Abstract
Purpose
To highlight the surgical and medical management used in an extensive globe penetrating injury caused by an acupuncture needle.
Observations
We report on a case of acupuncture treatment error resulting in needle penetration of the eye, retinal detachment, and progressive post-traumatic proliferative vitreoretinopathy (PVR). This patient required aggressive surgical management with multiple vitrectomies along with adjunctive intravitreal methotrexate to control ongoing PVR. At last follow-up, 15 months after presentation, the patient's BCVA was 20/40 and the periphery was flat with fibrosis stable.
Conclusions and Importance
Open globe injuries are a subtype of ocular trauma which can cause irreparable vision loss. This case highlights the extensive potential complications which can occur following traumatic injury to the retina and choroid, as well as the role of both surgical and medical management of retinal detachment and PVR. In addition, this is the first report of the use of off-label adjunctive intravitreal methotrexate to control post-traumatic PVR. Further research into this treatment approach could reveal a role of adjunctive methotrexate in the management of such injuries.
Keywords: Acupuncture, Globe penetration, Retinal detachment, Proliferative vitreoretinopathy, Methotrexate
1. Introduction
Open globe injuries are a dangerous form of ocular trauma and can cause irreparable vision loss.1 These injuries can damage any structure of the eye and give rise to several complications including hypotony, increased intraocular pressure (IOP), cataract, endophthalmitis, optic nerve damage, retinal tears and detachment, and proliferative vitreoretinopathy (PVR).2, 3, 4, 5, 6 Risk factors for poor, even no light perception, vision in globe injuries include rupture, wounds posterior to the limbus, damage to the ciliary body and choroid, severe intraocular hemorrhage, closed funnel retinal detachment, and retinal prolapse.1
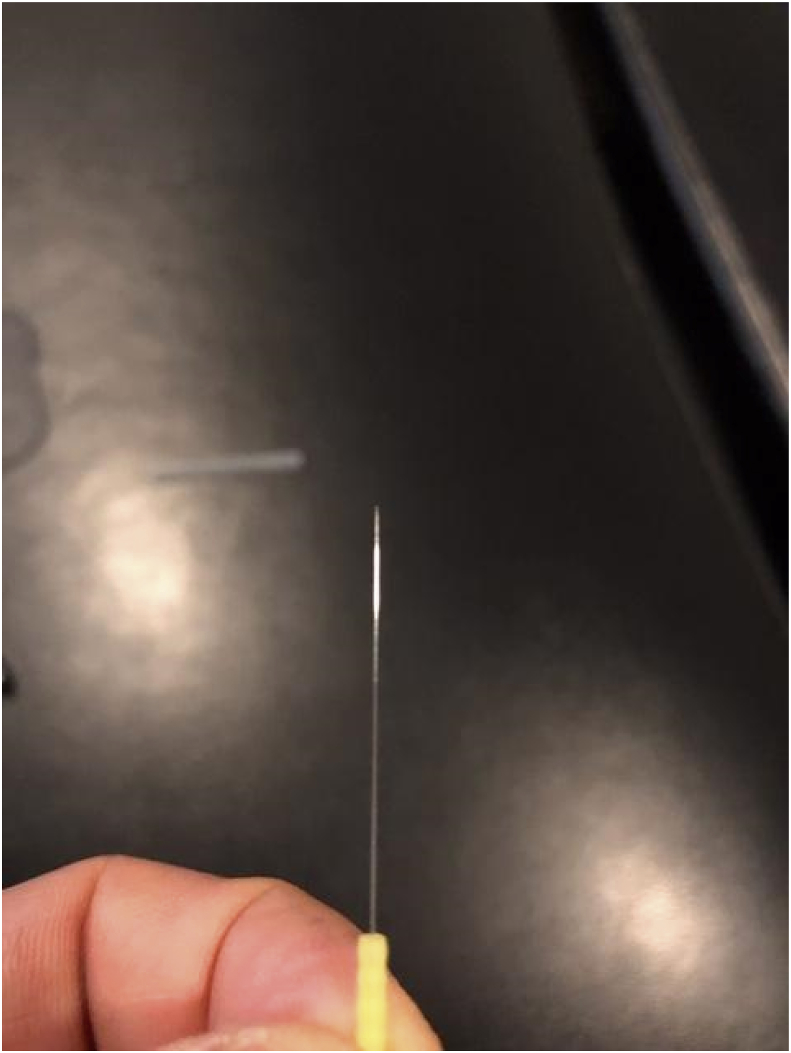
Penetrating or perforating needle injuries to the eye can cause a variety of complications influenced by the site of injury, type of needle, and ocular structures involved. Scleral penetrations and perforations are a known complication of peribulbar injections and procedures such as strabismus surgery, and rarely from other needle injuries. Iatrogenic scleral penetration by needles commonly results in retinal tears and detachments.5,7,8 Acupuncture needles have thin diameters, ranging from 0.12 mm to 0.25 mm, allowing them to slide between muscle fibers (Fig. 1). Due to this thin diameter, acupuncture needles are much more flexible than typical hypodermic needles.
