Abstract
We report an 85-year-old patient with severe osteoporosis who had suffered from multiple episodes of periprosthetic fracture of the femur. Revision fixation with long-spanning cable plate for bisphosphonate-induced atypical periprosthetic femoral fracture was performed. Nonunion and implant failure occurred at 16 months requiring revision surgery using long-stem femoral prosthesis with cable-plate fixation. To further facilitate bone healing, allograft and bone morphogenetic protein (BMP) were added. Eventually bone union was achieved after one year.
Keywords: Alendronate, Arthroplasty, Hip, Periprosthetic fractures, Fracture, Stress, Non-union, Case report
Introduction
Osteoporosis represents a major public health problem, and this burden is growing with increasing life expectancy and ageing population [7]. Periprosthetic femoral fractures are increasingly common and the management of such fractures on osteoportic bones poses a great challenge. Nonunion is not uncommon in bisphosphonate-induced atypical fractures due to the altered biology of fracture healing. In our case, we tackled such problem by addressing both the biological and mechanical aspects of fracture healing.
Case report
An 85-year-old lady was presented to our unit for severe left leg pain after a low energy fall injury at home. Two years before cemented unipolar hemiarthroplasty was done for fracture neck of femur. She was prescribed with oral Fosamax for two years since the first surgery.
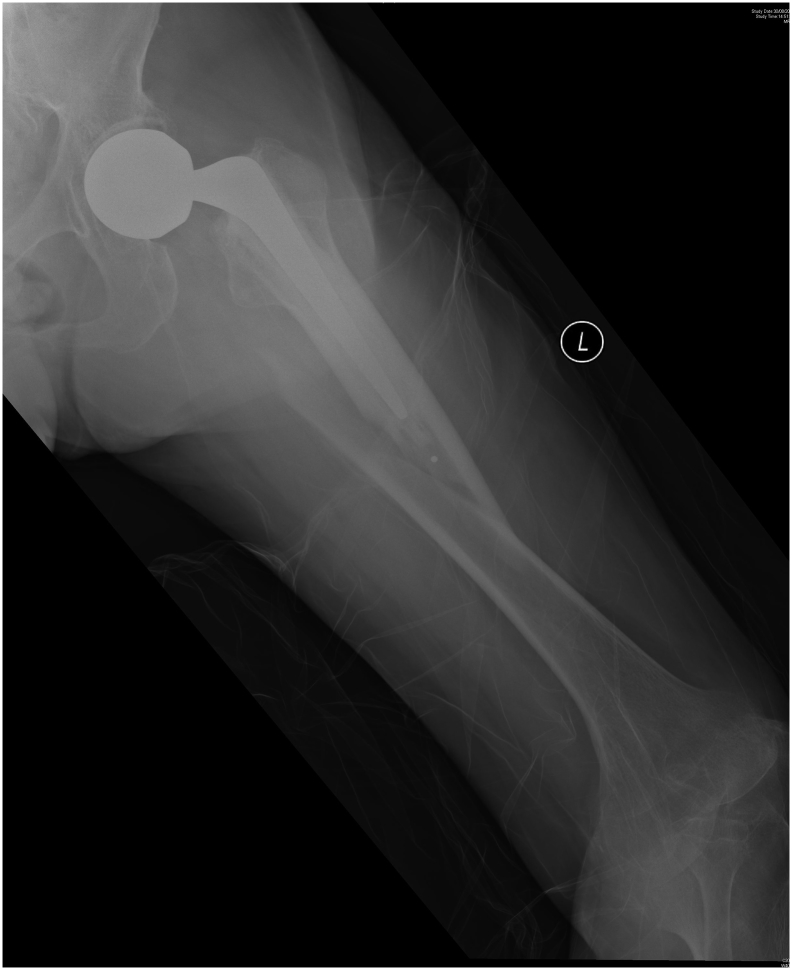
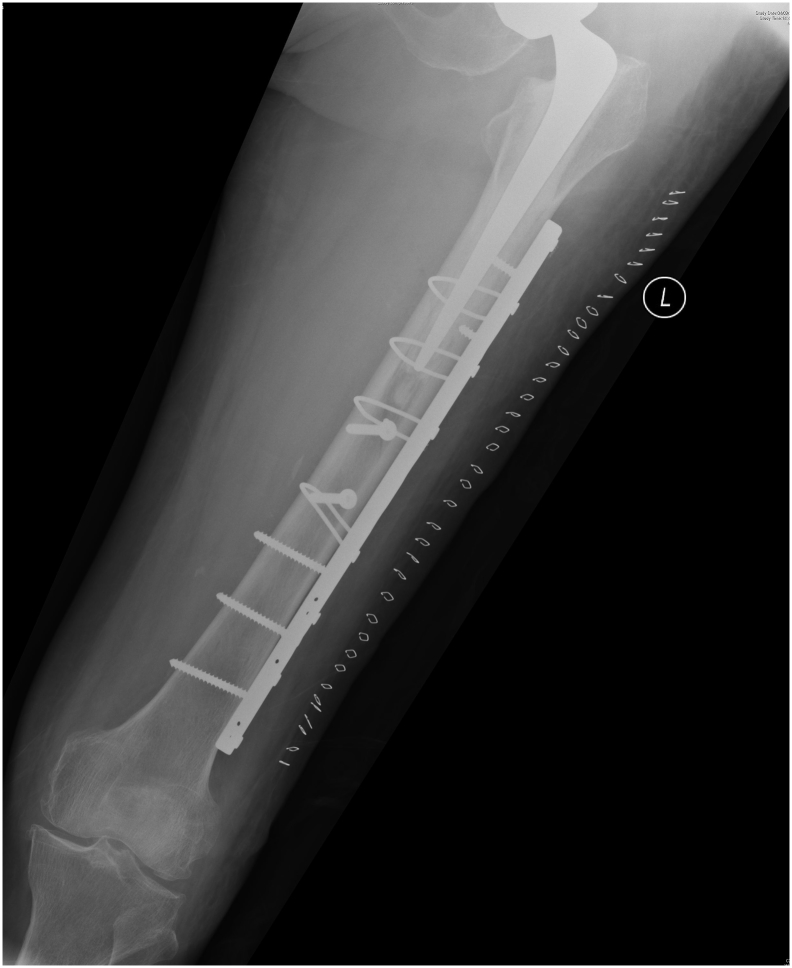
Radiographs revealed a Vancouver's B1 periprosthetic fracture of the left femur (Fig. 1, Fig. 2). Open reduction and internal fixation with locking cable-plate was performed (Figs. 3, Fig. 4, Fig. 5). There were two cortical diameters overlapping between the plate and stem to prevent stress riser. Intraoperatively the stem was found to be stable. Two lag screws were used to provide compression at the fracture site. The proximal fragment was fixed with two unicortical screws and three gripping cables. The distal fragment was fixed with three bicortical screws. The patient was allowed protected weight bearing for 8 weeks and then full-wright bearing walking. Subsequently the patient could walk with stick and radiographs at 6 months revealed satisfactory healing over the fracture site (Fig. 6, Fig. 7).
