoods and Communities Programme (MC_UU_12017-10).
Biographies
Author professional/contact information
Niamh K Shortt is a Reader in human geography and co-director of the Centre for Research on Environment, Society & Health in the School of GeoSciences, University of Edinburgh, EH8 9XP, United Kingdom. Email: niamh.shortt@ed.ac.uk Her research interests include exploring the relationship between health behaviours, the environment and health inequalities.
ESTHER RIND is a researcher and project manager at the Institute of Occupational and Social Medicine & Health Services Research, University Hospital Tuebingen, Wilhelmstr. 27, 72074 Tuebingen., Germany. E-mail: esther.rind@med.uni-tuebingen.de. Her research interests include the study of health behaviours & health inequalities and the prevention of mental distress for personnel working in the health care system.
Jamie Pearce is Professor of Heath Geography and co-Director of the Centre for Research on Environment, Society & Health in the School of GeoSciences, University of Edinburgh, EH8 9XP, United Kingdom. Email: jamie.pearce@ed.ac.uk His research interests include geographical explanations for health inequalities and behaviours including the consumption of tobacco and alcohol.
RICHARD MITCHELL is Professor of Health and Environment, and leads the Neighbourhoods and Communities research programme, at the MRC/CSO Social and Public Health Sciences Unit, University of Glasgow, G2 3QB. He is also a co-Director of the Centre for Research on Environment, Society & Health Email: Richard.Mitchell@glasgow.ac.uk. His research interests include how social and physical environment can protect health and narrow health inequalities, the health impacts of natural environments, and the application of complex systems approaches to these topics.
Professor Sarah Curtis is Honorary Professor, University of Edinburgh and Professor Emeritus, Durham University, UK. Email: s.e.curtis@durham.ac.uk. She specialises in geographies of health and health care.
Contributor Information
Niamh K Shortt, Centre for Research on Environment, Society and Health, School of Geosciences, University of Edinburgh, Drummond Street, Edinburgh, UK, EH8 9XP.
Esther Rind, Institute of Occupational and Social Medicine & Health Services Research, University Hospital Tuebingen, Tuebingen, Germany.
Jamie Pearce, Centre for Research on Environment, Society and Health, School of Geosciences, University of Edinburgh, Drummond Street, Edinburgh, UK, EH8 9XP.
Richard Mitchell, MRC/CSO Social & Public Health Sciences Unit, Institute of Health and Wellbeing, University of Glasgow, Glasgow, UK, G2 3QB.
Sarah Curtis, Department of Geography, Durham University, Durham, UK, DH1 3LE.
References
- Abel T, Frohlich KL. Capitals and capabilities: Linking structure and agency to reduce health inequalities. Social Science and Medicine. 2012;74(2):236–244. doi: 10.1016/j.socscimed.2011.10.028. [DOI] [PubMed] [Google Scholar]
- Angus C, et al. Estimating the cost-effectiveness of brief interventions for heavy drinking in primary health care across Europe. European Journal of Public Health. 2017;27(2):345–351. doi: 10.1093/eurpub/ckw122. [DOI] [PubMed] [Google Scholar]
- Ayuka F, Barnett R, Pearce J. Neighbourhood availability of alcohol outlets and hazardous alcohol consumption in New Zealand. Health & Place. 2014;29:186–199. doi: 10.1016/j.healthplace.2014.07.002. //www.sciencedirect.com/science/article/pii/S135382921400094X. [DOI] [PubMed] [Google Scholar]
- Babor TF. Alcohol: No Ordinary Commodity—Research and Public Policy. O. U. Press; Oxford: 2003. [Google Scholar]
- Babor TF, Robaina K. Public Health, Academic Medicine, and the Alcohol Industry’s Corporate Social Responsibility Activities. American Journal of Public Health. 2013;103(2):206–214. doi: 10.2105/AJPH.2012.300847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett R, et al. Smoking Geographies: Space, place and Tobacco. London: Wiley-Blackwell; 2016. [Google Scholar]
