Abstract
Introduction
Obstructed hemivagina ipsilateral renal agenesis (OHVIRA) is a rare anomaly of the urogenital system. The characteristic triad of this syndrome, which was initially reported in 1950, is didelphys uterus, obstructed hemivagina, and ipsilateral renal agenesis (Embrey, 1950 [1]).
Case
A 17-year-old girl was referred with a 6-month history of offensive vaginal discharge. Magnetic resonance imaging (MRI) established the diagnosis of OHVIRA. She underwent surgery for drainage of the hematocolpos and excision of the vaginal septum followed by an uncomplicated recovery and the patient had normal menstrual cycles after surgery.
Conclusion
There should be a high suspicion of OHVIRA syndrome when encountering adolescent patients with non-specific abdominal or pelvic symptoms.
Keywords: Mullerian anomaly, Urogenital malformation, OHVIRA, Didelphys and bicollis, Obstructed hemivagina, Renal agenesis
Abbreviations: OHVIRA, Obstructed hemivagina ipsilateral renal agenesis; MRI, magnetic resonance imaging; USS, ultrasound scan
Highlights
-
•
The characteristic triad of this syndrome includes didelphys uterus, obstructed hemivagina, and ipsilateral renal agenesis.
-
•
Differentials of nonspecific abdominal symptoms with unilateral renal agenesis must include obstructive genital tract anomaly.
-
•
Early diagnosis and treatment is important to avoid complications.
1. Introduction
Obstructed hemivagina ipsilateral renal agenesis (OHVIRA) is a rare complex urogenital malformation. Clinical symptoms of this syndrome vary widely. OHVIRA should be considered as a differential diagnosis in young women and adolescents presenting with pelvic pain, tenderness, pelvic mass, persistent vaginal discharge, urinary symptoms and primary infertility. Strong suspicion and knowledge about this are important for accurate diagnosis. Clinical diagnosis is challenging and requires imaging studies; ultrasound scan (USS) and magnetic resonance imaging (MRI) play an essential role in diagnosis and treatment planning. Patients are usually diagnosed at puberty after menarche. Delayed diagnosis can lead to complications such as abscess formation, pelvic inflammatory disease, endometriosis, pyometra and infertility [2]. The differential diagnosis for unilateral kidney agenesis accompanied by non-specific abdominal symptoms in adolescent girls should include obstructive genital tract anomaly. Surgical removal of the vaginal septum (septostomy) is the main treatment method, outcomes of which are usually satisfactory. Expeditious surgical correction of the genital tract anomaly results in relief of symptoms.