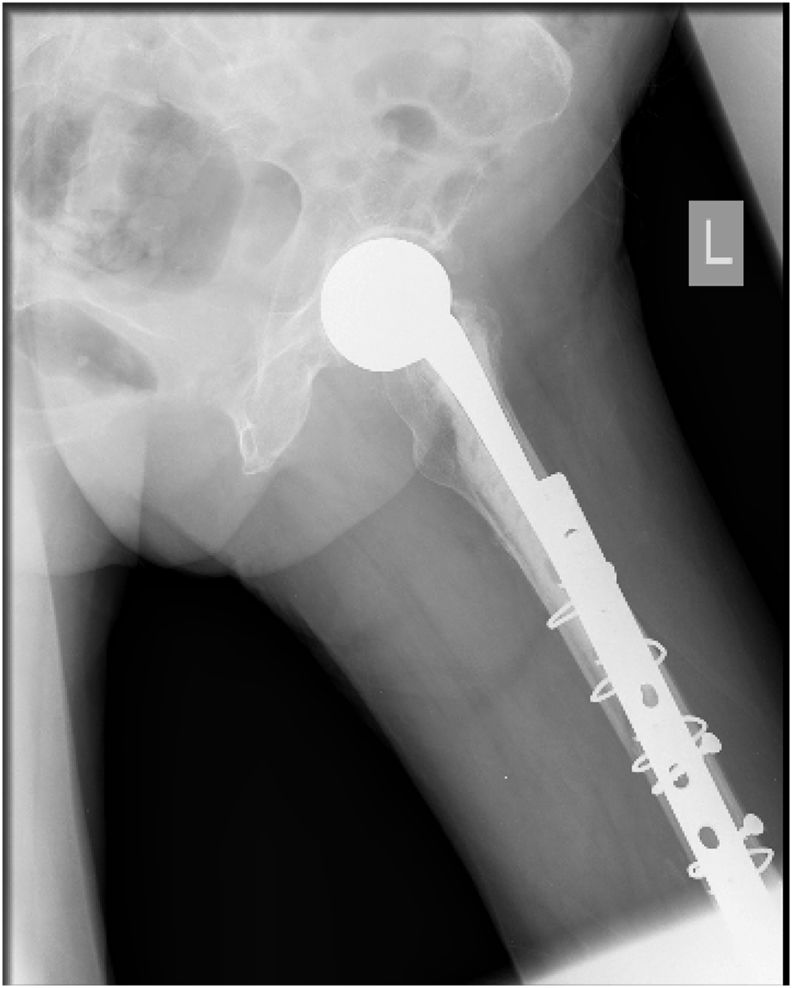
Fig. 1.
Radiograph (AP view) showing Vancouver's B1 periprosthetic fracture of the left femur.
Fig. 2.
Radiographs (lateral view) showing Vancouver's B1 periprosthetic fracture of the left femur.
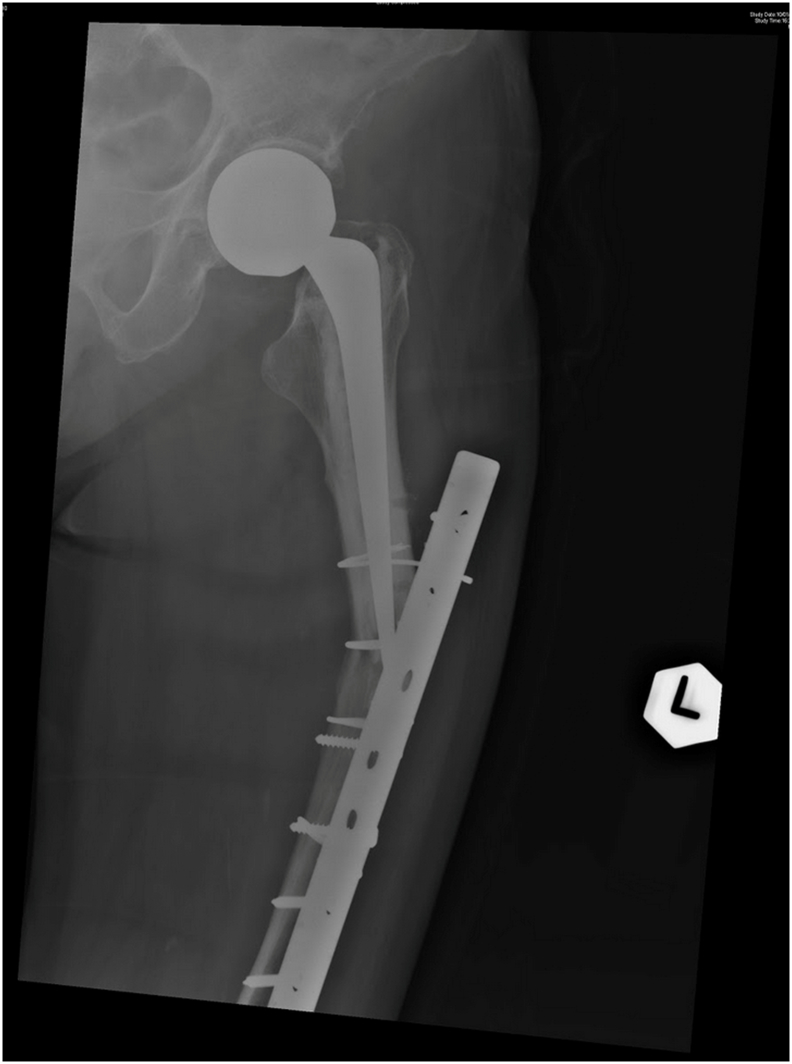
Figs. 3.
