SUMMARY
OBJECTIVE:
To calculate the per-session and annual direct program costs to implement directly observed therapy (DOT) for tuberculosis treatment and to conduct a cost attribution analysis under varying proportions of DOT utilization for four DOT types.
DESIGN:
Program data covering the study period from September 2014 to August 2015 in New York City (NYC) were used to conduct a retrospective bottom-up micro-costing economic evaluation. For each DOT type, potential per-session and annual program savings were estimated as the cost averted by adopting a uniform distribution of DOT alternatives. Sensitivity analyses explored aggregate cost impacts of unequal distributions.
RESULTS:
There was a total of 38 035 unique DOT visits, of which 12 002 (32%) were clinic-based (CDOT); 15 483 (41%) were field-based (FDOT); 7185 (19%) were live-video (LVDOT); and 3365 (9%) were recorded-video (RVDOT). The per-session direct costs (in 2016 $US) for DOT services delivered during the study period were $8.46 for CDOT; $19.83 for FDOT; $6.54 for LVDOT; and $5.35 for RVDOT. Sensitivity analyses supported the main findings.
CONCLUSIONS:
Significant cost savings were estimated with increased utilization of VDOT. Assuming equivalent treatment adherence, duration, completion, and adverse events across DOT types, RVDOT was the modality that most minimized cost.
Keywords: telemedicine, micro-costing, program evaluation, attribution analysis
RESUME
OBJECTIF:
Calculer les coûts directs du programme par session et par an en termes de mise en œuvre de la thérapie sous observation directe (DOT) pour le traitement de la tuberculose et de réaliser une analyse d’attribution des coûts en fonction des variations du taux d’utilisation des DOT dans quatre types de DOT.
SCHÉMA:
Les données de programme couvrant la période d’étude, de septembre 2014 à août 2015, dans la ville de New York (NYC) ont été utilisées pour réaliser une évaluation économique rétrospective participative des micro coûts. Pour chaque stratégie de DOT, les économies potentielles pour le programme par session et par an ont été; estimées comme le coût évité en adoptant une distribution uniforme des alternatives au DOT. Les analyses de sensibilité ont exploré les impacts de coût aggrégé des distributions inégales.
RÉSULTATS:
Le nombre total de DOT uniques a été de 38 035, avec la distribution suivante—DOT en structures de santé (CDOT), 12 002 (32%); DOT sur le terrain (FDOT), 15 483 (41%); DOT sous vidéo en temps réel (LVDOT), 7185 (19%); et sous vidéo enregistrée (RVDOT), 3365 (9%). Les coûts directs par session (en $US 2016) pour les services DOT fournis pendant la période d’étude ont été de 8,46$ pour les CDOT; de 19,83$ pour les FDOT; de 6,54$ pour les LVDOT; et de 5,35$ pour les RVDOT. Les analyses de sensibilité ont confirmé les principaux résultats.
CONCLUSION:
Des économies significatives ont été estimées grâce à l’utilisation accrue des VDOT. Les RVDOT ont été la modalité de réduction des coûts en admettant que l’observance au traitement, sa durée, son achèvement et les effets secondaires sont équivalents dans toutes les stratégies de DOT.
RESUMEN
OBJETIVO:
Calcular los costos programáticos por sesión y los costos anuales directos de la ejecución del tratamiento antituberculoso con observación directa (DOT) y realizar un análisis de atribución de costos en diferentes situaciones hipotéticas de la proporción de utilizatión de cuatro tipos de DOT.
MÉTODO:
Se utilizaron los datos del programa de septiembre del 2014 a agosto del 2015 de la ciudad de Nueva York, con el fin de realizar una evaluatión económica de tipo ascendente del análisis detallado de los costos. Para cada tipo de DOT se calcularon los posibles ahorros para el programa por sesión y anuales como el costo evitado al adoptar una distributión uniforme de las otras opciones de DOT. Mediante un análisis de sensibilidad se evaluaron los efectos del costo agregado de las distribuciones desiguales.