2. Case Presentation
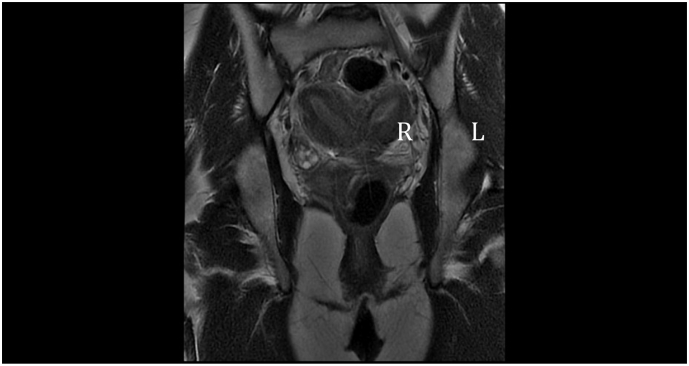
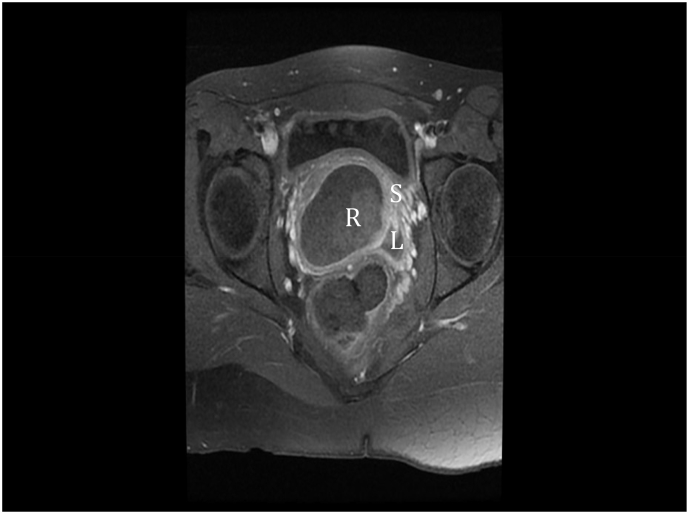
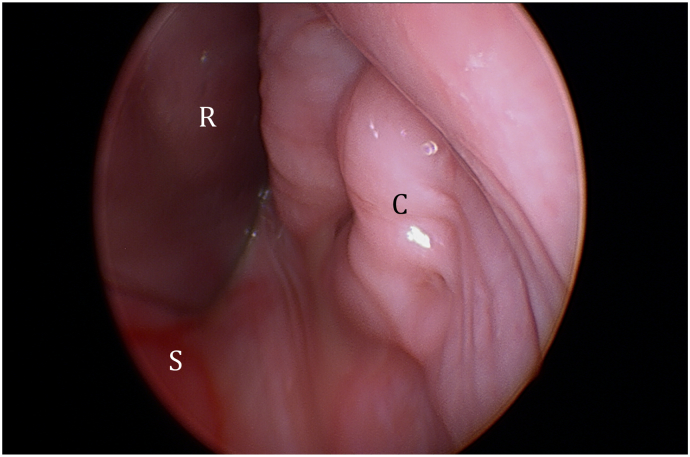
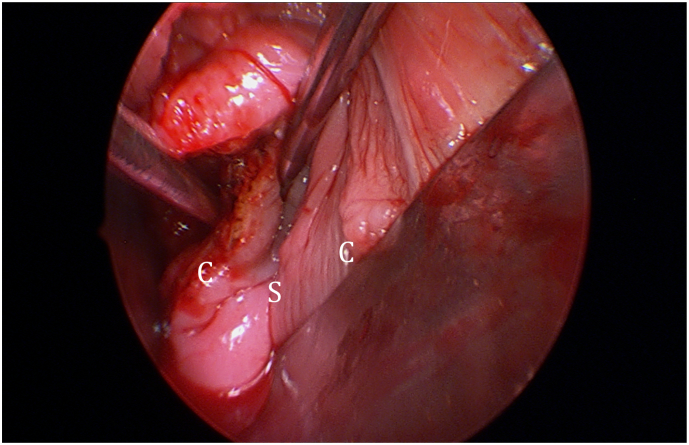
A 17-year-old female presented with a 6-month history of offensive vaginal discharge. She had achieved coitarche and used tampons with little concern. She did not have any significant medical or surgical history. She also denied dyspareunia, post-coital bleeding or urinary symptoms. Abdominal examination revealed mild lower abdominal tenderness without rebound or guarding. Vaginal examination demonstrated a bulge in the right upper vagina. USS findings were suspicious for right-sided renal agenesis and uterus didelphis. A subsequent MRI demonstrated the classical findings of right-sided OHVIRA. She had uterus didelphis (Fig. 1), bicolis and a right-sided obstructed hemivagina (Fig. 2). She underwent an examination under anesthetic (Fig. 3), hysteroscopy, incision and drainage of mucopyohaematoculpos and excision of vaginal septum (Fig. 4, Fig. 5). Intraoperative hysteroscopy confirmed uterus didelphis and bicolis. The septotomy was performed with a hand-held harmonic scalpel with minimal bleeding. There were no complications. She was discharged on day 1. Recovery was uncomplicated. At 6-week review, she had 1 normal menstrual cycle, no persistent abnormal vaginal discharge and normal coitus with no concerns.
Fig. 1.
MRI coronal view demonstrating left (L) and right (R) uterine horns with left and right vagina.
Fig. 2.
MRI transverse view demonstrating right obstructed hemivagina (R) with vaginal septum (S) and left vagina (L).
Fig. 3.
Retractor (R) against vaginal septum (S) and left cervix (C) exposed. (For interpretation of the references to color in this figure, the reader is referred to the web version of this article.)
Fig. 4.
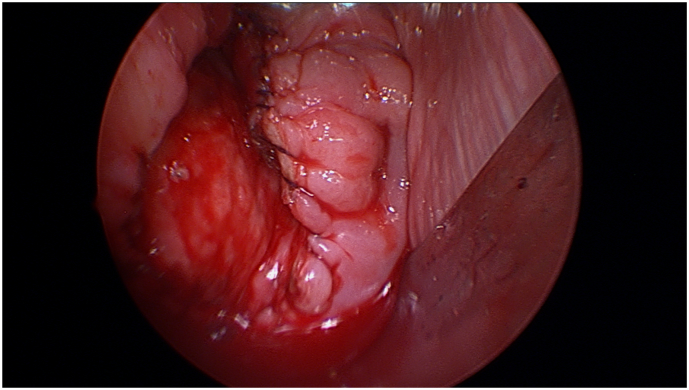
After excision of septum with dilator in both cervix. (For interpretation of the references to color in this figure, the reader is referred to the web version of this article.)