Fig. 1.
Example of typical acupuncture needle.
Management of globe penetrating needle injuries is guided by the injury mechanism and sequelae of post traumatic complications. When PVR develops, adjunctive pharmacological treatments have been used including steroids and anti-neoplastic agents.10 Off-label intravitreal methotrexate has also been shown to be effective in reducing incidence of PVR in one case series of retinal detachment patients.11 We present a case of retinal detachment and post-traumatic PVR caused by a scleral penetrating injury with an acupuncture needle. This patient was managed with multiple vitrectomies and adjunctive intravitreal methotrexate for progressive PVR.
2. Case report
A 49-year-old woman presented to our center with a 3-h history of pain and vision loss in her left eye. She was undergoing acupuncture treatment for left-sided headache with needles being inserted around the orbital rim. She described acute pain, red eye, and loss of vision in the left eye. She was referred to our centre for assessment and management. Besides a recent root canal dental procedure, for which she was on amoxicillin, she was otherwise healthy and had no allergies. Her past ocular history was positive for a metallic foreign body in her cornea which had been removed years prior with no sequelae. She had no previous ocular surgeries.
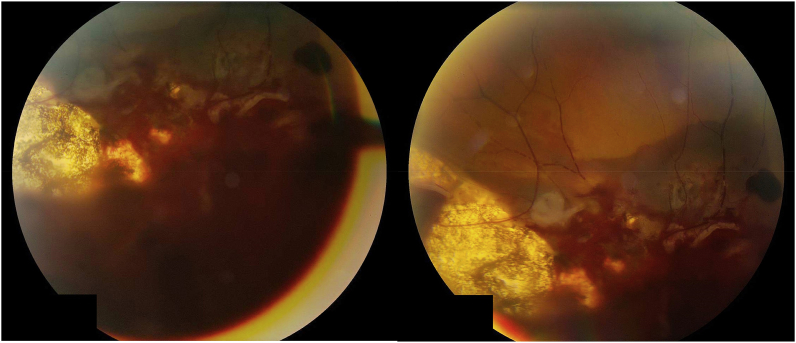
On initial examination, her best corrected visual acuity (BCVA) was 20/20 in the right eye and light perception in the left. IOP by Goldmann applanation was 15 mmHg in the right and 8 mmHg in the left. Anterior segment examination of the left eye revealed a 180-degree subconjunctival hemorrhage from 6:00 to 12:00 on the nasal side which was Seidel negative. The anterior chamber had 4+ cell (SUN Uveitis Criteria) and significant fibrin material. The cornea and lens appeared clear, with no visible entry sites. Posterior segment examination showed a dense vitreous hemorrhage with a large area of white material nasal to the disc presumed to be bare sclera (Fig. 2). An urgent diagnostic and therapeutic 25-gauge pars plana vitrectomy was performed to seal the entry site and repair the presumed retinal injury.
Fig. 2.
Posterior segment photographs on first day of presentation.
The subconjunctival space was explored for occult perforation. No entry site was found anterior to the equator. Under widefield visualization, a posterior vitreous detachment was induced, and the significant vitreous hemorrhage removed. Nasal to the disc, a large area of bare sclera was visible with overlying loss of the retina and choroid, extending almost from the ora serrata to the nasal side of the disc. A significant subretinal hemorrhage was present. Decalin (C10H18) was instilled to protect the fovea and an air-fluid exchange was performed to flatten the periphery allowing for endolaser to be applied around the large retinal tears. The decalin was removed via an air-fluid exchange and the eye filled with silicone oil.