RESULTADOS:
El número total de citas únicas por DOT fue 38 035, con la siguiente distributión: en consultorio (CDOT), 12 002 (32%); en el terreno (FDOT), 15 483 (41%); con video directo (LVDOT), 7185 (19%); y con video grabado (RVDOT), 3365 (9%). Los costos directos por sesión (en $US del 2016) por los servicios de DOT prestados durante el período del estudio fueron como sigue: 8,46 $US por CDOT; 19,83 $US por FDOT; 6,54 $US por LVDOT; y 5,35 para RVDOT. Los análisis de sensibilidad respaldaron los resultados principales.
CONCLUSIÓN:
Se calcularon ahorros considerables en los costos al aumentar la utilizatión de VDOT. La optión RVDOT sería la modalidad de minimizatión de costos, al suponer una equivalencia en la adhesión, la duratión, la completión y las reacciones adversas al tratamiento con todos los tipos de DOT.
The US national incidence rate for tuberculosis (TB) cases in 2016 was 2.9 per 100 000 population.1 Treatment for TB disease usually requires 6 months or longer with multiple drugs. Treatment adherence is critical to successful patient outcomes.2 Directly observed therapy (DOT) is the standard of care in New York City (NYC) to ensure proper adherence during the treatment of TB disease; however, it is a resource intensive intervention.
DOT involves trained individuals observing each dose of anti-TB medication administered for the duration of treatment. DOT can be conducted through face-to-face (in-person) or electronic observation, including videoconferencing and recorded-video sessions (VDOT).3 In prior studies, use of live-videoconferencing or recorded-video DOT (LVDOT, RVDOT) has been shown to promote treatment adherence and completion outcomes similar to in-person clinic and field-based DOT (CDOT, FDOT).4–7 VDOT was also shown to be highly accepted by patients and health-care providers.8 Program savings associated with reduced travel and staff time for telehealth strategies are potentially substantial, although studies are limited.7,9–11
The NYC Department of Health and Mental Hygiene (DOHMH) provides DOT at four clinics, homes, worksites and locations requested by patients. Patients eligible for DOT include those on treatment for TB disease (e.g., confirmed or probable TB cases), and certain patients treated for latent TB infection (e.g., household contacts of infectious TB patients).5,12 The DOHMH offers four types of DOT: CDOT, FDOT, LVDOT, and RVDOT.
We conducted a cost-minimization analysis to estimate and compare the costs of offering each DOT type in NYC. Our study objectives were 1) to calculate labor and non-labor costs associated with all DOT types offered by the DOHMH, 2) to calculate per-session and annual program costs to implement DOT, and 3) to assess cost impacts when re-assigning the observed DOT sessions to alternative types (i.e., cost attribution).
METHODS
Cost analysis
This study used a retrospective, bottom-up micro-costing cost-minimization evaluation methodology taking the TB program perspective.13–15 Cost-minimization analyses identify and compare costs of interventions while assuming equivalent health outcomes between types,16 thereby focusing solely on cost differences to inform program evaluation.17 This methodology has previously been used in analyses of TB treatment activities.18 Costs were calculated for all DOT sessions conducted by the DOHMH TB program during September 2014–August 2015. The cost data from 2016 were applied to resource utilization in the study period due to the unavailability of cost information. Labor and non-labor cost inputs were obtained from the DOHMH TB program except for gasoline costs, which were obtained through the New York State Energy Research and Development Authority.19 The analysis focused on cost per DOT session, rather than per patient, since some patients receive DOT from non-DOHMH providers for part of their treatment.
Labor costs
Labor costs per minute were estimated by taking the annual salary plus fringe benefits for each DOT worker and dividing by the minutes in 261 paid 7-hour working days (including holidays). DOT staff, who are trained, non-licensed professionals, range in job titles and salaries; therefore, we calculated the cost per session for each of the 17 DOT workers by multiplying cost per minute with each DOT type’s observation time. The duration of one LVDOT session was previously observed to be 5 minutes.5 We assumed the same duration for CDOT and one half of the LVDOT observation time (2.5 minutes) for RVDOT, since no real-time interactions occur during RVDOT sessions. For FDOT, we assumed the same observation time as for LVDOT plus one-way travel time. The per-session labor cost was the average of all the workers’ cost per session for each DOT type.