Fig. 5.
After entire septum excised and raw edges sutured. (For interpretation of the references to color in this figure, the reader is referred to the web version of this article.)
3. Discussion
Obstructed hemivagina ipsilateral renal agenesis (OHVIRA) is a rare form of Mullerian tract abnormality. The overall prevalence of Mullerian tract abnormality is 2% to 3% [3]. The incidence of OHVIRA syndrome is still unknown, with only few published case reports so far. Of note, Smith et al. reported 27 cases of OHVIRA and Candiani et al. reported long-term follow-up of 36 cases with double uterus, blind hemivagina and ipsilateral renal agenesis [4,5]. The characteristic triad of this syndrome is didelphys uterus, obstructed hemivagina, and ipsilateral renal agenesis [1]. The most common renal anomaly associated with this syndrome is renal agenesis, although other forms of renal malformations have been reported, including dysplastic kidney and renal duplication [5].
The pathogenesis of OHVIRA syndrome is thought to be multifactorial. It is related to an anomaly in development of paramesonephric (Mullerian) and mesonephric (Wolffian) ducts. The Wolffian ducts induce the normal development of Mullerian ducts and give origin to the kidneys. Abnormal development of the Wolffian ducts leads to the unilateral renal agenesis and imperforated hemivagina associated with OHVIRA syndrome [6]. Fusion failure of the Mullerian ducts leads to uterine didelphys and bicollis. Due to embryological development of the female urinary and reproductive symptoms, patients with renal malformations will benefit from evaluation of the reproductive structures and vice versa.
The clinical presentation of Mullerian duct anomaly varies widely in symptoms and age at onset. A number of presentations have been reported, including pre-pubertal with urinary incontinence [7], adolescence with dysmenorrhea, difficulty with sexual intercourse or using a tampon, as well as delayed diagnosis in pregnancy due to cervical incompetence [8] and a rare case of a ruptured gravid uterus [9]. Early diagnosis is important to relieve symptoms and to avoid adverse effects. Timely treatment will prevent adverse obstetric outcomes such as miscarriage, preterm birth, malpresentation, fetal growth restriction and cesarean delivery [10,11]. Preconception counseling is important, as is antenatal care in a high-risk setting. Associated renal anomalies also confer an increased risk of hypertensive disease in pregnancy as well as long-term implications for chronic renal and cardiovascular disease [12].
Given the association with a variety of renal tract anomalies, including ectopic ureters, consideration should be given to pre-operative renal tract imaging to prevent the risk of iatrogenic urinary incontinence, should the ureter implant into the subsequently unobstructed vagina [13]. In addition, it may be time to address whether the term ‘agenesis’ should be changed to ‘anomaly’ due to the variety of renal tract anomalies associated with OHVIRA.
First line of investigation for pelvic symptoms is usually an ultrasound scan, as it is easily available. However, MRI remains the imaging modality of choice to evaluate Mullerian duct abnormalities. MRI will accurately show the shape of uterine cavity, contour, cervical and vaginal abnormalities. Pre-operative imaging with MRI is essential to define the Mullerian duct structures and renal tract. It also assists with surgical planning [14]. Laparoscopy is still the gold standard for investigation of gynecological congenital abnormalities but is only used if MRI fails to establish a diagnosis or MRI is unavailable [15].
Treatment of OHVIRA is vaginoplasty. It is ideally a single surgery with drainage of the obstructed hemivagina and resection of the septum to restore normal vaginal function.
4. Conclusion
Gynecologists, pediatricians and radiologists should have high suspicion for OHVIRA syndrome when encountering adolescent patients with non-specific abdominal or pelvic symptoms. Knowledge of the syndrome is important for early diagnosis as well as an appropriate early treatment to avoid adverse effects.
Acknowledgments
Contributors
All three authors were involved in literature review, design of the case report, obtaining consent from the patient and writing the case report.
Conflict of Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Funding
No funding from an external source supported the publication of this case report.
Patient Consent
The patient described in this case study provided written informed consent. The report presented here was reviewed by the Chair of the relevant Ethics Committee and deemed to constitute a case study that does not require further ethical review.
Provenance and Peer Review
This case report was peer reviewed.