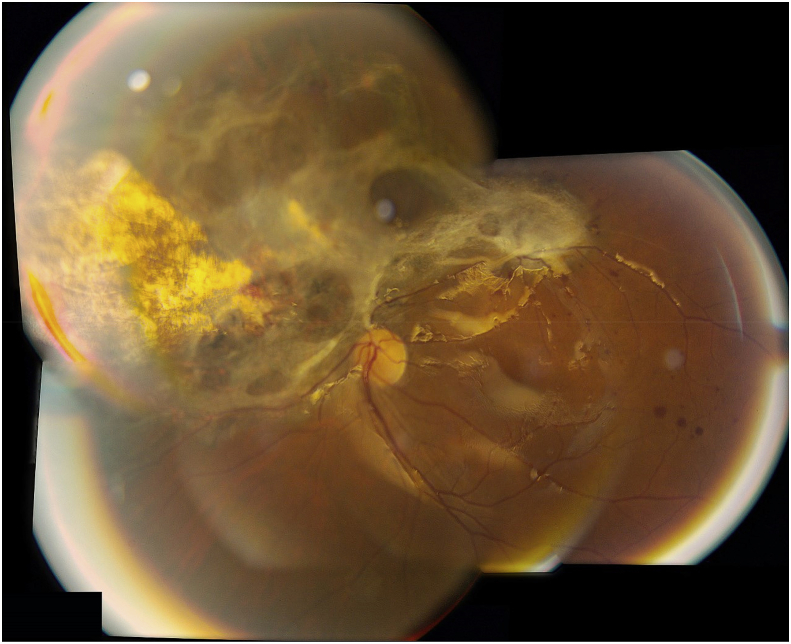
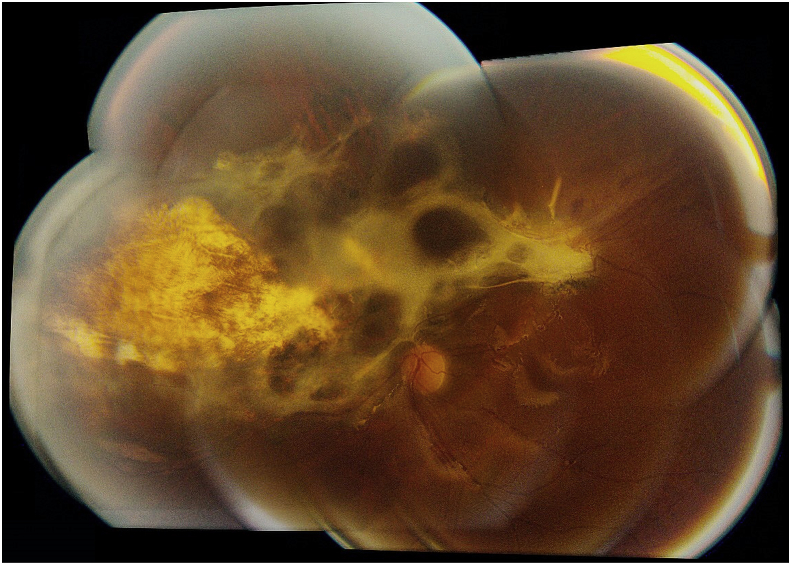
One-month post-op the BCVA was count fingers in the affected eye with considerable PVR along the superior arcade. The patient was consented for a second vitrectomy, epiretinal membrane peel, and silicone oil exchange with administration of intravitreal triamcinolone acetonide. Five weeks post-op, the retina was flat with a BCVA of 20/400, but PVR had recurred with significant fibrosis prompting the initiation of intravitreal methotrexate treatment (Fig. 3). Intravitreal 200 μg/0.1mL methotrexate injections were initiated every 2–3 weeks for a total of 9 treatments. Six months after presentation, the BCVA was 20/40 and the macula was flat and fibrosis stable without progression following initiation of methotrexate (Fig. 4). Ten months following presentation, the patient underwent phacoemulsification and intraocular lens implant for cataract and removal of significant membranous proliferation. Further installation of silicone oil was deemed necessary due to the extent of the ongoing PVR and traction seen superior-temporally in Fig. 5.
Fig. 3.
Posterior segment photograph 5 weeks after second vitrectomy demonstrating significant development of fibrosis following resolution of the hemorrhage.
Fig. 4.
Posterior segment photograph 6 months after initial presentation showing no progression of fibrosis following methotrexate injection.