To calculate the FDOT travel times, we reviewed vehicle travel logs completed as part of standard program practice. Only DOT-specific trips submitted by DOT workers using designated vehicles were included. We randomly selected one weekday every 2 weeks (excluding holidays) from January 2014 through August 2014 and from January 2015 through August 2015 to obtain a representative sample of travel. The miles traveled and the travel times between locations were calculated. We excluded trips where neither the arrival nor departure site was a DOT location (e.g., relocation of vehicles for parking). We also excluded non-DOT trips (e.g., maintenance, hospital visits) and incomplete records—missing or illegible mileage information or data entry errors (e.g., negative mileage). Logs with missing travel times were excluded from the average travel time calculation.
Non-labor costs
Non-labor cost inputs included resources used for one or multiple DOT types. Costs associated with multiple program activities, which could not be separated from DOT, were excluded (e.g., administrative costs for operating clinics). Additionally, only costs directly incurred by the TB program were included in the analysis, which excludes other DOHMH and city government expenses (e.g., insurance). Table 1 shows the non-labor costs.
Table 1.
New York City Health Department Bureau of Tuberculosis Control non-labor cost per session categorized by DOT type
| DOT type | Cost input | Units n | Unit cost USD | Total amortized cost USD | Cost/day USD | Cost/session USD | Total cost/session USD |
|---|---|---|---|---|---|---|---|
| LVDOT | Webcams | 9 | 51.94 | 156.00 | 0.63 | 0.02 | 3.63 |
| Signature pads | 2 | 370.00 | 246.67 | 1.00 | 0.03 | ||
| Software | 1 | N/A* | |||||
| Patient phones | 81 | N/A* | |||||
| Headsets | 9 | 46.95 | 141.00 | 0.57 | 0.01 | ||
| Patient phone service | 81 | 420.00 | 34,020.00 | 137.73 | 3.58 | ||
| RVDOT | Software license | 1 | 19,440.00 | 19,440.00 | 78.70 | 2.04 | 3.88 |
| Signature pads | 2 | 370.00 | 246.67 | 1.00 | 0.03 | ||
| Patient phones | 41 | N/A | |||||
| Patient phone service | 41 | 420.00 | 17,220.00 | 69.72 | 1.81 | ||
| CDOT | Two-way transit card† | 1 | 5.50 | 52,302.00 | 211.75 | 5.50 | 5.55 |
| Signature pads | 4 | 370.00 | 493.33 | 2.00 | 0.05 | ||
| FDOT | Gasoline | Variable | 0.34 | 3,247.00 | 13.14 | 0.34‡ | 1.16 |
| Staff phones | 10 | N/A* | |||||
| Staff tablets | 10 | 1076.25 | 3,588.00 | 14.52 | 0.38 | ||
| Staff phone service | 10 | 420.00 | 4,200.00 | 17.00 | 0.44 |
N/A indicates costs that were not directly incurred by the program. Straight-line amortization over 3 years with no salvage value was applied to the program costs for tangible assets.
Total amortized cost calculated by multiplying the unit cost per two-way transit card times by the number of CDOT sessions in the steady state (i.e., 9510 sessions annually).
Amount reflects the average of the monthly estimates for the cost of gasoline per session during January 2014–August 2014 and January 2015–August 2015. DOT = directly observed therapy; USD = US dollars; LVDOT = live-video DOT; N/A = not applicable; RVDOT = recorded-video DOT; CDOT = clinic-based DOT; FDOT = field-based DOT.