References
- 1.Embrey M.P. A case of uterus didelphys with unilateral gynatresia. Br. Med. J. 1950;1(4657):820. doi: 10.1136/bmj.1.4657.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cox D., Ching B.H. Herlyn-Werner-Wunderlich syndrome: a rare presentation with pyocolpos. J. Radiol. Case Rep. 2012;6(3):9. doi: 10.3941/jrcr.v6i3.877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Shavell V.I., Montgomery S.E., Johnson S.C., Diamond M.P., Berman J.M. Complete septate uterus, obstructed hemivagina, and ipsilateral renal anomaly: pregnancy course complicated by a rare urogenital anomaly. Arch. Gynecol. Obstet. 2009;280(3):449–452. doi: 10.1007/s00404-008-0919-6. [DOI] [PubMed] [Google Scholar]
- 4.Candiani G.B., Fedele L., Candiani M. Double uterus, blind hemivagina, and ipsilateral renal agenesis: 36 cases and long-term follow-up. Obstet. Gynecol. 1997;90(1):26–32. doi: 10.1016/S0029-7844(97)83836-7. [DOI] [PubMed] [Google Scholar]
- 5.Smith N.A., Laufer M.R. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: management and follow-up. Fertil. Steril. 2007;87(4):918–922. doi: 10.1016/j.fertnstert.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 6.Ugurlucan F.G., Bastu E., Gulsen G., Eken M.K., Akhan S.E. OHVIRA syndrome presenting with acute abdomen: a case report and review of the literature. Clin. Imaging. 2014;38(3):357–359. doi: 10.1016/j.clinimag.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 7.Ma I., Williamson A., Rowe D., Ritchey M., Graziano K. OHVIRA with a twist: obstructed hemivagina ipsilateral renal anomaly with urogenital sinus in 2 patients. J. Pediatr. Adolesc. Gynecol. 2014;27(2):104–106. doi: 10.1016/j.jpag.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 8.Muraoka A., Tsuda H., Kotani T., Kikkawa F. Severe hemoperitoneum during pregnancy with obstructed hemivagina and ipsilateral renal anomaly syndrome: a case report. J. Reprod. Med. 2016;61(5–6):290–294. [PubMed] [Google Scholar]
- 9.Mizutamari E., Honda T., Ohba T., Katabuchi H. Spontaneous rupture of an unscarred gravid uterus in a primigravid woman at 32 weeks of gestation. Case Rep. Obstet. Gynecol. 2014;2014 doi: 10.1155/2014/209585. https://www.hindawi.com/journals/criog/2014/209585/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Del Vescovo R., Battisti S., Di Paola V., Piccolo C.L., Cazzato R.L., Sansoni I.…Zobel B.B. Herlyn-Werner-Wunderlich syndrome: MRI findings, radiological guide (two cases and literature review), and differential diagnosis. BMC Medical Imaging. 2012;12(1):4. doi: 10.1186/1471-2342-12-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gholoum S., Puligandla P.S., Hui T., Su W., Quiros E., Laberge J.M. Management and outcome of patients with combined vaginal septum, bifid uterus, and ipsilateral renal agenesis (Herlyn-Werner-Wunderlich syndrome) J. Pediatr. Surg. 2006;41(5):987–992. doi: 10.1016/j.jpedsurg.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 12.Heinonen P.K. Gestational hypertension and preeclampsia associated with unilateral renal agenesis in women with uterine malformations. Eur. J. Obstet. Gynecol. Reprod. Biol. 2004;114(1):39–43. doi: 10.1016/j.ejogrb.2003.10.030. [DOI] [PubMed] [Google Scholar]
- 13.Schlomer B., Rodriguez E., Baskin L. Obstructed hemivagina and ipsilateral renal agenesis (OHVIRA) syndrome should be redefined as ipsilateral renal anomalies: cases of symptomatic atrophic and dysplastic kidney with ectopic ureter to obstructed hemivagina. J. Pediatr. Urol. 2015;11(2) doi: 10.1016/j.jpurol.2014.12.004. 77-e1. [DOI] [PubMed] [Google Scholar]
- 14.Tanaka Y.O., Kurosaki Y., Kobayashi T., Eguchi N., Mori K., Satoh Y.…Itai Y. Uterus didelphys associated with obstructed hemivagina and ipsilateral renal agenesis: MR findings in seven cases. Abdominal imaging. 1998;23(4):437–441. doi: 10.1007/s002619900375. [DOI] [PubMed] [Google Scholar]
- 15.Park N.H., Park H.J., Park C.S., Park S.I. Herlyn-Werner-Wunderlich syndrome with unilateral hemivaginal obstruction, ipsilateral renal agenesis, and contralateral renal thin GBM disease: a case report with radiological follow up. J. Korean Soc. Radiol. 2010;62(4):383–388. [Google Scholar]