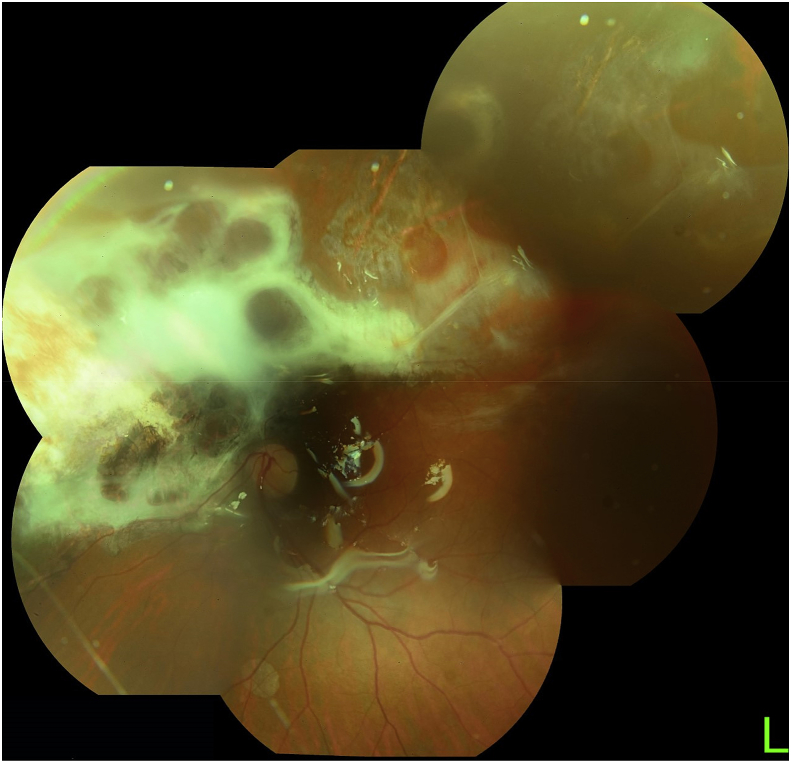
Fig. 5.
Posterior segment photo 12 months after initial injury and 2 months after phacoemulsification, intraocular lens implant and pars plana victrectomy. Note progressive fibrosis superior-temporally without methotrexate.
At last follow-up, 15 months after presentation, the patient's BCVA was 20/40 and the periphery was flat with fibrosis stable. The IOP was elevated at 30 mmHg OS and a combination brimonidine tartrate 0.2% and timolol 0.5% drop were added to control IOP.
3. Discussion
This case report of a 49-year-old woman with a scleral penetrating injury during periorbital acupuncture treatment highlights the severity of the fibrosis and PVR which can develop following traumatic injuries to the retina and choroid. Furthermore, we observed a cessation of progression of PVR following initiation of methotrexate. These findings may suggest a clinical benefit of methotrexate in controlling PVR. Previous cases of acupuncture needle injury to the eye have been reported.9,12, 13, 14 A corneal penetrating injury caused anterior and posterior capsule rupture and traumatic cataract, requiring phacoemulsification, anterior vitrectomy and intraocular lens implant.12 Another patient with penetrating retinal hole induced by an acupuncture needle and a VA of 20/100 in the affected eye, was managed and recovered vision to VA 20/25 following argon laser photocoagulation treatment.13 In a third case, the needle entered the subretinal space, forming a long subretinal tract with no other subsequent sequelae.9 This formation of a long subretinal tract is an unusual injury and has not been reported in penetrating eye injuries with other needle types. The authors speculate that the flexibility of acupuncture needles allowed for the needle to penetrate and track through the potential subretinal space. Physical characteristics of needles such as diameter and flexibility may therefore influence the pattern of damage caused to ocular structures. Lastly, a patient presented with two full-thickness posterior segment wounds and retinal laceration caused by acupuncture needle to the right eye with a VA OD of 20/50. The patient underwent vitrectomy with laser photocoagulation and air-fluid gas exchange without complication.14 One-month post-op, the VA OD was 20/40 and the periphery was flat.