Based on the mileage logs, the average daily miles traveled for FDOT were aggregated by month and divided by the number of working days in that month. Fuel economy for hybrid sedans was assumed to be 30 miles per gallon of gasoline. The mean daily travel cost was the average daily distance in miles per gallon multiplied by the 2016 monthly per-gallon gasoline costs for the NYC metropolitan area.19 The number of daily FDOT sessions was the total number of one-way trips in that month divided by the number of person-days. Travel cost per session was the mean daily travel cost divided by the average FDOT sessions per day.
To calculate the total per-session costs, we defined a steady state of DOT implementation comprising equal use of all DOT types (i.e., 25% RVDOT, 25% LVDOT, 25% FDOT, 25% CDOT), given the average daily DOT capacity, which was the sum of observed DOT sessions across all DOT types divided by 247 working days. For all non-labor assets (e.g., webcams, signature pads, headsets, and tablets), we determined a 3-year useful life and a depreciation rate of one third. This rate, multiplied by the total asset cost, derives the annual cost assuming zero salvage value. Cost per day was the total cost of each non-labor input divided by 247 working days. Cost per session was the cost per day divided by the number of steady state sessions per day. The total non-labor cost per session for each DOT type was the sum of their costs of inputs per session.
Cost attribution analyses
Cost attribution analysis captures the changes in resource use as the parameters of the intervention are modified. We modified the proportions of DOT utilization and multiplied by the program’s total DOT capacity to identify the number of sessions for each DOT type. We multiplied these by the total per-session costs and examined the savings potential. We identified 35 implementation scenarios for the attribution analysis by adjusting the DOT proportions at quartile increments (0, 0.25, 0.50, 0.75, and 1) and choosing a proportion for each DOT type where the sum of the proportions equals one. We hypothesized that increased use of VDOT would significantly (P < 0.05) decrease the annual program cost.
We applied four bivariate generalized linear models to the scenario data to predict the average changes in cost outcome. We created four ordinal variables, one for each DOT type. Each variable indicated the quartile of utilization for that DOT type. For example, in a scenario where only RVDOT is used, the variable for RVDOT would indicate a value of ‘4,’ as 100% utilization describes the highest quartile. The variables for all other DOT types would equal ‘0.’ Three sensitivity checks were conducted on the re-attributed data set: 1) re-allocating non-labor inputs across VDOT types, 2) increasing RVDOT session time to match LVDOT, and 3) evaluating the economies of scale assumption.
Microsoft Excel (Microsoft Corp, Redmond, WA, USA) was used to generate random dates for assessing the DOT logs and to develop the data tables for the cost analysis. Regression analyses were implemented using Stata v14 (StataCorp, College Station, TX, USA).
Ethics
This analysis was considered a public health program evaluation activity and did not require review by the DOHMH Institutional Review Board (IRB). This project was reviewed by the Centers for Disease Control (Atlanta, GA, USA) and determined to not be research requiring IRB review.
RESULTS
Between September 2014 and August 2015, there were 38 035 unique DOT sessions with the following distribution: CDOT 12 002 (32%); FDOT 15 483 (41%); LVDOT 7185 (19%); and RVDOT 3365 (9%), and with the following average DOT sessions per day: CDOT 49; FDOT 63; LVDOT 29; and RVDOT 14. The total annual cost for all DOT delivery in the study period in $US was $476 405: $102 494 for CDOT; $308 521 for FDOT; $46 927 for LVDOT; and $18 463 for RVDOT. The total cost per session was $8.46 for CDOT, $19.83 for FDOT, $6.54 for LVDOT, and $5.35 for RVDOT (Table 2). Per-session cost derivations showed both RVDOT and LVDOT costs to be lower than CDOT and FDOT costs. The Figure shows that FDOT comprised approximately 65% of the total cost and an even greater proportion (83%) of the total labor cost for DOT.
Table 2.