- Beck U. Risk Society. London: Sage; 1992. [Google Scholar]
- Beckingham D. Gender, space, and drunkenness: Liverpool’s licensed premises, 1860–1914. Annals of the Association of American Geographers. 2012;102(3):647–666. [Google Scholar]
- Bellis MA, et al. The alcohol harm paradox: using a national survey to explore how alcohol may disproportionately impact health in deprived individuals. BMC Public Health. 2016;16(1):111. doi: 10.1186/s12889-016-2766-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briscoe S, Donnell N. Problematic Licensed Premises for Assault in Inner Sydney, Newcastle and Wollongong. Australian & New Zealand Journal of Criminology. 2003;36(1):18–33. doi: 10.1375/acri.36.1.18. [DOI] [Google Scholar]
- Buck D, Frosini F. Clustering of unhealthy behaviours over time - Implications for policy and practice. The Kings Fund. 2012:1–24. Available at: www.kingsfund.org.uk. [Google Scholar]
- Cameron MP, et al. Alcohol outlet density is related to police events and motor vehicle accidents in Manukau City, New Zealand. Australian and New Zealand journal of public health. 2012;36(6):537–542. doi: 10.1111/j.1753-6405.2012.00935.x. [DOI] [PubMed] [Google Scholar]
- Carpenter J, Kenward M. Guidelines for handling missing data in Social Science Research [Google Scholar]
- Cook PJ, Tauchen G. The Effect of Liquor Taxes on Heavy Drinking. The Bell Journal of Economics. 1982;13(2):379–390. Available at: http://www.jstor.org/stable/3003461. [Google Scholar]
- Corbett J, et al. The Scottish Health Survey 2008 - Volume 1: Main Report. Edinburgh: Scottish Government; 2008. [Google Scholar]
- Cunradi CB, et al. Alcohol Outlet Density and Intimate Partner Violence-Related Emergency Department Visits. Alcoholism: Clinical and Experimental Research. 2012;36(5):847–853. doi: 10.1111/j.1530-0277.2011.01683.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curtis S, Jones IR. Is there a place for geography in the analysis of health inequality? Socioloy of Health & Illness. 1998;20(5):645–672. doi: 10.1111/1467-9566.00123. [DOI] [Google Scholar]
- Demant J, Landolt S. Youth Drinking in Public Places: The Production of Drinking Spaces in and Outside Nightlife Areas. Urban Studies. 2013;51(1):170–184. doi: 10.1177/0042098013484532. [DOI] [Google Scholar]
- Forrest R, Kearns A. Social Cohesion, Social Capital and the Neighbourhood. Urban Studies. 2001;38(12):2125–2143. doi: 10.1080/00420980120087081. [DOI] [Google Scholar]
- Gabe J. Health, medicine and risk: the need for a sociological approach. In: Gabe J, editor. Medicine Health and Risk: Scoiological Approaches. Oxford: Blackwell; 1995. [Google Scholar]
- Giddens A. Risk and Responsibility. The Modern Law Review. 1999;62(1):1–10. doi: 10.1111/1468-2230.00188. [DOI] [Google Scholar]
- Gilmore AB, Savell E, Collin J. Public health, corporations and the New Responsibility Deal: promoting partnerships with vectors of disease? Journal of Public Health. 2011;33(1):2–4. doi: 10.1093/pubmed/fdr008. [DOI] [PubMed] [Google Scholar]
- Glasgow S, Schrecker T. The double burden of neoliberalism? Noncommunicable disease policies and the global political economy of risk. Health & Place. 2016;39:204–211. doi: 10.1016/j.healthplace.2016.04.003. Available at: http://www.sciencedirect.com/science/article/pii/S1353829216300211. [DOI] [PubMed] [Google Scholar]
- Gray L, et al. Use of record-linkage to handle non-response and improve alcohol consumption estimates in health survey data: a study protocol. BMJ Open. 2013;3(3) doi: 10.1136/bmjopen-2013-002647. Available at: http://bmjopen.bmj.com/content/3/3/e002647.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins B, Holden C, McCambridge J. Alcohol industry influence on UK alcohol policy: A new research agenda for public health. Critical Public Health. 2012;22(3):297–305. doi: 10.1080/09581596.2012.658027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrick C. Governing Health and Consumption: Sensible Citizens, Behaviour and the City. Bristol: The Policy Press; 2011. [Google Scholar]