Open reduction and internal fixation with locking cable-plate (Post-op AP view).
Fig. 4.
Open reduction and internal fixation with locking cable-plate (Post-op lateral view).
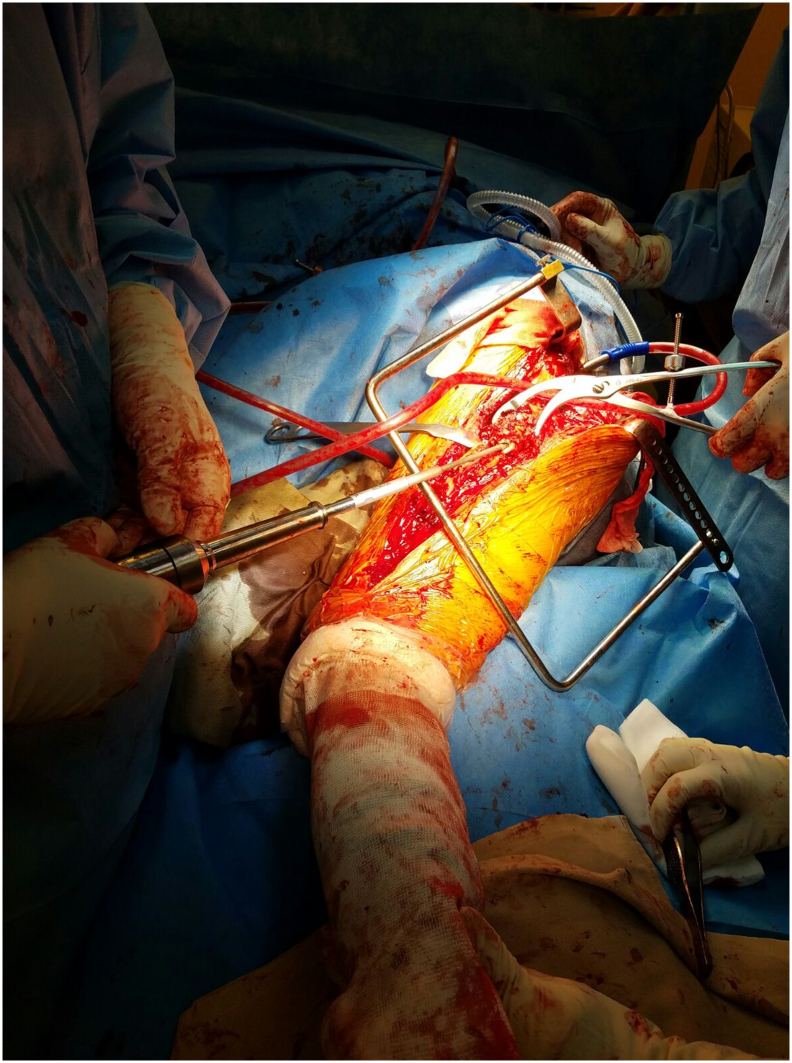
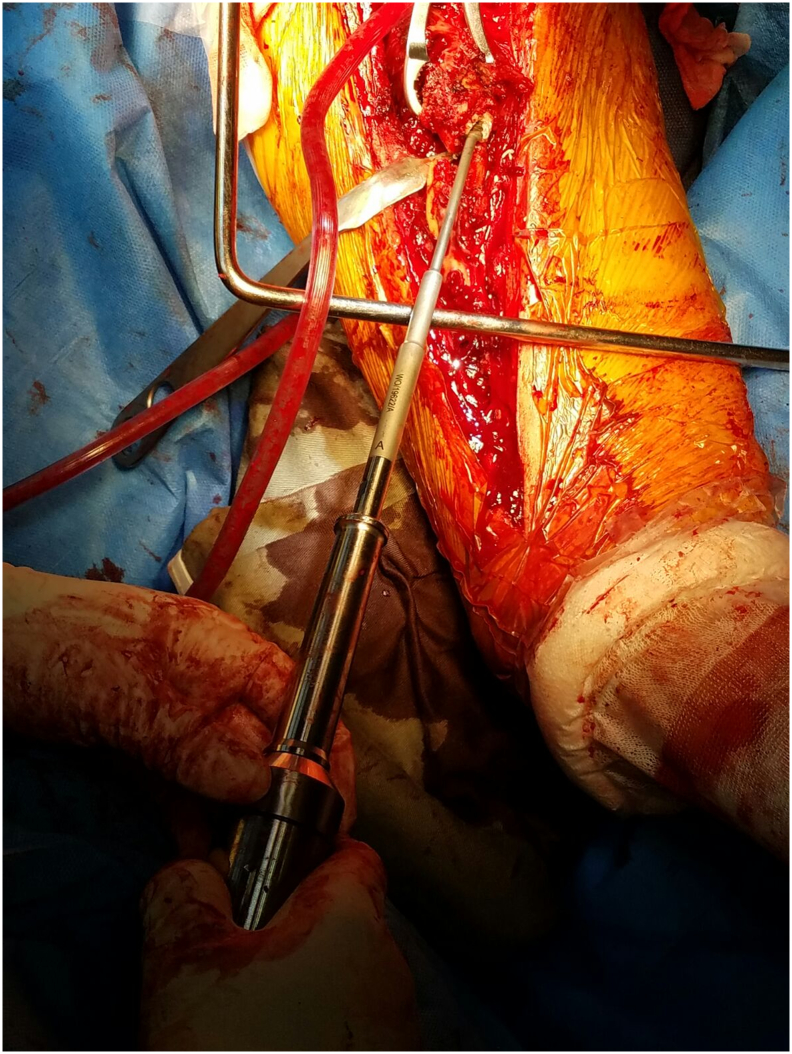
Fig. 5.
Intra-operative photo.
Fig. 6.
Radiograph (AP view) showing satisfactory fracture healing 6 months after the operation.
Fig. 7.
Radiograph (lateral view) showing satisfactory fracture healing 6 months after the operation.
Dual energy X-ray absorbsiometry (DEXA) revealed low T-score for the hip (−3.9), femoral neck (−3.0) and spine (−2.9). According to the World Health Organization Fracture Risk Assessment Tool (FRAX), her 10-year probability of major osteoporotic fracture was high: her FRAX score was 48 for major fracture risk and 36 for hip fracture risk. She was prescribed subcutaneous injection of teriparatide (Forteo) 20 μg daily for 18 months.