Calculated annual and per-session cost of delivering DOT, New York City, September 2014–August 2015*
| LVDOT $US | RVDOT $US | CDOT $US | FDOT $US | |
|---|---|---|---|---|
| Average labor cost per session† | 2.91 | 1.47 | 2.91 | 18.67 |
| Non-labor bureau cost per session | 3.63 | 3.88 | 5.55 | 1.16 |
| Total cost per session (labor + non-labor) | 6.54 | 5.35 | 8.46 | 19.83 |
| Average sessions per day in study period, n | 29 | 14 | 49 | 63 |
| Total cost per day (total cost per session times average sessions per day) | 190 | 75 | 415 | 1,249 |
| Total annual DOT cost (247 working days) | 46 927 | 18 463 | 102 494 | 308 521 |
Estimates may vary due to rounding. The average annual salary for NYC DOT workers was $47 353 in 2016 $US.
Average labor cost per DOT type i Session∑j [(annual salary plus fringe j/min in 261, 7-h days) × 3Mi min/session × 1/J] where j = 1, 2, 3,… J indicates one of 17 NYC DOT workers (J = 17) and M indicates the number of min/session for DOT type i. Note M for RVDOT is 2.5 min; M for FDOT is 5 min/session + average one-way travel time for DOT (i.e., 27 min); M for LVDOT and CDOT is 5 min.
DOT = directly observed therapy; LVDOT = live-video DOT; RVDOT = recorded-video DOT; CDOT = clinic-based DOT; FDOT = field-based DOT; $US = US dollars; NYC = New York City.
Figure.
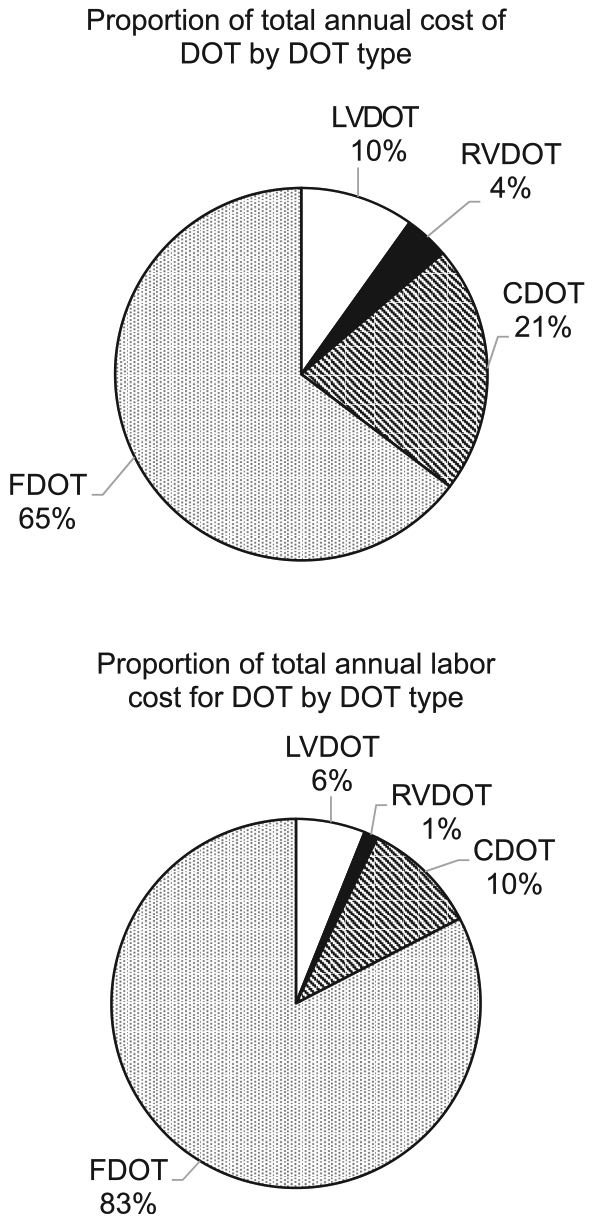
Annual total (top) and labor costs (bottom) by DOT type based on utilization between September 2014 and August 2015 in New York City, NY, USA. CDOT = clinic-based DOT; FDOT = field-based DOT; LVDOT = live-video DOT; RVDOT = recorded-video DOT.