- Hill S, et al. Impact of tobacco control interventions on socioeconomic inequalities in smoking: review of the evidence. Tobacco Control. 2014;23(e2):e89–LP-e97. doi: 10.1136/tobaccocontrol-2013-051110. Available at: http://tobaccocontrol.bmj.com/content/23/e2/e89.abstract. [DOI] [PubMed] [Google Scholar]
- Hunter DJ. Leading for Health and Wellbeing: the need for a new paradigm. Journal of Public Health. 2009;31(2):202–204. doi: 10.1093/pubmed/fdp036. [DOI] [PubMed] [Google Scholar]
- Ivory VC, et al. Social Science & Medicine Could strength of exposure to the residential neighbourhood modify associations between walkability and physical activity? 2015;147:232–241. doi: 10.1016/j.socscimed.2015.10.053. [DOI] [PubMed] [Google Scholar]
- Jayne M, Valentine G, Gould M. Family life and alcohol consumption: The transmission of “public” and “private” drinking cultures. Drugs: Education, Prevention and Policy. 2012;19(3):192–200. doi: 10.3109/09687637.2011.640720. [DOI] [Google Scholar]
- Jayne M, Valentine G, Holloway SL. Alcohol, drinking, drunkeness:(Dis) orderly spaces. Ashgate Publishing, Ltd; 2011. [Google Scholar]
- Jayne M, Valentine G, Holloway SL. What Use Are Units? Critical Geographies of Alcohol Policy. 44(3):828–846. [Google Scholar]
- Jayne M, Valentine G, Holloway SL. What Use Are Units? Critical Geographies of Alcohol Policy. Antipode. 2012;44(3):828–846. doi: 10.1111/j.146-8330.2011.00927.x. [DOI] [Google Scholar]
- Jones K, Moon G. Medical geography: taking space seriously. Progress in human geography. 1993;17(4):515–524. [Google Scholar]
- King TL, et al. Does parkland influence walking? The relationship between area of parkland and walking trips in Melbourne, Australia. International Journal of Behavioral Nutrition and Physical Activity. 2012 Sep 19;9(115) doi: 10.1186/1479-5868-9-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewer D, et al. Unravelling the alcohol harm paradox: a population-based study of social gradients across very heavy drinking thresholds. BMC Public Health. 2016;16(1):599. doi: 10.1186/s12889-016-3265-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livingston M. A longitudinal analysis of alcohol outlet density and domestic violence. Addiction (Abingdon, England) 2011;106(5):919–925. doi: 10.1111/j.1360-0443.2010.03333.x. [DOI] [PubMed] [Google Scholar]
- Livingston M. Alcohol outlet density and assault: A spatial analysis. Addiction. 2008;103:619–628. doi: 10.1111/j.1360-0443.2008.02136.x. [DOI] [PubMed] [Google Scholar]
- Livingston M, et al. Changing the density of alcohol outlets to reduce alcohol-related problems. Drug and alcohol review. 2007;26(5):557–566. doi: 10.1080/09595230701499191. [DOI] [PubMed] [Google Scholar]
- Lupton D. Risk as Moral Danger: The Social and Political Functions of Risk Discourse in Public Health. International Journal of Health Services. 1993;23(3):425–435. doi: 10.2190/16AY-E2GC-DFLD-51X2. [DOI] [PubMed] [Google Scholar]
- Lyons AC, Emslie C, Hunt K. Staying “in the zone” but not passing the “point of no return”: embodiment, gender and drinking in mid-life. Sociology of Health & Illness. 2014;36(2):264–277. doi: 10.1111/1467-9566.12103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macintyre S, Ellaway A. Social and local variations in the use of urban neighbourhoods: A case study in Glasgow. Health and Place. 1998;4(1):91–94. doi: 10.1016/s1353-8292(97)00030-0. [DOI] [PubMed] [Google Scholar]
- Macintyre S, Ellaway A, Cummins S. Place effects on health: How can we conceptualise, operationalise and measure them? Social Science and Medicine. 2002;55(1):125–139. doi: 10.1016/s0277-9536(01)00214-3. [DOI] [PubMed] [Google Scholar]