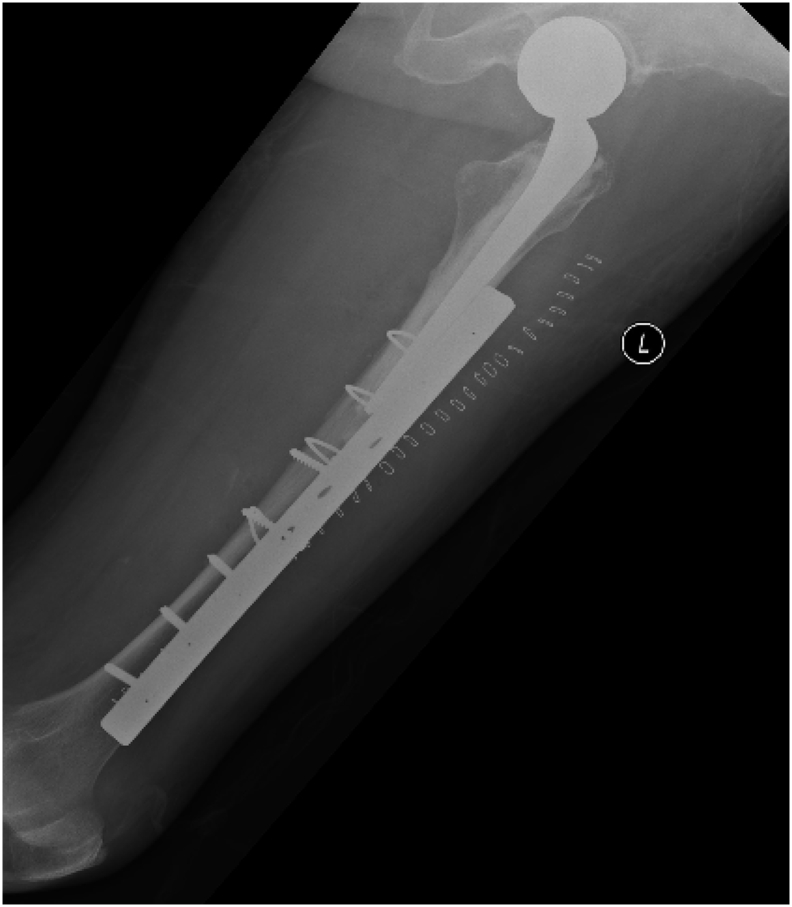
She was presented to us one year afterwards after a trivial fall injury. Radiographs revealed a new displaced periprosthetic fracture at the stem tip, proximal to the previous fracture site (Fig. 8, Fig. 9). Revision surgery was performed. The locking plate was removed. The fracture was fixed with pre-contoured long-spanning femur locking plate that covers the greater trochanter with complete overlapping with the stem (Fig. 10, Fig. 11, Fig. 12). Extra caution was given this time with regards to the post-operative weight bearing regime with 12 weeks of protected weight bearing.
Fig. 8.
Radiograph (AP view) showing a periprosthetic fracture around the stem tip.
Fig. 9.
Radiograph (lateral view) showing a periprosthetic fracture around the stem tip.
Fig. 10.
Revision fixation with pre-contoured long-spanning femur locking plate that covers the greater trochanter with complete overlapping with the stem (radiograph AP view).
Fig. 11.
Fig. 11: Revision fixation with pre-contoured long-spanning femur locking plate that covers the greater trochanter with complete overlapping with the stem (radiograph lateral view).
Fig. 12.
Intra-operative photo.
Radiograph one year later revealed non-union around the fracture site without displacement (Fig. 13, Fig. 14). Patient was a non-smoker. Blood tests revealed normal fasting glucose and inflammatory markers. She declined revision surgery because of improvement in pain. Four months afterwards she was admitted again for increasing left thigh pain. Radiograph revealed breakage of the locking plate with fracture displacement (Fig. 15, Fig. 16). There was sign of loosening over the femoral stem.
Fig. 13.
Radiograph (AP view) showing non-union over the fracture site without displacement.
Fig. 14.
Radiograph (latera view) showing non-union over the fracture site without displacement.
Fig. 15.
Radiograph (AP view) showing breakage of the locking plate with fracture displacement.
Fig. 16.
Radiograph (lateral view) showing breakage of the locking plate with fracture displacement.