Cost inputs
Of 34 randomized days, 33 had FDOT observations conducted and 2494 one-way trips were identified with 223 (8.9%) trips excluded due to incomplete records or identification as non-DOT trips. Of 2271 trips included in the mileage calculations, 1703 (75%) were retained to calculate the average FDOT travel time; the others were excluded due to incomplete or inaccurate times. The mean travel time was 27.43 minutes (interquartile range [IQR] 15–35). The average miles traveled per person-day was 38.4 miles and the average steady state per-session gasoline cost was $0.34.
The average annual salary was $47 353. Average labor costs per session were $2.91 for CDOT, $18.67 for FDOT, $2.91 for LVDOT, and $1.47 for RVDOT. Notably, $15.21 (81%) of the FDOT labor cost per session was attributed to travel time. Table 1 shows the non-labor cost components.
Cost attribution analysis
Table 3 summarizes the cost impacts in the attribution analysis. We started by assuming that one DOT type is unused and the others are held in equal proportions (33%). We then increased the use of that DOT type by 25% (one quartile) and estimated the new total program cost. The mean cost for DOT without using RVDOT was $422 938 (model 4). For each quartile increase in RVDOT utilization, we noted a 16% decrease (P < 0.001) in the total costs to $359 232 (95% confidence interval [CI] $332 743–$387 830), keeping the non-labor input allocations unchanged. By comparison, each quartile increase of LVDOT use produced an 11% decline (model 3; P = 0.01), and for FDOT, there was a 30% increase (model 2; P < 0.01). Using a uniform distribution of DOT delivery (25% for each DOT type, or 9510 sessions each), the total annual cost was $382 145 (or $10 using a per-session average basis), reflecting a 20% reduction in cost.
Table 3.
Generalized linear model results of the cost simulation*
| Model | DOT type | Intercept | Coefficient | P value | ||
|---|---|---|---|---|---|---|
| US$ | 95%CI | % | 95%CI | |||
| 1 | CDOT | 370 586 | 310 305–442 577 | −3 | −12 to 5 | 0.48 |
| 2 | FDOT | 265 343 | 250 644–280 904 | +30 | 27 to 34 | <0.01 |
| 3 | LVDOT | 400 432 | 340 190–471 342 | −11 | −19 to −3 | 0.01 |
| 4 | RVDOT | 422 938 | 365 722–489 104 | −16 | −24 to −9 | <0.01 |
Estimates may vary due to rounding. The reported intercept for each model is the annual cost when the specified DOT type is not used and the other three are used in equal proportions (33%). The coefficient represents the percentage change in the total costs for each additional quartile increase in use.
DOT = directly observed therapy; US$ = US dollars; CI = confidence interval; CDOT = clinic-based DOT; FDOT = field-based DOT; LVDOT = live-video DOT; RVDOT = recorded-video DOT
Sensitivity analyses
First, we re-distributed the patient phones equally across VDOT types, which did not statistically change the absolute cost outcome for RVDOT ($359 433, 95%CI $331 670–$389,521; P = 0.003). Second, we increased the per-session RVDOT observation time from 2.5 to 5 min, resulting in a smaller decrease, from 16% to 11% (P = 0.003), matching the LVDOT cost outcome. Finally, we reduced the program capacity for each DOT type by 10%, which increased the cost for a one quartile increase in RVDOT to $369 733 (an increase of 3%, or approximately $10 500). The sensitivity analyses demonstrated the robustness of RVDOT as a cost-minimizing DOT type.
DISCUSSION
The use of VDOT has increased among US TB programs in recent years.3 While some studies demonstrated equivalent treatment outcomes using VDOT, few studies have assessed its economic value to public health programs. Our study calculated both annual and per-session costs of four different DOT types in NYC, which represents a novel contribution due to the multiple DOT types assessed and the volume of observation data included. We subsequently offered another noteworthy addition by estimating the cost savings with the increased utilization of either type of VDOT offered by the DOHMH. We identified RVDOT as the modality that most minimized costs, assuming equivalent treatment adherence, duration, completion, and adverse events across the DOT types. However, the sensitivity analysis indicated that the cost savings for RVDOT would be similar to LVDOT if the observation time matched.