In our case, the patient had trauma to a large area of retina and choroid, inciting significant PVR following surgery. The patient required multiple vitrectomies and a series of intravitreal methotrexate injections. Given the nature of the injury of a penetration, there was concern about significant scarring of Tenon's capsule and conjunctiva. Since the posterior entry site of the acupuncture needle was stable, a clinical decision was made to not open the sub-tenon space and proceed with an intraocular approach. Therefore, multiple vitrectomy attempts were made, and a scleral buckle was not employed. We used a 200 μg/0.1mL dose of methotrexate, based on previous safety reports of intravitreal methotrexate use in silicone-filled eyes.15 A typical dose of 400 μg/0.1mL methotrexate used as an adjunctive treatment in primary CNS lymphoma is safe in eyes without silicone oil.16 Silicone-filled eyes may exhibit delayed clearance of low molecular weight drugs such as methotrexate.15 Sadaka et al. reported potential benefits of methotrexate intraocular infusion during surgery in the management of retinal detachment patients at risk for PVR in a retrospective review of 29 eyes.11 The authors describe the rationale for this infusion method as a way to address unpredictability of drug concentration achieved in eyes with silicone oil or gas bubble tamponade. In a case series of 5 patients with complex retinal detachment caused by PVR, relaxing retinectomy with perfluorocarbon tamponade and adjunctive 100–200 μg/0.05mL intravitreal methotrexate yielded good visual outcomes.17 Our patient responded well to aggressive surgical management and adjunctive methotrexate injections and has maintained a BCVA of 20/40 fifteen months after presentation.
4. Conclusion
This case highlights the importance of aggressive surgical management of traumatic retinal injuries and subsequent PVR. Furthermore, we report on the use of adjunctive intravitreal methotrexate to help control PVR. Further study into the potential risks and benefits of such treatment in the form of randomized controlled trials would be required to determine the potential role of this treatment in such cases.
Patient consent
Written consent to publish this case has not been obtained. This report does not contain any personal identifying information.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
The following authors have no financial disclosures: JD, DCS, VD, TGS.
Acknowledgements
The authors would like to thank Chris Lincoln and Nicole Ronald for ophthalmic photography and the Ivey Eye Institute for research support.
References
- 1.Feng K., Hu Y.T., Ma Z. Prognostic indicators for No light perception after open-globe injury: eye injury vitrectomy study. Am J Ophthalmol. 2011 Oct;152(4):654–662. doi: 10.1016/j.ajo.2011.04.004. https://linkinghub.elsevier.com/retrieve/pii/S0002939411003151 cited 2019 Feb 28. e2. Available from: [DOI] [PubMed] [Google Scholar]
- 2.Rabiah P.K. Penetrating needle injury of the eye causing cataract in children. Ophthalmology. 2003;110(1):173–176. doi: 10.1016/s0161-6420(02)01717-7. http://www.sciencedirect.com/science/article/pii/S0161642002017177 Available from: [DOI] [PubMed] [Google Scholar]
- 3.Faghihi H., Hajizadeh F., Esfahani M.R. Posttraumatic endophthalmitis. Retina. 2012 Jan;32(1):146–151. doi: 10.1097/IAE.0b013e3182180087. https://insights.ovid.com/crossref?an=00006982-201201000-00021 cited 2019 Feb 28. Available from: [DOI] [PubMed] [Google Scholar]
- 4.Nili-Ahmadabadi M., Faghihi H., Hadjizadeh F., Rasoolinejad S.A., Rajabi M.T. Penetrating needle injury of the eye. Injury. 2009 May;40(5):545–547. doi: 10.1016/j.injury.2007.08.039. https://linkinghub.elsevier.com/retrieve/pii/S0020138307003646 cited 2019 Feb 28. Available from: [DOI] [PubMed] [Google Scholar]