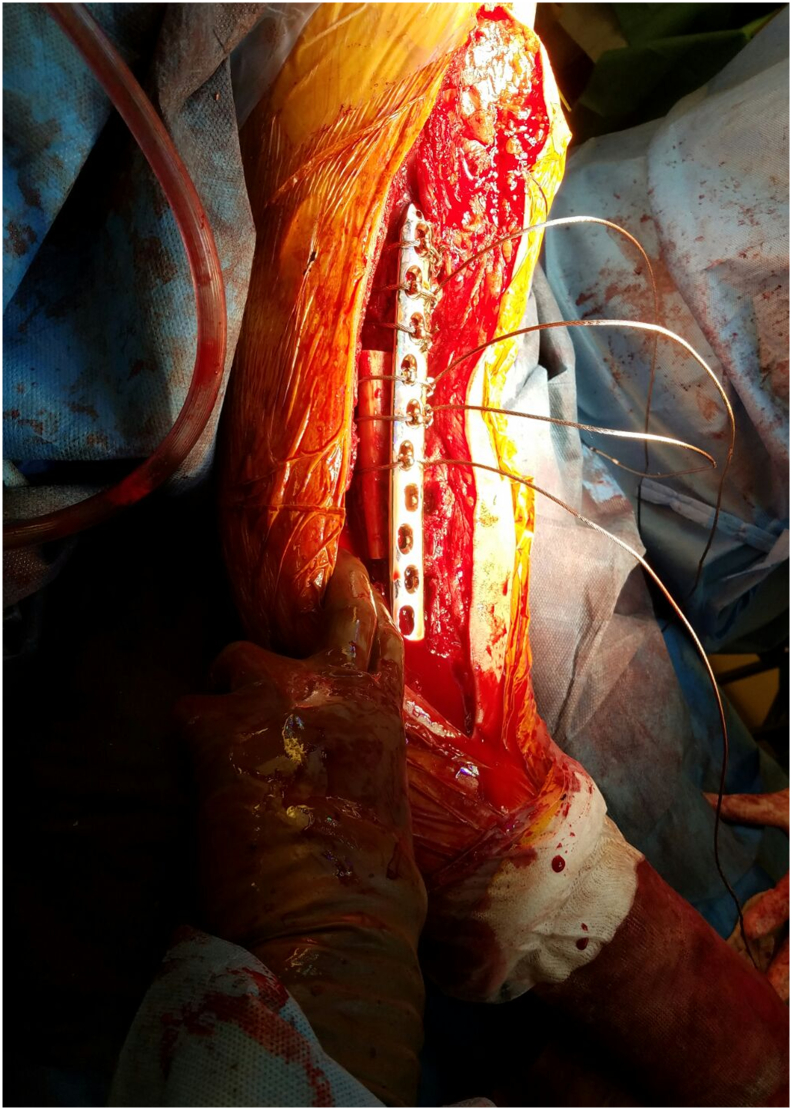
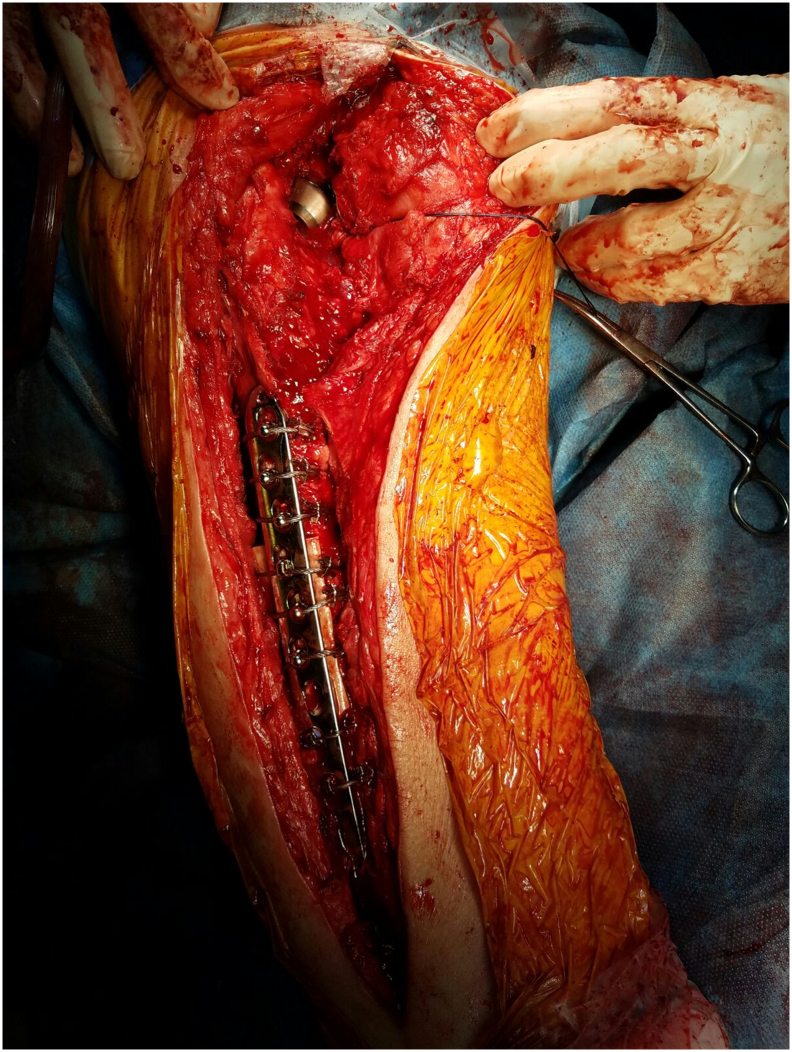
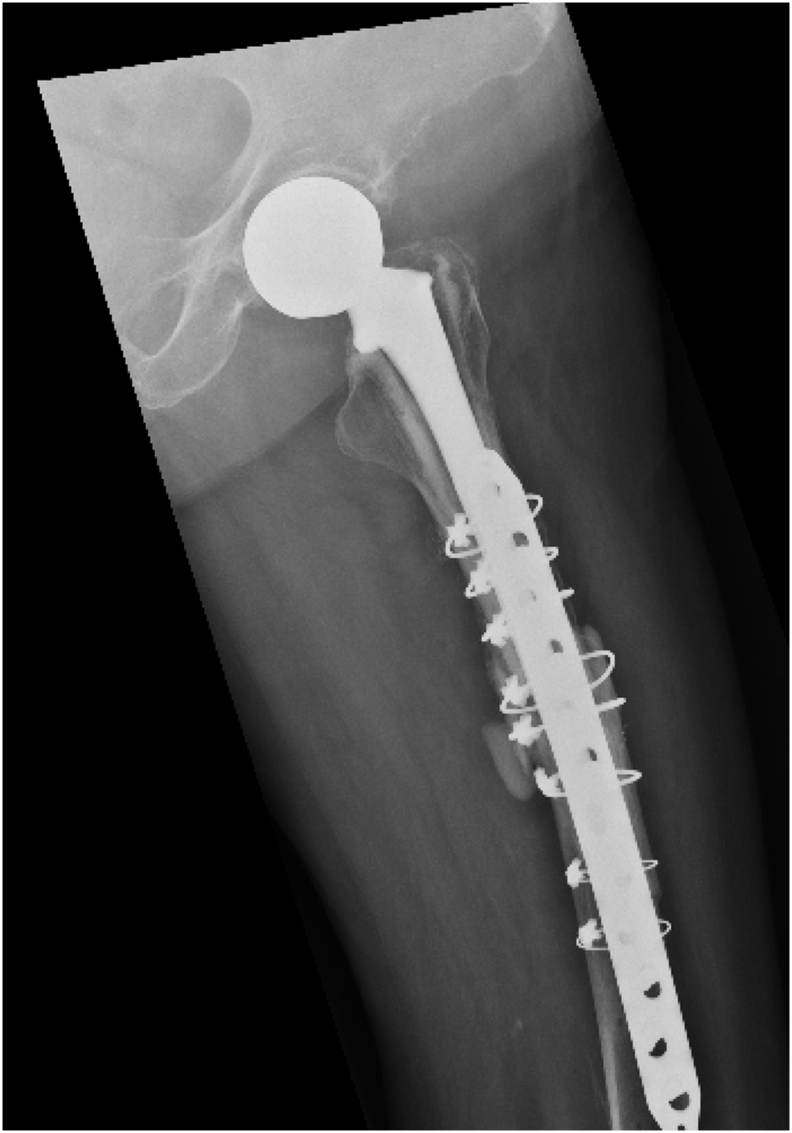
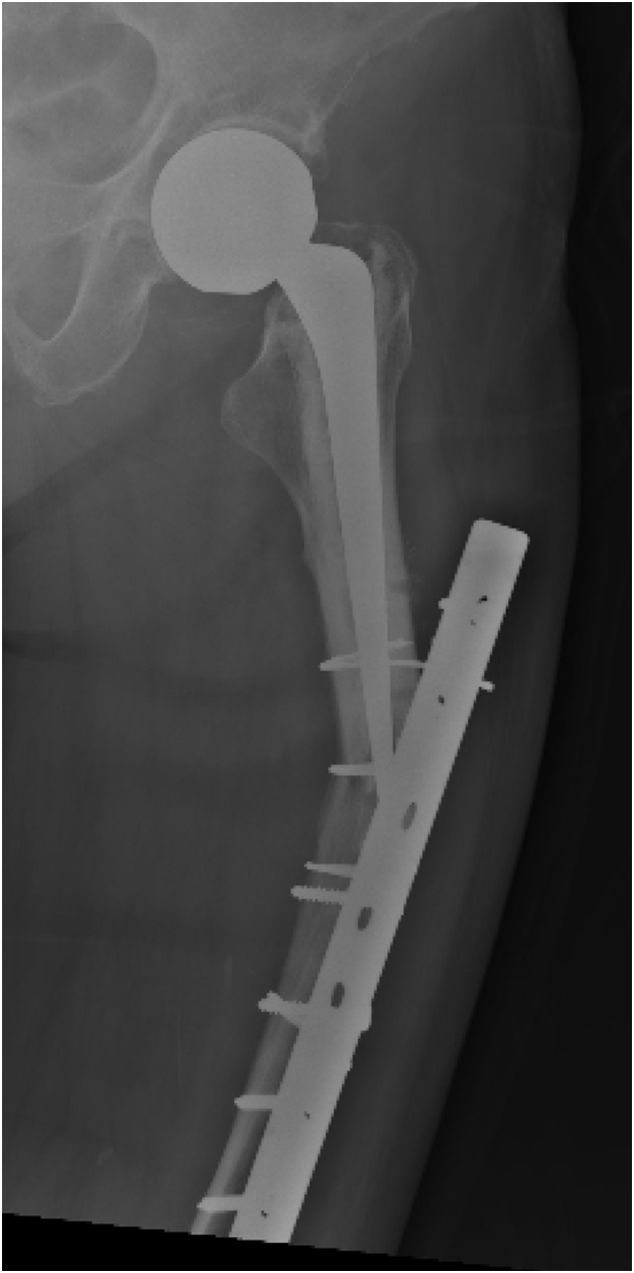
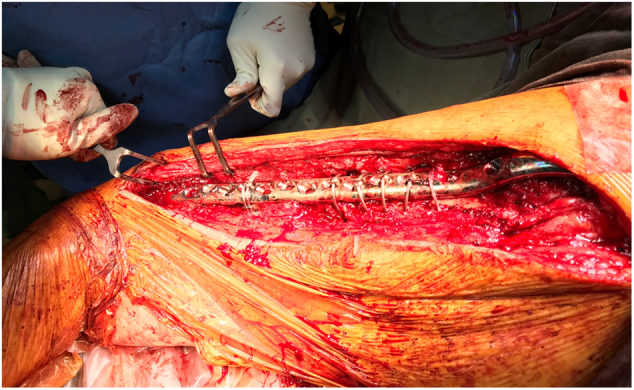
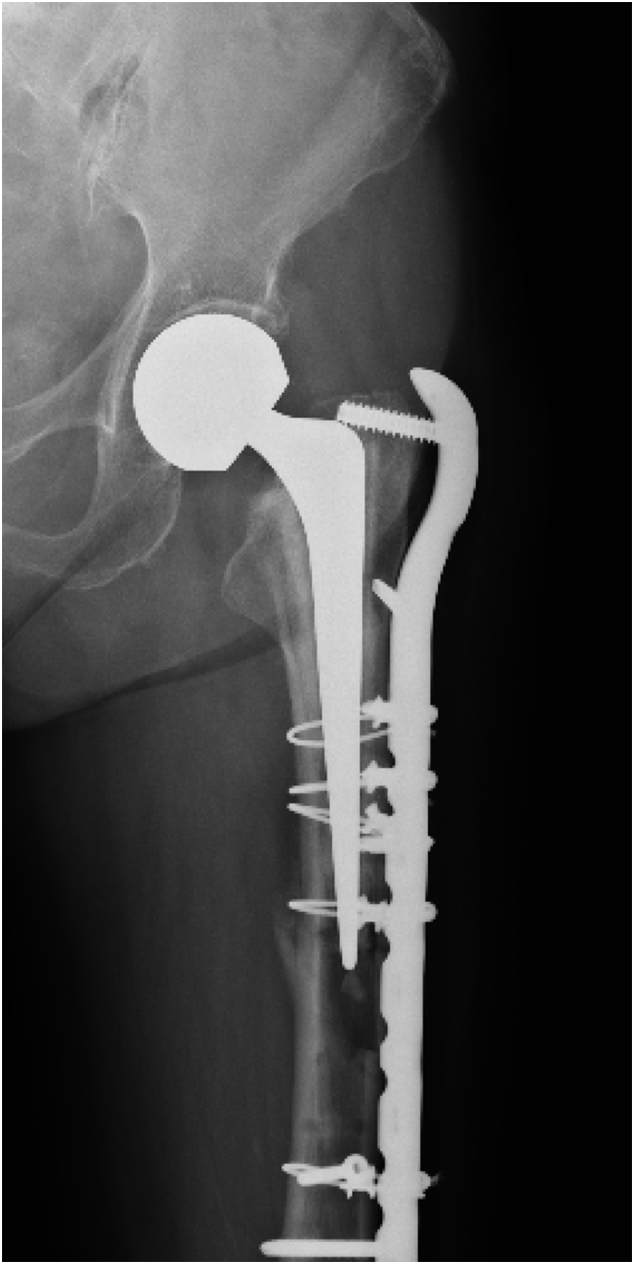
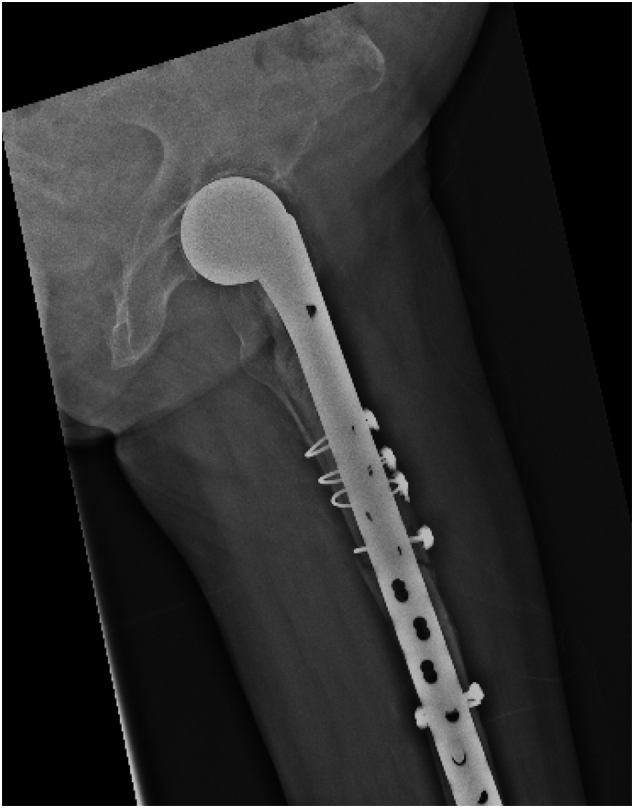
She underwent revision surgery and exchange of hip prosthesis with a long stem. The patient was put in a lateral decubitus position under general anaesthesia. Postero-lateral approach to the hip extended down from the previous incision. The cable locking plate was removed (Fig. 17, Fig. 18). The hip was dislocated posteriorly and the hip prosthesis was removed. Cement removal was performed with the assistance of OSCAR® 3 Ultrasonic System (Orthofix) (Fig. 19, Fig. 20), which was a system consisting of a probe to emit high frequency soundwaves to soften the cement. Cortical