There were limitations with the mileage logs. First, a sample of FDOT trips encompassing 8 months prior to and 8 months during the study period was used due to missing logs during the study period, potentially resulting in different numbers of per-day FDOT trips, mileage, and time. Second, we were unable to use the exact number FDOT observations (e.g., trips with multiple patients at one location) to calculate per-session travel time and distance, potentially increasing the FDOT costs. However, we expect our sample contained few trips with multiple observations. Third, public transportation was excluded due to unavailable data on the number of visits and travel times. However, as FDOT costs mostly consist of labor, including public transportation, which requires more time, this will likely increase FDOT costs.
Another limitation to this study is that only DOT costs directly incurred by the TB program were used. We excluded costs absorbed by the NYC Health Department such as insurance, purchase, and maintenance costs for vehicles and clinics’ operating costs. Including these would increase the annual cost for FDOT and CDOT. Other costs not incorporated into these estimates (Table 1) include the LVDOT software cost, which was not directly incurred by the program, and phone purchase costs. The exclusion of phone purchase costs, for VDOT, may mirror localities where patients must use their personal devices. Furthermore, nursing salaries were excluded. In NYC, nurses perform observations for injectable medications and occasionally for oral medications. Excluding these salaries represents an underestimate in labor costs. Labor costs also did not capture time spent resolving VDOT issues. As previously reported, technology problems occur for both patients and Health Department staff.5 However, as the technology evolves and the patient population becomes more comfortable and adept with technology, we anticipate that fewer problems requiring assistance will occur.
This economic evaluation assessed cost inputs for four types of DOT to calculate the annual and per-session costs. Using known distributions of utilization by DOT type, we estimated potential savings through increased utilization of VDOT. Although not statistically significant, CDOT also presented a viable alternative. If costs for operating clinics were included, however, potential savings would likely decrease. This evaluation focused solely on costs from a TB program perspective, excluding patient considerations. Patients’ time and travel costs would likely also increase the cost of CDOT and contribute evidence for increasing the utilization of VDOT. An ongoing Centers for Disease Control (Atlanta, GA, USA) evaluation (CDC-RFA-PS15–150103CONT17) compares costs from a societal perspective. Finally, the current evaluation focused on per-sessions costs based on the known DOT utilization of the TB program. Analyses assessing DOT costs for monitoring patients through the end of treatment, while factoring in patient and disease characteristics as well as outcomes, would provide an alternate and informative perspective for TB programs.
In striving to provide more patient-centered care, offering a single DOT type may not be the optimal solution even if it generates the greatest savings. Some patients require alternate means of treatment monitoring (e.g., experienced adverse events, needs in-person evaluation). For these situations, offering multiple DOT types allows the program to accommodate individual patient needs. Our results support adopting a strategy with multiple DOT types to accommodate complex treatment needs while encouraging VDOT when possible to lower costs. Other TB programs may apply similar methodology to assess cost savings when developing a DOT strategy.
Acknowledgements
The authors would like to thank the doctors, nurses, public health advisors, and all other staff of the New York City Department of Health Bureau of Tuberculosis Control Chest Center for their commitment and dedication in delivering the highest quality care to patients.
This work was supported by the New York City Department of Health and Mental Hygiene (New York, NY, USA).
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily reflect the official position of the Centers for Disease Control and Prevention (Atlanta, GA, USA) or the authors’ affiliated institutions.
Conflicts of interest: none declared.