- MacLean S, Moore D. “Hyped up”: Assemblages of alcohol, excitement and violence for outer-suburban young adults in the inner-city at night. International Journal of Drug Policy. 2014;25(3):378–385. doi: 10.1016/j.drugpo.2014.02.006. [DOI] [PubMed] [Google Scholar]
- Mathews V, Picton RM. Intoxifying gentrification: brew pubs and the geography of post-industrial heritage. Urban Geography. 2014;35(3):337–356. [Google Scholar]
- Mennis J, Stahler GJ, Mason MJ. Risky substance use environments and addiction: A new frontier for environmental justice research. International Journal of Environmental Research and Public Health. 2016;13(6) doi: 10.3390/ijerph13060607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morency C, et al. Distance traveled in three Canadian cities: Spatial analysis from the perspective of vulnerable population segments. Journal of Transport Geography. 2011;19(1):39–50. Available at: http://www.sciencedirect.com/science/article/pii/S0966692309001525. [Google Scholar]
- Morrison C, et al. Relating off-premises alcohol outlet density to intentional and unintentional injuries. Addiction. 2015;(ix) doi: 10.1111/add.13098. p.n/a-n/a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulia N, et al. Social Disadvantage, Stress, and Alcohol Use Among Black, Hispanic, and White Americans: Findings From the 2005 U.S. National Alcohol Survey. Journal of Studies on Alcohol and Drugs. 2008;69(6):824–833. doi: 10.15288/jsad.2008.69.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nayak A. Last of the “Real Geordies”? White Masculinities and the Subcultural Response to Deindustrialisation. Environment and Planning D: Society and Space. 2003;21(1):7–25. doi: 10.1068/d44j. [DOI] [Google Scholar]
- Pattoni L, et al. The Relationship Between Off-Sales and Problem Drinking in Scotland: Literature Review. Edinburgh: 2007. [Google Scholar]
- Pearce J, et al. Tobacco Retail Environments and Social Inequalities in Individual-Level Smoking and Cessation Among Scottish Adults. Nicotine & tobacco research : official journal of the Society for Research on Nicotine and Tobacco. 2015;18(2):138–46. doi: 10.1093/ntr/ntv089. [DOI] [PubMed] [Google Scholar]
- Perchoux C, et al. Conceptualization and measurement of environmental exposure in epidemiology: Accounting for activity space related to daily mobility. Health & Place. 2013;21:86–93. doi: 10.1016/j.healthplace.2013.01.005. Available at: http://www.sciencedirect.com/science/article/pii/S1353829213000117. [DOI] [PubMed] [Google Scholar]
- Petticrew M, et al. How alcohol industry organisations mislead the public about alcohol and cancer. Drug and Alcohol Review. 2017 doi: 10.1111/dar.12596. doi:10.111, p.n/a-n/a. [DOI] [PubMed] [Google Scholar]
- van der Plight J. Perceived risk and vulnerability as predictors of precautionary behaviour. British Journal of Health Psychology. 1998;3(3):1–14. [Google Scholar]
- Rhodes T. Risk environments and drug harms: A social science for harm reduction approach. International Journal of Drug Policy. 2009;20(3):193–201. doi: 10.1016/j.drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Rhodes T. The “risk environment”: A framework for understanding and reducing drug-related harm. International Journal of Drug Policy. 2002;13(2):85–94. [Google Scholar]
- Richardson Ea, et al. Is local alcohol outlet density related to alcohol-related morbidity and mortality in Scottish cities? Health Place. 2015 Apr;33:172–180. doi: 10.1016/j.healthplace.2015.02.014. Available at: http://ac.els-cdn.com/S1353829215000349/1-s2.0-S1353829215000349-main.pdf?_tid=b6ad3634-33d0-11e5-85c4-00000aacb362&acdnat=1437940901_c4009938bbe0a855a3005feb48e674fb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Room R. Addiction and personal responsibility as solutions to the contradictions of neoliberal consumerism. Critical Public Health. 2011;21(2):141–151. doi: 10.1080/09581596.2010.529424. [DOI] [Google Scholar]