bone would not be affected due to then energy levels used. It did not absorb ultrasound as readily as cement and therefore the surgeon would have awareness of the position of the probe within the bone through both audible and tactile feedback. The nonunion site was debrided and the intramedullary portion was recanalized using drill bits. The fracture site was temporarily reduced with two Verbrugge clamps. The femur with reamed and a bowed long full-coated stem (Restoration; Stryker) was inserted. The construct was augmented with a long 4.5 mm metaphyseal locking compression plate (Depuy Synthes), spanning the fracture with four gripping cables over the proximal fragment, two gripping cables and three locking screws over the distal fragment. A piece of allograft, meticulously chiselled, was lodged into the fracture gap (Fig. 21, Fig. 22). Bone morphogenetic protein (BMP-2) strip was added to the fracture gap to further facilitate bone union.
Fig. 17.
Intra-operative photo showing a broken locking plate, which was removed together with the hip prosthesis.
Fig. 18.
Removal of the broken implants.
Fig. 19.
Intra-operative photos showing cement removal with the assistance of OSCAR.
Fig. 20.
Intra-operative photos showing cement removal with the assistance of OSCAR.
Fig. 21.
Intra-operative photos showing a piece of allograft was chiselled and lodged into the fracture gap.
Fig. 22.
Intra-operative photos showing a piece of allograft was chiselled and lodged into the fracture gap.
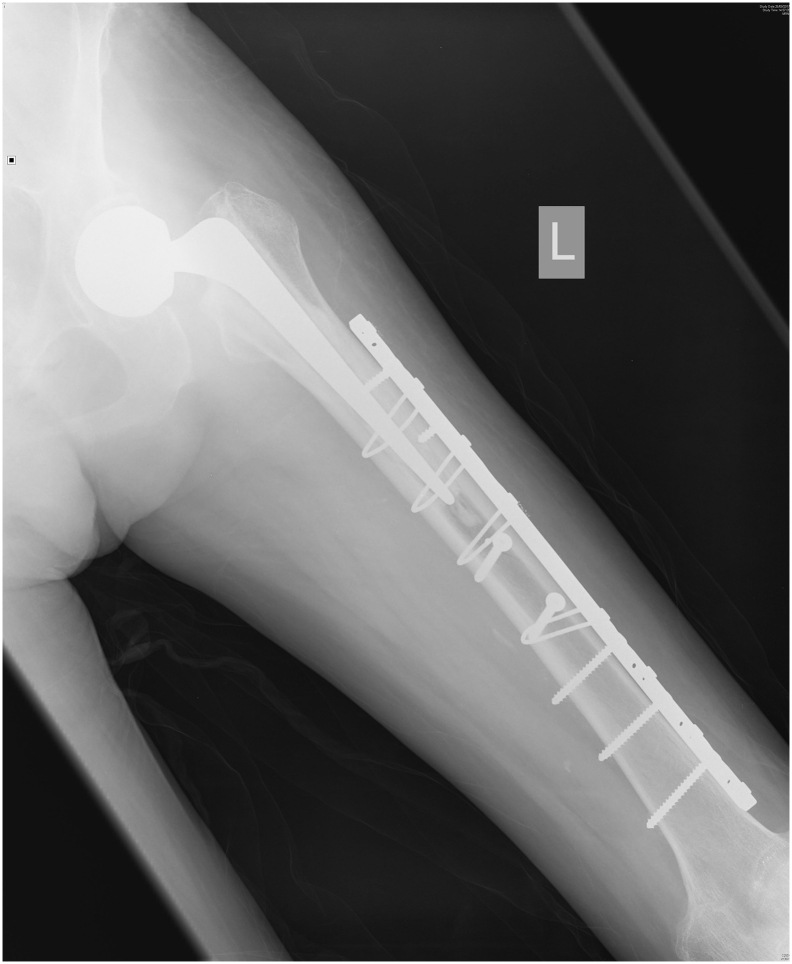
The patient was allowed protected weight bearing for 8 weeks and then full-wright bearing walking. At the one-year follow up, completed bone union was achieved (Fig. 13).