References
- 1.Centers for Disease Control and Prevention (CDC). Reported tuberculosis in the United States, 2016. Atlanta, GA, USA: US Department of Health and Human Services, CDC, 2017. [Google Scholar]
- 2.Imperial MZ, Nahid P, Phillips PPJ, et al. A patient-level pooled analysis of treatment-shortening regimens for drug-susceptible pulmonary tuberculosis. Nat Med 2018; 24(11): 1708–1715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macaraig M, Lobato MN, McGinnis Pilote K, Wegener D. a national survey on the use of electronic directly observed therapy for treatment of tuberculosis. J Public Health Manag Pract 2018; 24(6): 567–570. [DOI] [PubMed] [Google Scholar]
- 4.Garfein RS, Collins K, Munoz F, et al. Feasibility of tuberculosis treatment monitoring by video directly observed therapy: a binational pilot study. Int J Tuberc Lung Dis 2015; 19(9): 1057–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chuck C, Robinson E, Macaraig M, Alexander M, Burzynski J. Enhancing management of tuberculosis treatment with video directly observed therapy in New York City. Int J Tuberc Lung Dis 2016; 20(5): 588–593. [DOI] [PubMed] [Google Scholar]
- 6.Mirsaeidi M, Farshidpour M, Banks-Tripp D, Hashmi S, Kujoth C, Schraufnagel D. Video directly observed therapy for treatment of tuberculosis is patient-oriented and cost-effective. Eur Respir J 2015; 46(3): 871–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garfein RS, Liu L, Cuevas-Mota J, et al. Tuberculosis treatment monitoring by video directly observed therapy in 5 health districts, California, USA. Emerg Infect Dis 2018; 24(10): 1806–1815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zúñiga ML, Collins K, Muñoz F, et al. A qualitative study exploring stakeholder perceptions of video directly observed therapy for monitoring tuberculosis treatment in the US-Mexico border region. J Mob Technol Med 2016; 5(2): 12–23. [Google Scholar]
- 9.DeMaio J, Schwartz L, Cooley P, Tice A. The application of telemedicine technology to a directly observed therapy program for tuberculosis: a pilot project. Clin Infect Dis 2001; 33(12): 2082–2084. [DOI] [PubMed] [Google Scholar]
- 10.Krueger K, Ruby D, Cooley P, et al. Videophone utilization as an alternative to directly observed therapy for tuberculosis. Int J Tuberc Lung Dis 2010; 14(6): 779–781. [PubMed] [Google Scholar]
- 11.Buchman T, Cabello C. A new method to directly observe tuberculosis treatment: Skype observed therapy, a patient-centered approach. J Public Health Manag Pract 2017; 23(2): 175–177. [DOI] [PubMed] [Google Scholar]
- 12.Bureau of Tuberculosis Control. Clinical Policies and Protocols. 4th ed: New York, NY, USA: New York City Department of Health and Mental Hygiene, 2008. [Google Scholar]
- 13.Tan SS. Micro-costing in economic evaluations: issues of accuracy, feasibility, consistency and generalizability. Rotterdam, Netherlands: Erasmus Universiteit Rotterdam, 2009. [Google Scholar]
- 14.Hendriks ME, Kundu P, Boers AC, et al. Step-by-step guideline for disease-specific costing studies in low- and middle-income countries: a mixed methodology. Glob Health Action 2014; 7: 23573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Frick KD. Microcosting quantity data collection methods. Med Care 2009; 47(Suppl 1): S76–S81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Briggs AH, O’Brien BJ. The death of cost-minimization analysis? Health Econ 2001; 10(2): 179–184. [DOI] [PubMed] [Google Scholar]
- 17.Drummond MF, Sculper MK, Claxton K, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. 4th ed Oxford, UK: Oxford University Press, 2015. [Google Scholar]
- 18.Musa BM, John D, Habib AG, Kuznik A. Cost-optimization in the treatment of multidrug resistant tuberculosis in Nigeria. Trop Med Int Health 2016; 21(2): 176–182. [DOI] [PubMed] [Google Scholar]
- 19.New York State Energy Research and Development Authority. Monthly average motor gasoline prices, 2017. Albany, NY, USA: NYSERDA; 2017. https://www.nyserda.ny.gov/Researchers-and-Policymakers/Energy-Prices/Motor-Gasoline/Monthly-Average-Motor-Gasoline-Prices Accessed August 2019. [Google Scholar]