- Rose G. The strategy of preventive medicine. Oxford: University Press; 1992. [Google Scholar]
- Rosenberg M. Health geography III. Progress in Human Geography. 2016 doi: 10.1177/0309132516670054. p.309132516670054. [DOI] [Google Scholar]
- Rutherford L, Hinchliffe SCS. Scottish Health Survey 2012 - Volume 1 Main Report. Edinburgh: 2013. [Google Scholar]
- Scribner RA, MacKinnon DP, Dwyer JH. Alcohol outlet density and motor vehicle crashes in Los Angeles County cities. Journal of studies on alcohol. 1994;55(4):447–453. doi: 10.15288/jsa.1994.55.447. [DOI] [PubMed] [Google Scholar]
- Shortt NK, et al. A cross-sectional analysis of the relationship between tobacco and alcohol outlet density and neighbourhood deprivation. BMC Public Health. 2015;15:1014. doi: 10.1186/s12889-015-2321-1. Available at: http://www.biomedcentral.com/1471-2458/15/1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shortt NK, et al. Integrating environmental justice and socioecological models of health to understand population-level physical activity. Environment and Planning A. 2014;46(6):1479–1495. [Google Scholar]
- Shortt NK, et al. The density of tobacco retailers in home and school environments and relationship with adolescent smoking behaviours in Scotland. Tobacco Control. 2016;25(1):75–82. doi: 10.1136/tobaccocontrol-2013-051473. Available at: http://tobaccocontrol.bmj.com/content/early/2014/11/04/tobaccocontrol-2013-051473.abstract. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith K, Foster J. Alcohol, Health Inequalities and the Harm Paradox: Why some groups face greater problems despite consuming less alcohol. Institute of Alcohol Studies. 2014 [Google Scholar]
- Spoerri A, et al. Alcohol-selling outlets and mortality in Switzerland-the Swiss National Cohort. Addiction. 2013;108:1603–1611. doi: 10.1111/add.12218. [DOI] [PubMed] [Google Scholar]
- Stafford M, Marmot M. Neighbourhood deprivation and health: does it affect us all equally? International journal of epidemiology. 2003;32(3):357–366. doi: 10.1093/ije/dyg084. [DOI] [PubMed] [Google Scholar]
- Stockwell T, et al. Impact on alcohol-related mortality of a rapid rise in the density of private liquor outlets in British Columbia: A local area multi-level analysis. Addiction. 2011;106(i):768–776. doi: 10.1111/j.1360-0443.2010.03331.x. [DOI] [PubMed] [Google Scholar]
- Thurnell-Read T. #x201C;Yobs” and’Snobs’: Embodying Drink and the Problematic Male Drinking Body. Sociological Research Online. 2013;18(2):3. [Google Scholar]
- Treno aJ, et al. Alcohol outlet densities and alcohol price: the British Columbia experiment in the partial privatization of alcohol sales off-premise. Alcohol Clin Exp Res. 2013;37(5):854–859. doi: 10.1111/acer.12065. Available at: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4204796/pdf/nihms634276.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogl M, et al. Smoking and health-related quality of life in English general population: implications for economic evaluations. BMC Public Health. 2012;12(1):203. doi: 10.1186/1471-2458-12-203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO. Global Status Report on Alcohol and Health 2014. Geneva: 2014. [Google Scholar]
- WHO. Global strategy to reduce harmful use of alcohol. Geneva: 2010. [Google Scholar]
- Wolburg JM. How responsible are “responsible” drinking campaigns for preventing alcohol abuse? Journal of Consumer Marketing. 2005;22(4):176–177. doi: 10.1108/07363760510605281. [DOI] [Google Scholar]
- Zhu L, Gorman DM, Horel S. Alcohol outlet density and violence: A geospatial analysis. Alcohol and Alcoholism. 2004;39(4):369–375. doi: 10.1093/alcalc/agh062. [DOI] [PubMed] [Google Scholar]