Discussions
Periprosthetic femoral fractures are increasingly common [[1], [2], [3], [4]] as a result of an ageing population and the increased numbers of hip arthroplasties performed, secondary to both trauma and degenerative conditions. Majority of the cases, including the aforementioned patient, have co-existing osteoporosis. The management of such fractures with suboptimal bone qualities is often complex and demanding (Fig. 23).
Fig. 23.
Radiograph (AP view) one year after the revision surgery showing stable bone union.
The Vancouver's classification is a reliable and relevant system for post-operative periprosthetic femoral fractures [5,6]. Factors including fracture location, implant stability, and the quality of the femoral bone stock are taken into account. Type B2 fractures with femoral stem loosening are typically treated with long stem revision, and open reduction internal fixation using cables and plates. Revision surgery should be considered for pain relief and restoration of the pre-operatively mobility status. Revision femoral stem passing the fracture with at least two cortical diameters should be used to prevent a stress riser. For fixation of long bone, it is preferable to have at least eight cortices screw purchase on each side of the fragment. But in this case, it is difficult to achieve because of presence of the canal filling stem. To tackle this, unicortical screws and cerclage cables can be used (Fig. 24).
Fig. 24.
Radiograph (lateral view) one year after the revision surgery showing stable bone union.
As in our patient with osteoporotic bone, an anatomically contoured locking plate can be used. As an ‘internal-fixator’ it is particularly beneficial for suboptimal bone quality when only unicortical screws are used. It serves as a fixed-angle device with improved pull-out strength.
There were a number of factors contributing to the non-union in our patient. The transverse fracture pattern after the first revision surgery was inherently unstable and difficult to treat with a stand-alone plate. The fracture was located at the watershed area between a stiff femoral stem and a pliable region distal to the stem tip. In addition, the patient had features of atypical fracture secondary to long-term bisphosphonate treatment, including thickened femoral cortex and transverse, short oblique fracture pattern. Having recognized the atypical bisphosphonate-related fracture patterns, we have tried to provide additional stability to the construct by using a pre-contoured, long-spanning locking plate extending proximally into the trochanteric region, with four bicortical screws and one gripping cable over the distal fragment. Unfortunately, the fixation was not strong and rigid enough to provide absolute stability for bone union. The refracture occurred at the stress riser area wherein the plate broke. This suggested that the plate has sustained a prolonged loading at this area, resulting in an occult fatigue failure just before the fracture occurred. Despite the two-cortical-diameter concept was applied, the number of cortices with screw purchase over the proximal fragment was deemed not sufficient in retrospect.
Bone morphogenetic protein (BMP) is a family of at least 20 glycoproteins able to stimulate ecotopic bone formation. Of which, BMP 2 and 7 have been found to possess independent osteoinductive activity [[8], [9], [10]].
In the last revision surgery for our patient, we tackled the problem by addressing both the biological and mechanical aspects of fracture healing. We provided biology by means of allograft and bone morphogenetic protein. We increased the rigidity of the construct with a long-spanning locking compression plate. Satisfactory bone union was achieved in the end and the patient could return to the community and enjoyed her well-deserved retirement. The successful outcome was also contributed by the long stem prosthesis bypassing the fracture site.
References
- 1.Berry D.J. Epidemiology: hip and knee. Orthop. Clin. N. Am. 1999;30(2):183–190. doi: 10.1016/s0030-5898(05)70073-0. [DOI] [PubMed] [Google Scholar]
- 2.Berry D.J. Periprosthetic fractures associated with osteolysis: a problem on the rise. J. Arthroplast. 2003;18(3 suppl 1):107–111. doi: 10.1054/arth.2003.50109. [DOI] [PubMed] [Google Scholar]
- 3.Lewallen D.G., Berry D.J. Periprosthetic fracture of the femur after total hip arthroplasty. Treatment and results to date. J. Bone Joint Surg. Am. 1997;79(12):1881–1890. [Google Scholar]
- 4.Lewallen D.G., Berry D.J. Periprosthetic fracture of the femur after total hip arthroplasty: treatment and results to date. Instr. Course Lect. 1998;47:243–249. [PubMed] [Google Scholar]
- 5.Duncan C.P., Masri B.A. Fractures of the femur after hip replacement. Instr. Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 6.Brady O.H., Garbuz D.S., Masri B.A., Duncan C.P. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J. Arthroplast. 2000;15:59–62. doi: 10.1016/s0883-5403(00)91181-1. [DOI] [PubMed] [Google Scholar]
- 7.The Osteoporosis Society of Hong Kong (OSHK) 2013 OSHK guideline for clinical management of postmenopausal osteoporosis in Hong Kong. Hong Kong Med. J. 2013:1–40. Apr. [PubMed] [Google Scholar]
- 8.Shen B., Wei A., Tao H., Diwan A.D., Ma D.D. BMP-2 enhances TGF-beta3-mediated chondrogenic differentiation of human bone marrow multipotent mesenchymal stromal cells in alginate bead culture. Tissue Eng. A. 2008;15:1311–1320. doi: 10.1089/ten.tea.2008.0132. [DOI] [PubMed] [Google Scholar]
- 9.Gori F., Thomas T., Hicok K.C., Spelsberg T.C., Riggs B.L. Differentiation of human marrow stromal precursor cells: bone morphogenetic protein-2 increases OSF2/CBFA1, enhances osteoblast commitment, and inhibits late adipocyte maturation. J. Bone Miner. Res. 1999;14:1522–1535. doi: 10.1359/jbmr.1999.14.9.1522. [DOI] [PubMed] [Google Scholar]
- 10.Ji X., Chen D., Xu C., Harris S.E., Mundy G.R., Yoneda T. Patterns of gene expression associated with BMP-2-induced osteoblast and adipocyte differentiation of mesenchymal progenitor cell 3T3-F442A. J. Bone Miner. Metab. 2000;18:132–139. doi: 10.1007/s007740050103. [DOI] [PubMed] [Google Scholar]