- 5.Schrader W.F., Schargus M., Schneider E., Josifova T. Risks and sequelae of scleral perforation during peribulbar or retrobulbar anesthesia. J Cataract Refract Surg. 2010 Jun;36(6):885–889. doi: 10.1016/j.jcrs.2009.12.029. https://linkinghub.elsevier.com/retrieve/pii/S0886335010003615 cited 2019 Feb 28. Available from: [DOI] [PubMed] [Google Scholar]
- 6.Jonas J.B., Knorr H.L.J., Budde W.M. Prognostic factors in ocular injuries caused by intraocular or retrobulbar foreign bodies. Ophthalmology. 2000;107(5):823–828. doi: 10.1016/s0161-6420(00)00079-8. http://www.sciencedirect.com/science/article/pii/S0161642000000798 Available from: [DOI] [PubMed] [Google Scholar]
- 7.Dang Y., Racu C., Isenberg S.J. Scleral penetrations and perforations in strabismus surgery and associated risk factors. J Am Assoc Pediatr Ophthalmol Strabismus. 2004;8(4):325–331. doi: 10.1016/j.jaapos.2004.03.003. http://www.sciencedirect.com/science/article/pii/S1091853104000497 Available from: [DOI] [PubMed] [Google Scholar]
- 8.Wagner R.S., Nelson L.B. Complications following strabismus surgery. Int Ophthalmol Clin. 1985;25(4):171–178. doi: 10.1097/00004397-198502540-00016. https://insights.ovid.com/crossref?an=00004397-198502540-00016 cited 2019 Feb 28. Available from: [DOI] [PubMed] [Google Scholar]
- 9.You T.T., Youn D.W., Maggiano J., Chen S., Alexandrescu B., Casiano M. Unusual ocular injury BY an acupuncture needle. Retin Cases Brief Rep. 2014;8(2):116–119. doi: 10.1097/ICB.0000000000000018. http://insights.ovid.com/crossref?an=01271216-201400820-00009 cited 2019 Mar 21. Available from: [DOI] [PubMed] [Google Scholar]
- 10.Khan M.A., Brady C.J., Kaiser R.S. Clinical management OF proliferative vitreoretinopathy. Retina. 2015 Feb;35(2):165–175. doi: 10.1097/IAE.0000000000000447. https://insights.ovid.com/crossref?an=00006982-201502000-00001 cited 2019 May 29. Available from: [DOI] [PubMed] [Google Scholar]
- 11.Sadaka A., Sisk R., Osher J., Toygar O., Duncan M., Riemann C. Intravitreal methotrexate infusion for proliferative vitreoretinopathy. Clin Ophthalmol. 2016 Sep 1;10:1811–1817. doi: 10.2147/OPTH.S111893. https://www.dovepress.com/intravitreal-methotrexate-infusion-for-proliferative-vitreoretinopathy-peer-reviewed-article-OPTH cited 2019 Feb 28. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shuang H., Yichun K. A case of perforating injury of eyeball and traumatic cataract caused by acupuncture. Indian J Ophthalmol. 2016 Apr 1;64(4) doi: 10.4103/0301-4738.182952. http://go.galegroup.com.proxy1.lib.uwo.ca/ps/i.do?p=AONE&u=lond95336&id=GALE%7CA453465227&v=2.1&it=r&sid=summon cited 2019 Feb 28. 326–326. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kao T.-E., Kuo Y.-W., Wu K.-Y. Acupuncture-related penetrating eye injury. Kaohsiung J Med Sci. 2017 Sep;33(9):473–474. doi: 10.1016/j.kjms.2017.05.006. cited 2019 Feb 28. Available from: [DOI] [PubMed] [Google Scholar]
- 14.Fielden M., Hall R., Kherani F., Crichton A., Kherani A. Ocular perforation by an acupuncture needle. Can J Ophthalmol. 2011 Feb;46(1):94–95. doi: 10.3129/i10-122. https://linkinghub.elsevier.com/retrieve/pii/S0008418211800232 cited 2019 Feb 28. Available from: [DOI] [PubMed] [Google Scholar]
- 15.Hardwig P.W., Pulido J.S., Bakri S.J. The safety OF intraocular methotrexate IN silicone-filled eyes. Retina. 2008 Sep;28(8):1082–1086. doi: 10.1097/IAE.0b013e3181754231. https://insights.ovid.com/crossref?an=00006982-200809000-00008 cited 2019 Mar 28. Available from: [DOI] [PubMed] [Google Scholar]
- 16.Fishbume B.C., Wilson D.J., Rosenbaum J.T., Neuwdt E.A. Intravitreal methotrexate as an adjunctive treatment of intraocular lymphoma. Arch Ophthalmol. 1997;115(9):1152–1156. doi: 10.1001/archopht.1997.01100160322009. Available from: [DOI] [PubMed] [Google Scholar]
- 17.Benner J.D., Dao D., Butler J.W., Hamill K.I. Intravitreal methotrexate for the treatment of proliferative vitreoretinopathy. BMJ Open Ophthalmol. 2019 Apr;4(1) doi: 10.1136/bmjophth-2019-000293. https://bmjophth.bmj.com/content/4/1/e000293 [cited 2019 Oct 29] 1. e000293. Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]